Abstract
Prior to Hurricane Maria, Puerto Rico already had 200+ hazardous waste sites, significant contamination of water resources, and among the highest rates of preterm birth in the US. To address these issues, the Puerto Rico Testsite for Exploring Contamination Threats (PROTECT) Center was formed in 2010 to investigate prenatal environmental exposures, particularly phthalates, and adverse birth outcomes. Recent work from the PROTECT study confirms that in utero exposure to certain phthalates is associated with shorter gestation and increased risk of preterm birth. However, previous research also suggests that pregnant women who experience a natural disaster such as Hurricane Maria are at higher risk of adverse birth outcomes, but it is unknown whether this is due to stress, hazardous exposures, or a combination of factors. Thus, the aim of this analysis was to characterize hurricane-related changes in phthalate exposures and experiences within the PROTECT cohort. Among 176 participants who were pregnant during or within 5 months after Maria, 122 completed a questionnaire on hurricane-related experiences. Questionnaire results and biomarkers of exposure suggest that participants did not have regular access to fresh foods and water during hurricane recovery, and almost half reported structural damage to their home. In addition, biomarker concentrations of phthalates commonly used in food packaging were higher among participants post-hurricane, while phthalates commonly used in personal care products were lower compared to pre-hurricane levels. Hurricane-related increases in phthalate exposure, as well as widespread structural damage, food and water shortages, and long-term absence of electricity and cell phone service, likely increased the risk of adverse birth outcomes among this already vulnerable population.
Keywords: Puerto Rico, Hurricane Maria, pregnancy, birth cohort, environmental exposures
Introduction
On September 6th, 2017, Hurricane Irma, the strongest storm ever recorded in the Atlantic, passed just north of Puerto Rico, causing severe damage and power outages. Just two weeks later, on September 20th, Hurricane Maria struck Puerto Rico as the most powerful hurricane to hit the island in over 80 years. Although the official death count is 2,975 (Milken Institute SPH 2018, Sanchez 2018), Kishore et al. estimate over 4,500 excess deaths attributable to Maria (Kishore et al. 2018). The US National Hurricane Center estimates that Hurricane Maria caused $65–115 billion in damage in Puerto Rico and the US Virgin Islands (Pasch et al. 2018), although other estimates have been much higher (Florido 2018). Hurricane Maria destroyed Puerto Rico’s already beleaguered power grid, such that it took almost a year for the Puerto Rico Electric Power Authority to restore power to their 1.4 million customers (Campisi and White 2018), and concerns that the Puerto Rico Aqueduct and Sewer Authority (PRASA) – Puerto Rico’s main water supplier – may not be able to supply safe drinking water remain (Hersher 2018; Milman 2018; Schmidt and Voisin 2018). According to FEMA estimates, hurricanes Irma and Maria also destroyed or caused major damage to over 13,000 homes in Puerto Rico (HUD 2018), although this does not include households who did not apply for FEMA aid. Due to the difficult and slow recovery, many Puerto Ricans are still living in hurricane-damaged, substandard housing, while over one hundred thousand have left for the mainland US (Census Bureau 2018; HUD 2018), and thousands more will likely leave the island in the following years (Melendez and Hinojosa 2017).
Natural disasters such as Hurricane Maria can have long-term physical and psychological health consequences particularly in vulnerable populations. Pregnant women exposed to such events are at higher risk of giving birth preterm (<37 weeks gestation), having low birthweight babies, and other adverse birth outcomes (Antipova and Curtis 2015; Currie and Rossin-Slater 2013; Grabich et al. 2016; Harville et al. 2010; Harville et al. 2015; Oni et al. 2015; Tong et al. 2011; Torche 2011; Xiong et al. 2008; Zahran et al. 2010; Zahran et al. 2014), which are in turn associated with neurocognitive disabilities and increased risk for metabolic disorders, obesity, and cardiovascular disease in offspring later in life (Barker 2006; Gluckman and Hanson 2006; Nobili et al. 2008). Indeed, limited studies have shown associations between the occurrence of natural disasters during gestation and poorer neurocognitive and metabolic outcomes in adulthood (Buekens et al. 2006; Sotomayor 2013). However, exactly what factors involved in experiencing a natural disaster during pregnancy play a role in increasing risk for adverse birth outcomes has not been explored. Identification of specific hurricane-related experiences, situations, environmental exposures, or other stressors that can impact birth outcomes would be valuable for emergency response planning and exposure reduction in natural disaster situations, and potentially minimize the effects of future events.
Prior to Hurricane Maria, Puerto Rico already had a significant health burden compared to the mainland US. For decades, rates of preterm birth rose dramatically in Puerto Rico to one of the highest in the world at 19.6% in 2008 (Blencowe et al. 2012; Martin et al. 2011). In 2017, the preterm birth rate in Puerto Rico was 11.4%, which although lower, is still much higher than the national average (9.8%) (March of Dimes 2017). This disparity may be due in part to high levels of contamination on the island, as well as lower socioeconomic status (SES) and high rates of poverty in Puerto Rico, which are linked to adverse birth outcomes (IOM 2007; Kramer et al. 2000; Shapiro et al. 2013).
Environmental contamination in Puerto Rico was extensive prior to the 2017 hurricane season, with 200+ hazardous waste sites including 18 active Superfund sites and significant contamination of water resources (EPA 2019; Padilla et al. 2011). Although the U.S Environmental Protection Agency (EPA) has not reported any major hurricane-related spills from current Superfund or other regulated sites (EPA 2018), flooding and damage caused by Maria likely exacerbated existing contamination. Residents of Puerto Rico were likely exposed to a range of hazardous substances during the long recovery after the storm through use of water from uncertain sources for drinking, cooking, and washing. In addition, food shortages during the aftermath of Maria may have led to increased consumption of canned and packaged foods, with reduced nutritional value and subsequent increases in exposure to phthalates, a class of chemicals used in a range of consumer products, including food packaging and processing materials, PVC plastics, and personal care products (CDC 2017). Prior research indicates that prenatal phthalate exposure is associated with increased risk of preterm birth and other adverse birth outcomes (Ferguson et al. 2014; Ferguson et al. 2019; Meeker et al. 2009), as well as a range of reproductive, metabolic, and neurodevelopmental outcomes in offspring (Ejaredar et al. 2015; Radke et al. 2018, 2019a, 2019b).
Hurricane-related environmental exposures, increased rates of depression, anxiety, and post-traumatic stress in the aftermath of Maria (Ferre et al. 2018; Ramphal 2018), and a loss of resources in an already challenging economic atmosphere, have created strong potential for increased risks of adverse birth outcomes in Puerto Rico. Prenatal maternal stress, anxiety, and depression are known risk factors for preterm birth (Dunkel Schetter and Tanner 2012; Roy-Matton et al. 2011; Shapiro et al. 2013) and low birth weight babies (Ashdown-Lambert 2005; Nkansah-Amankra et al. 2010), and hurricanes and other natural disasters can be tremendous sources of maternal stress (Harville et al. 2010; Oni et al. 2015; Torche 2011; Xiong et al. 2010). Disentangling the effects of hurricane-related stress and chemical exposures on adverse birth outcomes is an important public health issue, as this will highlight important target areas for prevention (Callaghan et al. 2007; Cordero 1993). In this analysis, we begin to address this research gap by characterizing hurricane-related experiences and phthalate exposure within an ongoing birth cohort in Puerto Rico.
