Abstract
Non-communicable diseases like hypertension are increasingly common among individuals living with HIV in low-resource settings. The prevalence of hypertension among people with HIV in Malawi, e.g. has been estimated to be as high as 46%. However, few qualitative studies have explored the patient experience with comorbid chronic disease. Our study aimed to address this gap by using the health belief model (HBM) to examine how comparative perceptions of illness and treatment among participants with both HIV and hypertension may affect medication adherence behaviours. We conducted semi-structured interviews with 75 adults with HIV and hypertension at an urban clinic in Lilongwe, Malawi. Questions addressed participants’ experiences with antiretroviral and antihypertensive medications, as well as their perspectives on HIV and hypertension as illnesses. Interviews were performed in Chichewa, transcribed, translated into English and analysed using ATLAS.ti. Deductive codes were drawn from the HBM and interview guide, with inductive codes added as they emerged from the data. Self-reported medication adherence was much poorer for hypertension than HIV, but participants saw hypertension as a disease at least as concerning as HIV—primarily due to the perceived severity of hypertension’s consequences and participants’ limited ability to anticipate them compared with HIV. Differences in medication adherence were attributed to the high costs of antihypertensive medications relative to the free availability of antiretroviral therapy, with other factors like lifestyle changes and self-efficacy also influencing adherence practices. These findings demonstrate how participants draw on past experiences with HIV to make sense of hypertension in the present, and suggest that although patients are motivated to control their hypertension, they face individual- and system-level obstacles in adhering to treatment. Thus, health policies and systems seeking to provide integrated care for HIV and hypertension should be attentive to the complex illness experiences of individuals living with these diseases.
Keywords: Adherence, non-communicable disease, HIV, qualitative research, perceptions, health behaviour, access, social determinants
Key Messages
Adherence to medication is much poorer for hypertension than for HIV.
Hypertension is an illness perceived as severely as HIV, if not more so.
Medication cost is seen as the main barrier to hypertension control.
Experiences with HIV care shape perceptions and expectations of hypertension care.
Introduction
Through concerted, sustained efforts to extend antiretroviral therapy (ART) coverage to communities across the world, people with HIV are now living much longer (Smit et al., 2015; Wang et al., 2016). This aging population faces new challenges, including a global non-communicable disease (NCD) crisis (Beaglehole et al., 2011; Bennett et al., 2018). NCDs are the largest cause of mortality in the world (World Health Organization, 2017), and they exert particular burden on low- and middle- income countries where healthcare systems are already stretched by HIV and other infectious diseases (Levitt et al., 2011). More than 85% of all ‘premature’ NCD-related deaths occur in low- and middle-income countries (World Health Organization, 2017).
International donor structures have not historically prioritized funding for preventing or managing NCDs (Nugent and Feigl, 2010). Donor investment in HIV has increased coverage of ART and provided funds for health system strengthening (Moucheraud et al., 2016), but there is debate about whether, and to what extent, these investments can improve care for other health issues like NCDs (Wroe et al., 2015; Patel et al., 2018a).
In Malawi, the burden of hypertension among the general adult population is estimated to be 33% according to a World Health Organization household survey (Ministry of Health Malawi World Health Organization, 2010; Msyamboza et al., 2011); the adult (ages 15–64) HIV prevalence is 10.6% (Patel et al., 2018b). Among adults with HIV in Malawi, studies have found hypertension prevalence rates of 24% to as high as 46% (Muronya et al., 2011; Divala et al., 2016). The Malawian Ministry of Health formally added the screening and treatment of NCDs to its Essential Health Package in 2011 (Ministry of Health Malawi, 2011), displaying governmental commitment to addressing NCDs, but how these services will be implemented and scaled remains unclear (Pfaff et al., 2017; Moucheraud, 2018; Patel et al., 2018b).
As the burden of NCDs raises questions about health system capacity to deliver high-quality primary care (Samb et al., 2010; Levitt et al., 2011; Atun et al., 2013; Kane et al., 2017), it has also called attention to the need for better understanding of patient experiences with chronic disease, particularly how individuals cope with multiple morbidities and barriers that may affect treatment adherence and retention in care (Monroe et al., 2013). Although a robust body of research explores the determinants of ART adherence (Watt et al., 2009; Heestermans et al., 2016; De Kok et al., 2018), few published studies have investigated factors affecting adherence to NCD medications for people in low-income countries, and even fewer have explored the unique challenges that may exist for people living with both NCDs and HIV (Ameh et al., 2017; Stockton et al., 2018; Venables et al., 2016; Zimmermann et al., 2018).
As such, better recognition of the personal, interpersonal and structural factors affecting NCD adherence in people living with HIV may unveil new opportunities for improving care delivery and improving clinical outcomes (Boyer et al., 2011; Wang et al., 2015; Kahana et al., 2016). We sought to identify and explore factors influencing adherence among individuals with HIV and hypertension in Malawi. In providing a more nuanced recognition of the forces influencing adherence to HIV and hypertension, the findings of this study may help inform future interventions and policies that seek to address the dual burden of chronic disease and improve outcomes for patients and communities in low-income settings.
Theoretical framework
The health belief model (HBM) is a prominent theoretical framework to understand how illness perception, the patient context and the environment affect health behaviours such as treatment adherence. The HBM posits six determinants of health behaviours (Janz and Becker, 1984):
Perceived susceptibility to disease: one’s opinion on the likelihood of contracting a given disease.
Perceived severity of disease: one’s opinion of how seriously a disease and its consequences will physically, mentally and socially affect one’s life.
