Abstract
Objective
Start Treatment and Recover (STAR) is an emergency department (ED) program that expands access to medication for opioid use disorder by identifying patients with opioid use disorder and offering ED‐initiated buprenorphine/naloxone and rapid access to outpatient treatment. We sought to determine the impacts of the coronavirus disease 2019 pandemic on STAR and the patients with opioid use disorder it serves.
Methods
We conducted a retrospective review of records comparing 2 periods: pre‐pandemic (February 1, 2019–February 29, 2020) and pandemic (March 1, 2020–May 31, 2020). Variables evaluated included the number of STAR enrollments, ED census, percentage of census screening positive for opioid use disorder, number and percentage of ED overdose visits, and overdose fatalities by month. All analyses were conducted using 2‐sample t tests to calculate the mean and 95% confidence intervals (CIs).
Results
Comparing the pre‐pandemic to the pandemic period, the mean monthly ED visits decreased from 5126.9 to 3306.7 (difference = −1820.3; 95% CI, −3406.3 to −234.2), STAR mean monthly enrollments decreased from 9.7 to 1.3 (difference = −8.4; 95% CI, −12.8 to −4.0), and statewide monthly opioid‐related fatalities increased from 9.4 to 15.3 (difference = 5.9; 95% CI, 0.8 to 11.1). However, the percentage of individuals who presented to the ED with opioid use disorder or overdose remained unchanged.
Conclusion
Although overall ED visits declined during the pandemic period, the percentage of patients presenting with opioid use disorder or overdose remained constant, yet there was a dramatic decline in enrollment in ED‐initiated medication for opioid use disorder and an increase in statewide monthly opioid‐related fatalities. Strategies to maintain medication for opioid use disorder treatment options must be implemented for this vulnerable population during the ongoing pandemic.
Keywords: buprenorphine naloxone drug combination, COVID‐19, emergency departments, opioid medication assisted treatment, opioid use disorder, opioid‐related disorders, vulnerable populations
1. INTRODUCTION
1.1. Background
Since coronavirus disease 2019 (COVID‐19) was declared a pandemic, the United States, already in the midst of a devastating opioid epidemic, has seen an increase in fatal opioid‐related overdoses. 1 Explanations for the connection between COVID‐19 and the increased rates of opioid‐related fatalities include social isolation, disruptions in medication for opioid use disorder, lack of access to mental health care services, increase in relapse, lack of access to harm reduction or health care services, increased homelessness and incarceration, and concurrent COVID‐19 infection. 2 Emergency departments (EDs) are uniquely positioned to identify and initiate treatment for patients with opioid use disorder. Many EDs have implemented programs that initiate medication for opioid use disorder, consistently demonstrating that providing access to buprenorphine/naloxone leads to increased enrollment and maintenance in outpatient treatment programs. 3 Start Treatment and Recover (STAR), a program initiated in February 2019 at the University of Vermont Medical Center (UVMMC) ED, expands access to medication for opioid use disorder by identifying patients meeting the criteria for opioid use disorder and offering ED‐initiated medication for opioid use disorder with buprenorphine/naloxone and rapid access to an outpatient addiction treatment program within 72 hours.
1.2. Importance
Opioid use disorder is a complex disease, and combatting opioid use disorder successfully requires a multisystem approach with significant time and resource allocation. The COVID‐19 pandemic has disturbed this system and thus is having a negative impact on patients with opioid use disorder.
1.3. Goals of this investigation
The purpose of this article is to describe the impact of COVID‐19 on STAR and on patients with opioid use disorder who present to the ED.
2. METHODS
2.1. Study design and setting
A retrospective review of records was conducted comparing 2 periods: pre‐pandemic and pandemic. The pre‐pandemic period was defined as February 1, 2019 to February 29, 2020; whereas, the pandemic period was defined as March 1, 2020 to May 31, 2020. The COVID‐19 pandemic was declared a national emergency on March 13, 2020. The start of the pandemic period was chosen as March 1 as we believe impacts from COVID‐19 to the ED realistically predated the emergency declaration. This research was reviewed and approved by the University of Vermont Institutional Review Board.
