Abstract
Social anxiety (SA) is implicated in problematic undergraduate drinking. Brief motivational interventions (BMIs) reduce problematic undergraduate drinking. However, not all students benefit. Identification of vulnerable subgroups is an important next step. The current study examined the role of SA and protective behavioral strategies (PBS) on BMI outcomes. We reanalyzed a subset of data (53.3%; N = 120; 62.5% male) from a randomized trial in which heavy drinking undergraduates were randomized to a BMI or control. SA, past-month typical drinks, peak drinks, weekly quantity, alcohol problems, and PBS were assessed at baseline and 6-weeks. Main effects and interaction among the intervention condition (BMI vs. control) and SA group (low vs. high) were tested on alcohol outcomes and PBS. High SA undergraduates reported greater baseline drinking, more alcohol problems, and lower PBS. Post-BMI, high SA drinkers continued to report greater peak drinks, typical drinks, alcohol problems, and lower PBS use, controlling for baseline use. Among the BMI condition, parallel multiple mediation analyses revealed the PBS subscale Manner of Drinking uniquely mediated the relationship between SA and heavier post-BMI drinking. The PBS Manner of Drinking and Serious Harm Reduction subscales jointly mediated the relationship between SA and greater post-BMI alcohol problems. BMIs may need to be refined to improve outcomes for socially anxious drinkers. Increasing PBS utilization post-BMI may help improve BMI efficacy in this vulnerable group. Clinical implications are discussed.
Keywords: brief motivational intervention, college student alcohol intervention, social anxiety, protective behavioral strategies, treatment mediator
Problematic College Drinking
Undergraduate heavy drinking remains a public health concern in the United States. Epidemiological data suggest over 30% of undergraduates drink heavily (i.e., consuming 5 or more drinks in a row) and more than 12% endorse extreme heavy episodic drinking (i.e., consuming 10 or more drinks in a row; Schulenberg, et al., 2017). Students who engage in heavy drinking report poorer health (e.g., more physical and mental health problems, poor sleep quality), lower academic achievements, greater alcohol-related problems (e.g., assault or unwanted sexual encounters), more frequent risky behavior (e.g., driving after drinking, fights, unprotected sex), and problems with law enforcement (Barnett, Goldstein, Murphy, Colby & Monti, 2006; Barnett, et al., 2004; Hingson, Zha & Smyth, 2017; Wechsler, 1994; Wechsler, Dowdall, Maenner, Gledhill-Hoyt & Lee, 1998). Unfortunately, most at-risk heavy drinking students are not detected until their drinking results in problems with their physical health or as a result of community law enforcement or campus police (Barnett & Read, 2005; Lenk, Erickson, Winters, Nelson & Toomey, 2012). Therefore, colleges and universities continue to play a critical role in the detection and prevention of heavy and problematic drinking.
The Brief Motivational Intervention (BMI)
Over the past decade, a greater number of colleges and universities have offered interventions for risky alcohol use on campus for students who are caught for drinking as well as for those students who are referred by health professionals or self-refer via student health (Lenk, et al., 2012; Nelson, Toomey, Lenk, Erickson & Winters, 2010). Some universities offer motivational enhancement interventions such as a BMI, which focuses on increasing motivation for behavior change (i.e., reduced drinking) following a harm-reduction approach (Marlatt, Baer & Larimer, 1995). Most BMIs include personalized feedback on the participant’s drinking habits, psychoeducation about alcohol and its effects, normative drinking behaviour among peers, and harm-reduction strategies (Dimeff, Baer, Kivlahan & Marlatt, 1999). Several meta-analyses and review articles suggest that BMIs are associated with decreased drinking, lower alcohol problems or both (Carey, Henson, Carey & Maisto, 2007; Carey, Scott-Sheldon, Elliott, Garey & Carey, 2012; Hennessy, Tanner-Smith, Mavridis & Grant, 2019; Larimer & Cronce, 2002, 2007; Samson & Tanner-Smith, 2015; Tanner-Smith & Lipsey, 2015).