In 2010, the Puerto Rico Testsite for Exploring Contamination Threats (PROTECT) cohort was started to study the effects of prenatal environmental exposures, particularly phthalates, on preterm birth on the island. Here we provide a brief overview of the ongoing hurricane-related research within the PROTECT cohort, characterize the post-hurricane PROTECT population and their experiences during Maria, and compare pre- and post-hurricane measures of phthalate exposure within PROTECT women.
Methods
Study Design
The PROTECT project is a prospective birth cohort in northern Puerto Rico testing the hypothesis that exposure to environmental contamination contributes to the high preterm birth rate in Puerto Rico. As of January 1, 2019, there were over 1200 PROTECT participants, and enrollment of pregnant women during their first trimester of pregnancy is ongoing. From this cohort, 102 PROTECT participants were actively pregnant at the time Hurricane Maria made landfall in Puerto Rico. We have an expansive dataset of environmental, clinical, social, demographic, behavioral, and dietary information on PROTECT mothers, as well as repeated prenatal biospecimens, which enables us to evaluate these factors both before and after Maria.
Prior to 16 weeks gestation, pregnant women visiting participating prenatal clinics are approached by their nurse and/or physician about the study, screened for eligibility, and, if eligible and interested in participating, give informed consent. Exclusion criteria include residing outside the study region, age (<18 or >40 years), multiple gestations, medical complications (e.g., diabetes, hypertension, liver/kidney disease), no first-trimester ultrasound for gestational age, oral contraceptives within three months prior to pregnancy, and pregnancies stemming from assisted reproductive technologies. Participating women provide urine and blood samples and complete extensive interview questionnaires at each visit (Figure 1): Visit 1 (V1; 16–20 wks), Visit 2 (V2; 20–24 wks), Visit 3 (V3; 24–28 wks), and at delivery. Detailed medical information is collected via systematic abstraction of medical record data. Women enrolled in PROTECT are approached at the third study visit regarding potential enrollment of their child into the CRECE cohort, which involves assessments of infant growth, neurodevelopment, and respiratory health from birth through 4 years of age (birth, 4–6 weeks, 6–8 months, annually).
Figure 1.
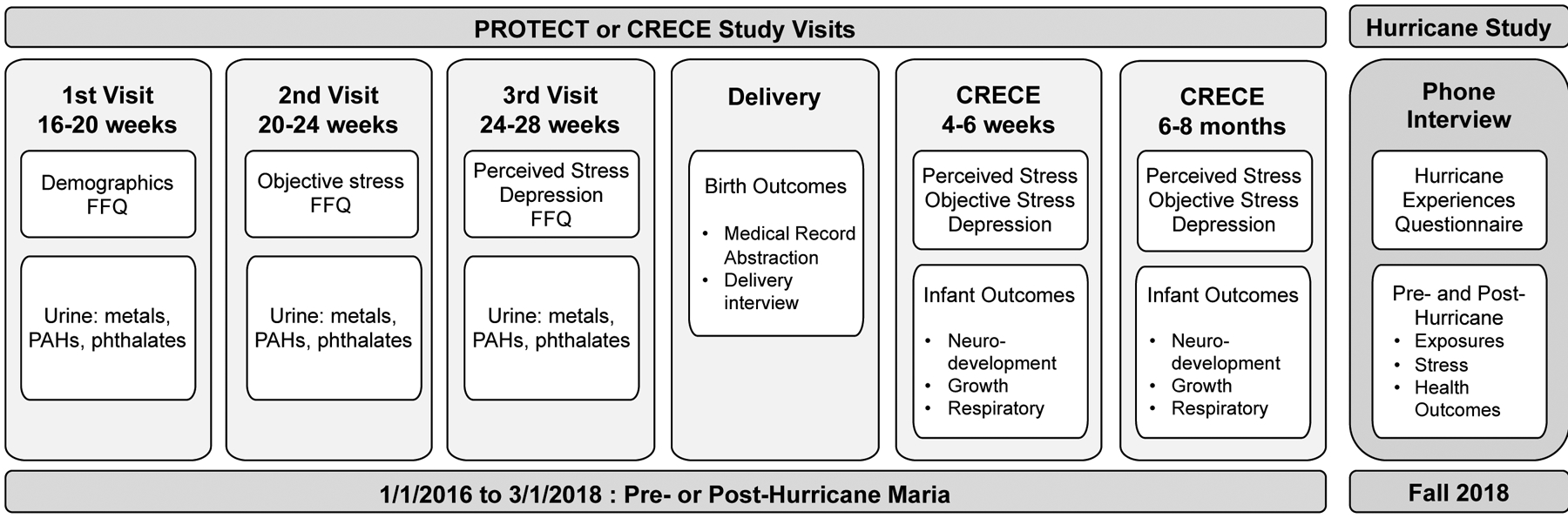
PROTECT, CRECE, and Hurricane Study Design
In the larger ongoing PROTECT “Hurricane Study”, we are utilizing the existing PROTECT and CRECE infrastructure to assess hurricane-related exposure to a range of environmental exposures and stress, and evaluating subsequent effects on adverse birth outcomes and infant development through one year of age (Figure 1). In the present analysis, we assessed pre- and post-hurricane phthalate levels, as these chemicals have been associated with increased risk of adverse birth outcomes, both in PROTECT and other birth cohorts (Ferguson et al. 2014; Ferguson et al. 2019). Women were grouped into three categories: 1) pregnant and delivered prior to Hurricanes Irma and Maria; 2) pregnant during Hurricane Maria; and 3) became pregnant in the 5 months after Hurricane Maria. To reduce the effect of temporal trends in exposure (Johns et al. 2015; Zota et al. 2014), group 1 was restricted to women who became pregnant and enrolled in PROTECT after January 1, 2016. Women in groups 2 and 3 were contacted to participate in a phone-administered questionnaire to collect information on their experiences during Hurricane Maria. If specific phthalate metabolites were significantly higher post-hurricane, we then used questionnaire responses to attempt to identify potential sources of exposure.
Hurricane Experience Questionnaire
To characterize experiences that PROTECT women may have had either during Hurricane Maria or during recovery, we designed a hurricane experience questionnaire to collect this information in a systematic manner. Although there are no standard questionnaires for assessing disaster experiences, we based our questionnaire on two commonly used scales: The Traumatic Exposure Severity Scale (TESS) (Chan and Rhodes 2014; Elal and Slade 2005) and the Hurricane Related Traumatic Experiences Questionnaire (HURTE) (Chan and Rhodes 2014; Vernberg et al. 1996). Questions from these scales were selected and modified based on our study population and experiences specific to Hurricane Maria and Puerto Rico. Participants were asked to answer questions on storm-related damage to housing, injuries to participants, families, and friends, illness, power availability, availability and sources of food and water, pesticide exposure, noise, financial difficulties, and medical and prenatal care based on their experiences in the immediate aftermath of Hurricane Maria. The questionnaire was translated from English to Spanish by bilingual native Puerto Rican Spanish speakers.