The Bottom Line
During the COVID‐19 pandemic, the rates of opioid‐related fatalities have increased. In this study comparing pandemic and pre‐pandemic periods at an urban academic emergency department, although the percentage of patients presenting with opioid use disorders or overdoses remained constant, there was a 90% decline in enrollments in ED‐initiated medications for opioid use disorder and an increase in statewide monthly opioid‐related fatalities. These results highlight the need for additional focus on access to opioid use disorder treatment during the ongoing pandemic.
2.2. STAR patient enrollment and treatment
Research coordinators screened the medical records of every patient presenting to the ED for signs of opioid use disorder, including prescribed or illicit use of oral opioids and/or buprenorphine/naloxone, known history of opioid use disorder, intravenous drug use, withdrawal, or referral. Screening started in February 2019 and was performed 21 hours per day until March 31, 2020, at which point research hours were temporarily reduced to 12 hours per day because of the restraints associated with COVID‐19. During the reduced staffing hours, research staff continued to be available on‐call for remote enrollments 24 hours a day/7 days a week. Patients who were aged < 18 years were excluded, whereas those aged > 65 years were initially excluded from the study, but were included as of July 24, 2019. When a potential study subject was identified, a research coordinator consulted with the patient's ED physician to confirm enrollment eligibility. Exclusion criteria included current use of medication for opioid use disorder, altered mental status, medical extremis, incarceration, suboxone injection within 1 year, hepatic impairment, suicidality, opioid use disorder in remission, physician discretion, planned admission, or previous enrollment in STAR.
If the patient met the eligibility criteria, research staff explained the study and enrollment procedure to the patient. This process occurred in person until March 16, 2020, at which point research staff were required to function remotely by phone. For patients interested in participation, research staff obtained consent and collected contact information and enrollment questionnaires. Patients were evaluated by an ED physician and scored via the Clinical Opioid Withdrawal Score (COWS) to determine withdrawal severity. A starter kit containing twelve 2 mg sublingual film strips of buprenorphine/naloxone with home induction instructions and a guaranteed appointment with the UVMMC Addiction Treatment Program within 72 hours were provided. Patients manifesting withdrawal with a COWS score ≥ 8 were administered an immediate 4 mg dose from the starter pack before discharge from the ED.
2.3. Measurements
For each period, we assessed the ED census, percentage of patients screened positive for opioid use disorder, number of patients who presented with overdose, percentage of ED census with overdose, number of patients who screened positive for opioid use disorder, number of patients deemed eligible for STAR, and the number of patients enrolled in STAR by month. These data were obtained from UVMMC ED electronic medical records and the STAR program registry. For additional context, we also examined the statewide and local county opioid fatalities during each period. These data were obtained from the Vermont Department of Health vital records.
2.4. Outcomes
ED census, percentage of census screening positive for opioid use disorder, and number of ED overdose visits were used to assess for enrollment potential. STAR enrollments (primary outcome) were measured to gauge interest in engaging with medication for opioid use disorder. Chittenden County and statewide opioid‐related fatalities were included to identify patterns of opioid use in the local community and larger statewide trends.
2.5. Analysis
Variables were compared between the pre‐pandemic and pandemic periods. All analyses were conducted using a 2‐sample t tests using Stata (version 16; StataCorp, College Station, TX) to determine means and 95% confidence intervals (CIs). Variance ratio testing was performed to determine if the t tests should be conducted with equal or unequal variances.
3. RESULTS
3.1. Patient screening and enrollment
From a total of 54,354 patients screened for opioid use disorder in the ED, 47,706 were screened in the pre‐pandemic period and 6648 in the pandemic period. In the pre‐pandemic period, 1911 individuals screened positive for opioid use disorder, 156 of them were eligible for enrollment after the application of the exclusion criteria, and 126 of them consented to STAR enrollment. During the pandemic period, 308 individuals screened positive for opioid use disorder, 8 of them were eligible for enrollment after the application of the exclusion criteria, and 4 of them consented to STAR enrollment (Figure 1).