Perceived benefits to action: one’s belief in the efficacy of an advised treatment or action to reduce the risk or seriousness of impact of a disease.
Perceived barriers to action: one’s perceptions of the physical and psychological costs of adhering to an advised treatment or action.
Cues to action: strategies, events or structures that encourage someone to adhere to an advised treatment or action.
Perceived self-efficacy: one’s confidence in their ability to take advised actions for the disease.
Dimensions of the HBM have been widely applied to understanding HIV and ART behaviours, with perceptions of increased self-efficacy, susceptibility and benefits of treatment correlating with better adherence for individuals with HIV in Tanzania, Italy and the USA, (Rosenstock et al., 1994; De Paoli et al., 2004; Munro et al., 2007; Fumaz et al., 2008). Similar findings have been demonstrated for treatment adherence among people with hypertension in the UK and USA, and with diabetes in Ethiopia (Kirscht and Rosenstock, 1977; Harrison et al., 1992; Abraham and Sheeran, 2005; Ayele et al., 2012). However, explorations of the theory for people with coexisting HIV and NCD(s) are limited (Juma et al., 2018).
In this study, we utilize the HBM to explore how people’s perceptions of HIV and hypertension and their experiences with each disease’s respective treatments may influence their adherence behaviours. We hypothesized that individuals would perceive HIV as more severe than hypertension, due to the universality of messages about the risks of HIV and the importance of ART (particularly compared with the dearth of such messages for NCDs); and thus, would be more motivated to adhere to ART than to antihypertensive medications. In addition, we hypothesized that structural factors in Malawi (affecting medication availability and affordability) would facilitate better adherence to ART therapy than to antihypertensive therapy.
Methods
Study setting
Interviews were conducted at Partners in Hope Medical Center, an HIV treatment site in Lilongwe, Malawi, supported by the United States Agency for International Development (USAID)-President’s Emergency Plan for AIDS Relief (PEPFAR). With an active cohort of approximately 5000 adult patients, the HIV clinic provides free ART and HIV-related services (including consultations, counselling and testing, and medications for HIV and related illnesses) and consultation and treatment for common NCDs diseases including hypertension and diabetes. However, unlike ART, medications for NCDs are available only for purchase at the on-site pharmacy or patients can purchase the medication elsewhere or obtain certain medications free-of-charge from a number of public facilities in Malawi.
Eligibility and recruitment
Individuals were eligible to participate in this study if they were at least 18 years old, were diagnosed with both HIV and hypertension and had been prescribed ART for 1 year or longer and at least one antihypertensive medication for 1 year or longer. Participants were recruited from the ART clinic at the time they came for routine HIV care. Prospective participants were identified by research staff through referrals from clinical officers, and eligibility was confirmed via chart review. If eligible, patients were taken to a separate room by a member of the study team who explained the study and conducted the informed consent process. Participants were reimbursed with 1500 kwacha (∼2 USD) and refreshments for participation in the study.
Data collection
Data were collected between June and December 2017. A trained member of the research team conducted an individual, in depth, semi-structured interview in Chichewa with each participant. Interview duration ranged from 10 to 30 min, with the majority lasting between 15 and 20 min, and was audio-recorded with consent. Questions included the impact of hypertension on daily life, experiences in seeking and obtaining ART and antihypertensive medications, perceptions of HIV and hypertension as illnesses, and how participants prioritize their HIV care vs their hypertension care. There were both open- and close-ended questions. The interviewer also collected information on participants’ demographics and their self-reported adherence to ART and hypertension therapy.
Data analysis
Audio recordings of the interviews were transcribed and then translated into English by trained Malawian research staff at Partners in Hope. English-language transcriptions were coded and analysed by a first investigator (M.H.) using ATLAS.ti. Deductive codes were drawn from the interview guide and the HBM; a few inductive codes were added as they emerged from the data. Two investigators (M.H. and C.M.) independently coded a random sample of transcripts, and met to discuss key themes and to revise the codebook accordingly. M.H. then coded all transcripts using the finalized codebook. Findings were summarized per HBM construct, and responses about HIV and hypertension were compared and analysed within each construct. Count data were calculated only for questions that were asked of every participant.
Ethical review
Data were collected anonymously and all participants provided oral consent to participate. The research was approved by the authors’ institutional review boards.
Results
The results are structured to first describe the characteristics of the study participants, including their self-reported adherence patterns to hypertension medications and ART. Next, the main themes from participant interviews are presented along the six constructs of the HBM. Representative quotes are included to illustrate key findings within each theme.
Demographics
Demographics of the 75 participants are summarized in Table 1. Self-reported non-adherence (missing ≥1 dose per week) to antihypertensive medication(s) was more common than non-adherence to ART (77.3% vs 6.7%, respectively). The majority of participants (84%) had uncontrolled blood pressure at their most recent clinic visit (systolic >140 mmHg and/or diastolic >90 mmHg). Participants were either on one- or two-pill ART regimens, with most taking a once daily fixed-dose combination tablet of efavirenz, lamivudine and tenofovir disoproxil fumarate.
Table 1.
Participant characteristics (n = 75)
| Characteristic | |
|---|---|
| Female sex, n (%) | 48 (64.0) |
| Median age, years (SD) | 53 (10.1) |
| Uncontrolled blood pressurea (systolic >140 mmHg and/or diastolic >90 mmHg), n (%) | 63 (84.0) |
| Median number of hypertension medications (range) | 2 (1-4) |
| Median duration of hypertension treatment, years (SD) | 4 (7.7) |
| Missed ≥1 dose per week of ART therapy, n (%) | 5 (6.7) |
| Missed ≥1 dose per week of hypertension medication(s), n (%) | 58 (77.3) |
aSingle measurement from clinic visit at time of participant's enrollment.
