Abstract
Background
Many studies have addressed influenza vaccine uptake in risk-group populations (e.g. the elderly). However, it is also necessary to assess influenza vaccine uptake in the active adult population, since they are considered to be a high-transmitter group. In several countries pharmacists are involved in adult vaccination in order to increase uptake. This study therefore aimed to investigate the determinants of influenza vaccination uptake and examine the willingness to be vaccinated by pharmacists.
Methods
A cross-sectional study was conducted among Hungarian adults using a self-administered online questionnaire distributed via social media (Facebook). The questionnaire included five domains: demographics, vaccine uptake, factors that motivated or discouraged vaccination, knowledge and willingness of participants to accept pharmacists as influenza vaccine administrators. Descriptive statistics were applied and logistic regression was conducted to assess the possible determinants of vaccination uptake.
Results
Data from 1631 participants who completed the questionnaires were analysed. Almost 58% of respondents (944/1631) had occupational and/or health risk factors for influenza. Just over one-tenth (12.3%;200/1631) of participants were vaccinated during the 2017/18 influenza season, 15.4% (145/944) of whom had a risk factor for influenza. Approximately half of the participants (47.4%) believed that influenza vaccination can cause flu, and just over half of them (51.6%), were not knowledgeable about the safety of influenza vaccine ingredients. Logistic regression found that age, sex, health risk factor and knowledge on influenza/influenza vaccination were associated with influenza vaccination uptake (p < 0.05). The most frequently cited reason for having an influenza vaccination was self-protection (95.0%). The most common reason given for refusing the influenza vaccine was that the respondent stated they rarely had an infectious disease (67.7%). The number of participants who were willing to be vaccinated by pharmacists was two-times higher than the number of participants who were actually vaccinated during the 2017/18 influenza season.
Conclusion
Influenza vaccine uptake in the active adult population is low in Hungary. Public awareness and knowledge about influenza vaccination and influenza disease should be increased. The results also suggest a need to extend the role played by pharmacists in Hungary.
Keywords: Influenza vaccine, Vaccine uptake, Determinants, Adult, Pharmacists
Background
Influenza is a highly infectious viral disease that spreads around the world in annual outbreaks, resulting in between 3 and 5 million cases of severe illness and 290,000–650,000 deaths [1, 2]. One study ranked influenza as the infectious disease with the highest impact on population health in Europe [3].
The most effective way for individuals to avoid this disease is to have an influenza vaccination each year [1, 4]. Influenza vaccination has been recommended by the WHO for some specific populations (e.g. pregnant women and the elderly) [1]. Despite the well-recognised target population for seasonal influenza vaccination, there is some evidence suggesting that vaccination should be also prioritised among those with the highest number of social contacts, i.e. schoolchildren and active adults, to avoid transmission of infections and large outbreaks [5, 6]. Additionally, protective immune response after vaccination may develop in higher rate in the young ones, compared to elderly with immunosenescence [7].
Factors relating to influenza vaccine uptake have previously been investigated mainly in the Western European countries and the USA [8, 9]; a limited number of studies have been performed in Central and Eastern European countries [8–10]. In a multi-site study from eleven European countries, various factors (e.g. socio-economics factors, gender, size of household, educational level and household income) were identified as potential determinants of influenza vaccine uptake, but no data was reported for Hungary [10]. Therefore, there is a need to assess and understand factors that may influence influenza vaccination uptake in Hungary. Beside the lack of knowledge on associated factors of influenza uptake in Hungary, the other motivation of this research was that no other studies focused specifically on the active adult population, which may play crucial role in flu epidemic development.
A review article summarised the strategies that have been applied in an attempt to achieve higher coverage rates for influenza vaccination [11]. As access to influenza vaccination is an important challenge in many countries, one of the recommended strategies was the involvement of community pharmacists as influenza vaccine administrators, due to their better access to patients and more convenient opening time. Pharmacy-based vaccination services have been gradually developing since the end of the twentieth century. These services were first established in Argentina, South-Africa, USA and Australia, but have since expanded to some European countries (Denmark, Ireland, Portugal, Switzerland and the UK) and also to some countries outside of Europe (Canada, Philippines) [12–14]. A systematic review and meta-analysis showed that the involvement of pharmacists in vaccination programmes, whether as educators, facilitators or administrators of vaccines, resulted in increased vaccination rates [15]. Accordingly, the International Federation of Pharmacists (FIP) has a strong commitment to improve vaccination coverage through pharmacists and actively advocate pharmacy vaccination for more than a decade [14, 16]. Despite the well-recognised benefits of the involvement of pharmacists, no pharmacy-based vaccination services currently exist in Central or Eastern Europe and it is important to observe whether the patients willing to be vaccinated by pharmacists in Hungary. As access to influenza vaccination may be challenging for Hungarian adults as well, there is potential to improve access and vaccination uptake by enabling pharmacists to give flu vaccinations.
The main objective of the present study was to investigate the determinants of influenza vaccination uptake in the active adult population in Hungary and secondly to explore participants’ willingness to accept pharmacists as influenza vaccine administrators.
Methods
Study design and setting
The study was an observational cross-sectional study carried out in Hungary between March and July 2018. The self-administered questionnaire was distributed via social media (Facebook). Facebook is the most popular social media used in Hungary and majority (80%) of the users belong to the 20–59 years age group [17]. The questionnaire was constructed on Google docs and the link was shared to public via various Hungarian Facebook Groups (N = 35). In order to achieve a neutral sampling, we targeted participants based on various leisure time activities (i.e. different newspaper readers, fishermen, bee keepers, cooking groups, etc.). First, we contacted the group administrators to put the link on the open page and sent them reminders for 2–3 times.
Participants
Everyone who lives in Hungary, understands Hungarian and has a Facebook account was eligible to voluntarily take part in this study. No financial or other incentives were applied. During the analysis, however, we focused on the active adult population, aged 20 to 59 years.
Sample size
We adopted the sample size calculation written by Lemeshow et al. and published by the World Health Organisation [18]. We assumed that each of the main outcome measures has a prevalence between 5 and 95% (not very rare or very frequent). After we targeted the highest minimal sample size (N = 384) that could be required, with a precision estimate of ±5% and the type I error (alpha) of 5% at 95% confidence level.
