Abstract
Objectives
A meta-analysis examined family functioning and medical adherence in children and adolescents with chronic health conditions. Family functioning was evaluated at the level of the family unit, as well as parent–child interactions.
Methods
We conducted literature searches using PubMed, PsycINFO, SCOPUS, Web of Science, and Cochrane. After reviewing 764 articles, 62 studies met eligibility criteria. Pearson’s r correlations were the effect size of interest. We conducted both omnibus and domain-specific (e.g., family conflict, cohesion) meta-analyses. Meta-regressions examined whether relevant covariates related to the magnitude of the effect.
Results
The omnibus meta-analysis showed that family functioning was significantly related to medical adherence across a variety of pediatric chronic health conditions. Lower family conflict, greater family cohesion, greater family flexibility, more positive communication, and better family problem-solving were each associated with better adherence. There were no significant differences in the magnitude of the omnibus effect based on child age, measurement features (subjective vs. objective or bioassay adherence; family unit vs. parent–child interactions), or study quality.
Conclusions
Consistent with social–ecological frameworks, findings supported links between family functioning and medical adherence. This study highlights several limitations of the extant research, including absence of a guiding theoretical framework and several methodological weaknesses. We offer clinical and research recommendations for enhancing scientific understanding and promotion of adherence within the family context.
Keywords: adherence, family functioning, meta-analysis
Medical adherence is a necessary component of effective pediatric disease self-management but is exceptionally difficult to achieve. Medical adherence refers to the correspondence between a patient’s or caregiver’s behavior with medical provider prescription (Haynes, 1979) and involves a triadic partnership between patients, family members, and medical providers (De Civita & Dobkin, 2004). Across childhood diseases, patients and families are required to adhere to multifaceted and complex treatment regimens, involving routine administration of medications, regular clinic attendance, monitoring for symptoms, and other necessary lifestyle recommendations (e.g., dietary modifications, physical activity, and skin/wound care). Nonadherence remains a ubiquitous yet perplexing challenge across disease groups and regimens, with documented rates of nonadherence averaging at approximately 50% and even higher rates (up to 75%) observed among adolescents (Rapoff, 2009). Nonadherence can result in numerous poor outcomes, including poor disease control, preventable complications, poor health-related quality of life, increased health-care utilization, and health care spending >$300 billion across all nonadherent patients (McGrady & Hommel, 2016). Recognizing the role of family in addressing this complex pediatric behavioral health issue, research has examined relationships between family functioning and adherence, as well as intervened at the family level (Wysocki et al., 2007). To optimize such family-based intervention approaches, we sought to rigorously evaluate components of family functioning that correlate with pediatric medical adherence by conducting a meta-analytic review.
Family functioning refers to the structural and relational aspects of a family environment and encompasses several conceptual dimensions of family life (Alderfer et al., 2008; Herzer et al., 2010; Miller, Ryan, Keitner, Bishop, & Epstein, 2000; Moos & Moos, 1994; Olson, 2000). Assessment of family functioning may be at the family unit level (e.g., family environment), as well as at the dyadic level (e.g., parent–child interaction; Hayden et al., 1998; Palermo & Chambers, 2005), and includes components of healthy family functioning (e.g., clear communication, collaborative problem-solving) and poor family functioning (e.g., conflict, disorganization). For children with and without chronic health conditions, family functioning is dynamic over the course of development. Increased family conflict during early adolescence is normative, usually temporary, and plays an important role in negotiating family roles such as greater adolescent independence (Holmbeck, 1996; Smetana, Campione-Barr, & Metzger, 2006). For example, family conflict surrounding an adolescent’s nonadherence may promote developmentally appropriate realignments in the allocation of treatment responsibilities (i.e., parents become more involved and adherence improves). On the other hand, chronically high or unresolved levels of family conflict result in poorer medical adherence (Anderson et al., 2009; Butner et al., 2009; Psihogios & Holmbeck, 2013).
There are many ways in which family functioning is theoretically and empirically important to consider in relation to child adaptation to chronic illness, including adherence. Models of family functioning, including the McMaster Approach to Families (Miller et al., 2000) and the Circumplex Model of Marital and Family Systems (Olson, 2000), each propose specific components of family functioning that impact child adjustment, including conflict, cohesion, flexibility, communication, and problem-solving. Relatedly, social–ecological theories of family adaptation to chronic health conditions (e.g., the Pediatric Psychosocial Preventative Health Model; Kazak, 2006) and pediatric disease self-management (e.g., The Pediatric Self-Management Model; Modi et al., 2012) posit that managing a chronic illness while maneuvering broader developmental issues not only impacts the child with a chronic health condition but also affects individual members of the family (e.g., a parent or sibling) and the family as a whole. At the same time, family plays a reciprocal role in child adjustment, including a child’s adherence to the medical regimen and their development of self-management skills.
Across the many investigations evaluating family functioning and adherence, adherence appears to be maximized when there are low levels of family conflict (Hilliard, Mann, Peugh, & Hood, 2013; Hood et al., 2007; Stepansky, Roache, Holmbeck, & Schultz, 2010) and high levels of family cohesion (DeLambo, Ievers-Landis, Drotar, & Quittner, 2004), adaptive problem-solving (Modi, Guilfoyle, Mann, & Rausch, 2016; Wysocki et al., 2008), and positive communication (Iskander, Rohan, Pendley, Delamater, & Drotar, 2015; Loiselle, Rausch, & Modi, 2015). In pediatric populations, family functioning surrounding disease management is also important to consider, with evidence to suggest that family conflict regarding adherence behaviors accounts for substantial variance in adherence (Hood, Butler, Anderson, & Laffel, 2007). A supportive and collaborative family environment is also an important prerequisite for the development of other relevant self-management skills and beliefs, such as youth self-efficacy for disease management (Noser, Huffhines, Clements, & Patton, 2017). Nevertheless, further delineation of the family functioning components that most closely relate to adherence is strongly needed to maximize the effectiveness and efficiency of adherence interventions. For example, it is possible that some components of family functioning are critical for adherence, while others play a smaller role.
While various reviews summarized the impact of broad social support on adherence (e.g., practical and social support and family cohesion and conflict; DiMatteo, 2004), the efficacy of adherence interventions (Kahana, Drotar, & Frazier, 2008; Pai & McGrady, 2014), and the role of family functioning on general child adjustment (Leeman et al., 2016; Van Schoors et al., 2017), there are no known meta-analyses that summarize empirical evidence investigating associations between family functioning and pediatric medical adherence. Leeman and colleagues (2016) conducted a sub-analysis of family functioning and adherence, although their search was restricted to four generic measures of family functioning and yielded only four studies (all related to type 1 diabetes). They ultimately did not find significance, which may be owed to the narrow scope of their search and few studies included. Meta-analyses examining adherence interventions have confirmed the impact of behavioral and multicomponent interventions, many of which involve family-based approaches, on improving adherence (Kahana et al., 2008). Nonetheless, the essential family functioning components that most closely relate to nonadherence remain unknown (McGrady, Ryan, Brown, & Cushing, 2015). A Comprehensive Meta-Analysis (CMA) is needed to summarize and evaluate the current state of the research, with attention to a broad range of pediatric populations, family functioning components, levels of family assessment (family functioning as a unit vs. dyadic functioning), and multifaceted adherence demands.
Thus, guided by social–ecological theories and previous literature stressing the importance of examining family functioning in relation to adherence, the primary aim of this article was to conduct a meta-analysis and commentary on the current state of evidence related to family functioning and pediatric adherence across pediatric populations. Specifically, we sought to examine the magnitude of the overall effect of family functioning on adherence, as well as the strength of specific core family functioning components described by family functioning theoretical models: family conflict, cohesion, communication, flexibility, and problem-solving. In addition, we examined the relationships of various study characteristics and methods, such as child age, measurement approaches, and article quality, on effect sizes. This meta-analysis advances adherence science by comprehensively summarizing and examining relationships between family functioning and pediatric adherence across disease groups and methodological approaches.
Method
Literature Search and Inclusion Criteria
The first author (A. M. P.) conducted literature searches of the following databases: PubMed, PsycINFO, SCOPUS, Web of Science, and Cochrane. Search terms were (chronic disease* OR diabetes OR asthma OR cancer OR sickle cell disease OR transplant OR spina bifida OR cystic fibrosis OR obesity OR HIV or arthritis OR inflammatory bowel disease) AND (pediatric* OR child OR adolescent) AND (medical adherence) AND (family functioning* OR family conflict OR family cohesion OR family communication OR family flexibility OR family problem-solving). We conducted a parallel search to capture relationships between parent–child interaction and adherence (parent–child interaction* OR parent–child relationship quality OR parent–child conflict OR parent–child communication OR parent–child problem-solving). Our intention was to include any pediatric chronic condition or treatment (e.g., solid organ recipient) that requires adherence to one or more treatment demands. We specified several specific disease groups to increase the reach of our search. Selection of these disease search terms was informed by similar adherence meta-analyses/systematic reviews (Kahana et al., 2008; Pai & McGrady, 2014). We also screened reference lists of included articles and the online table of contents of the Journal of Pediatric Psychology, which contributed more articles than any other publication (approximately 30% articles). To ensure studies were peer-reviewed, gray literature, such as conference abstracts and dissertations, was not included (Schmucker et al., 2013).