Perceived susceptibility to HIV and hypertension
Participants expressed initial difficulty in accepting the diagnosis of hypertension given its asymptomatic presentation. When probed about what made them accept the diagnosis, they stated that seeing other people in their community who took medications for hypertension helped persuade them that it was a legitimate disease.
It was hard for me to accept that I have hypertension compared to what people were saying concerning hypertension … It did not affect any of my lifestyle, everything was okay … but with the counselling I received from the doctors, I accepted as I did with HIV, knowing that I was not the first one, because there are a lot of people who are taking both ART and hypertension drugs (Female, 38 years old).
Some participants also noted that they had seen community members suffering from complications, such as stroke (chilonda), which they perceived as related to hypertension.
[Hypertension] is a sickness we see taking more lives every day (Male, 39 years old).
Participants also discussed differences in risk factors for HIV compared with hypertension. Some participants viewed hypertension as a disease that is not directly contracted by ‘contact with infected blood’ but rather that ‘just comes’. The perceived lack of control around risk hypertension caused these participants to feel more susceptible to contracting hypertension than HIV.
HIV is transmitted, but [hypertension] is not … it just comes (Male, 56 years old).
Perceived severity of HIV and hypertension
All participants were asked to directly compare disease severity, and nearly half (45%) perceived hypertension as more severe than HIV; an additional 18% perceived the two diseases as equally severe. A common characterization of the diseases emerged that juxtaposed the experience of ‘dying instantly’ with hypertension against ‘being sick for a long time’ with HIV.
Hypertension can kill you tomorrow but HIV gives you time. Some diseases take life slowly while others take life instantly (Male, 61 years old).
The dangerous disease nowadays is blood pressure, because even sitting on this chair right now I can die. While HIV, you stay longer, you cannot die a sudden death. You have prolonged sickness for some days but not with high blood pressure (Female, 70 years old).
Although less common (reported by only 37% of participants), those who saw HIV as more dangerous than hypertension associated this with ART resistance and the fear associated with having an untreatable strain of HIV, as well as the sentiment that uncontrolled HIV can cause ‘many diseases’, such as tuberculosis, malaria and cancers.
[Without ART], I would have many different diseases, like malaria, diarrhea, cough … Yes, you can get sick from strange things (Female, 48 years old).
Some participants also stated that because HIV can only be controlled by medications whereas hypertension can be improved with non-pharmacologic measures, HIV must be the more serious disease.
HIV disease is very dangerous, because many people have died of the disease, though many people have died of BP [high blood pressure] too. But BP has so many controlling measures…with HIV the only control measure is the medicine. Staying without medicine you may die anytime (Male, 62 years old).
Perceived benefits of controlling HIV and hypertension
Most participants believed that ART effectively reduced the risks of HIV. They noted that ART was ‘life-giving’, making people physically stronger and preventing other communicable diseases. They also discussed specifically how it protects the immune system, and why it was important to take it every day in order to prevent viral resistance. Other than death, ART resistance was seen as the most feared consequence of not adhering to ART.
ART helps people to live. There are some people who think they are clever, they stop taking the drugs, but if you quit the ART you will die. You get sick and start regretting … you can get sick from strange things, and the diseases could be worsening until you lose focus and it reaches an extent that even if you take the drugs, your body doesn’t react (Female, 66 years old).
The perceived benefits of antihypertensive medications were reducing the negative ‘symptoms’ of hypertension (headaches, dizziness, body pains, and anger and irritability) and preventing the feared consequence of stroke. Participants also noted that these medications gave them more energy and strength, allowing them improved capacity to work and ‘feel at peace’.
I was not living well with my friends. I was always feeling angry. When I slept, I could feel headaches but now it has stopped. Now I am able to live and chat well with my friends because of the hypertension medicine (Male, 53 years old).
Some participants discussed their personal experiences recovering from HIV due to ART, which instilled faith in the efficacy of ART. There were also beliefs that despite taking antihypertensive medications, one might still suffer a stroke, whereas taking ART correctly is completely protective against HIV complications.
There is a way you can control hypertension. Not eating salty foods. But after you start taking ART, if you skip you begin to experience some problems. You can even die because the body immunity becomes weak. So I feel that between high blood pressure medication and ART, the ART medicine is better. You cannot skip ART (Female, 61 years old).
Perceived barriers to controlling HIV and hypertension
The majority of participants noted barriers related to the financial aspects of hypertension medications. Antihypertensive medications were perceived as too much to afford monthly, and if purchased, came at the expense of other household items.
When I have money I am able to buy my [hypertension medications] … It does affect my day to day. It might happen that the small money you had and wanted to use to buy relish, you have to stop and use it to buy medicine. That means the kids will suffer so it’s hard, there is some food you end up not getting … what else would one do? (Female, 64 years old).
The [hypertension] drugs are not hard to find, but the price is high, plus the transport to go where they sell them…it’s hard, because the money [with] which you are supposed to buy food, you end up buying drugs (Female, 39 years old).
In order to maintain their medication adherence, several participants mentioned that family members or friends would sometimes lend them money to pay for the drugs, but they expressed shame at having to ask that burden of their loved ones.
Sometimes it happens that you don’t have money, so most of the times the support comes from children … you eventually feel ashamed of begging from your children—each time you want [hypertension] medication you have to ask for money … I feel bad for him because he has a family to support. It doesn’t mean that if I ask him he would refuse, but I know he also has his family (Female, 39 years old).