Questionnaire
The survey instrument was a questionnaire. The questions included general characteristics (e.g. age, sex, risk factors for influenza based on The Annual Vaccine Guideline of the Hungarian Ministry of Health [19]), uptake of the seasonal influenza vaccine during the 2017/18 influenza season, factors motivating or discouraging uptake of the vaccine (see complete list of questions in Table 3), participants’ knowledge in relation to influenza and influenza vaccination (see complete list of questions in Table 5) and the willingness of the participants to receive an influenza vaccination from their community pharmacist. Questions on potential determinants and knowledge items were based on published studies [20–23] and own ideas of the study team. The study team discussed potential questions at several rounds, and included questions after consensus. Then the questionnaire was piloted with a sample of ten individuals to ensure the clarity of the questions.
Table 3.
Participants’ cited reasons for their vaccination statusa
| Reasons for being … | Number (%) |
|---|---|
| Vaccinated, n = 200 (100%) | |
| To protect myself from the flu and its complications | 190(95.0) |
| To protect those with risk factors around me | 122(61.0) |
| I consider flu a severe disease | 105(52.5) |
| I belong to a risk group, I am prone to infections/diseases | 69(34.5) |
| I had severe influenza previously | 31(15.5) |
| Death due to influenza complications around me (in my neighbourhood) | 7(3.5) |
| Unvaccinated, n = 1431 (100%) | |
| Because I rarely get infectious diseases (including influenza) | 968(67.7) |
| Because I do not have a risk factor | 700(48.9) |
| Because nobody has a risk factor around me | 587(41.0) |
| Because I prefer alternative therapies (e.g. natural medicine) | 511(35.7) |
| I consider influenza a minor disease | 463(32.4) |
| Because I am afraid of the side effects | 451(31.5) |
| Because of the contradictory opinions on flu vaccine | 411(28.7) |
| I consider the vaccine ineffective | 380(26.6) |
| Because I prefer medical therapy | 361(25.2) |
| Previous bad experience with flu vaccine among family members/acquaintance | 341(23.8) |
| Because I forgot and missed it | 263(18.4) |
| Because I am afraid of the needles | 172(12.0) |
| I received the flu vaccine previously, but it was ineffective because I got the flu | 156(10.9) |
| Influenza vaccine is contraindicated to me | 93(6.5) |
| I received the flu vaccine previously, but I experienced major/serious side effects | 85(5.9) |
aParticipants’ could give more than one reason
Table 5.
Participants’ knowledge about influenza and influenza vaccination
| Question | Correct answer | Answer | Vaccinated n = 200 (100%) |
Unvaccinated n = 1431 (100%) |
Total n = 1631 (100%) |
|---|---|---|---|---|---|
| Number (%) | Number (%) | Number (%) | |||
| Influenza is an infectious disease | True | Correct | 194(97.0) | 1333(93.2) | 1527(93.6) |
| Wrong | 4(2.0) | 57(4.0) | 61(3.7) | ||
| Do not know | 0(0.0) | 30(2.1) | 30(1.8) | ||
| NA | 2(1.0) | 11(0.8) | 13(0.8) | ||
| Influenza vaccination is recommended annually for the risk groups | True | Correct | 194(97.0) | 1122(78.4) | 1316(80.7) |
| Wrong | 0(0.0) | 87(6.1) | 87(5.3) | ||
| Do not know | 3(1.5) | 205(14.3) | 208(12.8) | ||
| NA | 3(1.5) | 17(1.2) | 20(1.2) | ||
| Influenza vaccination is highly/specially recommended for the elderly | True | Correct | 189(94.5) | 988(69.0) | 1282(78.6) |
| Wrong | 1(0.5) | 148(10.3) | 119(7.3) | ||
| Do not know | 6(3.0) | 280(19.6) | 209(12.8) | ||
| NA | 4(2.0) | 15(1.1) | 21(1.3) | ||
| Influenza vaccination is highly/specially recommended for those with chronic diseases | True | Correct | 185(92.5) | 1093(76.4) | 1173(71.9) |
| Wrong | 4(2.0) | 118(8.3) | 152(9.3) | ||
| Do not know | 9(4.5) | 203(14.2) | 289(17.7) | ||
| NA | 2(1.0) | 17(1.2) | 17(1.0) | ||
| Elderly and those with certain chronic diseases can get the flu vaccination for free | True | Correct | 183(91.5) | 1009(70.5) | 1192(73.1) |
| Wrong | 4(2.0) | 48(3.4) | 52(3.2) | ||
| Do not know | 11(5.5) | 360(25.2) | 371(22.8) | ||
| NA | 2(1.0) | 14(1.0) | 16(1.0) | ||
| Influenza is a synonym for common cold | False | Correct | 179(89.5) | 1239(86.6) | 1418(86.9) |
| Wrong | 9(4.5) | 106(7.4) | 115(7.1) | ||
| Do not know | 7(3.5) | 73(5.1) | 80(4.9) | ||
| NA | 5(2.5) | 13(0.9) | 18(1.1) | ||
| In case of fever the vaccination should be postponed | True | Correct | 177(88.5) | 1176(82.2) | 1353(83.0) |
| Wrong | 7(3.5) | 41(2.9) | 48(2.9) | ||
| Do not know | 13(6.5) | 199(13.9) | 212(13.0) | ||
| NA | 3(1.5) | 15(1.1) | 18(1.1) | ||
| The best method to prevent influenza is the influenza vaccination | True | Correct | 172(86.0) | 619(43.3) | 791(48.5) |
| Wrong | 12(6.0) | 453(31.7) | 465(28.5) | ||