Administration of the Hurricane Experience Questionnaire began in late August 2018 (Figure 1). Participants who were identified as having been pregnant either during or within the 5 months after Hurricane Maria were then called using the main contact number provided upon PROTECT enrollment, and invited to participate in the questionnaire over the phone. If participants did not answer their phone, a text message was sent informing them of the questionnaire. Participants were called twice, texted twice, then called twice again before being considered “unreachable”. Alternative phone numbers previously provided by participants were also used to contact hard to reach women. The Hurricane Experience Questionnaire and the overall PROTECT study were approved by the University of Puerto Rico Medical Sciences Campus Institutional Review Board (IRB).
PROTECT questionnaires
PROTECT questionnaires given to all participants at each study visit combine elements from the National Health and Nutrition Examination Survey (NHANES), the National Health Interview Survey, the Birth Defects Prevention Study, and the National Children’s Study, with modifications to capture important local Puerto Rico patterns or variables. These questionnaires were translated into Spanish by bilingual native Puerto Rican Spanish speakers, and were used to collect information on demographics, SES (income, health insurance, education), BMI, smoking, and reproductive history at V1.
Exposure Assessment
We examined pre- and post-hurricane exposure to phthalates, as these chemicals are present in food packaging, canned food, and storage containers, and the limited availability of fresh food after Maria has likely increased intake of pre-packaged foods. Exposure to these chemicals was assessed by measuring compound-specific biomarkers in urine samples provided by PROTECT women at each prenatal study visit (V1, V2, V3).
Spot urine samples were collected into polypropylene containers, labeled, and placed on ice for transport to the University of Puerto Rico (UPR) laboratory, where specific gravity was measured to account for urine dilution (Boeniger et al. 1993). Samples were divided into 2 mL aliquots and frozen at −80C until overnight shipment to the Center for Disease Control and Prevention (CDC) Division of Laboratory Sciences for phthalate analysis. A panel of 16 phthalate and phthalate replacement metabolites, comprised of mono(2-ethylhexyl) phthalate (MEHP), mono(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP), mono(2-ethyl-5-oxohexyl) phthalate (MEOHP), mono(2-ethyl-5-carboxypentyl) phthalate (MECPP), mono-benzyl phthalate (MBzP), monocarboxyoctyl phthalate (MCOP), monocarboxynonyl phthalate (MCNP), monooxoisononyl phthalate (MONP), mono (3-carboxypropyl) phthalate (MCPP), mono-ethyl phthalate (MEP), mono-n-butyl phthalate (MBP), mono-3-hydroxybutyl phthalate (MHBP), mono-isobutyl phthalate (MiBP) and mono-2-hydroxy-iso-butyl phthalate (MHiBP), mono-2-ethyl-5-carboxypentyl terephthalate (MECPTP), and mono-2-ethyl-5-hydroxyhexyl terephthalate (MEHHTP), were measured in urine samples using isotope dilution liquid chromatography-tandem mass spectrometry (LC-MS/MS), an approach well described in the literature (Lewis et al. 2013; Silva et al. 2004; Silva et al. 2018).
Statistical Analysis
Demographic statistics such as age, income, education, and marital status for participants pregnant during Hurricane Maria were calculated and compared to participants who delivered prior to Maria or became pregnant after Maria. Statistically significant differences between groups were determined using linear regression for continuous variables (age) and logistic regression for dichotomous or ordinal variables (income and education categories, and marital status). Summary statistics for the number of participants who have thus far completed the hurricane questionnaire, as well as information on loss to follow-up after Maria, were also calculated.
Prior to data analyses, phthalate metabolite concentrations were corrected for specific gravity to adjust for urinary dilution using the equation Pc=P (1.019–1)/(SG-1) where Pc = corrected metabolite concentration, P = measured metabolite concentration, SG = specific gravity of the sample, and 1.019 = median specific gravity of all samples collected (Meeker et al. 2009). Corrected phthalate metabolite concentrations were right skewed, and therefore natural log-transformed to obtain a normal distribution. Linear mixed effect models were used to assess the impact of Maria on urinary phthalate metabolite levels to determine hurricane-related changes in phthalate exposure. To do this, a dichotomous time variable (pre- vs. post-hurricane) was entered into models predicting exposure measures, while controlling for within individual correlations over time. To determine if phthalates were higher directly after Hurricane Maria, post-hurricane samples from only the first three months after the storm were included in models, while all post-hurricane samples were included in models to determine if phthalates remained high during the extended recovery period.
To potentially link phthalate levels to hurricane-related experiences, we evaluated specific questionnaire responses as predictors of post-hurricane phthalate concentrations. Only phthalate metabolites that were significantly higher post-hurricane and questions related, based on prior knowledge, to potential exposure to those specific phthalates were assessed.
Results
Characteristics of PROTECT mothers who became pregnant after January 1, 2016 and who gave birth prior to Hurricane Maria (n=160), were pregnant during Hurricane Maria (n=102), and became pregnant in the 5 months after Hurricane Maria (n=76) are shown in Table 1. On average, women in the three categories were of similar age (28–29 years) and just under 90% were married or living with their partner. Participants who were pregnant during Hurricane Maria were less likely to be in a lower income category (OR=0.46; 95%CI=0.27, 0.77) and less likely to be in a lower education category (OR=0.62; 95%CI=0.39, 0.98) compared to participants who gave birth before the hurricane. However, women who became pregnant after Hurricane Maria were not significantly different from women who gave birth before Hurricane Maria in either income or education.
Table 1.
Characteristics of PROTECT participants by timing of pregnancy in relation to Hurricane Maria
| Delivery prior to Hurricane Maria | Pregnant during Hurricane Maria | Became pregnant after Hurricane Maria | ||||
|---|---|---|---|---|---|---|
| N=160 | N=102 | N=74 | ||||
| Characteristic | n | (mean, SD) | n | (mean, SD) | n | (mean, SD) |
| Age | 159 | 27.9 (5.5) | 102 | 28.8 (5.1) | 74 | 28.0 (5.2) |
| n | % | n | % | n | % | |
| Education* | ||||||
| High School or less | 21 | 13.1 | 7 | 6.9 | 9 | 12.2 |
| Some college/Associate | 54 | 33.8 | 28 | 27.5 | 23 | 31.1 |
| Bachelor’s | 60 | 37.5 | 44 | 43.1 | 28 | 37.8 |
| Master’s/Doctoral | 21 | 13.1 | 18 | 17.6 | 10 | 13.5 |
| missing | 4 | 2.5 | 5 | 4.9 | 4 | 5.4 |
| Income* | ||||||
| <$20,000 | 69 | 43.1 | 23 | 22.5 | 23 | 31.1 |
| $20,000-$49,999 | 62 | 38.8 | 47 | 46.1 | 33 | 44.6 |
| >$50,000 | 16 | 10.0 | 15 | 14.7 | 9 | 12.2 |
| missing | 13 | 8.1 | 17 | 16.7 | 9 | 12.2 |
| Marital status | ||||||
| Married/Living Together | 140 | 87.5 | 88 | 86.3 | 65 | 87.8 |
| Single/Divorced | 17 | 10.6 | 10 | 9.8 | 5 | 6.8 |
| missing | 3 | 1.9 | 4 | 3.9 | 4 | 5.4 |
Statistically significant difference between participants pregnant during Hurricane Maria and participants who gave birth prior to Hurricane Maria (p<0.05).