When discussing the financial dimensions of hypertension adherence, participants contrasted them unfavourably to the ease with which they access HIV care, particularly free ART. Individuals expressed worry and anxiety in knowing that they had a health issue—hypertension—but were unable able to take action on it because of money.
Taking [hypertension] medicine is not a choice but a problem where I cannot find the medicine, while the ART, I have never been in a situation that I want to go get the drugs but find that there is no medicine at the hospital … all times they are there and are free (Male, 51 years old).
When you are buying the [hypertension] medicine, it depends on your financial status whether you may get the medicine or not. If we were getting the medicine for free, you can take the medicine like we do any other medicine. (Male, 35 years old).
Pill burden for managing both conditions was also mentioned as a challenge and a ‘tiresome’ experience.
The difference is that I am taking a lot of medicine while in the past I was only taking one tablet. Right now I am taking a lot of pills (Male, 53 years old).
Because I take medicine every day, it’s tiresome (Male, 52 years old).
Only one participant mentioned the side effects of hypertension medication as an impediment to adherence, which for him was frequent urination disrupting his sleep. No participants commented on negative side effects of ART.
Initiating the lifestyle changes associated with hypertension were another barrier that participants frequently highlighted as a source of stress. They voiced frustration at being told by healthcare providers to change lifestyle habits; e.g. to eat different meals from their families and poorly seasoned food.
Slowly I accepted it, but it was not easy to stop eating certain types of food. In that time I used to eat food that contained oil. It was a difficult situation and I was also worried because I started taking more medication every day (Female, 53 years old).
[The doctors’] perception is sort of controlling. The fact that the doctors told me what to do, and what not to do, like salt and not too much oily stuff … it was difficult at first (Male, 52 years old).
Perceived self-efficacy in controlling HIV and hypertension
When asked about the impact that hypertension had on their daily lives, many participants noted an initial period of adjustment with taking on a new medication regimen and implementing lifestyle changes. But over time, individuals commonly reported feeling more confident in their ability to make the necessary dietary changes—some participants even expressed excitement that, unlike HIV, hypertension was a disease that they could improve in ways other than medication.
Such things, like not eating food containing salt, oil and other things, they affected me when I was told to start taking the blood pressure drugs. It affected me and I got worried because of it, but I decided to adapt to the situation … having HIV and high blood pressure, it is an experience that you always think about, and get disappointed about, but you can see that we work every day. Doing things properly, [accepting] the situation, you definitely live a happy life (Female, 38 years old).
Some participants expressed low confidence, even futility, in their ability to consistently afford their hypertension medications and felt that there was ‘nothing you can do’ if your medications run out and you cannot buy more. Recurrent medication costs generated a sense of uncertainty that disrupted interviewees’ faith in their capacity to adhere.
Sometimes it happens that you don’t have money to buy the drugs … with time if you haven’t done any work, and the drugs are almost finished, you don’t know what to do (Female, 47 years old).
When I am taking the [hypertension] drugs accordingly, I feel well … it is hard, because the drugs are needed, but I have little money and the drugs are expensive. So it happens that I buy some drugs and haven’t bought others because the money is not enough, so you just buy 2 or 3 and you don’t buy the other, and live without taking them (Female, 59 years old).
Self-efficacy for one disease appeared to reinforce self-efficacy for the other. Several participants felt that their experience taking a daily medication (whether ART or antihypertensive medication) facilitated adherence to their new medication.
The hypertension [medications] are the first that I started taking and when I was given the medicine, I was told that I will be taking them for life, so I am used to taking the medicine on a daily basis. On the time I received the ARTs, I was also told that I will take them for life, so for me it was not a new thing because I already had the experience of taking the hypertension medication every day (Male, 51 years old).
Cues to action for controlling HIV and hypertension
As a whole, participants noted strong cues to action (strategies or supports that encourage someone to adhere to treatment) for ART that primarily stemmed from powerful, personal experiences with HIV. Drawing from either their own illness narratives or those of friends and family, many participants noted fears about getting sick like they ‘were before’ starting ART as their primary impetus to remain adherent.
Since I started taking [ART], I see I live a better life. That is why I try my best to take the medicine and why try to remember every day not to forget (Male, 58 years old).
My cousin … he stopped taking ART because he wanted to hide from his wife. After three months, when he started the drugs again they didn’t work, then later he died. So I get worried about not taking ART (Male, 67 years old).
‘Symptoms’ were the most consistent cue for hypertension. Participants attributed heart palpitations, headaches and fatigue to missed doses of antihypertensive medication.
If I don’t take [hypertension] drugs, my heart beat is faster, so when I have not taken the medicine I do feel that I have done wrong and I remember to take the medicine (Female, 55 years old).
With [hypertension] medicine … sometimes you forget because you can think about a lot of things … Unless I am feeling in my body that my blood pressure has gone very high … but if I am not feeling like that, it is very easy to forget to take medicine (Male, 61 years old).
Similarly, though to a lesser extent than HIV, participants also shared cautionary stories of friends impacted by hypertension as sources of motivation:
I have seen it back then from my parents … my father died of hypertension, and the younger brother of my father who stays in South Africa had a stroke because of [hypertension], so I don’t for a day miss the [hypertension] drugs (Male, 52 years old).
There were several practical strategies that participants recognized as facilitating adherence to both hypertension medications and ART. These included taking both types of medications at the same time, involving family members in their care and asking them for daily reminders, and having a shared ‘drug bag’ so that all the medications were in the same place in the home.
I actually tell the boys and guardians that I stay with that they should remind me. When they realize that I have forgotten, they say ‘Mother, you have forgotten your medications’. And you would see that they are bringing me a cup of water so that I take the pills (Female, 58 years old).