| Do not know | 13(6.5) | 339(23.7) | 352(21.6) | ||
| NA | 3(1.5) | 20(1.4) | 23(1.4) | ||
| Time to onset of action is 2 weeks for influenza vaccination in case of adults | True | Correct | 163(81.5) | 841(58.8) | 1004(61.6) |
| Wrong | 6(3.0) | 68(4.8) | 74(4.5) | ||
| Do not know | 29(14.5) | 501(35.0) | 530(32.5) | ||
| NA | 2(1.0) | 21(1.5) | 23(1.4) | ||
| Influenza vaccine contains safe ingredients | True | Correct | 159(79.5) | 606(42.4) | 765(46.9) |
| Wrong | 8(4.0) | 258(18.0) | 266(16.3) | ||
| Do not know | 31(15.5) | 544(38.0) | 575(35.3) | ||
| NA | 2(1.0) | 23(1.6) | 25(1.5) | ||
| Influenza can be prevented by high dose vitamin C (min. 500 mg daily) instead of vaccination | False | Correct | 156(78.0) | 662(46.3) | 818(50.2) |
| Wrong | 12(6.0) | 407(28.4) | 419(25.7) | ||
| Do not know | 30(15.0) | 344(24.0) | 374(22.9) | ||
| NA | 2(1.0) | 18(1.3) | 20(1.2) | ||
| Antibiotics work against influenza | False | Correct | 155(77.5) | 953(66.6) | 1108(67.9) |
| Wrong | 24(12.0) | 321(22.4) | 345(21.2) | ||
| Do not know | 18(9.0) | 144(10.1) | 162(9.9) | ||
| NA | 3(1.5) | 13(0.9) | 16(1.0) | ||
| The flu vaccination can weaken the immune system | False | Correct | 151(75.5) | 652(45.6) | 803(49.2) |
| Wrong | 24(12.0) | 439(30.7) | 463(28.4) | ||
| Do not know | 22(11.0) | 320(22.4) | 342(21.0) | ||
| NA | 3(1.5) | 20(1.4) | 23(1.4) | ||
| Influenza can be prevented by herbs (e.g. honey, ginger tea) instead of vaccination | False | Correct | 143(71.5) | 672(47.0) | 815(50.0) |
| Wrong | 13(6.5) | 374(26.1) | 387(23.7) | ||
| Do not know | 41(20.5) | 368(25.7) | 409(25.1) | ||
| NA | 3(1.5) | 17(1.2) | 20(1.2) | ||
| You should not take influenza vaccination if you have already got influenza | False | Correct | 117(58.5) | 625(43.7) | 742(45.5) |
| Wrong | 49(24.5) | 421(29.4) | 470(28.8) | ||
| Do not know | 32(16.0) | 370(25.9) | 402(24.7) | ||
| NA | 2(1.0) | 15(1.0) | 17(1.0) | ||
| The flu vaccination can cause flu | False | Correct | 109(54.5) | 390(27.3) | 499(30.6) |
| Wrong | 62(31.0) | 711(49.7) | 773(47.4) | ||
| Do not know | 27(13.5) | 308(21.5) | 335(20.5) | ||
| NA | 2(1.0) | 22(1.5) | 24(1.5) | ||
| In case of egg allergy, the flu vaccination can be taken | True | Correct | 58(29.0) | 323(22.6) | 381(23.4) |
| Wrong | 61(30.5) | 264(18.5) | 325(19.9) | ||
| Do not know | 79(39.5) | 822(57.4) | 901(55.2) | ||
| NA | 2(1.0) | 22(1.5) | 24(1.5) |
Binary questions were asked about both seasonal influenza vaccination uptake and the willingness of participants to receive an influenza vaccination from a pharmacist. Multiple choice questions were used to gain information relating to factors motivating or discouraging influenza vaccination uptake.
The knowledge of participants relating to influenza/influenza vaccination was measured using a set of 17 questions. For each question, there were three possible answers: ‛yes’, ‛no’ or ‛don’t know’. One point was assigned for each correct answer, zero points were given for the ‛don’t know’ answer and one point was subtracted for giving the wrong answer. Finally, the total was calculated, with a range from − 17 to + 17, then calculated as the percentage of the total achievable points. For this knowledge section, the answers of participants who had more than five missing answers were excluded from the analysis.
Data analysis
Descriptive, bivariate and multivariate statistical analyses were applied to describe all survey items. Descriptive statistics, including means, standard deviations and percentages were used to describe all variables. Bivariate analyses, such as Pearson’s chi-square test and Fisher’s exact test, were used to compare categorical variables. Logistic regression was conducted to assess the potential associated factors of influenza vaccination uptake and adjusted odds ratios were reported. The level of statistical significance was set at p < 0.05. All statistical analyses were performed using R software (R version 3.6.1).
Results
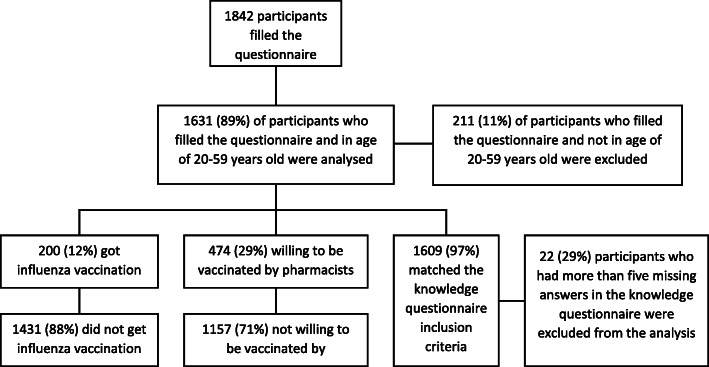
In total, 1842 questionnaires were filled. Of these, 1631 questionnaires were analysed and 211 were excluded since those were filled by participants who were not in the active adult (20–59 years old) population (Fig. 1). The mean age of participants was 33.7 years (SD = 10.7; CI 95% 33.2–34.2), while 944 participants (57.9%; CI 95% 55.5–60.3) had occupational and/or health risk factors for influenza. Just over one-tenth (12.3%; CI 95% 10.8–13.9) of participants had received an influenza vaccination during the previous influenza season, and 15.4% (145/944; CI 95% 13.2–17.8) of those had a risk factor for influenza. The general characteristics of the participants are presented in Table 1.
Fig. 1.
Flow chart of participants in the study
Table 1.