Among the 102 women who were pregnant when Hurricane Maria struck Puerto Rico, 73% completed the questionnaire, 3% declined, and 24% were unreachable (Table 2). Among women who became pregnant after Maria, slightly higher percentages declined (5%) or were unreachable (30%), while slightly fewer completed the questionnaire (65%). Among women who were unreachable, there were a total of 6 with phone numbers that were no longer in service.
Table 2.
Administration status of Hurricane Experience Questionnaire among PROTECT participants who were pregnant during or who became pregnant after Hurricane Maria.
| Hurricane Experience Questionnaire Administration | ||
|---|---|---|
| Participants pregnant during Hurricane Maria (n=102) | ||
| Status | n | % |
| Completed | 74 | 72.6 |
| Declined | 3 | 2.9 |
| Total unreachable | 25 | 24.5 |
| No answer | 24 | |
| Disconnected | 1 | |
| Participants who became pregnant in the 5 months after Hurricane Maria (n=74) | ||
| Status | n | % |
| Completed | 48 | 64.9 |
| Declined | 4 | 5.4 |
| Total unreachable | 22 | 29.7 |
| No answer | 17 | |
| Disconnected | 5 | |
Results of select questions from the questionnaire are presented in Figure 2. Regarding health, 30% reported post-hurricane illnesses, including gastrointestinal and respiratory illnesses, fever, headache, and colds, and 11% reported that they had trouble accessing health services or medications in the hurricane aftermath. Almost half of respondents reported having hurricane-related structural damage to their home, including damage to ceilings, walls, windows, or doors (n=58), and 40% of these women (n=23) report that their house had not yet been repaired at the time questionnaire administration. Many also reported having mold (25%), mice (26%), or mosquitoes (75%) in or around their home after Maria. The median reported number of days without electricity was 90 days, but this ranged from 7 days to over a year. Many respondents did report having a generator at their home (86%), but many had trouble getting fuel for generators or vehicles in the first weeks after the hurricane (75%). Almost a quarter of respondents (24%) were still not living in their own residence a year after Hurricane Maria. In addition, 80% reported not having cell phone or internet service after Maria, limiting communication with family, friends, and emergency and recovery services. Finally, only 14% of participants said they did not have PRASA water in the first months after Maria, although only 2% reported drinking tap water while 98% reported drinking bottled water. In addition, 13% of PROTECT participants did not have access to adequate food.
Figure 2.
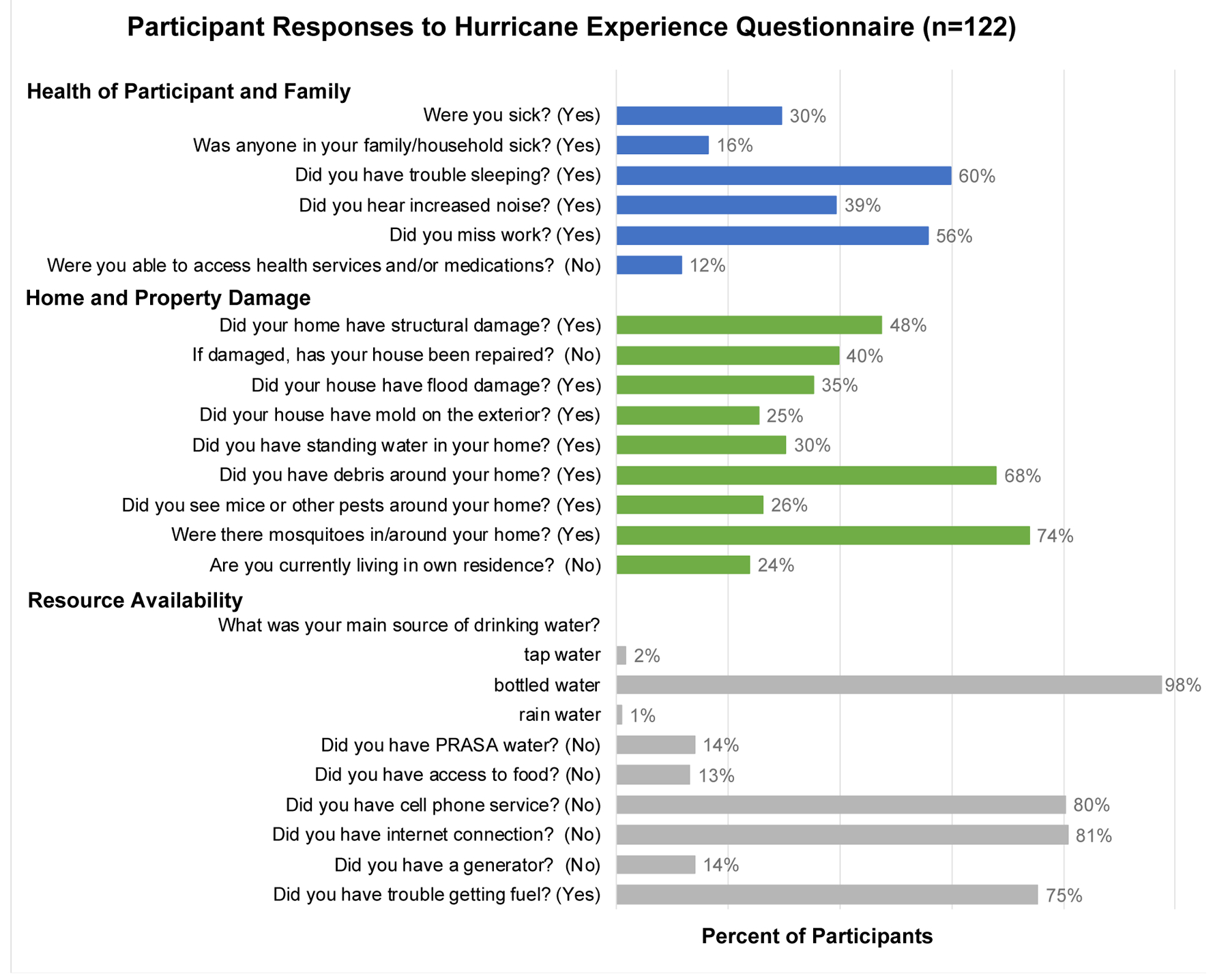
Responses to the Hurricane Experiences Questionnaire among PROTECT participants pregnant during or after Hurricane Maria (n=122).