Taking blood pressure treatment is important …. With friends that I live with in the same house, I tell them to remind me when to take the treatment (Male, 42 years old).
Discussion
Our study suggests substantial differences in illness experience and adherence behaviours between HIV and hypertension among adults with comorbid disease in Malawi. Contrary to our initial hypothesis, hypertension was widely viewed as severe and dangerous—equally, if not more so, than HIV. Our findings echo a study conducted in Baltimore showing that adults with HIV and hypertension and/or diabetes reported greater fear about their comorbidities than HIV (Monroe et al., 2013). In our sample, the serious consequences of hypertension—stroke leading to death—in tandem with its unforeseeable disease course, contributed to perceived susceptibility and severity. In contrast, HIV was seen to cause a gradual, observable health decline—an AIDS-attributable death was viewed as something that could be anticipated and averted.
Participants demonstrated an accurate understanding of the value of treatment for both diseases. They provided clear, specific descriptions of the risks of HIV and the benefits of ART, and participants accurately recognized the consequences of hypertension and the dual pharmacological and lifestyle measures available to prevent them. Cues to action for both diseases were heavily informed by personal experiences with illness and treatment. Interestingly, though hypertension is typically an asymptomatic disease, participants attributed several physical manifestations to it that appeared to improve with their medications. Prior studies (Meyer et al., 1985; Monroe et al., 2013) have identified an association between beliefs in symptoms of hypertension and increased motivation to adhere to treatment and our sample reflects a similar relationship.
However, despite reporting high susceptibility to and severity of hypertension, and a number of cues to action, adherence to hypertension medications was markedly worse than ART. Out-of-pocket expenditures for medication, plus other costs for transportation or opportunity costs of lost wages, were the most common treatment barrier in this population. Partners in Hope is similar to many HIV clinics in Malawi in providing free HIV care but not free NCD medications (Malawi NCDI Poverty Commission, 2018). For this population, the strengthening of health systems for HIV care has not provided equivalent benefits for other chronic diseases—and participants observed this inconsistency, expressing frustration at having to pay for antihypertensive medications while receiving ART for free. Many studies have identified medicine cost as an essential determinant of successful uptake and adherence to treatment (Mojtabai and Olfson, 2003; Johnson et al., 2012; Wirtz et al., 2017), including for NCDs and hypertension specifically (Murphy et al., 2016; Attaei et al., 2017; van der Laan et al., 2017); and this barrier is likely to affect the poorest and most vulnerable populations. The success of HIV programmes speaks to the benefits of free healthcare, and lessons learned from HIV care can be applied to other chronic diseases. For example, infrastructure already developed for HIV services may be leveraged to provide NCD care with increased efficiency and reduced cost through integrated care models (Njuguna et al., 2018; Pastakia et al., 2018). In addition, given the significant role of foreign aid in Malawi’s health system—external donor funding comprises the majority of Malawi’s health expenditure (World Health Organization, 2019)—increased donor prioritization of NCDs may be another mechanism to offset medication costs and optimize care delivery for people with chronic comorbidities.
Individuals’ sense of self-efficacy around hypertension management, particularly around lifestyle changes, was complex and influenced by both their perceptions of disease severity and treatment barriers. Though the initial adjustment period was difficult, echoing findings from previous studies (Mellen et al., 2008; King et al., 2009), many participants were ultimately optimistic in making dietary and lifestyle changes. In a context where there is widespread anxiety around the dangers of hypertension and widespread reported difficulty in consistently affording hypertension medications, lifestyle and nutritional changes are a cheaper alternative to pharmacologic therapy that still allow participants to feel like they are doing ‘something’ to control their illness. Further research is needed, particularly in LMIC settings, to understand how participants’ openness to lifestyle interventions would change if medications were easily accessible, whether these individuals can actualize these lifestyle changes, and whether these changes can avert the need for medication. In addition, further education and counselling about feasible lifestyle and dietary modifications in the Malawian context, and about the appropriate role of medical treatment for hypertension, could improve overall adherence. NCD programmes might learn from successes in HIV health education of how to communicate complex clinical concepts that may improve adherence, particularly delivering simple messages via community sensitization, familial involvement and education campaigns. For example, the broad educational campaign ‘Know Your Viral Load’ in Malawi involved billboards, radio and other messaging platforms to raise awareness of viral load monitoring for people with HIV and the general population; an analogous campaign around ‘knowing your blood pressure’ could be implemented for hypertension.
This qualitative study also raises questions about how living in a context with high HIV prevalence may impact individuals’ perceptions of other diseases like NCDs. A systematic review assessing the overlap between HIV and type-2 diabetes in sub-Saharan Africa suggested that the legacy of HIV has led people to discuss and interpret the symptoms of type-2 diabetes in terms of their similarities to those of HIV (Zimmermann et al., 2018). Our findings indicate similar patterns around perceptions of hypertension—HIV may provide an initial framework through which individuals can approach and make sense of hypertension.