FIGURE 1.
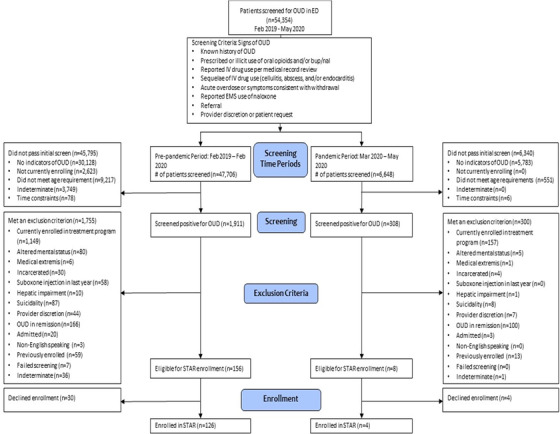
Flowchart of patient screening and enrollment into STAR during pre‐pandemic and pandemic periods. bup/nal, buprenorphine/naloxone; ED, emergency department; EMS, emergency medical services; IV; intravenous; OUD, opioid use disorder; STAR, Start Treatment and Recover
3.2. ED data
The monthly average number of ED visits decreased significantly from 5126.9 to 3306.7 between the pre‐pandemic and pandemic periods (difference = −1820.3; 95% CI, −3406.3 to −234.2). The monthly average percentage of patients screening positive for opioid use disorder increased slightly from 4.3 to 4.6 (difference = 0.3; 95% CI, −0.4 to 1.0), and the average number of monthly ED visits for overdose increased slightly from 17.7 to 20.3 between the pre‐pandemic and pandemic periods (difference = 2.6; 95% CI, −4.8 to 10.1). The average monthly proportion of ED visits for overdose also increased between the pre‐pandemic and pandemic periods, although this was not statistically significant: 0.4% versus 0.7% (difference = 0.3; 95% CI, −0.3 to 0.9). The monthly average number of STAR enrollments dropped significantly from 9.7 to 1.3 (difference = −8.4; 95% CI, −12.8 to −4.0; Table 1, Figure 2).
TABLE 1.
Mean monthly characteristics and outcome measures of patients presenting to the emergency department during the pre‐pandemic (February 1, 2019–February 29, 2020) and pandemic (March 1, 2020–May 31, 2020) periods of the study
| Variable | Pre‐pandemic mean monthly | Pandemic mean monthly | Difference mean (95% CI) |
|---|---|---|---|
| ED census, n | 5126.9 | 3306.7 | −1820.3 (−3406.3 to −234.2) |
| Opioid use disorder of census, % | 4.3 | 4.6 | 0.3 (−0.4 to 1.0) |
| ED overdose, n | 17.7 | 20.3 | 2.6 (−4.8 to 10.1) |
| ED overdose of census, % | 0.4 | 0.7 | 0.3 (−0.3 to 0.9) |
| STAR enrollments, n | 9.7 | 1.3 | −8.4 (−12.8 to −4.0) |
| State overdose fatalities, n | 9.4 | 15.3 | 5.9 (0.8 to 11.1) |
| Chittenden County, VT, overdose fatalities, n | 1.5 | 2.3 | 0.8 (−0.7 to 2.3) |
CI, confidence interval; ED, emergency department; STAR, Start Treatment and Recover.
FIGURE 2.