Inclusion Criteria
Inclusion criteria were (1) focus on global family functioning of the unit or parent–child interaction, (2) assess adherence, (3) relate to any pediatric chronic health condition or treatment (e.g., solid organ recipient) that requires ongoing adherence to one or more treatment demands, and (4) provide empirical research with correlation coefficient(s) reported or provided to compare the magnitude of effect size(s) across studies. Exclusion criteria included: (1) focus on the individual (e.g., parenting style; parent or child adjustment), (2) age of the sample extended outside the scope of children and adolescents (i.e., an adult sample, defined by M age >18 years), (3) focus on acute disease (e.g., pneumonia) or routine preventative health behaviors (e.g., adherence to scheduled vaccinations), (4) literature reviews or summaries, consensus, and opinion papers, and (5) qualitative research. As no known meta-analyses examined associations between family functioning and medical adherence across pediatric chronic diseases, we did not restrict our search to a specific time frame.
Study Definitions
The primary outcome was adherence, defined as “the extent to which a person’s behavior coincides with medical or health advice” (Haynes, 1979, pp. 1, 2). Measures of adherence may be objective (electronic monitors, pill count, clinic attendance via chart review), subjective (self-, parent-, and provider-reported questionnaires, daily diary assessments, or semi-structured interviews), or bioassays (e.g., hemoglobin A1C; HbA1C or tacrolimus blood levels). Based on theoretical models of family functioning (Olson, 2000; Miller et al., 2000), we defined family conflict as disagreements, openly expressed anger or negativity, and relationship difficulties. Family cohesion included the emotional bond family members have with one another, including affective responsiveness, warmth, and relationship quality. We defined family communication by how information is exchanged within a family, including listening and speaking skills, reciprocity, and respect and regard. Family flexibility included how the family balances structure (e.g. clearly defined roles, rules, and organization) with adaptability (e.g., modifying roles when needed). Family problem-solving described a family’s ability to resolve problems that threaten the integrity or functioning of the family. Family functioning may have been assessed at the level of the family unit (e.g., family conflict) or parent–child interactions (e.g., parent–child conflict).
Study Selection
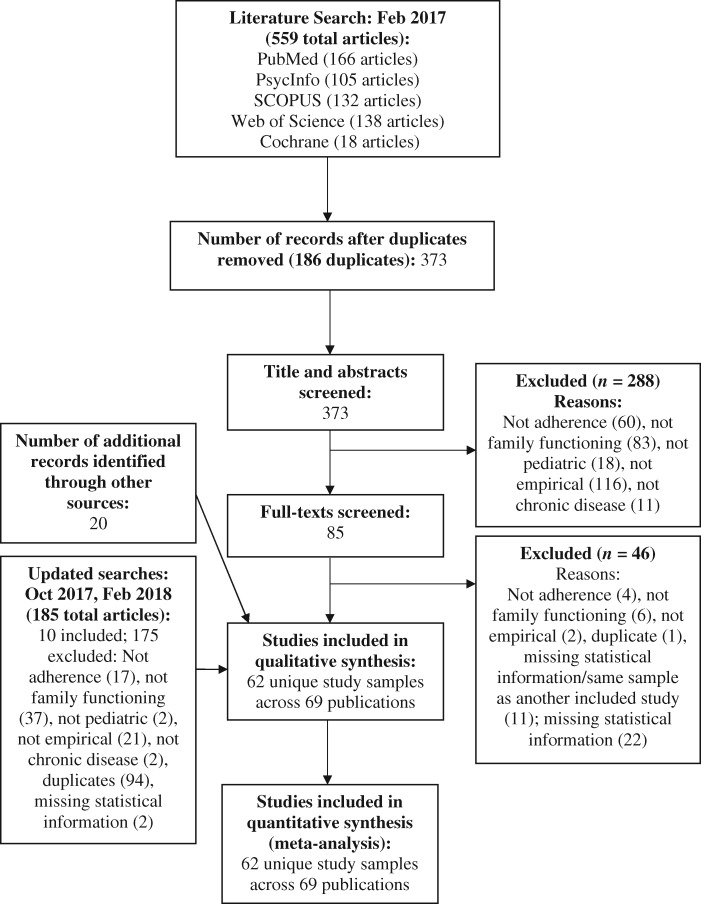
The original literature search (February 2017) yielded 559 total articles; 373 articles were unique papers (186 duplicates were removed; see Figure 1). The first author (A. M. P.) screened the 373 titles and abstracts and identified 85 potentially relevant abstracts for further review. Of the 85 full texts that were screened, 46 were subsequently excluded. The most common reason for exclusion was lacking necessary statistical information for inclusion in the meta-analysis (n = 38; i.e., missing bivariate correlation(s) for family functioning and medical adherence variables). Of the 38 studies that lacked necessary statistical information, 11 were already accounted for in the meta-analysis by papers that published on the same data set. We attempted to contact the remaining 27 authors to obtain necessary statistics. Total 5 author groups provided information, 6 authors indicated that they no longer had access to the relevant data, 11 did not respond, and valid contact information was unavailable for authors of the remaining 5 studies.
Figure 1.
PRISMA diagram.
In October 2017, we conducted an update of this procedure, yielding an additional 25 papers, and of those, 2 articles met eligibility criteria. In February 2018, we conducted a third update by expanding search terms to include parent–child interactions. Our parent–child interactions search yielded 160 articles, 8 of which met eligibility criteria. Screening references lists and the Journal of Pediatric Psychology online table of contents yielded an additional 20 articles. Thus, the final number of studies included in the meta-analysis was 62 studies across 69 publications (four data sets were published more than once; see Figure 1 for PRISMA diagram).
Data Extraction
The first and second authors conducted data extraction using a standardized template that summarized basic study information (e.g., year of publication, sample size and characteristics, and study design), theoretical framework (if provided), methodology (e.g., family functioning and adherence measures, including coding level of family assessment and objective/subjective adherence measures), statistical information (e.g., bivariate correlation(s) between family functioning and medical adherence; Ms, SDs, and reliability coefficients of family functioning and adherence variables), and the study abstract. The first author (A. M. P.) then checked for accuracy and completeness. We synthesized and described this information in Supplementary Table S1.
Quality Assessment
We adopted Alderfer et al. (2010) method for rating the scientific merit and potential bias of each included study. This system evaluates nine aspects of correlational studies on a three-point scale (1 = no or little evidence in fulfilling the criterion/low quality to 3 = good evidence/high quality): (1) explicit scientific context and purpose, (2) methodological design and analysis, (3) measurement reliability and statistical interpretation, (4) statistical power, (5) internal validity, (6) measurement validity and generalizability, (7) external validity, (8) appropriate discussion and limitations, and (9) contribution of knowledge (see Supplementary Table S1 for further information). The first and second author rated each article using these criteria. When ratings were >1 point apart, the raters convened and reached a consensus rating; this occurred once. As recommended by Alderfer and colleagues (2010), individual scores within each article, across both raters, were averaged to obtain an overall rating for each paper (see Supplementary Table S1). The average intraclass correlation coefficient was .84 across the two raters, demonstrating good interrater reliability.
Data Analyses
The statistical information extracted from each study or provided by authors was entered into CMA 3.0 statistical software. Pearson’s r values were transformed into Fisher’s Z correlations with calculation of the corresponding standard error from sample size for meta-analysis, and then (back) transformed to Pearson’s r for interpretation and creation of forest plots. When authors indicated nonsignificant findings but did not provide a bivariate correlation, r = 0 was used (Rosenthal, 1995). One study did not provide correlation coefficients but provided the sample size and p-values; thus, we estimated correlation coefficients based on the sample size and p-values. We standardized the sign of the correlation, so that a positive value indicated a positive association between family functioning (e.g., more cohesion, better problem-solving, and less conflict) and better adherence (e.g., higher self-reported adherence and lower HbA1C).