Bivariate analysis of participants’ general characteristics and influenza vaccination uptake during the 2017/18 influenza season
| Variable | Vaccination status | Statistical test | p-value | ||
|---|---|---|---|---|---|
| Yes (n = 200) | No (n = 1431) | Total | |||
| Number (Row %) | Number (Row %) | Number (Col.%) | |||
| Age (years) | |||||
| (mean ± SD) | 37.5 ± 11.2 | 33.2 ± 10.5 | 33.7 ± 10.7 | Welch’s two Sample t-test | < 0.001 |
| Sex | |||||
| Male | 50 (16.1) | 260 (83.9) | 310 (19.0) | Pearson’s Chi-square test | 0.0214 |
| Female | 150 (11.4) | 1170 (88.6) | 1320 (80.9) | ||
| N/A | 0 (00.0) | 1 (100) | 1 (00.0) | ||
| Type of residence | |||||
| Village | 33 (13.3) | 225 (86.8) | 258 (15.8) | Pearson’s Chi-square test | 0.7587 |
| City | 166 (12.1) | 1205 (87.9) | 1371 (84.1) | ||
| N/A | 1(0.5) | 1 (0.5) | 2 (0.1) | ||
| Educational level | |||||
| Primary |
4 (15.4) |
22 (84.6) |
26 (1.6) |
Fisher’s exact test for count data | 0.0146 |
| Secondary |
87 (10.1) |
772 (89.9) |
859 (52.7) |
||
| Tertiary |
109 (14.7) |
635 (85.4) |
744 (45.6) |
||
| N/A |
0 (0.0) |
2 (100) |
2 (0.1) |
||
| Occupational risk factor a | |||||
| Yes | 88(17.2) | 424(82.8) | 512(31.4) | Pearson’s Chi-square test | < 0.001 |
| No | 112(10.1) | 1002(89.9) | 1114(68.3) | ||
| N/A | 0(0.0) | 5(100) | 5(0.3) | ||
| Health risk factor b | |||||
| Yes | 95(15.1) | 536(84.9) | 631(38.7) | Pearson’s Chi-square test | 0.0063 |
| No | 105(10.5) | 895(89.5) | 1000(61.3) | ||
| Knowledge (N = 1609) | |||||
| (mean ± SD) | 85.4 ± 9.7 | 70.7 ± 15.1 | 72.5 ± 15.3 | Welch’s two Sample t-test | < 0.001 |
aOccupational risk factors include participants who have at least one of the following statuses: students in the health care field; work in health care services; social institution/long care term facility; nursery school/kindergarten; livestock or animal transfer (swine, poultry, horse); poultry processing or abattoir; work with immigrants/foreign people
bHealth risk factors include participants who had at least one of the following conditions in the previous year: heart failure; coronary artery disease; chronic pulmonary disease; immune disease; taking immunosuppressive drugs; inflammatory bowel disease; chronic liver disease; chronic kidney disease; pregnancy/planning pregnancy; disabled (physically); smoker
Demographics relating to vaccination uptake among participants
Overall, there were significant differences in age, sex, educational level, occupational risk factor, health risk factor and knowledge of vaccinated versus unvaccinated participants (p < 0.05) in the bivariate analysis. Participants’ type of residence was the only variable that showed no significant difference between vaccinated and unvaccinated participants (Table 1). Furthermore, logistic regression showed that age, sex, health risk factor and knowledge about influenza were associated with influenza vaccination uptake (Table 2).
Table 2.
Logistic regression analysis to identify associated factors for influenza vaccination uptake (n = 1602)
| OR | 95% CI | p-value | |
|---|---|---|---|
| Age | 1.028 | 1.012–1.044 | 0.001 |
| Sex (male) | 1.838 | 1.217–2.774 | 0.004 |
| Occupational risk factor | 1.211 | 0.838–1.751 | 0.309 |
| Health risk factor | 2.070 | 1.472–2.910 | 0.000 |
| Educational level – Primary (reference) | – | – | – |
| Secondary | 0.568 | 0.149–2.171 | 0.408 |
| Tertiary | 0.585 | 0.153–2.241 | 0.434 |
| Knowledge | 1.096 | 1.078–1.114 | 0.000 |
Factors which motivated or discouraged vaccination uptake
The reasons for obtaining or not obtaining the influenza vaccination are summarised in Table 3. The most commonly cited reasons for having the vaccination were ‛self-protection’ (95.0%), ‛to protect those with risk factors around’ (61.0%) and ‛consider influenza as severe disease’ (52.5%). The most cited reasons for not having the vaccination were ‛I rarely get infectious diseases’ (67.7%), followed by ‛I do not have a risk factor’ (48.9%) and ‛nobody has risk factor around’ (41.0%). In total, 700 (48.9%) unvaccinated participants selected ‛I do not have a risk factor’ as their reason for not having the vaccination; however, we discovered that in reality just over half of them (353/700) had at least one risk factor for influenza.
Table 4 shows the role played by different sources of advice or opinions when it came to participants’ vaccination status. Most participants stated that they were not influenced (indifferent or not influenced categories) by any external opinions with regard to their influenza vaccination uptake. Approximately one-third of vaccinated participants stated that their decision had been influenced by a recommendation from a specialist doctor, a GP, another healthcare worker or a family member.
Table 4.
The role played by different sources of recommendations/opinions on individuals’ vaccination uptake decision
| Source of recommendation or opinion | To have the influenza vaccine n = 200 (100%) |
To not have the influenza vaccine n = 1431 (100%) |
|---|---|---|
| Number (%) | Number (%) | |
| Specialist | ||
| Influenced | 75(37.5) | 234(16.4) |
| Indifferent | 19(9.5) | 256(17.9) |
| Not influenced | 84(42.0) | 841(58.8) |
| N/A | 22(11.0) | 100(7.0) |
| Family member | ||
| Influenced | 70(35.0) | 368(25.7) |
| Indifferent | 32(16.0) | 280(19.6) |
| Not influenced | 77(38.5) | 701(49.0) |
| N/A | 21(10.5) | 82(5.7) |
| General practitioner | ||
| Influenced | 68(34.0) | 187(13.1) |
| Indifferent | 27(13.5) | 277(19.4) |
| Not influenced | 85(42.5) | 861(60.2) |
| N/A | 20(10.0) | 106(7.4) |
| Other healthcare worker | ||
| Influenced | 62(31.0) | 301(21.0) |
| Indifferent | 26(13.0) | 266(18.6) |
| Not influenced | 89(44.5) | 783(54.7) |
| N/A | 23(11.5) | 81(5.7) |
| Pharmacist | ||
| Influenced | 28(14.0) | 173(12.1) |
| Indifferent | 28(14.0) | 279(19.5) |
| Not influenced | 112(56.0) | 870(60.8) |
| N/A | 32(16.0) | 109(7.6) |
| Media (internet/television/radio) | ||
| Influenced | 12(6.0) | 109(7.6) |
| Indifferent | 30(15.0) | 330(23.1) |
| Not influenced | 124(62.0) | 888(62.1) |
| N/A | 34(17.0) | 104(7.3) |
Knowledge of influenza vaccination/influenza disease
The participants’ knowledge in response to certain questions is summarised in Table 5. Most participants (93.6%) knew that influenza is an infectious disease. On the other hand, approximately half of the participants (47.4%) believed that influenza vaccination can cause flu, and just over half of them (51.6%), calculated from the sum of ‘wrong’ and ‘unknown’ answers) were not knowledgeable about the safety of influenza vaccine ingredients (Table 5).