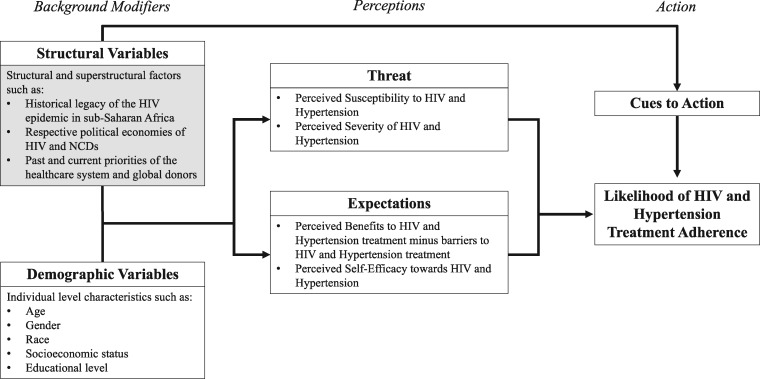
Although the HBM has been criticized for minimizing the influence of political and structural factors on health behaviour (Green and Murphy, 2014), this study suggests ways in which future research might work to augment the HBM and increase its utility in assessing these dimensions. We propose one such model (Figure 1), which elucidates how underlying structural forces beyond just the individual factors that the HBM traditionally encompasses may modify individuals’ perceptions of disease and treatment and shapes their cues to action (Champion and Skinner, 2008). For example, the sociopolitical context of widespread availability of ART in Malawi—over 70% of those living with HIV are on ART (UNAIDS, 2017)—affected our participants’ expectations about what appropriate treatment for chronic diseases should entail (e.g. free medications), and many interviewees drew cues to act on hypertension from their past direct and indirect experiences with the HIV epidemic. These relationships would not have necessarily been captured in previous iterations of the HBM. Such an expanded framework could enhance future research exploring the drivers of health behaviours, and help to inform the development of policies and programmes that can comprehensively address adherence issues given their deeper historical and social context.
Figure 1.
Proposed version of the HBM that includes structural factors (greyed box) that may influence health behaviours.
This study has limitations that should be noted. First, participants were recruited from only one health facility in Malawi. Future work should seek to collect data from more diverse sites and from more countries in order to increase generalizability. Second, in the context of low screening and treatment rates for NCDs in Malawi, individuals diagnosed and on treatment for hypertension are a unique subgroup within the population and their perceptions may not hold true across the population. According to the WHO household survey, 75% of adults with hypertension are undiagnosed, and only 24% of those diagnosed reported currently taking antihypertensive medications (Ministry of Health Malawi and World Health Organization, 2010). Future studies may seek to explore whether and how time since diagnosis, and which disease was diagnosed first, may affect patient experience and perceptions. Third, self-reported adherence is subject to social desirability bias; however, we hypothesize that the bias would be equivalent for both diseases and, therefore, should have minimal impact on the comparative results presented here between adherence to ART and hypertension medications. Fourth, clinicians were not recruited for interviews, and subsequent studies that elicit their experiences with treating HIV and hypertension would further inform other dimensions of comorbid illness. Lastly, the interview guide included only three very broad, open-ended questions about illness and treatment experiences. Future research should probe these areas more comprehensively using theory-informed interview guides; deductive research with high internal and external validity is important for addressing these research questions with rigour.
Despite these limitations, this study is one of the first qualitative reports from sub-Saharan Africa specifically assessing the illness, treatment and adherence experiences of individuals with HIV and NCD comorbidities. The high prevalence of hypertension among adults on ART in Malawi represents an urgent health need, and the suboptimal adherence to antihypertensive therapy we found among our participants poses opportunities for intervention. As the epidemiologic collision of HIV and NCDs in low-income settings unfolds, it is paramount that qualitative and quantitative research continues to explore patients’ experiences to help inform successful models of care that can address the range of health problems that individuals face over the life course.
Acknowledgements
We sincerely thank the participants and the staff at Partners in Hope for their support of this project, in particular, Khumbo Phiri and Kathryn Dovel. R.H. receives support from the UCLA Center for AIDS Research under grant AI028697 with support from the UCLA AIDS Institute. Partners in Hope receives support from the U.S. Agency for International Development (USAID) and the Presidents Emergency Plan for AIDS Relief (PEPFAR) under Cooperative Agreement [AID-OAA-A-15-00070]. C.M. receives support from the Center for HIV Identification, Prevention, and Treatment (CHIPTS) NIMH grant MH58107; the UCLA Center for AIDS Research (CFAR) grant 5P30AI028697; and the National Center for Advancing Translational Sciences through UCLA CTSI Grant UL1TR000124. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH. The research was approved by the Institutional Review Board at the University of California Los Angeles and the Malawi National Health Sciences Research Committee.
Conflict of interest statement. None declared.
Ethical approval. Data were collected anonymously and all participants provided oral consent to participate. The research was approved by the Institutional Review Board at the University of California Los Angeles and the Malawi National Health Sciences Research Committee.
Appendix
Semi-structured Interview Questions
Please describe any ways in which needing medications for blood pressure affects your quality of life.
Do you think that medication for HIV is more important, equally important, or less important than medication that you take for high blood pressure? Please tell me more about why you think this.
On an average day, do you think differently about your ART compared to your blood pressure medications?