Distributions of urinary phthalate metabolite concentrations in samples collected from PROTECT women before and after Hurricane Maria are presented in Table 3. Metabolites of phthalates used in PVC plastics, including MECPTP, MEHHTP, and MONP, were significantly higher in post-hurricane samples, with geometric mean MECPTP concentrations increasing from 31.4 ng/ml pre-hurricane to 46.0 ng/ml in samples collected within the 3 months post-hurricane, and geometric mean concentrations of MEHHTP increasing from 4.97 ng/ml pre-Maria to 8.14 ng/ml post-Maria. During this same time period, urinary concentrations of MEP, a metabolite of a phthalate often used in personal care products, decreased from 40.6 ng/mL to 28.8 ng/mL. MECPP concentrations were also lower in post-hurricane samples, but this difference disappeared when we only considered post-hurricane samples that were collected within 3 months of Hurricane Maria.
Table 3.
Specific gravity adjusted urinary phthalate metabolite concentrations in samples collected from PROTECT participants before and after Hurricane Maria.
| Urinary Phthalate Metabolite Concentrations (ng/mL) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Samples collected PRE-MARIAa | Samples collected within 5 months POST-MARIA | Samples collected within 3 months POST-MARIA | ||||||||||||
| (n=530 samples, 215 women) | (n= 206 samples, 100 women) | (n= 62 samples, 48 women) | ||||||||||||
| GM | GSD | 25th% | 95th% | GM | GSD | 25th% | 95th% | P for Δb | GM | GSD | 25th% | 95th% | P for Δc | |
| MEHP | 1.98 | 2.50 | 1.14 | 8.28 | 1.69 | 2.50 | 1.03 | 9.01 | 0.13 | 1.87 | 2.54 | 1.14 | 11.4 | 0.81 |
| MECPP | 11.0 | 2.12 | 6.86 | 36.4 | 8.86 | 1.94 | 5.70 | 31.0 | 0.03 | 10.9 | 1.84 | 7.36 | 31.0 | 0.74 |
| MEHHP | 5.98 | 2.38 | 3.80 | 23.7 | 5.17 | 1.91 | 3.34 | 22.0 | 0.19 | 5.86 | 2.01 | 3.93 | 23.8 | 0.86 |
| MEOHP | 5.32 | 2.41 | 3.17 | 20.5 | 4.92 | 1.94 | 3.13 | 21.7 | 0.57 | 5.58 | 2.01 | 3.55 | 23.4 | 0.57 |
| MBzP | 2.16 | 2.98 | 1.06 | 15.6 | 2.05 | 3.16 | 0.95 | 18.7 | 0.84 | 2.33 | 3.02 | 0.95 | 18.7 | 0.44 |
| MCPP | 0.92 | 2.53 | 0.51 | 4.53 | 0.89 | 2.36 | 0.54 | 3.33 | 0.60 | 0.94 | 2.66 | 0.51 | 6.97 | 0.86 |
| MCNP | 0.92 | 2.10 | 0.84 | 4.82 | 1.28 | 2.11 | 0.76 | 6.26 | 0.31 | 1.38 | 2.03 | 0.87 | 5.59 | 0.98 |
| MCOP | 6.18 | 2.50 | 3.48 | 28.6 | 5.91 | 2.90 | 3.17 | 52.9 | 0.58 | 7.30 | 2.92 | 3.64 | 58.1 | 0.23 |
| MONP | 1.96 | 2.83 | 1.02 | 10.8 | 2.47 | 2.93 | 1.21 | 17.9 | 0.02 | 2.66 | 2.88 | 1.27 | 30.0 | 0.06 |
| MEP | 40.6 | 4.88 | 12.4 | 768 | 29.4 | 4.73 | 9.20 | 542 | 0.05 | 28.8 | 4.19 | 9.82 | 472 | 0.08 |
| MBP | 13.4 | 2.56 | 7.43 | 58.6 | 12.4 | 2.29 | 7.16 | 56.9 | 0.77 | 15.5 | 2.43 | 8.49 | 77.6 | 0.27 |
| MIBP | 8.68 | 2.52 | 4.70 | 44.7 | 7.81 | 2.23 | 4.39 | 29.3 | 0.66 | 8.93 | 2.18 | 5.45 | 34.5 | 0.67 |
| MHBP | 1.37 | 2.59 | 0.74 | 6.61 | 1.23 | 2.42 | 0.79 | 6.15 | 0.51 | 1.58 | 2.48 | 0.89 | 9.69 | 0.32 |
| MHIBP | 3.76 | 2.42 | 2.07 | 17.6 | 3.19 | 2.21 | 1.82 | 12.2 | 0.23 | 3.51 | 2.27 | 2.17 | 13.7 | 0.78 |
| MECPTP | 31.4 | 3.45 | 13.6 | 381 | 41.5 | 3.87 | 15.4 | 676 | 0.01 | 46.0 | 4.48 | 14.3 | 659 | 0.03 |
| MEHHTP | 4.97 | 3.42 | 2.09 | 59.6 | 7.95 | 3.55 | 3.07 | 92.5 | <.0001 | 8.14 | 4.46 | 2.85 | 74.2 | 0.006 |
Pre-Maria samples restricted to women who became pregnant after 1/1/2016; Women pregnant during Maria could contribute to both PRE-MARIA and POST-MARIA samples depending on timing of urine sample collection.
p-values for difference between pre-hurricane samples and all post-hurricane samples, from mixed models accounting for within person correlation across samples. Blue shading indicates lower post-Maria concentrations, orange shading indicates higher post-Maria concentrations.
p-values for difference between pre-hurricane samples and post-hurricane samples collected in 2017 (within approximately 3 months after Hurricane Maria), from mixed models accounting for within person correlation across samples. Blue shading indicates lower post-Maria concentrations, orange shading indicates higher post-Maria concentrations.
Although bottled water is a potential source of phthalate exposure, 98% of our participants predominantly drank bottled water after the hurricane, limiting our ability to assess associations between bottled water and significantly higher phthalate metabolites (MONP, MEHHTP, and MECPTP). However, participants who reported having access to food after the hurricane did have somewhat higher concentrations of MEHHTP, and MECPTP, although this is based on a small sample size (42 participants answered this question and had post-hurricane phthalate measurements) and the findings were not significant (p=0.1 for MEHHTP and MECPTP). Having PRASA water after Maria was not associated with changes in urinary MONP, MEHHTP, or MECPTP, although very few participants reported drinking this water (n=2).
Discussion
After Hurricane Maria hit Puerto Rico in September 2017, the PROTECT and CRECE study clinic reopened within 2 weeks, and our research team resumed study recruitment within 1 month. However, the full impact of Maria on the PROTECT and CRECE projects, including our research team in Puerto Rico, study participants, and the surrounding community, are still coming to light. Preliminary findings presented here indicate that patterns of phthalate exposure were altered in the months after Hurricane Maria, with higher urinary metabolite concentrations of compounds used as plasticizers in PVC plastics and food packaging, and lower concentrations of compounds commonly associated with personal care products. In addition, pregnant women who continued to participate in PROTECT or who became pregnant and enrolled in PROTECT in the aftermath of Maria had on average higher incomes and more education compared to previous PROTECT participants, suggesting that women with fewer resources had greater barriers to participation during the storm aftermath. These factors highlight that pregnant women are an especially vulnerable population during natural disasters, as increased environmental exposures and lack of prenatal care put women at risk of adverse birth outcomes. The ongoing study of the effects of Hurricane Maria on maternal stress, chemical exposures, and birth and infant outcomes within the PROTECT and CRECE cohorts will continue to examine the long-term effects of this devastating storm.