In total, only 30.6% of all participants gave a correct answer to the statement ‛flu vaccine can cause influenza disease’; however, the vaccinated group showed better knowledge compared with the knowledge of the unvaccinated group (54.5% vs 27.3%) (Table 5). Moreover, vaccinated participants scored higher for each knowledge question in comparison with the scores of non-vaccinated participants. This higher level of knowledge was identified as one of the factors associated with influenza vaccine uptake (p < 0.05) (Table 2).
There were large differences in the level of knowledge between vaccinated and unvaccinated participants with regard to assumptions that influenza vaccination is the best method to prevent influenza (12.5% vs 55.4%), the safety of vaccine ingredients (19.5% vs 56.1%) and whether the influenza vaccine can cause influenza disease (44.5% vs 71.2%) (These numbers were calculated from the sum of ‘wrong’ and ‘unknown’ answers in Table 5).
Willingness to accept pharmacists as influenza vaccine administrators
Overall, almost one-third (29.1%; CI 95% 26.9–31.3) of all participants would accept an influenza vaccination from a pharmacist. Table 6 shows that the willingness to accept pharmacists as vaccine administrators was significantly higher among participants who had been vaccinated during the last influenza season (p < 0.05). Similarly, the mean knowledge score of participants who were willing to get their influenza vaccination at a pharmacy was significantly higher compared with the knowledge of those who said they would refuse a pharmacy-based service (p < 0.05). The number of participants who were willing to be vaccinated by pharmacists (n = 474) was two times higher than the number of participants who were actually vaccinated during the 2017/18 influenza season (n = 200).
Table 6.
Bivariate analysis of general characteristics and participants’ willingness to be vaccinated by a pharmacist
| Variable | Willingness to be vaccinated by a pharmacist | Statistical test | p-value | |
|---|---|---|---|---|
| Yes n = 474 (100%) |
No n = 1157 (100%) |
|||
| Number (%) | Number (%) | |||
| Age (years) | ||||
| (mean ± SD) | 32.5 ± 10.8 | 34.2 ± 10.6 | Welch’s two sample t-test | 0.0029 |
| Sex | ||||
| Male | 132(42.6) | 178(57.4) | Pearson’s Chi-square test | < 0.001 |
| Female | 341(25.8) | 979(74.2) | ||
| N/A | 1(100) | 0(0.0) | ||
| Type of residence | ||||
| Village | 61(23.6) | 197(76.4) | Pearson’s Chi-square test | 0.0375 |
| City | 412(30.0) | 959(70.0) | ||
| N/A | 1(50.0) | 1(50.0) | ||
| Education level | ||||
| Primary | 14(53.9) | 12(46.1) | Pearson’s Chi-square test | 0.0192 |
| Secondary | 245(28.5) | 614(71.5) | ||
| Tertiary | 214(28.8) | 530(71.2) | ||
| N/A | 1(50.0) | 1(50.0) | ||
| Occupational risk a | ||||
| Yes | 122(23.8) | 390 (76.2) | Pearson’s Chi-square test | 0.0014 |
| No | 352(31.6) | 762(68.4) | ||
| N/A | 0(0.0) | 5(100) | ||
| Health conditions risk b | ||||
| Yes | 179(28.4) | 452(71.6) | Pearson’s Chi-square test | 0.6238 |
| No | 295(29.5) | 705 (70.5) | ||
| Vaccinated | ||||
| Yes | 116(58.0) | 84(42.0) | Pearson’s Chi-square test | < 0.001 |
| No | 358(25.0) | 1073(75.0) | ||
| Knowledge (n = 1609) | ||||
| (mean ± SD) | 79.3 ± 12.4 | 69.8 ± 15.5 | Welch’s two sample t-test | < 0.001 |
aOccupational risk factors include participants who have at least one of the following statuses: students in the healthcare field; work in health care services; social institution/long care term facility; nursery school/kindergarten; livestock or animal transfer (swine, poultry, horse); poultry processing or abattoir; work with immigrants/foreign people
bHealth risk factors include participants who had at least one of following conditions in the previous year: heart failure; coronary artery disease; chronic pulmonary disease; immune disease; taking immunosuppressive drugs; inflammatory bowel disease; chronic liver disease; chronic kidney disease; pregnancy/planning pregnancy; disabled (physically); smoker
Discussion
There are limited data available relating to influenza vaccine uptake patterns in Central and Eastern Europe. The technical report of the ECDC on seasonal influenza coverage rate [24] showed that in Hungary, vaccination rate among the elderly (above 60 years) was 21.9% in 2017/2018, which is far from the target of 75%. In the present study focusing on only active adults, the influenza vaccination uptake of respondents was low, 12.3%. A similarly low level (9.5%) of vaccination coverage was reported from Poland (considering the whole population), and generally influenza vaccination uptake was suboptimal across Europe [10]. More than half (944/1631) of participants in the present study had occupational and/or health risk factors, and only 15.4% of them had been vaccinated against influenza. Recent studies have reported that vaccination rates among adults aged 16 to 65 years old who had a risk factor were higher, at between 29.8 and 49.2% in Australia and between 45.7 and 49.4% in England [25, 26].
Our findings showed that approximately one in two participants believed that the influenza vaccine can cause influenza (47.4%) and half of them were not knowledgeable about the safety of influenza vaccine ingredients (51.6%). These factors might have influenced these participants’ decisions not to have an influenza vaccination during the 2017/18 influenza season.
Demographics relating to vaccination uptake among participants
With regard to the demographic factors associated with influenza vaccine uptake, some of our findings are similar to previously published findings. In the present study, older age was associated with influenza vaccination uptake (Table 2). A similar finding was reported by a systematic review that focused on European and Asian populations [27]. The present study also showed that being male was associated with being vaccinated (Table 2). Additionally, some studies have noted that being female can be a barrier to influenza vaccine uptake [8, 10, 28]. However, the aforementioned systematic review reported that sex was not a consistent predictor of influenza vaccination across different European countries [27].
Another factor associated with influenza vaccination uptake was having a health risk factor. A similar association between health risk factors and vaccine uptake has been reported in some previous studies [20, 28, 29]. However, the earlier systematic review found that occupational health risk factors were not a consistent predictor of influenza vaccination uptake [27].