References
- Abraham C, Sheeran P. 2005. The health belief model. Predicting Health Behaviour 2: 28–80. [Google Scholar]
- Ameh S, Klipstein-Grobusch K, D’ambruoso L et al. 2017. Quality of integrated chronic disease care in rural South Africa: user and provider perspectives. Health Policy and Planning 32: 257–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attaei MW, Khatib R, McKee M et al. 2017. Availability and affordability of blood pressure-lowering medicines and the effect on blood pressure control in high-income, middle-income, and low-income countries: an analysis of the PURE study data. The Lancet Public Health 2: e411–9. [DOI] [PubMed] [Google Scholar]
- Atun R, Jaffar S, Nishtar S et al. 2013. Improving responsiveness of health systems to non-communicable diseases. The Lancet 381: 690–7. [DOI] [PubMed] [Google Scholar]
- Ayele K, Tesfa B, Abebe L, Tilahun T, Girma E. 2012. Self care behavior among patients with diabetes in Harari, Eastern Ethiopia: the health belief model perspective. PLoS One 7: e35515.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaglehole R, Bonita R, Horton R et al. 2011. Priority actions for the non-communicable disease crisis. The Lancet 377: 1438–47. [DOI] [PubMed] [Google Scholar]
- Bennett JE, Stevens GA, Mathers CD et al. 2018. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. The Lancet 392: 1072–88. [DOI] [PubMed] [Google Scholar]
- Boyer S, Clerc I, Bonono C-R et al. 2011. Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: individual and healthcare supply-related factors. Social Science & Medicine 72: 1383–92. [DOI] [PubMed] [Google Scholar]
- Champion VL, Skinner CS. 2008. The health belief model. Health Behavior and Health Education: Theory, Research, and Practice 4: 45–65. [Google Scholar]
- De Kok B, Widdicombe S, Pilnick A, Laurier E. 2018. Doing patient-centredness versus achieving public health targets: a critical review of interactional dilemmas in ART adherence support. Social Science & Medicine 205: 17–25. [DOI] [PubMed] [Google Scholar]
- De Paoli MM, Manongi R, Klepp K-I. 2004. Factors influencing acceptability of voluntary counselling and HIV-testing among pregnant women in Northern Tanzania. AIDS Care 16: 411–25. [DOI] [PubMed] [Google Scholar]
- Divala OH, Amberbir A, Ismail Z et al. 2016. The burden of hypertension, diabetes mellitus, and cardiovascular risk factors among adult Malawians in HIV care: consequences for integrated services. BMC Public Health 16: 1243.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fumaz CR, Muñoz-Moreno JA, Moltó J et al. 2008. Sustained antiretroviral treatment adherence in survivors of the pre-HAART era: attitudes and beliefs. AIDS Care 20: 796–805. [DOI] [PubMed] [Google Scholar]
- Green EC, Murphy E. 2014. Health belief model. In: Cockerham WC (ed). The Wiley Blackwell Encyclopedia of Health, Illness, Behavior, and Society. Chichester, West Sussex: Wiley Blackwell, 766–9. [Google Scholar]
- Harrison JA, Mullen PD, Green LW. 1992. A meta-analysis of studies of the health belief model with adults. Health Education Research 7: 107–16. [DOI] [PubMed] [Google Scholar]
- Heestermans T, Browne JL, Aitken SC, Vervoort SC, Klipstein-Grobusch K. 2016. Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-Saharan Africa: a systematic review. BMJ Global Health 1: e000125.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janz NK, Becker MH. 1984. The health belief model: a decade later. Health Education Quarterly 11: 1–47. [DOI] [PubMed] [Google Scholar]
- Johnson A, Goss A, Beckerman J, Castro A. 2012. Hidden costs: the direct and indirect impact of user fees on access to malaria treatment and primary care in Mali. Social Science & Medicine 75: 1786–92. [DOI] [PubMed] [Google Scholar]
- Juma K, Reid M, Roy M et al. 2018. From HIV prevention to non-communicable disease health promotion efforts in sub-Saharan Africa: a narrative review. AIDS 32: S63–73. [DOI] [PubMed] [Google Scholar]
- Kahana SY, Jenkins RA, Bruce D et al. 2016. Structural determinants of antiretroviral therapy use, HIV care attendance, and viral suppression among adolescents and young adults living with HIV. PLoS One 11: e0151106.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane J, Landes M, Carroll C, Nolen A, Sodhi S. 2017. A systematic review of primary care models for non-communicable disease interventions in Sub-Saharan Africa. BMC Family Practice 18: 46.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DE, Mainous AG III, Carnemolla M, Everett CJ. 2009. Adherence to healthy lifestyle habits in US adults, 1988–2006. The American Journal of Medicine 122: 528–34. [DOI] [PubMed] [Google Scholar]
- Kirscht JP, Rosenstock IM. 1977. Patient adherence to antihypertensive medical regimens. Journal of Community Health 3: 115–24. [DOI] [PubMed] [Google Scholar]
- Levitt NS, Steyn K, Dave J, Bradshaw D. 2011. Chronic noncommunicable diseases and HIV-AIDS on a collision course: relevance for health care delivery, particularly in low-resource settings—insights from South Africa. The American Journal of Clinical Nutrition 94: 1690S–6S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malawi NCDI Poverty Commission. 2018. Malawi Noncommunicable Diseases & Injuries Poverty Commission Report. In: Health R.o.M.M.o. (Ed.). Malawi: Republic of Malawi Ministry of Health. [Google Scholar]
- Mellen PB, Gao SK, Vitolins MZ, Goff DC. 2008. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Archives of Internal Medicine 168: 308–14. [DOI] [PubMed] [Google Scholar]
- Meyer D, Leventhal H, Gutmann M. 1985. Common-sense models of illness: the example of hypertension. Health Psychology 4: 115.. [DOI] [PubMed] [Google Scholar]
- Ministry of Health Malawi. 2011. Malawi Health Sector Strategic Plan 2011–2016. Lilongwe: Republic of Malawi Ministry of Health. [Google Scholar]
- Ministry of Health Malawi, World Health Organization. 2010. Malawi National STEPS Survey for Chronic Non-Communicable Diseases and Their Risk Factors. Lilongwe: Republic of Malawi Ministry of Health. [Google Scholar]