The first analysis took an omnibus approach to summarize statistical data across all domains of family functioning and medical adherence. We evaluated the Q statistic to determine the heterogeneity of the effect. If the Q statistic indicated significant random error, we used random-effects models to account for nonnormal distribution of effect sizes and methodology heterogeneity across studies. For fixed- and random-effects models, relative weights are assigned to each study based on sample size (Borenstein, Hedges, & Rothstein, 2007). For the omnibus meta-analysis, we averaged multiple effect sizes within studies (e.g., multiple measures of family functioning, multiple measures of adherence, and multiple reporters) and samples (e.g., multiple time points) for this analysis. When separate publications reported on the same data set, these publications were treated as dependent and combined. This technique is preferable to treating dependent findings as independent, which distorts standard error estimates (Hedges, Tipton, & Johnson, 2010; Olkin & Gleser, 2009). To assess and adjust for the possibility of publication bias, we created a funnel plot of the standard error and used the “trim and fill” algorithm (Duval & Tweedie, 2000). Using methods derived from symmetry assumptions, this approach estimates the number of missing studies and then imputes the missing values to estimate an overall adjusted effect. The second set of analyses involved subgroup meta-analyses to better estimate the size of the associations between specific family functioning components and adherence. Associations between relevant covariates (child age, subjective vs. objective or bioassay adherence: subjective as the reference group, family unit vs. parent–child family functioning assessment, and article quality) were examined via meta-regression analyses.
Results
Qualitative Synthesis
Sample Characteristics
For the 62 unique studies, we provided descriptive information regarding each study design, guiding theoretical model, sample, measures, and correlational findings in Supplementary Table S1. The cumulative sample size across the 62 studies was 6,427 participants. The average sample size was 104 (SD = 72, range = 13–338). There were nine unique disease groups, including asthma (n = 4 studies), cystic fibrosis (n = 5 studies), epilepsy (n = 2 studies), inflammatory bowel disease (n = 2 studies), juvenile rheumatoid arthritis (n = 1), sickle cell disease (n = 3 studies), spina bifida (n = 2 studies), solid organ transplantation (n = 4 studies), and type 1 diabetes (n = 38 studies). One study included two disease groups (type 1 diabetes and cystic fibrosis). The mean age of patients was 12 years (SD = 3, range = 1–15). Study design. In terms of the study design, 51 of the 62 studies were cross-sectional (82.3%) and the remaining 11 were longitudinal (17.7%). Twenty-seven studies described a theoretical model as guiding their research question (43.5%). Of note, across these studies, 29 different theoretical frameworks were cited. The most common theoretical frameworks were: (1) McMaster Model of Family Functioning (n = 3 studies; Epstein, Baldwin, & Bishop, 1983) and (2) Family Systems Theory (n = 3 studies; Minuchin, 1988).
Measurement
Regarding measurement of family functioning, 57 studies included a questionnaire measure of family functioning (91.9%), while 9 studies included an observational measure of family functioning (14.5%). The most commonly used questionnaires were the Diabetes Family Conflict Scale (Rubin, Young-Hyman, & Peyrot, 1989)/the Revised Diabetes Conflict Scale (n = 12 studies; Hood et al., 2007), followed by the Family Environment Scale (n = 9 studies; Moos & Moos, 1994) and the Family Adaptability and Cohesion Evaluation Scale (n = 8 studies; Gorall, Tiesel, & Olson, 2004). Nearly half of studies (45.2%) assessed family functioning at the parent–child interactions level, while 41.9% of studies assessed family functioning at the level of the family unit and 12.9% assessed family functioning at both levels. Most studies included only one measure of family functioning (71.0%). Of the 57 studies that included a questionnaire measure of family functioning, 57.9% included child- and parent-report (n = 33 studies), 22.8% included parent-report only (n = 13 studies), and 12.3% of studies included child-report only (n = 7). Four studies did not specify the informant (7.0%).
In terms of adherence measurement, 44 studies used a subjective measure of adherence (e.g., interview, daily diary, or questionnaire; 71.0%), 33 studies used a bioassay (e.g., HbA1C or tacrolimus blood levels; 53.2%), and 17 studies used an objective measure (e.g., electronic monitor, clinic attendance documented in the health record; 27.4%). Over half of the studies (54.8%) included a single measure of adherence. Of those that included a subjective measure of adherence, the majority assessed adherence using multiple informants (parent, patient, and/or medical provider; 61.4%, n = 27).
Quality Ratings
On average, the quality rating across studies fell in the “good” range. The mean quality rating was 2.39 (SD = 0.25), with ratings ranging from 1.83 to 2.83 on a three-point scale (1 = poor evidence/low quality, 3 = good evidence/high quality; Alderfer et al., 2010). Six of the studies fell below 2.0 (see Supplementary Table S1). The most common weaknesses were insufficient statistical power, threats to internal validity (e.g., risks for common method variance given single-informant, measuring predictor(s) and outcome(s) at the same time point), and threats to external validity (e.g., findings not generalizable to the target population).
Meta-Analysis: Overall Association Between Family Functioning and Adherence
Across the 62 studies, spanning 69 publications, there were 695 correlations of interest. Within the omnibus meta-analysis, we did not find significant heterogeneity beyond the sampling error, validating the use of the fixed-effects model, Q(61) = 58.83, p > .05. With the fixed-effects model, the point estimate of the correlation between family functioning and medical adherence was .18, with a 95% confidence interval (CI) [.15, .20]. The point estimate was significantly different from 0 (Z = 13.60, p < .00001), suggesting that the overall association of family functioning and adherence was significant. The trim and fill approach suggested that publication bias resulted in 20 missing effects, resulting in an adjusted point estimate of .13, 95% CI [.11, .15]. Meta-regression analyses indicated that there were not significant differences in the magnitude of the effect size depending on child age, Q(1) = .22, p > .05, level of family assessment (unit vs. parent–child; Q(1) = .03, p > .05, type of adherence assessment (subjective vs. objective or bioassay; Q(2) = 2.72, p > .05, or article quality, Q(1) = 1.46, p > .05.
Meta-Analysis: Components of Family Functioning
Family Conflict
Thirty-two studies evaluated family conflict (operationalized as conflict, negativity, negative reciprocity/communication, and relationship difficulties). The Q statistic did not indicate significant random error, Q (31) = 38.63, p > .05. With the fixed-effects model, the point estimate of the correlation between family functioning and medical adherence was −.18, with a 95% CI of −.21 to −.15 (see Supplementary Figure S1). The point estimate was significantly different from 0 (Z = −10.51, p < .00001), suggesting a significant negative association between family conflict and adherence. The trim and fill approach showed that three studies needed to be imputed to account for probable publication bias. The adjusted coefficient for the fixed-effects model was −.16, 95% CI [−.19, −.13]. There were no significant differences in the effect size based on child age, Q(1) = 1.41, p > .05, level of family assessment, Q(1) = 1.53, p > .05, type of adherence assessment, Q(2) = 3.78, p > .05, or article quality, Q(1) = .25, p > .05.
Family Cohesion
Twenty-eight studies evaluated family cohesion (operationalized as family cohesion, affective involvement/responsiveness, warmth/caring, emotional support, relatedness, and relationship quality). The Q statistic did not indicate significant random error, Q(27) = 28.41, p > .05. With the fixed-effects model, the point estimate of the correlation between family functioning and medical adherence was .18, with a 95% CI of .14 to .21 (see Supplementary Figure S2). The point estimate was significantly different from 0 (Z = 8.97, p < .00001), suggesting a significant positive association between family cohesion and adherence. Per the trim and fill approach, publication bias did not result in missing effects. Again, there were no significant differences in the magnitude of the effect size depending child age, Q(1) = 2.53, p > .05, level of family assessment, Q(1) = .92, p > .05, type of adherence assessment, Q(2) = 1.71, p > .05, or article quality, Q(1) = 1.23, p > .05.
Family Flexibility
Twelve studies evaluated aspects of family flexibility (operationalized as roles, organization, rules about behavior, and adaptability). The Q statistic did not indicate significant random error, Q(11) = 4.99, p > .05. With the fixed-effects model, the point estimate of the correlation between family functioning and medical adherence was .13, with a 95% CI of .07 to .19 (see Supplementary Figure S3), which was significantly different from 0 (Z = 4.03, p = .0001). That is, family flexibility positively related to adherence. Publication bias resulted in one missing effect, with the adjusted point estimate remaining .13, 95% CI [.07, .19]. The magnitude of the effect size did not depend on child age, Q(1) = .13, p > .05, level of family assessment, Q(1) = .13, p > .05, type of adherence assessment, Q(2) = 1.95, p > .05, or article quality, Q(1) = .12, p > .05. As all studies measured family flexibility at the family level, we were unable to test level of family assessment as a moderator.