Factors that motivated or discouraged vaccination uptake
The most frequently cited reasons for having an influenza vaccination were ‛self-protection’ and ‛to protect those with risk factors around’, which were also noted in other studies [20, 22, 30], followed by ‛consider flu as a severe disease’. These stated reasons imply that vaccinated people are more likely to be aware of the negative impacts of influenza disease. Of note, social responsibility was an important motivating factor for influenza vaccination. In the unvaccinated group, the most frequently stated reasons for not having influenza vaccination were ‛rarely get influenza’, followed by ‛I do not have a risk factor’. Surprisingly, we found that participants who selected ‛I do not have a risk factor’ in fact had at least one existing risk factor. It can be assumed that participants’ perception of risk factors needs to be improved through some type of educational intervention by healthcare professionals. Previous studies have also shown that the low uptake of the influenza vaccine is related to the perceived low risk of the disease [8, 20, 28, 30–32].
More than one-third of vaccinated participants reported that healthcare workers or a family member influenced their decision to have the influenza vaccine. Previous studies have also reported that a recommendation or opinion from healthcare workers or family members is a factor that influences whether someone has an influenza vaccination [8, 20, 30, 33]. Interestingly, some of participants stated that they were influenced by healthcare workers (specialist, GP, pharmacist and other HCWs) not to take the influenza vaccine; the reason for this are unclear. It is possible that HCWs may have their own personal beliefs regarding to influenza and/or influenza vaccination. A systematic review showed that HCW’s personal beliefs may act as barriers to vaccine uptake, including concerns about side effects, scepticism about vaccine effectiveness and the belief that influenza is not a serious illness [34].
However, most participants in the present study stated that their decision was not influenced by any external source. It can be concluded that most participants’ decisions whether to have the influenza vaccination were mainly influenced by their own perceptions about influenza disease and/or the influenza vaccine. A previous systematic review found that perceptions around vaccine efficacy, safety and adverse events were the most influential factors in influenza vaccination uptake [27]. Consequently, educational interventions relating to influenza disease and/or influenza vaccine should be targeted at patients themselves.
Knowledge about influenza vaccination/influenza disease
This survey found that participants’ level of knowledge around influenza vaccination and influenza disease associated with influenza vaccine uptake. Other studies have also found a higher level of knowledge to be associated with higher vaccination uptake rates [21, 27, 29, 35]. Additionally, previous research has shown that a lack of general knowledge about influenza/influenza vaccination was a barrier to influenza vaccination uptake [8].
Large differences existed in the level of knowledge between vaccinated and unvaccinated groups with regard to assumptions around the best method to prevent influenza, the safety of vaccine ingredients and whether the influenza vaccine can cause influenza disease. Overall, the vaccinated participants were more knowledgeable than the unvaccinated ones in all other question items. These findings provide evidence that the lack of knowledge regarding the effectiveness and safety of the influenza vaccine in the unvaccinated group might influence these participants’ attitudes towards influenza vaccination.
Willingness to accept pharmacists as influenza vaccine administrators
Previous studies have suggested that pharmacy-provided vaccines may increase the uptake of the influenza vaccine [15, 36, 37]. In Hungary, pharmacy-provided vaccines are not yet available. However, this study found that almost one-third (29.1%) of participants would be willing to receive their influenza vaccine from pharmacists. The participants’ willingness in this regard may indicate that some of them already trust pharmacists to be vaccine administrators.
The results of the statistical analysis showed significant differences in the general characteristics of those who, in principle, said they accepted (the ‛willing group’) and those who, in principle, said they would refuse (the ‛unwilling group’) pharmacists as vaccine administrators. Of the demographic factors, sex, occupational risk factor, level of knowledge and vaccination status were variables having clinical relevance. These findings imply that male participants, participants with an occupational risk factor, participants with a higher level of knowledge about influenza vaccination/influenza disease and those who had been vaccinated against influenza were more willing to be vaccinated by pharmacists.
We observed that the number of participants who were willing to be vaccinated by pharmacists was two-times higher than the number of participants who were actually vaccinated during the 2017/18 influenza season. These findings suggest that influenza vaccination uptake in Hungary might be increased if pharmacists were involved. A number of studies into pharmacy-based influenza vaccination services have been published [12, 15, 38]. Studies have reported that patient satisfaction with pharmacist-administered vaccination was high [39–41]. Being vaccinated by pharmacists would also provide additional educational opportunities. For example, pharmacists can deliver correct information about the safety and quality of the influenza vaccine (e.g. the safety of the ingredients and quality assurance of the product).
Strengths and limitations
The strength of this study was the large sample size used to assess influenza vaccine uptake, related knowledge, and potential role of pharmacist as vaccine administrators. in Hungary. The findings in this study are, however, subject to some limitations. Data were self-reported by participants who were voluntary recruited via Facebook that could induce selection bias and the reported vaccination rates could not be verified by checking participants’ medical records (recall bias). Due to the method, the share of inhabitants below 40 years of age were overrepresented in the study group which leads to slight underestimation of influenza vaccination uptake. Those who are lacking internet access or Facebook account are not represented in the study group. As social media access might be associated with level of influenza vaccine acceptance, either directly or indirectly, this limitation may lead to over- or under-estimation of influenza vaccination coverage. The study of Ahmed et al. from the U.S. showed that users of Facebook or Twitter had higher influenza vaccination uptake, compared to non-users of social media [42]. On the contrary, a strong anti-vaccine content on Facebook were detected in some countries [43–45] (note that nowadays Facebook is reducing the distribution of misinformation about vaccination and increasing users’ exposure to credible, authoritative information) [46]. In Hungary, the presence of anti-vaccine content might only slightly influence the research findings, since the level of public trust in compulsory vaccinations are above 90% in Hungary and compulsory childhood vaccine uptake is close to 100%, which is outstanding in Europe [46].
Based on the survey method, our results may not represent well the whole Hungarian population. On the other hand, this exploratory study clearly identified problematic areas where educational interventions should focus.
Conclusions
Influenza vaccine uptake among active adults was low in Hungary. Increased public awareness and improved knowledge about influenza vaccination and/or influenza disease is necessary to achieve higher influenza vaccination uptake rates. Based on the insufficient knowledge of participants concerning the effectiveness and safety of the influenza vaccine, combined with the level of acceptance among participants to obtain an influenza vaccination from a pharmacist, we recommend that both the educational role played by pharmacists should be extended, while vaccine administrator role should be considered and implemented.