BMI Limitations
Despite the empirical support in favour of BMIs to reduce heavy drinking and alcohol problems, variability in outcomes exist. Among undergraduates, heavy drinkers with more significant co-occurring mental health issues, such as depression or social anxiety, do not appear to benefit as much from BMI-style treatments as do their peers (Boniface, et al., 2017; Geisner, Varvil-Weld, Mittmann, Mallett & Turrisi, 2015; Merrill, Reid, Carey & Carey, 2014; Sullivan, Fiellin & O’Connor, 2005; Terlecki, Buckner, Larimer & Copeland, 2011). As such, students with comorbid alcohol and mental health issues may continue to drink heavily or experience greater alcohol-problems even after receiving the recommended treatment (Boniface, et al., 2017; Geisner, et al., 2015; Merrill, et al., 2014; Sullivan, et al., 2005; Terlecki, et al., 2011). This finding is concerning because alcohol use disorders frequently co-occur with other mental health disorders such as anxiety, social anxiety, and depression (Grant, et al., 2015) and are prevalent among college-aged samples (Eisenberg, Gollust, Golberstein & Hefner, 2007; Hunt & Eisenberg, 2010; Zivin, Eisenberg, Gollust & Golberstein, 2009). Identification of individual differences variables such as co-morbid mental health issues that contribute to poorer BMI responses are important next steps to refine existing treatments and improve outcomes among vulnerable students.
Social Anxiety and Problematic College Drinking
Social anxiety is one key mental health variable that appears to be particularly relevant in college drinking models (Ham & Hope, 2005, 2006) and has been largely understudied in relation to BMI outcomes. At clinical levels, social anxiety disorder (SAD) is characterized by intense or persistent fears or avoidance of social scrutiny and/or social interactions (American Psychiatric Association, 2013). Social anxiety symptoms tend to onset prior to alcohol use disorder symptoms (Buckner, Timpano, Zvolensky, Sachs-Ericsson & Schmidt, 2008). Individuals diagnosed with SAD are four times more likely to develop a lifetime alcohol use disorder (Buckner, Schmidt, et al., 2008; Kushner, Abrams & Borchardt, 2000). The college environment may further exacerbate the social anxiety and problematic drinking relationship given that undergraduates may experience elevated social anxiety due to more frequent social anxiety-provoking social situations such as meeting new people, roommates, etc. (Spokas & Heimberg, 2009). The college drinking environment may also support heavy drinking as a means to ‘fit in’ (Litt, Stock & Lewis, 2012), to cope with social anxiety, or in an effort to conform to perceived drinking practices to avoid social scrutiny (Buckner, Eggleston & Schmidt, 2006; Buckner & Shah, 2015; Ham, Bonin & Hope, 2007).
Research consistently shows that undergraduates with elevated social anxiety report greater alcohol problems relative to their peers with more normative levels of social anxiety (for review see, Buckner, Heimberg, Ecker & Vinci, 2013). Although the mechanism underlying the social anxiety and drinking problems relation is unclear, it appears to be mediated by a range of psychosocial variables including greater susceptibility to perceived normative drinking behavior (Buckner, Ecker & Proctor, 2011; Neighbors, et al., 2007; Terlecki, Buckner, Larimer & Copeland, 2012), stronger drinking motives to cope with anxiety and/or to conform to perceived normative drinking practices to avoid social scrutiny (Buckner, Eggleston, et al., 2006; Buckner & Shah, 2015; Ham, et al., 2007; Ham, Zamboanga, Bacon & Garcia, 2009; Norberg, Norton, Olivier & Zvolensky, 2010; Terlecki & Buckner, 2015), and greater alcohol expectancies (Ham, 2009; Ham, Bacon, Carrigan, Zamboanga & Casner, 2016). Students with elevated social anxiety may drink more in certain settings than those without social anxiety, such as more frequent ‘pre-gaming’ or drinking before going out (Buckner, Lewis, Terlecki, Albery & Moss, 2020; Keough, Battista, O’Connor, Sherry & Stewart, 2016). Such pre-drinking may attenuate physical or cognitive symptoms of social anxiety in anticipation of the social event. Heavy drinking before a social event may render at-risk socially anxious drinkers vulnerable to heavy episodic drinking and higher blood alcohol levels, which may result in more alcohol problems. Further, socially anxious drinkers appear to drink heavily in different settings compared to those with normative social anxiety, particularly when alone (Buckner & Terlecki, 2016) such as before going out (Buckner, et al., 2020; Keough, et al., 2016), when alone to cope with negative emotions, and in intimate settings (Terlecki, Ecker & Buckner, 2014).