Family Communication
Eleven studies evaluated aspects of family communication (operationalized as communication and positive reciprocity). The Q statistic did not indicate significant random error, Q(10) = 6.97, p > .05. With the fixed-effects model, the point estimate was .13, 95% CI [.08, .19], which was significantly different from 0 (Z = 4.58, p < .00001) and indicated a positive relationship between family communication and adherence (see Supplementary Figure S4). Publication bias resulted in one missing effect, with the adjusted point estimate remaining .13, 95% CI [.07, .18]. The magnitude of the effect size did not depend on child age, Q(1) = 3.48, p = .06, level of family assessment, Q(1) = .01, p > .05, type of adherence assessment, Q(2) = .28, p > .05, or article quality, Q(1) = 1.94, p > .05.
Family Problem-Solving
Seven studies investigated family problem-solving and adherence. The Q statistic did not indicate significant random error, Q(6) = 5.94, p > .05. The point estimate for the fixed-effects model was .12, 95% CI [.04, .19], which was significant (Z = 2.90, p = .004). That is, better family problem-solving related to higher adherence (see Supplementary Figure S5). Publication bias resulted in one missing effect, with an adjusted point estimate of .09, 95% CI [.01, .16]. Meta-regression indicated that the size of the association was significantly related to child age, Q(1) = 3.96, p = .048. As child age increased, so did the magnitude of the effect, .03, 95% CI [.001, .07]. The magnitude of the effect size did not depend on level of family assessment, Q(1) = .22, p > .05, type of adherence assessment, Q(2) = .47, p > .05, or article quality, Q(1) = .17, p > .05.
Exploratory Analyses
As the effect size observed for family conflict and adherence was among the largest, we conducted exploratory meta-analyses to determine the magnitude of the effects for disease-related conflict (e.g., disease conflict surrounding diabetes management) and generic family conflict. Total 18 studies examined disease-related conflict, while 14 studies examined generic family conflict. For disease-related conflict, the point estimate for the fixed-effects model of disease-specific family conflict was −.21, 95% CI [−.25, −.17], which was significant (Z = −9.59, p < .00001). Publication bias resulted in four missing studies, with an adjusted point estimate of −.19, 95% CI [−.23, −.15]. For generic family conflict, the point estimate for the fixed-effects models of generic family conflict was −.13, 95% CI [−.18, −.07], which was also significant (Z = −4.72, p < .00001). The trim and fill approach showed no missing studies.
Discussion
This meta-analysis investigated associations between family functioning and medical adherence among pediatric patients with chronic health conditions. To our knowledge, this article represents the first meta-analysis to pool associations across disease groups and family functioning and adherence measurements. Tests were consistent in showing homogeneity of variance across studies, which supported our decision to include all pediatric disease groups and assessment methods. We analyzed 62 unique studies, across 69 publications, and found a significant overall effect of family functioning on adherence. Moreover, components of family functioning were significantly associated with adherence: lower family conflict, greater family cohesion, greater family flexibility, more positive communication, and adaptive family problem-solving each related to better adherence. The effect sizes of family cohesion and conflict were among the highest, falling between the small to moderate range, which may justify prioritization of these domains in psychosocial screening and family-based adherence interventions.
Across the omnibus and family functioning component meta-analyses, effect sizes were almost always consistent across child age, level of family assessment, type of adherence measure, and article quality, supporting the dependability of these findings across the developmental spectrum and methodological approaches. However, as child age increased, so did the correlation between family problem-solving and adherence. This may suggest that during adolescence, when patients are gaining increased responsibility for disease management and problem-solving new adherence-related challenges, interventions that target family problem-solving may be especially relevant. Nevertheless, effect sizes across analyses were generally small. Consistent with social–ecological models (e.g., the Pediatric Self-Management Model; Modi et al., 2012), this suggests that family functioning components are important but not the only factors to consider, when conceptualizing barriers and facilitators to adherence.
This meta-analysis is not without limitations. The studies included in the meta-analysis were heterogeneous with regard to the specific family functioning and adherence constructs assessed, assessment approaches (e.g., informant type, measures), disease type, demographic characteristics (e.g., child age), and study design (e.g., cross-sectional and longitudinal). For example, across the studies included in the meta-analysis, average participant age ranged from infancy to age 15 years. While studies were heterogeneous in several ways, each explored similar self-management tasks such as medication adherence, following dietary recommendations, and monitoring for symptoms. Cross-disease approaches such as this meta-analysis are less common than disease-specific approaches but are valuable in highlighting the similar processes that bring about adaptive and maladaptive health behaviors across pediatric populations (Martire & Helgeson, 2017). It is also important to consider that we were underpowered to test disease type as covariate (with the exception of type 1 diabetes, individual disease groups were represented in few publications), making within disease meta-analyses of family functioning and pediatric adherence unfeasible at this point in time.
Another possible limitation was our integration of a variety of subjective, objective, and bioassay adherence measurements, each of which possess unique strengths and limitations and do not perfectly correspond (Hood, Peterson, Rohan, & Drotar, 2009; Simons et al., 2009). While subjective measures tend to overestimate adherence rates because of recall bias and social desirability, bioassays such as HbA1C and immunosuppressant blood levels may be influenced by medication and physiological factors independent of adherence (e.g., puberty, timing of the dose; Duncan, Mentrikoski, Wu, & Fredericks, 2014; Stirratt et al., 2015). For these reasons, HbA1C is sometimes characterized as an objective adherence assessment (Duncan et al., 2014; Hommel, Ramsey, Rich, & Ryan, 2017) and other times characterized as a diabetes outcome that is distinct from, but intricately connected to, adherence (Hood et al., 2009). Nonetheless, HbA1C is a commonly used clinical indicator of adherence in routine practice (Wu et al., 2013). Among pediatric solid organ transplant recipients, combining subjective and objective adherence measures had greater sensitivity and specificity for clinical outcomes than a single measure of adherence alone (Simons et al., 2009). We adopted a similar approach in this meta-analysis by integrating each adherence method in an effort to triangulate actual adherence among pediatric patients and their family members. Without weighting or prioritizing certain adherence measures, it is possible that this approach may have impacted findings. However, this appears unlikely, as there were no differences in the magnitude of the effect when we compared these measures.
Additionally, examining specific components of family functioning may not fully capture the family system as a whole. Incorporating family strengths and deficits to better understand distinct family typologies may portray a more accurate image of how families work together to influence child adjustment outcomes (Ghriwati, Winter, & Everhart, 2017; Mandara & Murray, 2002). Ghriwati and colleagues (2017) used pattern-based approaches to identify four profiles of family functioning that related to child adjustment outcomes among a large sample of children with asthma: cohesive, permissive, controlling/disengaged, and controlling/enmeshed. More research is needed to determine whether these profiles are generalizable across disease groups and whether they relate to adherence outcomes. Finally, our method of estimating r = 0 when statistical data were not provided was conservative and likely led to underestimation of associations. However, this method is preferable to disregarding null findings or incomplete reporting of results (Rosenthal, 1995).
Data from the current study highlight several limitations of the extant research, as well as areas for future research and clinical innovation. First, less than half of the included studies cited a theoretical model. Among those articles that cited a theoretical model, there was notable heterogeneity (i.e., 29 different theoretical models reported across studies). These findings demonstrate the lack of a unifying theoretical framework for understanding how the family context, including family functioning, influences adherence to chronic illness demands over the course of childhood development. Existing pediatric social–ecological models, including the Pediatric Psychosocial Preventive Health Model (Kazak, 2006) and the Pediatric Self-Management Model (Modi et al., 2012), offer overarching frameworks for considering the complexities of managing a chronic illness within the family system while maneuvering broader developmental issues. To extend current models of pediatric disease management, we propose that a more detailed theoretical model of the nonmodifiable and modifiable family factors that relate to adherence is strongly needed (i.e., a model that “magnifies” the family context and highlights priorities for screening and intervention across the developmental continuum). As a starting point, the results from this meta-analysis suggest that family conflict and cohesion may be the most robust family functioning correlates with pediatric adherence.
Second, attention needs to be paid to the conceptualization and measurement of family functioning constructs in relation to adherence. Most of the studies included in the meta-analysis relied on a single family functioning questionnaire, some of which have demonstrated low internal consistency in pediatric populations (Alderfer et al., 2008). Additionally, with the exception of diabetes-related conflict, family functioning surrounding disease management remains largely untested in the literature. It is possible that generic measures of family functioning do not completely assess the family functioning processes that are necessary for adherence (e.g., problem-solving surrounding adherence tasks and clear communication of disease information). Randomized controlled trials that compare overall and disease-specific family functioning interventions are needed to determine whether targeting family functioning as whole or family functioning surrounding disease management is equally effective. Alternatively, it is possible that general family functioning and disease-related family functioning each account for unique variance in adherence patterns, which is consistent with the findings of relatively equivalent effect sizes for disease-related and generic family conflict with adherence.