Acknowledgements
We are grateful for the contribution of all those who participated in this study.
Abbreviations
- GP
General practitioner
- HCW
Healthcare worker
- USA
United States of America
- WHO
World Health Organization
Authors’ contributions
GFG: Formal analysis, writing original draft, interpretation and revise, editing; MM: Conceptualization, methodology, interpretation and revise, supervision; NM: Investigation, analysis, PD: design, interpretation and revise; KS: interpretation, revise and editing; ZE: investigation, interpretation and revise; RB: conceptualization, methodology, interpretation and revise, editing and supervision. All authors have read and approved the final manuscript.
Funding
The research project had no funding from any organizations. The manuscript publication was funded by University of Szeged Open Access Fund (grant number: 4597). This funding enable open access publication but has no role/influence on study design, data collection, −analysis and -interpretation and manuscript writing.
Availability of data and materials
Data will be made available on request from the corresponding author.
Declarations
Ethics approval and consent to participate
The National Medical Research Council (NMRC) was contacted and they confirmed that this study did not require ethics approval. Participants were informed the aims of the questionnaire and were asked to start filling-out the online questionnaire only if they consent to their anonymous participation (i.e. consent to participate was implied upon filling out and submitting the questionnaire).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO) Influenza (Seasonal) 2019. [Google Scholar]
- 2.European Centre for Disease Prevention and Control (ECDC) Vaccination recommendations and coverage rates in the EU Member States for eight influenza seasons 2007–2008 to 2014–2015. 2017. ECDC Technical Report: Seasonal influenza vaccination in Europe. [Google Scholar]
- 3.Cassini L, Colzani E, Pini A, Mangen M-JJ, Plass D, McDonald SA, et al. Impact of infectious diseases on population health using incidence-based disability-adjusted life years (DALYs): results from the burden of communicable diseases in Europe study, European Union and European economic countries, 2009 to 2013. Eurosurveillance. 2018;23(16):17–454. doi: 10.2807/1560-7917.ES.2018.23.16.17-00454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.European Centre for Disease Prevention and Control (ECDC) Key Facts about Influenza (Flu) & Flu Vaccine. Seas Influ. 2019. [Google Scholar]
- 5.Medlock J, Galvani AP. Optimizing Influenza Vaccine Distribution. Science. 2009;325(5948):1705–1709. doi: 10.1126/science.1175570. [DOI] [PubMed] [Google Scholar]
- 6.Knipl DH, Röost G. Modelling the strategies for age Spesific vaccination scheduling during influenza pandemic outbreaks. Math Biosci Eng. 2011;8(1):123–139. doi: 10.3934/mbe.2011.8.123. [DOI] [PubMed] [Google Scholar]
- 7.Aw D, Silva AB, Palmer DB. Immunosenescence: emerging challenges for an ageing population. Immunology. 2007;120(4):435–446. doi: 10.1111/j.1365-2567.2007.02555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmid P, Rauber D, Betsch C, Lidolt G, Denker L. Barriers of Influenza Vaccination Intention and Behavior – A Systematic Review of Influenza Vaccine Hesitancy , 2005–2016. PLoS One. 2017;12(1):2005–2016. doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yuen CYS, Tarrant M. Determinants of uptake of influenza vaccination among pregnant women – a systematic review. Vaccine. 2014;32(36):4602–4613. doi: 10.1016/j.vaccine.2014.06.067. [DOI] [PubMed] [Google Scholar]
- 10.Endrich MM, Blank PR, Szucs TD. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine. 2009;27(30):4018–4024. doi: 10.1016/j.vaccine.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 11.Rizzo C, Rezza G, Ricciardi W. Strategies in recommending influenza vaccination in Europe and US. Hum Vaccin Immunother. 2018;14(3):693–698. doi: 10.1080/21645515.2017.1367463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atkins K, Van Hoek AJ, Watson C, Baguelin M, Choga L, Patel A, et al. Seasonal influenza vaccination delivery through community pharmacists in England: evaluation of the London pilot. BMJ Open. 2016;6(2):1–11. doi: 10.1136/bmjopen-2015-009739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Pharmaceutical Group of the European Union (PGEU) European Union Communicable Diseases and Vaccination. 2019. [Google Scholar]
- 14.International Pharmaceutical Federation (FIP) An overview of pharmacy’s impact on immunisation coverage: a global survey. The Hague: International Pharmaceutical Federation; 2020. [Google Scholar]
- 15.Isenor JE, Edwards NT, Alia TA, Slayter KL, MacDougall DM, McNeil SA, et al. Impact of pharmacists as immunizers on vaccination rates: a systematic review and meta-analysis. Vaccine. 2016;34(47):5708–5723. doi: 10.1016/j.vaccine.2016.08.085. [DOI] [PubMed] [Google Scholar]
- 16.International Pharmaceutical Federation (FIP) Joint FIP/WHO guidelines on good pharmacy practice standards for quality of pharmacy services. 2011. [Google Scholar]
- 17.Forecast of Facebook user numbers in Hungary from 2017 to 2025 n.d. https://www.statista.com/statistics/568794/forecast-of-facebook-user-numbers-in-hungary/ (accessed January 15, 2018).
- 18.Ogston SA, Lemeshow S, Hosmer DW, Klar J, Lwanga SK. Adequacy of sample size in health studies. West Sussex: Wiley; 1991. [Google Scholar]
- 19.Emberi Erőforrások Minisztériuma (EMMI). EMMI módszertani levele a 2018. évi védőoltásokról 2018:1–44. https://www.antsz.hu/data/cms84807/EMMI_VML2018_kozlony.pdf (accessed July 20, 2019).