Post Hurricane Demographics
Women who were pregnant during Hurricane Maria and remained in PROTECT after the storm were of higher SES (i.e. income, education) compared to women who had previously participated in PROTECT. Participating in the PROTECT study may have been a lower priority for women with fewer resources after Hurricane Maria, as effort was likely directed toward addressing primary needs, such as adequate food, water, and shelter. In contrast, women with adequate resources may have actively sought out participation as a way to enhance their prenatal care during a time when the medical system in Puerto Rico was under a great deal of stress (Ramphal 2018). This finding indicates the need to put extra effort into getting needed care to less-resourced women, as they may be at higher risk for adverse birth outcomes, and to encourage vulnerable populations to seek care from a range of sources, including both clinical and research organizations, in disaster situations.
Hurricane Experience Questionnaire
Despite having slightly higher income and education compared to PROTECT participants who gave birth prior to Hurricane Maria, women who were enrolled in PROTECT and pregnant during and after Hurricane Maria experienced a substantial amount of hardship during the hurricane recovery efforts. While pregnant, many participants dealt with health concerns, damage to their homes and property, loss of communication, and hazardous environmental threats, such as contaminated water, mold, pests, heat, and debris. These experiences likely represent those of many pregnant women in Puerto Rico after Maria, as PROTECT participants are from a relatively large, diverse area on the north coast of Puerto Rico that was directly hit by the storm and includes both urban and rural areas. However, because higher SES populations generally have more resources to aid recovery in disaster situations, it is possible that participants who continued to participate in PROTECT and responded to the Hurricane Experience Questionnaire may have fared better in the aftermath of Hurricane Maria compared to the general population, but this is currently unknown. In our continuing work we will assess relationships between specific experiences reported through the questionnaire and measures of perceived stress, depression, and environmental exposures, as well as birth and child development outcomes.
Interpreting Findings of Post-Hurricane Phthalate Exposure
Urinary concentrations of MONP and terephthalate metabolites were higher in samples collected in the three to five months after Hurricane Maria compared to samples collected before, suggesting increased exposure to the parent compounds, diisononyl phthalate (DINP) and di(2-ethylhexyl)terephthalate (DEHTP), respectively. These chemicals are widely used as plasticizers in PVC plastics for a range of applications, so increased post-hurricane exposure could have originated from a range of sources. For example, potable water was likely stored and distributed in plastic containers, potentially leaching phthalates into the water and leading to increased exposure through ingestion. In the immediate aftermath of Maria, fresh food was also scarce and relief supplies sent to the island included predominantly packaged and processed foods, which are another potential source of phthalate exposure. Our findings that participants who reported having access to food after Maria had marginally higher levels of terephthalate metabolites compared to participants that didn’t does suggest that packaged foods may have been a source of increased post-hurricane DEHTP exposure. In contrast, urinary concentrations of MEP, a metabolite of diethyl phthalate (DEP), were lower after Hurricane Maria. DEP is used primarily in personal care products such as perfume and lotions, so this finding is consistent with participants changing their grooming habits, potentially as a result of reduced access to clean water or electricity, or efforts being directed towards meeting primary needs of food and drinking water. Comparative studies of other disasters could confirm our interpretation regarding increased phthalate exposure related to food and water packaging. If determined to be a significant source of contaminant exposure during emergency relief situations, disaster professionals could then implement changes to food and water storage containers and packaging.
Increases in phthalate exposure in the aftermath of a disaster is concerning, as it is unknown how the effects of exposure may differ in times of high stress. For example, prenatal exposure to specific phthalates has been associated with increased risk of preterm birth within multiple birth cohorts, including the PROTECT cohort prior to Hurricane Maria (Ferguson et al. 2014; Ferguson et al. 2019; Meeker et al. 2009), and prenatal maternal stress is another important risk factor for adverse birth outcomes (Dunkel Schetter and Tanner 2012; Roy-Matton et al. 2011; Shapiro et al. 2013; Torche 2011). In addition, concentrations of MONP, MECPTP, and MEHHTP were not only significantly higher after Maria, they were also higher compared to levels among NHANES participants, who are representative of the general US population. For example, the geometric mean and 95th percentile of MECPTP concentrations from samples collected within 5 months after Maria were 41.5 and 676 ng/mL, while the the geometric mean and 95th percentiles reported among females in NHANES (2015–2016) were 18.8 and 361 ng/mL (CDC 2019). This drastic shift in phthalate distributions sugggests that more women had relatively high levels of phthalate exposure after the hurricane, potentially putting them at increased risk of adverse birth outcomes.
Strengths and Limitations
The primary strength of this ongoing work is the utilization of the existing PROTECT research infrastructure and availability of pre- and post-hurricane measures of maternal stress, environmental exposures, and birth outcomes. However, a main limitation is the substantial amount of time that passed between when Hurricane Maria struck Puerto Rico and the administration of the Hurricane Experiences Questionnaire. Although efforts were made to expedite this time-sensitive work, we were not able to begin until 11–12 months after Maria. To address this limitation in future studies, we urge cohorts to develop protocols for rapid response approaches in case of emergency situations so that they will be prepared to provide aid and implement research protocols when needed. To help with the informed consent process, the National Institute of Environmental Health Sciences (NIEHS) has developed an IRB protocol that can be used for such rapid response (NIEHS 2018).
Almost 70% of PROTECT women who were pregnant during or in the aftermath of Hurricane Maria have completed the Hurricane Experience Questionnaire, which is considerable given that we began contacting participants 11 months after the storm. Information from the questionnaire provided us with a clearer understanding of potential disparities within our study area and population in emergency situations (e.g. access to food). Among the 26% of women who were unreachable after numerous attempts to contact them, it is unknown whether they did not respond because they were not interested in participating, did not want to discuss their experiences, or if they never received the messages (e.g. no longer at the phone number on file). Women whose phone numbers were no longer in service (n=6) may have been displaced after the hurricane, but we have been unable to confirm this.
In addition, although we based the Hurricane Experiences Questionnaire on other scales designed to capture experiences during a disaster, we modified the questions to specifically address our PROTECT population and the situation after Hurricane Maria. As a result, the questionnaire had not been previously validated. In addition, recall of specific hurricane-related experiences may have become less accurate over time, which may have affected our ability to fully characterize hurricane-related experiences in our cohort. However, considering the strength of the storm, the resulting devastation on the island, and the impact it had on many people’s lives, it may take much longer for Puerto Ricans to forget Hurricane Maria.
Conclusions
Our findings suggest that Hurricane Maria had a significant impact on pregnant women in Puerto Rico, altering environmental exposures and influencing decisions regarding pregnancy and access to prenatal care. This work is ongoing, but our findings will ultimately be valuable for emergency response planning and exposure reduction in natural disaster situations, as well as identify ways to minimize the effects of future hurricanes on birth and developmental outcomes.