Very few studies used observational measures of family functioning. While observational research can be time-consuming and labor-intensive, direct observation offers several benefits. Using observational methods will allow researchers to directly assess more specific types of family interactions (e.g., family communication surrounding the allocation of treatment responsibilities), rather than rely solely on child and family perceptions of generic family functioning (Murphy, Murray, & Compas, 2017; Wysocki, 2015). Electronic methods of family observation, such as using an Electronically Activated Recorder, permit researchers to naturalistically assess multiple aspects of family relationships, as they unfold in everyday life, including during adherence tasks (Imami et al., 2015; Slatcher & Robles, 2012).
Third, studies included in the meta-analysis relied on objective, subjective, and bioassay measures of adherence, with almost half of the studies using more than one measure of adherence. However, of note, none of the included studies leveraged new technologies to assess adherence. Ecological momentary assessment (EMA) strategies involve signaling participants via an smartphone, typically multiple time each days, to report on current or recent behaviors, states, and conditions (Smyth & Stone, 2003; Stone & Shiffman, 2002). Assessing adherence via EMA reduces recall bias and allows for the measurement of real-world, real-time adherence behaviors, and the context in which those adherence behaviors occurred. For example, Mulvaney and colleagues (2013) found that EMA of asthma adherence correlated with asthma control and was feasible and acceptable among African-American teenagers.
Fourth, regarding study rigor, common weaknesses included insufficient statistical power, threats to internal validity from cross-sectional, single-informant data, and questionable generalizability of findings given predominantly white and middle-class samples. It is well established that family functioning and adherence behaviors change over the course of child development. Yet, there remains a dearth of longitudinal research investigating these dynamic processes. Rigorous longitudinal designs with diverse populations will expand our understanding of how dynamic family processes impact adherence across the developmental continuum.
Finally, it is significant that over half of the included studies focused on type 1 diabetes and often used a single disease-specific measure of family conflict. While the emphasis on type 1 diabetes and diabetes-related conflict is relevant given well-documented adherence issues (Anderson et al., 2002; Hilliard, Guilfoyle, Dolan, & Hood, 2011), this knowledge may or may not be generalizable to other disease groups who face unique challenges (e.g., neurocognitive difficulties or greater perceived life threat). Indeed, particular pediatric conditions, such as pediatric cancer and obesity, were entirely unrepresented in the meta-analysis. We recommend further research with these disease groups, as well as attention to socioeconomically diverse families who likely possess distinct family strengths and challenges in relation to adherence.
To summarize, this meta-analysis indicates that overall family functioning and specific family functioning components, including family conflict, cohesion, flexibility, communication, and problem-solving, are correlated with medical adherence across several pediatric chronic health conditions. Therefore, we recommend that consideration of the family as a whole, including routine assessment of family functioning and delivery of family-based self-management support, has implications for adherence promotion. In clinical settings, we encourage health-care professionals to screen for family conflict, cohesion, flexibility, communication, and problem-solving to identify family risk and protective factors for adherence. Given measurement limitations, there is a possible need for a new and updated questionnaire that assesses central family functioning components in relation to adherence. Screening for family functioning will enable opportunities to shift toward prevention and integration of family-based self-management support before adherence problems become significant and health deteriorates (Hommel, Ramsey, Rich, & Ryan, 2017).
Supplementary Data
Supplementary data can be found at: http://www.jpepsy.oxfordjournals.org/.
Funding
The writing of this article was supported by a Postdoctoral Fellowship from the American Cancer Society (PF-16-166-01-CPPB) to A.M.P.
Conflicts of interest: None declared.
Supplementary Material
References
- References marked with an asterisk indicate studies included in the meta-analysis. [Google Scholar]
- Alderfer M. A., Fiese B. H., Gold J. I., Cutuli J. J., Holmbeck G. N., Goldbeck L., Chambers C. T., Abad M., Spetter D., Patterson J. (2008). Evidence-based assessment in pediatric psychology: family measures. Journal of Pediatric Psychology, 33, 1046–1061; discussion 1062–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderfer M. A., Long K. A., Lown E. A., Marsland A. L., Ostrowski N. L., Hock J. M., Ewing L. J. (2010). Psychosocial adjustment of siblings of children with cancer: a systematic review. Psycho-Oncology, 19, 789–805. [DOI] [PubMed] [Google Scholar]
- *Anderson B. J., Holmbeck G., Iannotti R. J., McKay S. V., Lochrie A., Volkening L. K., Laffel L. (2009). Dyadic measures of the parent–child relationship during the transition to adolescence and glycemic control in children with type 1 diabetes. Families, Systems, and Health, 27, 141–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Anderson B. J, Vangsness L., Connell A., Butler D., Goebel-Fabbri A., Laffel L. M. (2002). Family conflict, adherence, and glycaemic control in youth with short duration type 1 diabetes. Diabetic Medicine, 19, 635–642. [DOI] [PubMed] [Google Scholar]
- *Barakat L. P., Smith-Whitley K., Ohene-Frempong K. (2002). Treatment adherence in children with sickle cell disease: disease-related risk and psychosocial resistance factors. Journal of Clinical Psychology in Medical Settings, 9, 201–209. [Google Scholar]
- *Berg C. A., Butler J. M., Osborn P., King G., Palmer D. L., Butner J., Murray M., Lindsay R., Donaldson D., Foster C., Swinyard M., Wiebe D. J. (2008). Role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care, 31, 678–683. [DOI] [PubMed] [Google Scholar]
- *Berg C. A., King P. S., Butler J. M., Pham P., Palmer D., Wiebe D. J. (2011). Parental involvement and adolescents’ diabetes management: the mediating role of self-efficacy and externalizing and internalizing behaviors. Journal of Pediatric Psychology, 36, 329–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M., Hedges L., Rothstein H. (2007). Meta-analysis: Fixed effect vs. random effects. Retrieved from https://www.meta-analysis.com/downloads/M-a_f_e_v_r_e_sv.pdf. Retrieved March 20, 2018. [Google Scholar]
- *Butner J., Berg C. A., Osborn P., Butler J. M., Godri C., Fortenberry K. T., Barach I., Le H., Wiebe D. J. (2009). Parent–adolescent discrepancies in adolescents’ competence and the balance of adolescent autonomy and adolescent and parent well-being in the context of Type 1 diabetes. Developmental Psychology, 45, 835–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Caccavale L. J., Weaver P., Chen R., Streisand R., Holmes C. S. (2015). Family density and SES related to diabetes management and glycemic control in adolescents with type 1 diabetes. Journal of Pediatric Psychology, 40, 500–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Celano M., Klinnert M. D., Holsey C. N., McQuaid E. L. (2011). Validity of the family asthma management system scale with an Urban African-American sample. Journal of Pediatric Psychology, 36, 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Chaney J. M., Peterson L. (1989). Family variables and disease management in juvenile rheumatoid arthritis. Journal of Pediatric Psychology, 14, 389–403. [DOI] [PubMed] [Google Scholar]
- *Chisholm V., Atkinson L., Bayrami L., Noyes K., Payne A., Kelnar C. (2014). An exploratory study of positive and incongruent communication in young children with type 1 diabetes and their mothers. Child: Care, Health and Development, 40, 85–94. [DOI] [PubMed] [Google Scholar]
- *Chisholm V., Atkinson L., Donaldson C., Noyes K., Payne A., Kelnar C. (2007). Predictors of treatment adherence in young children with type 1 diabetes. Journal of Advanced Nursing, 57, 482–493. [DOI] [PubMed] [Google Scholar]
- *Cousino M., Hazen R., MacLeish S., Gubitosi-Klug R., Cuttler L. (2013). Quality of life among youth with poorly controlled Type 1 diabetes: role of family conflict and sharing of treatment responsibility. Diabetes Management, 3, 449–457. [Google Scholar]