- 20.Güvenç IA, Parıldar H, Şahin MK, Erbek SS. Better knowledge and regular vaccination practices correlate well with higher seasonal influenza vaccine uptake in people at risk: promising survey results from a university outpatient clinic. Am J Infect Control. 2017;45(7):740–745. doi: 10.1016/j.ajic.2017.02.041. [DOI] [PubMed] [Google Scholar]
- 21.Alqahtani AS, Althobaity HM, Al Aboud D, Abdel-Moneim AS. Knowledge and attitudes of Saudi populations regarding seasonal influenza vaccination. J Infect Public Health. 2017;10(6):897–900. doi: 10.1016/j.jiph.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 22.Haridi HK, Salman KA, Basaif EA, Al-Skaibi DK. Influenza vaccine uptake, determinants, motivators, and barriers of the vaccine receipt among healthcare workers in a tertiary care hospital in Saudi Arabia. J Hosp Infect. 2017;96(3):268–275. doi: 10.1016/j.jhin.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Bof de Andrade F, Sayuri Sato AP, Moura RF, Ferreira Antunes JL. Correlates of influenza vaccine uptake among community-dwelling older adults in Brazil. Hum Vaccines Immunother. 2017;13(1):103–110. doi: 10.1080/21645515.2016.1228501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.European Centre for Disease Prevention and Control (ECDC) Seasonal influenza vaccination and antiviral use in EU/EEA Member States. 2018. [Google Scholar]
- 25.Tessier E, Warburton F, Tsang C, Rafeeq S, Boddington N, Sinnathamby M, Pebody R Population-level factors predicting variation in influenza vaccine uptake among adults and young children in England , 2015 / 16 and 2016 / 17. Vaccine 2019;36:3231–3238. https://doi.org/10.1016/j.vaccine.2018.04.074, 23. [DOI] [PubMed]
- 26.Dyda A, Karki S, Hayen A, Macintyre CR, Menzies R, Banks E, et al. Influenza and pneumococcal vaccination in Australian adults : a systematic review of coverage and factors associated with uptake. BMC Infect Dis. 2016;16(1):1–15. doi: 10.1186/s12879-016-1820-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yeung S, Lam FLY, Coker R. Factors associated with the uptake of seasonal influenza vaccination in adults : a systematic review. J Public Health (Oxf) 2016;38:746–753. doi: 10.1093/pubmed/fdv194. [DOI] [PubMed] [Google Scholar]
- 28.Han YKJ, Michie S, Potts HWW, Rubin GJ. Predictors of influenza vaccine uptake during the 2009/10 influenza a H1N1v ('swine flu’) pandemic: results from five national surveys in the United Kingdom. Prev Med (Baltim) 2016;84:57–61. doi: 10.1016/j.ypmed.2015.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoffmann K, Van Bijnen EM, George A, Kutalek R, Jirovsky E, Wojczewski S, et al. Associations between the prevalence of influenza vaccination and patient’s knowledge about antibiotics. BMC Public Health. 2015;15(1):1–9. doi: 10.1186/s12889-015-2297-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bödeker B, Remschmidt C, Schmich P, Wichmann O. Why are older adults and individuals with underlying chronic diseases in Germany not vaccinated against flu ? A population-based study. 2015;15(1):1–10. doi: 10.1186/s12889-015-1970-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eilers R, Krabbe PFM, De Melker HE. Motives of Dutch persons aged 50 years and older to accept vaccination: a qualitative study. BMC Public Health. 2015;15(1):1–10. doi: 10.1186/s12889-015-1825-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klett-Tammen CJ, Krause G, Seefeld L, Ott JJ. Determinants of tetanus, pneumococcal and influenza vaccination in the elderly: a representative cross-sectional study on knowledge, attitude and practice (KAP) BMC Public Health. 2016;16(1):121. doi: 10.1186/s12889-016-2784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective : A systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 34.Lorenc T, Marshall D, Wright K, Sutcliffe K, Sowden A. Seasonal influenza vaccination of healthcare workers: systematic review of qualitative evidence. BMC Health Serv Res. 2017;17(1):1–8. doi: 10.1186/s12913-017-2703-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bonfiglioli R, Vignoli M, Guglielmi D, Depolo M, Violante FS. Getting vaccinated or not getting vaccinated? Different reasons for getting vaccinated against seasonal or pandemic influenza. BMC Public Health. 2013;13(1):1221–1228. doi: 10.1186/1471-2458-13-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thornley T, Alliance WB, Heights T, Weybridge B, Kt S. Benefits of pharmacist-led flu vaccination. Ann Pharm Fr. 2016;75(1):6–11. doi: 10.1016/j.pharma.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 37.Anderson C, Thornley T, Anderson C. Who uses pharmacy for flu vaccinations ? Population profiling through a UK pharmacy chain. Int J Clin Pharm. 2016;38(2):218–222. doi: 10.1007/s11096-016-0255-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.International Pharmaceutical Federation (FIP) An overview of current pharmacy impact on immunisation - A global report. The Hague: International Pharmaceutical Federation. 2016. [Google Scholar]
- 39.Burt S, Hattingh L, Czarniak P. Evaluation of patient satisfaction and experience towards pharmacist - administered vaccination services in Western Australia. Int J Clin Pharm. 2018;40(6):1519–1527. doi: 10.1007/s11096-018-0738-1. [DOI] [PubMed] [Google Scholar]
- 40.Isenor JE, Wagg AC, Bowles SK. Patient experiences with influenza immunizations administered by pharmacists. Hum Vaccines Immunother. 2018;14(3):706–711. doi: 10.1080/21645515.2018.1423930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Poulose S, Cheriyan E, Cheriyan R, Weeratunga D, Adham M. Pharmacist-administered influenza vaccine in a community pharmacy : a patient experience survey. Can Pharm J. 2015;148(2):64–67. doi: 10.1177/1715163515569344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ahmed N, Quinn SC, Hancock GR, Freimuth VS, Jamison A. Social media use and influenza vaccine uptake among white and African American adults. Vaccine. 2018;36(49):7556–7561. doi: 10.1016/j.vaccine.2018.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Faasse K, Chatman CJ, Martin LR. A comparison of language use in pro- and anti-vaccination comments in response to a high profile Facebook post. Vaccine. 2016;34(47):5808–5814. doi: 10.1016/j.vaccine.2016.09.029. [DOI] [PubMed] [Google Scholar]
- 44.Schmidt AL, Zollo F, Scala A, Betsch C, Quattrociocchi W. Polarization of the vaccination debate on Facebook. Vaccine. 2018;36(25):3606–3612. doi: 10.1016/j.vaccine.2018.05.040. [DOI] [PubMed] [Google Scholar]
- 45.Smith N, Graham T. Mapping the anti-vaccination movement on Facebook. Inf Commun Soc. 2019;22(9):1310–1327. doi: 10.1080/1369118X.2017.1418406. [DOI] [Google Scholar]
- 46.European Commission, World Health Organization . Global Vaccination Summit. 2019. pp. 1–3. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request from the corresponding author.