Acknowledgments
This work is supported by the National Institute of Environmental Health Sciences (NIEHS) grants R21ES029751, P42ES017198, P50ES026049, R21MD013709, and UG3OD023251, EPA grant R836155, and National Institute on Minority Health and Health Disparities grants U54MD007600 and R21MD013709. We would like to thank Drs. Antonia Calafat and Xiaoyun Ye at the Centers for Disease Control and Prevention for the measurement of phthalate metabolites in PROTECT urine samples. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the NIEHS, EPA, or CDC.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
REFERENCES
- Antipova A, Curtis A. 2015. The post-disaster negative health legacy: Pregnancy outcomes in Louisiana after hurricane Andrew. Disasters 39:665–686. [DOI] [PubMed] [Google Scholar]
- Ashdown-Lambert JR. 2005. A review of low birth weight: Predictors, precursors and morbidity outcomes. J R Soc Promot Health 125:76–83. [DOI] [PubMed] [Google Scholar]
- Barker DJ. 2006. Adult consequences of fetal growth restriction. Clin Obstet Gynecol 49:270–283. [DOI] [PubMed] [Google Scholar]
- Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al. 2012. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. Lancet 379:2162–2172. [DOI] [PubMed] [Google Scholar]
- Boeniger MF, Lowry LK, Rosenberg J. 1993. Interpretation of urine results used to assess chemical exposure with emphasis on creatinine adjustments: A review. Am Ind Hyg Assoc J 54:615–627. [DOI] [PubMed] [Google Scholar]
- Buekens P, Xiong X, Harville E. 2006. Hurricanes and pregnancy. Birth 33:91–93. [DOI] [PubMed] [Google Scholar]
- Bureau Census. 2018. Puerto Rico population estimates.
- Callaghan WM, Rasmussen SA, Jamieson DJ, Ventura SJ, Farr SL, Sutton PD, et al. 2007. Health concerns of women and infants in times of natural disasters: Lessons learned from Hurricane Katrina. Matern Child Health J 11:307–311. [DOI] [PubMed] [Google Scholar]
- Campisi J, White J. 2018. Finally, 11 months after Maria, power is restored in Puerto Rico — except for 25 customers. Available: https://www.cnn.com/2018/08/07/us/puerto-rico-maria-power-restored-wxc-trnd/index.html [accessed Janurary 10 2019].
- Centers for Disease Control and Prevention (CDC). 2019. Fourth national report on human exposure to environmental chemicals. Updated tables, January 2019. Atlanta, GA. [Google Scholar]
- Chan CS, Rhodes JE. 2014. Measuring exposure in Hurricane Katrina: A meta-analysis and an integrative data analysis. PloS One 9:e92899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordero JF. 1993. The epidemiology of disasters and adverse reproductive outcomes: Lessons learned. Environ Health Perspect 101 Suppl 2:131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J, Rossin-Slater M. 2013. Weathering the storm: Hurricanes and birth outcomes. J Health Econ 32:487–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel Schetter C, Tanner L. 2012. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr Opin Psychiatry 25:141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ejaredar M, Nyanza EC, Ten Eycke K, Dewey D. 2015. Phthalate exposure and childrens neurodevelopment: A systematic review. Environ Res 142:51–60. [DOI] [PubMed] [Google Scholar]
- Elal G, Slade P. 2005. Traumatic exposure severity scale (tess): A measure of exposure to major disasters. J Trauma Stress 18:213–220. [DOI] [PubMed] [Google Scholar]
- EPA. 2018. Hurricane Maria response. Available: https://response.epa.gov/site/site_profile.aspx?site_id=12403 [accessed January 16 2018]. [Google Scholar]
- EPA. 2019. National priorities list (npl) sites - by state. Available: https://www.epa.gov/superfund/national-priorities-list-npl-sites-state#PR [accessed March 1, 2019].
- Ferguson KK, McElrath TF, Meeker JD. 2014. Environmental phthalate exposure and preterm birth. JAMA Pediatr 168:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson KK, Rosen EM, Rosario Z, Feric Z, Calafat AM, McElrath TF, Velez Vega C, Cordero JF, Alshawabkeh A, Meeker JD. 2019. Environmental phthalate exposure and preterm birth in the PROTECT birth cohort. Environ Int 132:105099. doi: 10.1016/j.envint.2019.105099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferre IM, Negron S, Shultz JM, Schwartz SJ, Kossin JP, Pantin H. 2018. Hurricane Maria’s impact on Punta Santiago, Puerto Rico: Community needs and mental health assessment six months postimpact. Disaster Med Public Health Prep 1–6. [DOI] [PubMed] [Google Scholar]
- Florido A 2018. Puerto Rico estimates it will cost $139 billion to fully recover from Hurricane Maria. All Things Considered. Available: https://www.npr.org/2018/08/09/637230089/puerto-rico-estimates-it-will-cost-139-billion-to-fully-recover-from-hurricane-m [accessed March 1, 2019]. [Google Scholar]
- Gluckman PD, Hanson MA. 2006. The consequences of being born small - an adaptive perspective. Horm Res 65 Suppl 3:5–14. [DOI] [PubMed] [Google Scholar]
- Grabich SC, Robinson WR, Engel SM, Konrad CE, Richardson DB, Horney JA. 2016. Hurricane Charley exposure and hazard of preterm delivery, Florida 2004. Matern Child Health J 20:2474–2482. [DOI] [PubMed] [Google Scholar]
- Harville E, Xiong X, Buekens P. 2010. Disasters and perinatal health: A systematic review. Obstet Gynecol Surv 65:713–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harville EW, Giarratano G, Savage J, Barcelona de Mendoza V, Zotkiewicz T. 2015. Birth outcomes in a disaster recovery environment: New Orleans women after Katrina. Matern Child Health J 19:2512–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hersher R 2018. Puerto Rico’s tap water often goes untested, raising fears about lead contamination. Available: https://www.npr.org/sections/health-shots/2018/09/20/645625805/puerto-ricos-tap-water-often-goes-untested-raising-fears-about-lead-contaminatio [accessed January 10 2019].
- Department of Housing and Urban Development (HUD). 2018. Hurricanes Irma and Maria: Housing damage assessment and recovery strategies report Puerto Rico.
- Institute of Medicine (IOM) Committee on Understanding Premature Birth, Assuring Healthy Outcomes. 2007. In: Preterm birth: Causes, consequences, and prevention. (Behrman RE, Butler AS, eds). National Academies Press; [PubMed] [Google Scholar]
- Johns LE, Cooper GS, Galizia A, Meeker JD. 2015. Exposure assessment issues in epidemiology studies of phthalates. Environ Int 85:27–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishore N, Marques D, Mahmud A, Kiang MV, Rodriguez I, Fuller A, et al. 2018. Mortality in Puerto Rico after Hurricane Maria. N Engl J Med 379:162–170. [DOI] [PubMed] [Google Scholar]
- Kramer MS, Seguin L, Lydon J, Goulet L. 2000. Socio-economic disparities in pregnancy outcome: Why do the poor fare so poorly? Paediatr Perinat Epidemiol 14:194–210. [DOI] [PubMed] [Google Scholar]
- Lewis RC, Meeker JD, Peterson KE, Lee JM, Pace GG, Cantoral A, et al. 2013. Predictors of urinary bisphenol A and phthalate metabolite concentrations in Mexican children. Chemosphere 93:2390–2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March of Dimes. 2017. Premature birth report cards. Available: https://www.marchofdimes.org/mission/prematurity-reportcard.aspx [accessed March 1, 2019].
- Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Kirmeyer S, Mathews TJ, et al. 2011. Births: Final data for 2009. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 60:1–70. [PubMed] [Google Scholar]
- Meeker JD, Hu H, Cantonwine DE, Lamadrid-Figueroa H, Calafat AM, Ettinger AS, et al. 2009. Urinary phthalate metabolites in relation to preterm birth in Mexico City. Environmental Health Perspectives 117:1587–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melendez E, Hinojosa J. 2017. Estimates of post-Hurricane Maria exodus from Puerto Rico. Report: Hunter College, The City University of New York. [Google Scholar]
- Milken Institute School of Public Health. 2018. Ascertainment of the estimated excess mortality from Hurricane Maria in Puerto Rico. Milken Institute School of Public Health, The George Washington University, University of Puerto Rico Graduate School of Public Health [Google Scholar]
- Milman O 2018. Another Flint? Why Puerto Ricans no longer trust water after the hurricane. The Guardian. August 8. [Google Scholar]
- National Institute of Environmental Health Sciences (NIEHS). NIH disaster research response (DR2) - research protocols. Available: https://dr2.nlm.nih.gov/protocols [accessed March 1, 2019].
- Nkansah-Amankra S, Luchok KJ, Hussey JR, Watkins K, Liu X. 2010. Effects of maternal stress on low birth weight and preterm birth outcomes across neighborhoods of South Carolina, 2000–2003. Matern Child Health J 14:215–226. [DOI] [PubMed] [Google Scholar]
- Nobili V, Alisi A, Panera N, Agostoni C. 2008. Low birth weight and catch-up-growth associated with metabolic syndrome: A ten year systematic review. Pediatr Endocrinol Rev 6:241–247. [PubMed] [Google Scholar]
- Oni O, Harville E, Xiong X, Buekens P. 2015. Relationships among stress coping styles and pregnancy complications among women exposed to Hurricane Katrina. J Obstet Gynecol Neonatal Nurs 44:256–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padilla I, Irizarry C, Steele K. 2011. Historical contamination of groundwater resources in the north coast karst aquifers of Puerto Rico. Revista Dimension 3:7–12. [PMC free article] [PubMed] [Google Scholar]
- Pasch RJ, Penny AB, Berg R. 2018. NOAA National Hurricane Center tropical cyclone report: Hurricane Maria.
- Radke EG, Braun JM, Meeker JD, Cooper GS. 2018. Phthalate exposure and male reproductive outcomes: A systematic review of the human epidemiological evidence. Environ Int 121:764–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radke EG, Galizia A, Thayer KA, Cooper GS. 2019a. Phthalate exposure and metabolic effects: A systematic review of the human epidemiological evidence. Environ Int 132:104768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radke EG, Glenn BS, Braun JM, Cooper GS. 2019b. Phthalate exposure and female reproductive and developmental outcomes: A systematic review of the human epidemiological evidence. Environ Int 130:104580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramphal L 2018. Medical and psychosocial needs of the Puerto Rican people after Hurricane Maria. Proc (Bayl Univ Med Cent) 31:294–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy-Matton N, Moutquin JM, Brown C, Carrier N, Bell L. 2011. The impact of perceived maternal stress and other psychosocial risk factors on pregnancy complications. J Obstet Gynaecol Can 33:344–352. [DOI] [PubMed] [Google Scholar]
- Sanchez R 2018. How Puerto Rico’s death toll climbed from 64 to 2,957 in Hurricane Maria. Available: https://www.cnn.com/2018/08/29/us/puerto-rico-growing-death-toll/index.html [accessed January 10 2019].
- Schmidt S, Voisin SL. 2018. Puerto Rico after Maria “Water is Everything”. The Washington Post. [Google Scholar]
- Shapiro GD, Fraser WD, Frasch MG, Seguin JR. 2013. Psychosocial stress in pregnancy and preterm birth: Associations and mechanisms. J Perinat Med 41:631–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva MJ, Slakman AR, Reidy JA, Preau JL Jr., Herbert AR, Samandar E, et al. 2004. Analysis of human urine for fifteen phthalate metabolites using automated solid-phase extraction. J Chromatogr B Analyt Technol Biomed Life Sci 805:161–167. [DOI] [PubMed] [Google Scholar]
- Silva MJ, Wong LY, Samandar E, Preau JL Jr., Jia LT, Calafat AM. 2018. Exposure to di-2-ethylhexyl terephthalate in the U.S. general population from the 2015–2016 National Health and Nutrition Examination Survey. Environ Int 123:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotomayor O 2013. Fetal and infant origins of diabetes and ill health: Evidence from Puerto Rico’s 1928 and 1932 hurricanes. Econ Hum Biol 11:281–293. [DOI] [PubMed] [Google Scholar]
- Tong VT, Zotti ME, Hsia J. 2011. Impact of the Red River catastrophic flood on women giving birth in North Dakota, 1994–2000. Matern Child Health J 15:281–288. [DOI] [PubMed] [Google Scholar]
- Torche F 2011. The effect of maternal stress on birth outcomes: Exploiting a natural experiment. Demography 48:1473–1491. [DOI] [PubMed] [Google Scholar]
- Vernberg EM, Silverman WK, La Greca AM, Prinstein MJ. 1996. Prediction of posttraumatic stress symptoms in children after Hurricane Andrew. J Abnorm Psychol 105:237–248. [DOI] [PubMed] [Google Scholar]
- Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. 2008. Exposure to Hurricane Katrina, post-traumatic stress disorder and birth outcomes. Am J Med Sci 336:111–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. 2010. Hurricane Katrina experience and the risk of post-traumatic stress disorder and depression among pregnant women. Am J Disaster Med 5:181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahran S, Snodgrass JG, Peek L, Weiler S. 2010. Maternal hurricane exposure and fetal distress risk. Risk Anal 30:1590–1601. [DOI] [PubMed] [Google Scholar]
- Zahran S, Breunig IM, Link BG, Snodgrass JG, Weiler S, Mielke HW. 2014. Maternal exposure to hurricane destruction and fetal mortality. J Epidemiol Community Health 68:760–766. [DOI] [PubMed] [Google Scholar]
- Zota AR, Calafat AM, Woodruff TJ. 2014. Temporal trends in phthalate exposures: Findings from the National Health and Nutrition Examination Survey, 2001–2010. Environ Health Perspect 122:235–241. [DOI] [PMC free article] [PubMed] [Google Scholar]