- *Dashiff C., Bartolucci A., Wallander J., Abdullatif H. (2005). The relationship of family structure, maternal employment, and family conflict with self-care adherence of adolescents with type 1 diabetes. Families, Systems, and Health, 23, 66–79. [Google Scholar]
- De Civita M., Dobkin P. (2004). Pediatric adherence as a multidimensional and dynamic construct, involving a triadic partnership. Journal of Pediatric Psychology, 29, 157–169. [DOI] [PubMed] [Google Scholar]
- *DeBoer M. D., Valdez R., Chernavvsky D. R., Grover M., Burt Solorzano C., Herbert K., Patek S. (2017). The impact of frequency and tone of parent–youth communication on type 1 diabetes management. Diabetes Therapy, 8: 625–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *DeLambo K. E., Ievers-Landis C. E., Drotar D., Quittner A. L. (2004). Association of observed family relationship quality and problem-solving skills with treatment adherence in older children and adolescents with cystic fibrosis. Journal of Pediatric Psychology, 29, 343–353. [DOI] [PubMed] [Google Scholar]
- DiMatteo M. R. (2004). Social support and patient adherence to medical treatment: a meta-analysis. Health Psychology, 23, 207–218. [DOI] [PubMed] [Google Scholar]
- *Drew L. M., Berg C., Wiebe D. J. (2010). The mediating role of extreme peer orientation in the relationships between adolescent–parent relationship and diabetes management. Journal of Family Psychology, 24, 299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Drotar D., Ittenbach R., Rohan J. M., Gupta R., Pendley J. S., Delamater A. (2013). Diabetes management and glycemic control in youth with type 1 diabetes: test of a predictive model. Journal of Behavioral Medicine, 36, 234–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Duke D. C., Geffken G. R., Lewin A. B., Williams L. B., Storch E. A., Silverstein J. H. (2008). Glycemic control in youth with type 1 diabetes: family predictors and mediators. Journal of Pediatric Psychology, 33, 719–727. [DOI] [PubMed] [Google Scholar]
- Duncan C. L., Mentrikoski J. M., Wu Y. P., Fredericks E. M. (2014). Practice-based approach to assessing and treating non-adherence in pediatric regimens. Clinical Practice in Pediatric Psychology, 2, 322–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S., Tweedie R. (2000). Trim and fill: a simple funnel‐plot–based method of testing and adjusting for publication bias in meta‐analysis. Biometrics, 56, 455–463. [DOI] [PubMed] [Google Scholar]
- Epstein N. B., Baldwin L. M., Bishop D. S. (1983). The McMaster family assessment device. Journal of Marital and Family Therapy, 9, 171–180. [Google Scholar]
- *Foulkes L.-M., Boggs S. R., Fennell R. S., Skibinski K. (1993). Social support, family variables, and complicance in renal transplant children. Pediatric Nephrology, 7, 185–188. [DOI] [PubMed] [Google Scholar]
- *Fredericks E. M., Lopez M., Magee J. C., Shieck V., Opipari-Arrigan L. (2007). Psychological functioning, nonadherence and health outcomes after pediatric liver transplantation. American Journal of Transplantation, 7, 1974–1983. [DOI] [PubMed] [Google Scholar]
- *Fredericks E. M., Magee J. C., Opipari-Arrigan L., Shieck V., Well A., Lopez M. J. (2008). Adherence and health-related quality of life in adolescent liver transplant recipients. Pediatric Transplantation, 12, 289–299. [DOI] [PubMed] [Google Scholar]
- *Friedrich E., Jawad A. F., Miller V. A. (2016). Correlates of problem resolution during parent-child discussions about chronic illness management. Children's Health Care, 45, 323–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Geffken G. R., Lehmkuhl H., Walker K. N., Storch E. A., Heidgerken A. D., Lewin A., Williams L. B., Silverstein J. (2008). Family functioning processes and diabetic ketoacidosis in youths with type I diabetes. Rehabilitation Psychology, 53, 231–237. [Google Scholar]
- *Gerson A., Furth S., Neu A., Fivush B. (2004). Assessing associations between medication adherence and potentially modifiable psychosocial variables in pediatric kidney transplant recipients and their families. Pediatric Transplantation, 8, 543–550. [DOI] [PubMed] [Google Scholar]
- *Ghriwati N. A., Winter M. A., Everhart R. S. (2017). Examining profiles of family functioning in pediatric asthma: longitudinal associations with child adjustment and asthma severity. Journal of Pediatric Psychology, 42, 434–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorall D., Tiesel J., Olson D. (2004). FACES IV: Development and validation. Minneapolis, MN: Life Innovations. [Google Scholar]
- *Gray W. N., Dolan L. M., Hood K. K. (2013). Impact of blood glucose monitoring affect on family conflict and glycemic control in adolescents with type 1 diabetes. Diabetes Research and Clinical Practice, 99, 130–135. [DOI] [PubMed] [Google Scholar]
- *Gumidyala A. P., Greenley R. N. (2014). Correlates of health-related quality of life in pediatric inflammatory bowel disease: a cumulative risk model approach. Journal of Pediatric Psychology, 39, 55–64. [DOI] [PubMed] [Google Scholar]
- *Hanson C. L., De Guire M. J., Schinkel A. M., Kolterman O. G. (1995). Empirical validation for a family-centered model of care. Diabetes Care, 18, 1347–1356. [DOI] [PubMed] [Google Scholar]
- Hayden L. C., Schiller M., Dickstein S., Seifer R., Sameroff S., Miller I., Keitner G., Rasmussen S. (1998). Levels of family assessment: I. Family, marital, and parent–child interaction. Journal of Family Psychology, 12, 7–22. [Google Scholar]
- Haynes R. B. (1979). Introduction. In Haynes R. B., Taylor D. W., Sackett D. L. (Eds.), Compliance in health care (pp. 1–7). Baltimore, MD: Johns Hopkins University Press. [Google Scholar]
- Hedges L. V., Tipton E., Johnson M. C. (2010). Robust variance estimation in meta‐regression with dependent effect size estimates. Research Synthesis Methods, 1, 39–65. [DOI] [PubMed] [Google Scholar]
- *Herge W. M., Streisand R., Chen R., Holmes C., Kumar A., Mackey E. R. (2012). Family and youth factors associated with health beliefs and health outcomes in youth with type 1 diabetes. Journal of Pediatric Psychology, 37(9), 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzer M., Godiwala N., Hommel K. A., Driscoll K., Mitchell M., Crosby L. E., Piazza-Waggoner C., Zeller M. H., Modi A. C. (2010). Family functioning in the context of pediatric chronic conditions. Journal of Developmental and Behavioral Pediatrics, 31, 26.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Herzer M., Vesco A., Ingerski L. M., Dolan L. M., Hood K. K. (2011). Explaining the family conflict-glycemic control link through psychological variables in adolescents with type 1 diabetes. Journal of Behavioral Medicine, 34, 268–274. [DOI] [PubMed] [Google Scholar]
- *Hilliard M. E., Guilfoyle S. M., Dolan L. M., Hood K. K. (2011). Prediction of adolescents' glycemic control 1 year after diabetes-specific family conflict: the mediating role of blood glucose monitoring adherence. Archives of Pediatrics and Adolescent Medicine, 165, 624–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hilliard M. E., Holmes C. S., Chen R., Maher K., Robinson E., Streisand R. (2013). Disentangling the roles of parental monitoring and family conflict in adolescents' management of type 1 diabetes. Health Psychology, 32(4), 388–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hilliard M. E., Mann K. A., Peugh J. L., Hood K. K. (2013). How poorer quality of life in adolescence predicts subsequent type 1 diabetes management and control. Patient Education and Counseling, 91, 120–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck G. N. (1996). A model of family relational transformations during the transition to adolescence: parent–adolescent conflict and adaptation. In Graber J., Brooks-Funn J., Petersen A. (Eds.), Transitions through adolescence: Interpersonal domains and context. New Jersey: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Hommel K. A., Ramsey R. R., Rich K. L., Ryan J. L. (2017). Adherence to pediatric treatment regimens. In Roberts M. C., Steele R. G. (Eds.), Handbook of pediatric psychology (pp. 119–133). New York, NY: Guilford Press. [Google Scholar]
- *Hood K. K., Butler D. A., Anderson B. J., Laffel L. M. (2007). Updated and revised diabetes family conflict scale. Diabetes Care, 30, 1764–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood K. K., Peterson C. M., Rohan J. M., Drotar D. (2009). Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics, 124, e1171–e1179. [DOI] [PubMed] [Google Scholar]
- *Ievers-Landis C. E., Burant C. J., Hazen R. (2011). The concept of bootstrapping of structural equation models with smaller samples: an illustration using mealtime rituals in diabetes management. Journal of Developmental and Behavioral Pediatrics, 32, 619–626. [DOI] [PubMed] [Google Scholar]