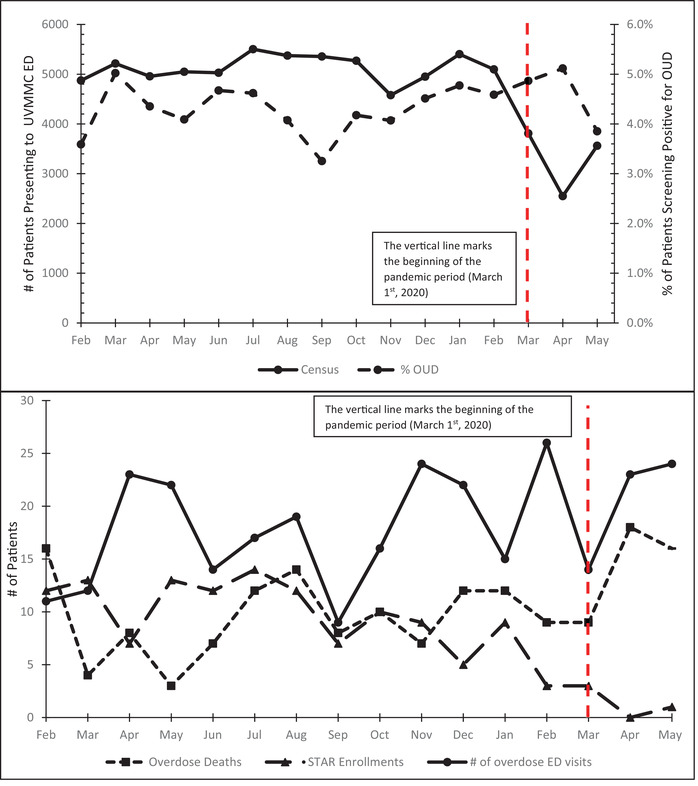
(A) Monthly UVMMC ED census and percentage of monthly census screening positive for opioid use disorder among patients presenting to the ED during the pre‐pandemic (February 1, 2019–February 29, 2020) and pandemic (March 1, 2020–May 31, 2020) periods of the study. (B) Number of enrollments in STAR, number of overdose deaths in Vermont, and number of visits to the ED with drug overdose as chief complaint by month among patients presenting to the ED during the pre‐pandemic (February 1, 2019–February 29, 2020) and pandemic (March 1, 2020–May 31, 2020) periods of the study. Vertical line represents the beginning of the pandemic period. ED, emergency department; OUD, opioid use disorder; STAR, Start Treatment and Recover; UVMMC, University of Vermont Medical Center
3.3. State and county overdose fatality data
Mean monthly statewide overdose‐related fatalities increased significantly from 9.4 to 15.3 (difference = 5.9; 95% CI, 0.8 to 11.1), whereas Chittenden County fatalities increased slightly from 1.5 to 2.3 (difference = 0.8; 95% CI, −0.7 to 2.3; Table 1, Figure 2).
3.4. Seasonal variation
To account for potential seasonal variations in opioid use, the analysis was repeated using pre‐pandemic data that were restricted to the same months of the pandemic (March–May) in 2019 and found similar results. During the seasonal period of 2019, there were 15 opioid‐related fatalities compared with 45 with 1 case pending during the pandemic period, representing a mean monthly increase between seasonal periods from 5.0 to 15.3 (difference = 10.3; 95% CI, 3.0 to 17.7; Table 2).
TABLE 2.
Mean monthly characteristics and outcome measures of patients presenting to the emergency department during the pandemic period (March 1, 2020–May 31, 2020) and the corresponding months of the pre‐pandemic period (March 1, 2019–May 31, 2019)
| Variable | Pre‐pandemic mean monthly | Pandemic mean monthly | Difference mean (95% CI) |
|---|---|---|---|
| ED census, n | 5073.3 | 3306.7 | −1766.7 (−2857.3 to −676.0) |
| Opioid use disorder of census, % | 4.5 | 4.6 | 0.1 (−1.2 to 1.4) |
| ED overdose, n | 19.0 | 20.3 | 1.3 (−11.8 to 14.5) |
| ED overdose of census, % | 0.4 | 0.6 | 0.3 (−0.2 to 0.7) |
| STAR enrollments, n | 11.0 | 1.3 | −9.7 (−15.7 to −3.6) |
| State overdose fatalities, n | 5.0 | 15.3 | 10.3 (3.0 to 17.7) |
| Chittenden County, VT, overdose fatalities, n | 0.3 | 2.3 | 2.0 (−0.6 to 4.6) |
CI, confidence interval; ED, emergency department; STAR, Start Treatment and Recover.