- Mojtabai R, Olfson M. 2003. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Affairs 22: 220–9. [DOI] [PubMed] [Google Scholar]
- Monroe AK, Rowe TL, Moore RD, Chander G. 2013. Medication adherence in HIV-positive patients with diabetes or hypertension: a focus group study. BMC Health Services Research 13: 488.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moucheraud C. 2018. Service readiness for noncommunicable diseases was low in five countries in 2013–15. Health Affairs 37: 1321–30. [DOI] [PubMed] [Google Scholar]
- Moucheraud C, Sparkes S, Nakamura Y et al. 2016. PEPFAR investments in governance and health systems were one-fifth of countries’ budgeted funds, 2004–14. Health Affairs 35: 847–55. [DOI] [PubMed] [Google Scholar]
- Msyamboza KP, Ngwira B, Dzowela T et al. 2011. The burden of selected chronic non-communicable diseases and their risk factors in Malawi: nationwide STEPS survey. PLoS One 6: e20316.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro S, Lewin S, Swart T, Volmink J. 2007. A review of health behaviour theories: how useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS? BMC Public Health 7: 104.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muronya W, Sanga E, Talama G, Kumwenda JJ, van Oosterhout JJ. 2011. Cardiovascular risk factors in adult Malawians on long-term antiretroviral therapy. Transactions of the Royal Society of Tropical Medicine and Hygiene 105: 644–9. [DOI] [PubMed] [Google Scholar]
- Murphy A, Jakab M, McKee M, Richardson E. 2016. Persistent low adherence to hypertension treatment in Kyrgyzstan: how can we understand the role of drug affordability? Health Policy and Planning 31: 1384–90. [DOI] [PubMed] [Google Scholar]
- Njuguna B, Vorkoper S, Patel P et al. 2018. Models of integration of HIV and noncommunicable disease care in sub-Saharan Africa: lessons learned and evidence gaps. AIDS 32: S33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nugent R, Feigl AB. 2010. Where have all the donors gone? scarce donor funding for non-communicable diseases. CGD Working Paper 228. Washington, D.C.: Center for Global Development. http://www.cgdev.org/content/publications/detail/1424546. [Google Scholar]
- Pastakia SD, Tran DN, Manji I et al. 2018. Building reliable supply chains for noncommunicable disease commodities: lessons learned from HIV and evidence needs. AIDS 32: S55–61. [DOI] [PubMed] [Google Scholar]
- Patel P, Rose CE, Collins PY et al. 2018. Noncommunicable diseases among HIV-infected persons in low-income and middle-income countries: a systematic review and meta-analysis. AIDS 32: S5–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel P, Speight C, Maida A et al. 2018. Integrating HIV and hypertension management in low-resource settings: lessons from Malawi. PLoS Medicine 15: e1002523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaff C, Scott V, Hoffman R, Mwagomba B. 2017. You can treat my HIV—but can you treat my blood pressure? Availability of integrated HIV and non-communicable disease care in northern Malawi. African Journal of Primary Health Care & Family Medicine 9: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. 1994. The Health Belief Model and HIV Risk Behavior Change. Preventing AIDS. New York: Plenum Press, 5–24. [Google Scholar]
- Samb B, Desai N, Nishtar S et al. 2010. Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. The Lancet 376: 1785–97. [DOI] [PubMed] [Google Scholar]
- Smit M, Brinkman K, Geerlings S et al. 2015. Future challenges for clinical care of an ageing population infected with HIV: a modelling study. The Lancet Infectious Diseases 15: 810–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockton MA, Giger K, Nyblade L. 2018. A scoping review of the role of HIV-related stigma and discrimination in noncommunicable disease care. PLoS One 13: e0199602.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. 2017. Ending AIDS: Progress towards the 90–90–90 targets. Global AIDS Update. Geneva: Joint United Nations Programme on HIV/AIDS. [Google Scholar]
- van der Laan D, Elders P, Boons C et al. 2017. Factors associated with antihypertensive medication non-adherence: a systematic review. Journal of Human Hypertension 31: 687.. [DOI] [PubMed] [Google Scholar]
- Venables E, Edwards JK, Baert S et al. 2016. “They just come, pick and go.” The acceptability of integrated medication adherence clubs for HIV and non communicable disease (NCD) patients in Kibera, Kenya. PLoS One 11: e0164634.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Wolock TM, Carter A et al. 2016. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: the Global Burden of Disease Study 2015. The Lancet HIV 3: e361–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, Brenner S, Leppert G et al. 2015. Health seeking behaviour and the related household out-of-pocket expenditure for chronic non-communicable diseases in rural Malawi. Health Policy and Planning 30: 242–52. [DOI] [PubMed] [Google Scholar]
- Watt MH, Maman S, Earp JA et al. 2009. “It’s all the time in my mind”: Facilitators of adherence to antiretroviral therapy in a Tanzanian setting. Social Science & Medicine 68: 1793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirtz VJ, Hogerzeil HV, Gray AL et al. 2017. Essential medicines for universal health coverage. Lancet (London, England) 389: 403–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. 2017. Non-Communicable Diseases Progress Monitor. Geneva: World Health Organization. [Google Scholar]
- World Health Organization. 2019. The Global Health Expenditure Database. Retrieved from https://apps.who.int/nha/database.
- Wroe EB, Kalanga N, Mailosi B et al. 2015. Leveraging HIV platforms to work toward comprehensive primary care in rural Malawi: the Integrated Chronic Care Clinic. Healthcare 3: 270–6. [DOI] [PubMed] [Google Scholar]
- Zimmermann M, Bunn C, Namadingo H, Gray CM, Lwanda J. 2018. Experiences of type 2 diabetes in sub-Saharan Africa: a scoping review. Global Health Research and Policy 3: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]