- Imami L., Tobin E. T., Kane H. S., Saleh D. J., Lupro T. H., Slatcher R. B. (2015). Effects of socioeconomic status on maternal and child positive behaviors in daily life among youth with asthma. Journal of Pediatric Psychology, 40, 55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Iskander J. M., Rohan J. M., Pendley J. S., Delamater A., Drotar D. (2015). A 3-year prospective study of parent–child communication in early adolescents with type 1 diabetes: relationship to adherence and glycemic control. Journal of Pediatric Psychology, 40, 109–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Jacobson A. M., Hauser S. T., Lavori P., Willett J. B., Cole C. F., Wolfsdorf J. I., Dumont R. H., Wertlieb D. (1994). Family environment and glycemic control: a four-year prospective study of children and adolescents with insulin-dependent diabetes mellitus. Psychosomatic Medicine, 56, 401–409. [DOI] [PubMed] [Google Scholar]
- Kahana S., Drotar D., Frazier T. (2008). Meta-analysis of psychological interventions to promote adherence to treatment in pediatric chronic health conditions. Journal of Pediatric Psychology, 33, 590–611. [DOI] [PubMed] [Google Scholar]
- Kazak A. E. (2006). Pediatric Psychosocial Preventative Health Model (PPPHM): Research, practice, and collaboration in pediatric family systems medicine. Families, Systems, & Health, 24(4), 381–395. [Google Scholar]
- *Klitzman P. H., Carmody J. K., Belkin M. H., Janicke D. M. (2018). Behavioral and pharmacological adherence in pediatric sickle cell disease: parent–child agreement and family factors associated with adherence. Journal of Pediatric Psychology, 43, 31–39. [DOI] [PubMed] [Google Scholar]
- *La Greca A. M., Auslander W. F., Greco P., Spetter D., Fisher E. B. Jr, Santiago J. V. (1995). I get by with a little help from my family and friends: adolescents' support for diabetes care. Journal of Pediatric Psychology, 20, 449–476. [DOI] [PubMed] [Google Scholar]
- *Lancaster B. M., Gadaire D. M., Holman K., LeBlanc L. A. (2015). Association between diabetes treatment adherence and parent–child agreement regarding treatment responsibilities. Families, Systems, and Health, 33, 120–125. [DOI] [PubMed] [Google Scholar]
- *Lee S. L., Lo F. S., Lee Y. J., Chen B. H., Wang R. H. (2015). Predictors of glycemic control in adolescents of various age groups with type 1 diabetes. Journal of Nursing Research, 23, 271–279. [DOI] [PubMed] [Google Scholar]
- Leeman J., Crandell J. L., Lee A., Bai J., Sandelowski M., Knafl K. (2016). Family functioning and the well-being of children with chronic conditions: a meta-analysis. Research in Nursing and Health, 39, 229–243. [DOI] [PubMed] [Google Scholar]
- *Lewandowski A., Drotar D. (2006). The relationship between parent-reported social support and adherence to medical treatment in families of adolescents with type 1 diabetes. Journal of Pediatric Psychology, 32, 427–436. [DOI] [PubMed] [Google Scholar]
- Lewin A. B., Heidgerken A. D., Geffken G. R., Williams L. B., Storch E. A., Gelfand K. M., Silverstein J. H. (2006). The relation between family factors and metabolic control: the role of diabetes adherence. Journal of Pediatric Psychology, 31, 174–183. [DOI] [PubMed] [Google Scholar]
- *Loiselle K., Rausch J. R., Modi A. C. (2015). Behavioral predictors of medication adherence trajectories among youth with newly diagnosed epilepsy. Epilepsy and Behavior, 50, 103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mackey E. R., Hilliard M. E., Berger S. S., Streisand R., Chen R., Holmes C. (2011). Individual and family strengths: an examination of the relation to disease management and metabolic control in youth with type 1 diabetes. Families, Systems, and Health, 29, 314–326. [DOI] [PubMed] [Google Scholar]
- *Main A., Wiebe D. J., Croom A. R., Sardone K., Godbey E., Tucker C., White P. C. (2014). Associations of parent–adolescent relationship quality with type 1 diabetes management and depressive symptoms in Latino and Caucasian youth. Journal of Pediatric Psychology, 39, 1104–1114. [DOI] [PubMed] [Google Scholar]
- Mandara J., Murray C. B. (2002). Development of an empirical typology of African American family functioning. Journal of Family Psychology, 16, 318–337. [DOI] [PubMed] [Google Scholar]
- *Markowitz J., Laffel L., Volkening L., Anderson B., Nansel T., Weissberg-Benchell J., Wysocki T. (2011). Validation of an abbreviated adherence measure for young people with Type 1 diabetes. Diabetic Medicine, 28, 1113–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire L. M., Helgeson V. S. (2017). Close relationships and the management of chronic illness: associations and interventions. American Psychologist, 72, 601–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrady M. E., Hommel K. A. (2016). Targeting health behaviors to reduce health care costs in pediatric psychology: Descriptive review and recommendations. Journal of Pediatric Psychology, 41, 835–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrady M. E., Ryan J. L., Brown G. A., Cushing C. C. (2015). Topical review: theoretical frameworks in pediatric adherence-promotion interventions: research findings and methodological implications. Journal of Pediatric Psychology, 40, 721–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Meunier J., Dorchy H., Luminet O. (2008). Does family cohesiveness and parental alexithymia predict glycaemic control in children and adolescents with diabetes? Diabetes and Metabolism, 34, 473–481. [DOI] [PubMed] [Google Scholar]
- *Miller V. A., Drotar D. (2003). Discrepancies between mother and adolescent perceptions of diabetes-related decision-making autonomy and their relationship to diabetes-related conflict and adherence to treatment. Journal of Pediatric Psychology, 28, 265–274. [DOI] [PubMed] [Google Scholar]
- *Miller V. A., Drotar D. (2007). Decision-making competence and adherence to treatment in adolescents with diabetes. Journal of Pediatric Psychology, 32, 178–188. [DOI] [PubMed] [Google Scholar]
- *Miller-Johnson S., Emery R. E., Marvin R. S., Clarke W., Lovinger R., Martin M. (1994). Parent-chld relationships and the management of insulin-dependent diabetes mellitus. Journal of Consulting and Clinical Psychology, 62, 603–610. [DOI] [PubMed] [Google Scholar]
- Miller I. W., Ryan C. E., Keitner G. I., Bishop D. S., Epstein N. B. (2000). The McMaster approach to families: theory, assessment, treatment and research. Journal of Family Therapy, 22, 168–189. [Google Scholar]
- Minuchin P. (1988). Relationships within the family: A systems perspective on development. In Hinde R. A., Stevenson-Hinde J. (Eds.), Relationships within families: Mutual Influences (pp. 7–26). Oxford: Clarendon. [Google Scholar]
- *Mitchell M. J., Powers S. W., Byars K. C., Dickstein S., Stark L. J. (2004). Family functioning in young children with cystic fibrosis: observations of interactions at mealtime. Journal of Developmental and Behavioral Pediatrics, 25, 335–346. [DOI] [PubMed] [Google Scholar]
- Modi A. C., Guilfoyle S. M., Mann K. A., Rausch J. R. (2016). A pilot randomized controlled clinical trial to improve antiepileptic drug adherence in young children with epilepsy. Epilepsia, 57, e69–e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modi A. C., Pai A. L., Hommel K. A., Hood K. K., Cortina S., Hilliard M. E., Guilfoyle S. M., Gray W. N., Drotar D. (2012). Pediatric self-management: a framework for research, practice, and policy. Pediatrics, 129, e473–e485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Monaghan M., Clary L., Mehta P., Stern A., Sharkey C., Cogen F. R., Vaidyanathan P., Streisand R. (2015). Checking in: A pilot of a physician-delivered intervention to increase parent–adolescent communication about blood glucose monitoring. Clinical Pediatrics, 54, 1346–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R. H., Moos B. S. (1994). Family environment scale manual. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Mulvaney S. A., Ho Y.-X., Cala C. M., Chen Q., Nian H., Patterson B. L., Johnson K. B. (2013). Assessing adolescent asthma symptoms and adherence using mobile phones. Journal of Medical Internet Research, 15, e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy L. K., Murray C. B., Compas B. E. (2017). Topical review: integrating findings on direct observation of family communication in studies comparing pediatric chronic illness and typically developing samples. Journal of Pediatric Psychology, 42, 85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noser A. E., Huffhines L., Clements M. A., Patton S. R. (2017). Diabetes conflict outstrips the positive impact of self-efficacy on youth adherence and glycemic control in type 1 diabetes. Pediatric Diabetes, 18, 614–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olkin I., Gleser L. (2009). Stochastically dependent effect sizes. In The handbook of research synthesis and meta-analysis New York, NY: Russell Sage Foundation, (pp. 357–376). [Google Scholar]