3.5. Limitations
A limitation of this study is the available sample size in the pandemic period. Because of the size of Vermont and the population that UVMMC serves, the sample size of patients with opioid use disorder, overdose visits, and opioid‐related fatalities were small, which limits generalizability to other EDs. However, UVMMC is typical of other community medical centers that also function as academic tertiary referral centers serving a larger rural population, which likely will face similar challenges during the COVID‐19 pandemic. Another limitation was not having access to data on the specific drugs involved in the ED overdoses; however, statewide data suggest that the most predominant misused drugs are opioids.
4. DISCUSSION
Although the overall number of patients presenting to the UVMMC ED during the COVID‐19 pandemic decreased dramatically, the percentage of patients screening positive for opioid use disorder did not change. Moreover, the number of overdose visits remained the same, leading to overdose visits as a percentage of the monthly ED census almost doubling. Despite these conditions, there was a significant 86.2% reduction in STAR enrollment. This suggests that although the need for treatment was unchanged, fewer patients were enrolled in STAR. This decrease may have been attributed to a reluctance from patients or may reflect an impediment on the ED to provide this service. COVID‐19 has created additional barriers to care and has led to an environment with increased risks for patients with opioid use disorder.
The most omnipresent barrier during the pandemic has been fear of contracting COVID‐19. Public messaging during this time was to “Stay Home and Stay Safe,” which may have influenced patients to defer or refuse emergency care and account for a decrease in ED census. Overall, visits to the UVMMC ED decreased by 35.5% during the pandemic. This is consistent with other research showing the total number of US ED visits was 42% lower than the same period a year earlier, 4 including fewer visits for acute processes such as stroke and acute coronary syndrome. 5 Moreover, patients with substance use disorders often experience stigma that prevents them from seeking care and engaging with medication for opioid use disorder. 6 Patients with opioid use disorder may decline emergency medical services (EMS) transport to the ED after an overdose because of concern around this stigma and/or fear of COVID‐19 infection. Research has shown both an increase in EMS calls for opioid overdose and a significant increase in the number of patients who were treated on scene and refused transport during the pandemic. 7 A concerning pattern in the police record management system of Chittenden County found that 88% of overdose fatalities were attributed to using opioids in isolation. 8 Statewide opioid‐related fatalities in Vermont increased by 63.4% during the pandemic period. This suggests that COVID‐19 has driven patients with opioid use disorder to riskier use, avoidance of treatment, and increased mortality.
Other factors may have contributed to the increased rate of overdose and overdose deaths as COVID‐19 has also reduced access to medication for opioid use disorder in community outpatient settings. Although there have been regulatory changes that have allowed medication for opioid use disorder to be initiated and maintained through telehealth, many patients with opioid use disorder lack access to the technology needed to use telehealth, whereas other patients with opioid use disorder may be unwilling to engage in this new treatment modality. Moreover, the transition away from in‐person visits have led to problems in the distribution of harm‐reduction materials. This includes naloxone, fentanyl testing strips, and other safe injection supplies. A lack of access to naloxone and fentanyl testing strips may also have contributed to the increase in fatal and non‐fatal overdoses. 9
Patients who do present to the ED during the pandemic may arrive with higher acuity and more severe disease. A case report illustrated this detailing a patient who, because of fear of COVID‐19, did not seek care for persistent chest pain for 2 days resulting in “catastrophic complications” related to their ST‐segment elevation myocardial infarction. 10 The impact of delaying care in patients with opioid use disorder may mean that people with opioid use disorder are not seeking emergency care until they are being transported to the ED after an overdose or have developed more severe complications associated with opioid use disorder. Once patients are in the ED, they face additional barriers to enrolling in STAR. Research assistants have had to operate remotely during the pandemic, complicating the logistics of completing an enrollment and prolonging the process. Having to enroll over the phone rather than face to face may have also discouraged enrollment through the lack of a personal connection that an in‐person interaction provides. Moreover, having to wait an extended duration in the ED after being medically cleared for discharge to complete the enrollment process may have further discouraged those who were already anxious about coming to the ED because of fears of COVID‐19.