- Olson D. H. (2000). Circumplex model of marital and family sytems. Journal of Family Therapy, 22, 144–167. [Google Scholar]
- Pai A. L., McGrady M. (2014). Systematic review and meta-analysis of psychological interventions to promote treatment adherence in children, adolescents, and young adults with chronic illness. Journal of Pediatric Psychology, 39, 918–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T. M., Chambers C. T. (2005). Parent and family factors in pediatric chronic pain and disability: an integrative approach. Pain, 119, 1–4. [DOI] [PubMed] [Google Scholar]
- *Patton S. R., Piazza-Waggoner C., Modi A. C., Dolan L. M., Powers S. W. (2009). Family functioning at meals relates to adherence in young children with type 1 diabetes. Journal of Paediatrics and Child Health, 45, 736–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Pereira M. G., Berg-Cross L., Almeida P., Machado J. C. (2008). Impact of family environment and support on adherence, metabolic control, and quality of life in adolescents with diabetes. International Journal of Behavioral Medicine, 15, 187–193. [DOI] [PubMed] [Google Scholar]
- *Psihogios A. M., Daniel L. C., Tarazi R., Smith-Whitley K., Patterson C. A., Barakat L. P. (2018). Family functioning, medical self-management, and health outcomes among school-aged children with sickle cell disease: a mediation model. Journal of Pediatric Psychology, 43, 423–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Psihogios A. M., Holmbeck G. N. (2013). Discrepancies in mother and child perceptions of spina bifida medical responsibilities during the transition to adolescence: associations with family conflict and medical adherence. Journal of Pediatric Psychology, 38, 859–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Psihogios A. M., Murray C., Zebracki K., Acevedo L., Holmbeck G. N. (2017). Testing the utility of a bio-neuropsychosocial model for predicting medical adherence and responsibility during early adolescence in youth with spina bifida. Journal of Pediatric Psychology, 42, 910–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapoff M. A. (2009). Adherence to pediatric medical regimens. New York, NY: Springer Science & Business Media. [Google Scholar]
- *Reed-Knight B., Lewis J. D., Blount R. L. (2011). Association of disease, adolescent, and family factors with medication adherence in pediatric inflammatory bowel disease. Journal of Pediatric Psychology, 36, 308–317. [DOI] [PubMed] [Google Scholar]
- *Ricker J. H., Delamater A. M., Hsu J. (1998). Correlates of regimen adherence in cystic fibrosis. Journal of Clinical Psychology in Medical Settings, 5, 159–172. [Google Scholar]
- Rosenthal R. (1995). Writing meta-analytic reviews. Psychological Bulletin, 118, 183–192. [Google Scholar]
- Rubin R., Young-Hyman D., Peyrot M. (1989). Parent–child responsibility and conflict in diabetes care. Diabetes, 38(Supp 2), 28a. [Google Scholar]
- Schmucker C., Bluemle A., Briel M., Portalupi S., Lang B., Motschall E., Schwarzer G., Bassler D., Mueller K. F., von Elm E., Meerpohl J. J.; OPEN Consortium. (2013). A protocol for a systematic review on the impact of unpublished studies and studies published in the gray literature in meta-analyses. Systematic Reviews, 2, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons L. E., Gilleland J., Blount R. L., Amaral S., Berg A., Mee L. L. (2009). Multidimensional adherence classification system: initial development with adolescent transplant recipients. Pediatric Transplantation, 13, 590–598. [DOI] [PubMed] [Google Scholar]
- Slatcher R. B., Robles T. F. (2012). Preschoolers’ everyday conflict at home and diurnal cortisol patterns. Health Psychology, 31, 834–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smetana J. G., Campione-Barr N., Metzger A. (2006). Adolescent development in interpersonal and societal contexts. Annual Review of Psychology, 57, 255–284. [DOI] [PubMed] [Google Scholar]
- *Smith A. W., Mara C., Ollier S., Combs A., Modi A. C. (2018). Rebellious behaviors in adolescents with epilepsy. Journal of Pediatric Psychology, 43, 52–60. [DOI] [PubMed] [Google Scholar]
- *Smith B. A., Modi A. C., Quittner A. L., Wood B. L. (2010). Depressive symptoms in children with cystic fibrosis and parents and its effects on adherence to airway clearance. Pediatric Pulmonology, 45, 756–763. [DOI] [PubMed] [Google Scholar]
- Smyth J. M., Stone A. A. (2003). Ecological momentary assessment research in behavioral medicine. Journal of Happiness Studies, 4, 35–52. [Google Scholar]
- *Sonney J. T., Segrin C., Ward T. M. (2017). Associations among behavioral sleep disturbance, family functioning, and controller medication adherence in children with asthma. Journal of Developmental and Behavioral Pediatrics, 38, 208–214. [DOI] [PubMed] [Google Scholar]
- *Stepansky M. A., Roache C. R., Holmbeck G. N., Schultz K. (2010). Medical adherence in young adolescents with spina bifida: Longitudinal associations with family functioning. Journal of Pediatric Psychology, 35, 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Stewart S. M., Lee P. W., Low L. C., Cheng A., Yeung W., Huen K.-F., O'Donnell D. (2000). Pathways from emotional adjustment to glycemic control in youths with diabetes in Hong Kong. Journal of Pediatric Psychology, 25, 393–402. [DOI] [PubMed] [Google Scholar]
- Stirratt M. J., Dunbar-Jacob J., Crane H. M., Simoni J. M., Czajkowski S., Hilliard M. E., Aikens J. E., Hunter C. M., Velligan D. I., Huntley K., Ogedegbe G., Rand C. S., Schron E., Nilsen W. J. (2015). Self-report measures of medication adherence behavior: recommendations on optimal use. Translational Behavioral Medicine, 5, 470–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone A. A., Shiffman S. (2002). Capturing momentary, self-report data: a proposal for reporting guidelines. Annals of Behavioral Medicine, 24, 236–243. [DOI] [PubMed] [Google Scholar]
- Tubiana-Rufi N., Moret L., Czernichow P., Chwalow J. (1998). The association of poor adherence and acute metabolic disorders with low levels of cohesion and adaptability in families with diabetic children. Acta Paediatrica, 87, 741–746. [DOI] [PubMed] [Google Scholar]
- Van Schoors M., Caes L., Knoble N. B., Goubert L., Verhofstadt L. L., Alderfer M. A. (2017). Associations between family functioning and child adjustment after pediatric cancer diagnosis: a meta-analysis. Journal of Pediatric Psychology, 42, 6–18. [DOI] [PubMed] [Google Scholar]
- *Waller D. A., Chipman J. J., Hardy B. W., Hightower M. S., North A. J., Williams S. B., Babick A. J. (1986). Measuring diabetes-specific family support and its relation to metabolic control: a preliminary report. Journal of the American Academy of Child Psychiatry, 25, 415–418. [Google Scholar]
- *White T., Miller J., Smith G. L., McMahon W. M. (2009). Adherence and psychopathology in children and adolescents with cystic fibrosis. European Child and Adolescent Psychiatry, 18, 96–104. [DOI] [PubMed] [Google Scholar]
- *Wood B. L., Miller B. D., Lim J., Lillis K., Ballow M., Stern T., Simmens S. (2006). Family relational factors in pediatric depression and asthma: pathways of effect. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 1494–1502. [DOI] [PubMed] [Google Scholar]
- *Wu Y. P., Rausch J., Rohan J. M., Hood K. K., Pendley J. S., Delamater A., Drotar D. (2014). Autonomy support and responsibility-sharing predict blood glucose monitoring frequency among youth with diabetes. Health Psychology, 33, 1224–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y. P., Rohan J. M., Martin S., Hommel K., Greenley R. N., Loiselle K., Ambrosino J., Fredericks E. M. (2013). Pediatric psychologist use of adherence assessments and interventions. Journal of Pediatric Psychology, 38, 595–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Wysocki T. (1993). Associations among teen-parent relationships, metabolic control, and adjustment to diabetes in adolescents. Journal of Pediatric Psychology, 18, 441–452. [DOI] [PubMed] [Google Scholar]
- Wysocki T. (2015). Introduction to the special issue: direct observation in pediatric psychology research. Journal of Pediatric Psychology, 40, 1–7. [DOI] [PubMed] [Google Scholar]
- Wysocki T., Harris M. A., Buckloh L. M., Mertlich D., Lochrie A. S., Mauras N., White N. H. (2007). Randomized trial of behavioral family systems therapy for diabetes. Diabetes Care, 30, 555–560. [DOI] [PubMed] [Google Scholar]
- Wysocki T., Iannotti R., Weissberg-Benchell J., Laffel L., Hood K., Anderson B., Chen R. (2008). Diabetes problem solving by youths with type 1 diabetes and their caregivers: measurement, validation, and longitudinal associations with glycemic control. Journal of Pediatric Psychology, 33, 875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.