In summary, the COVID‐19 pandemic is having a detrimental impact on patients with opioid use disorder presenting to the ED. Although overall ED visits decreased during the initial months of the pandemic, the percentage of patients presenting with opioid use disorder or overdose‐related visits remained constant, yet there was a significant 86.2% decrease in the number of patients enrolling in ED‐initiated medication for opioid use disorder. Allocation of healthcare resources and strategies devised to mitigate harm and maintain treatment options must be implemented for those struggling with opioid use disorder during the ongoing pandemic.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Daniel Wolfson and Warren Grunvald conceived the study. Daniel Wolfson, Ramsey Herrington, Miles Lamberson, Roz King, Scott Mackey, and Sanchit Maruti supervised the conduct of the trial and data collection. Daniel Wolfson, Roz King, Miles Lamberson managed the data, including quality control. Richard Rawson and Ramsey Herrington provided statistical advice on study design and analyzed the data. Warren Grunvald drafted the manuscript, and all authors contributed substantially to its revision. Daniel Wolfson takes responsibility for the article as a whole.
Biography
Warren Grunvald, BS, is a second‐year medical student at University of Vermont Larner College of Medicine.

Grunvald W, Herrington R, King R, et al. COVID‐19: a new barrier to treatment for opioid use disorder in the emergency department. JACEP Open. 2021;2:e12403. 10.1002/emp2.12403
Funding and support: Substance Abuse and Mental Health Services Administration (SAMHSA) 1H79TI081515‐01, National Institute on Drug Abuse (NIDA) 1R21DA049859‐01, National Institute of General Medical Sciences (NIGMS) 2P20GM103644‐06, and the 2019 University of Vermont Health Network Innovation Grant.
Supervising Editor: Remle P. Crowe, PhD, NREMT.
REFERENCES
- 1. Advocacy Resource Center . Issue Brief: Reports of Increases in Opioid‐related Overdose and Other Concerns during COVID Pandemic. Washington, DC: American Medical Association; 2020. [Google Scholar]
- 2. Mukherjee TI, El‐Bassel N. The perfect storm: COVID‐19, mass incarceration and the opioid epidemic. Int J Drug Policy. 2020:102819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. D'Onofrio G, Chawarski MC, O'Connor PG, et al. Emergency department‐initiated buprenorphine for opioid dependence with continuation in primary care: outcomes during and after intervention. J Gen Intern Med. 2017;32(6):660‐666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hartnett KP, Kite‐Powell A, DeVies J. Impact of the COVID‐19 pandemic on emergency department visits ‐ United States, January 1, 2019‐May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lange SJ, Goodman AB, Dias T, et al. Potential indirect effects of the COVID‐19 pandemic on use of emergency departments for acute life‐threatening conditions—United States, January–May 2020. MMWR Morb Mortal Wkly Rep. 2020(69):795‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Paquette CE, Syvertsen JL, Pollini RA. Stigma at every turn: health services experiences among people who inject drugs. Int J Drug Policy. 2018;57:104‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID‐19 from emergency medical services data. Drug Alcohol Depend. 2020;214:108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Valcour . Police Computer‐aided Dispatch and Record Management System. Chittenden County Opioid Alliance: Chittenden County, VT; 2020. [Google Scholar]
- 9. Vasylyeva TI, Smyrnov P, Strathdee S, Friedman SR. Challenges posed by COVID‐19 to people who inject drugs and lessons from other outbreaks. J Int AIDS Soc. 2020;23(7):e25583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Masroor S. Collateral damage of COVID‐19 pandemic: delayed medical care. J Card Surg. 2020;35(6):1345‐1347. [DOI] [PMC free article] [PubMed] [Google Scholar]