The relationship between social anxiety and drinking quantity is less clear. Some studies report that social anxiety is associated with greater drinking quantity (Neighbors, et al., 2007; Stewart, Morris, Mellings & Komar, 2006; Terlecki, et al., 2011). Yet, other studies have found social anxiety is associated with lower drinking quantity (Ham & Hope, 2005; Meade Eggleston, Woolaway-Bickel & Schmidt, 2004) and some studies have found no relationship (e.g., Bruch, Heimberg, Harvey & McCann, 1992; Bruch, Rivet, Heimberg & Levin, 1997; Buckner, et al., 2011; Buckner, Mallott, Schmidt & Taylor, 2006; Ham & Hope, 2006; O’Grady, Cullum, Armeli & Tennan, 2011). This inconsistent social anxiety and drinking quantity relation may exist because not all individuals with social anxiety drink alcohol more heavily or frequently as a rule. In fact, some socially anxious individuals may choose to avoid alcohol and social events where alcohol is served altogether (Meade Eggleston, et al., 2004). However, individuals with social anxiety who choose to drink remain vulnerable to problematic drinking, and understanding why this relation occurs is an important next step in this line of research.
Protective Behavioral Strategies
Protective behavioural strategies (PBS) are cognitive and behavioral strategies to decrease heavy alcohol use and alcohol problems using cognitive and behavioral techniques (Martens, et al., 2005). PBS include strategies related to behavioral self-control around alcohol (e.g., avoiding drinking games), alcohol control (e.g., consuming non-alcoholic drinks) and alcohol-reduction strategies (e.g., limiting the number of alcoholic drinks). PBS also include methods to reduce alcohol-related harms (e.g., using a designated driver; Martens, et al., 2005). Among undergraduates, greater PBS use results in less drinking and fewer alcohol problems (Araas & Adams, 2008; D’Lima, Pearson & Kelley, 2012; Labrie, Lac, Kenney & Mirza, 2011; Pearson, D’Lima & Kelley, 2013; Ray, Turrisi, Abar & Peters, 2009). BMI-style interventions generally include a PBS component as a means to increase awareness and use of potential strategies to reduce alcohol-related harm (Dimeff, et al., 1999; Kypri, et al., 2009). Post-intervention PBS mediates the effect of BMI-style interventions, suggesting that undergraduates who reported greater PBS use after treatment showed greater treatment gains (Barnett, Murphy, Colby & Monti, 2007; Larimer, et al., 2007; Murphy, et al., 2012). Taken together, PBS appears to be an ‘active ingredient’ in BMI-style interventions and is considered robust as a stand-alone intervention (Martens, Smith & Murphy, 2013).
PBS and Drinking among Undergraduates with Poorer Mental Health
Unfortunately, not all undergraduates can effectively implement PBS. This finding may help explain why individuals with poorer mental health remain vulnerable to not fully benefitting from BMI-style interventions with a dedicated PBS component. Among undergraduate samples, PBS use has been found to mediate (LaBrie, Kenney & Lac, 2010; LaBrie, Kenney, Lac, Garcia & Ferraiolo, 2009; Linden, Lau-Barraco & Milletich, 2013), partially mediate (Martens, Neighbors, et al., 2008), and moderate (Merrill, et al., 2014) the relationship between alcohol-related problems and mental health conditions such as depression (Martens, Martin, et al., 2008; Merrill, et al., 2014), general negative affect/poorer mental health (LaBrie, et al., 2010; LaBrie, et al., 2009), and anxiety (Linden, et al., 2013). This relationship also extends to social anxiety, such that those with higher social anxiety appear to underutilize PBS (Terlecki, Ecker & Buckner, 2019). Research shows that PBS underutilization mediates the relationship between social anxiety and greater alcohol problems, such that lower PBS use is associated with more problematic drinking (Terlecki, et al., 2019; Villarosa-Hurlocker, Madson, Mohn, Zeigler-Hill & Nicholson, 2018; Villarosa, Moorer, Madson, Zeigler-Hill & Noble, 2014). Therefore, BMI-style interventions with a PBS component may be insufficient for students with co-morbid mental health issues who might struggle with PBS implementation post-treatment. Among those with social anxiety disorder, there may be diagnosis-related symptoms (e.g., fears of social interactions or scrutiny) rendering PBS especially difficult to apply post-treatment. For example, if new PBS strategies are feared to result in social scrutiny or ridicule (e.g., drinking a non-alcoholic drink) or involve feared social interactions (e.g., declining participating in drinking games), the individual may avoid using such strategies and remain vulnerable to alcohol-related harm. Yet, there appears to be a relative lack of attention on this subject in the literature.
An important next step in BMI treatment outcome research is to identify whether socially anxious drinkers are vulnerable to underutilizing PBS post-treatment, and whether a post-treatment deficit can explain why socially anxious drinkers remain susceptible to experiencing greater alcohol problems. Our pilot data suggests that undergraduates with high social anxiety do not fully benefit from a BMI and continue to report both elevated drinking and greater alcohol problems after treatment (Terlecki, et al., 2011) and this outcome may be related to PBS underutilization. Furthermore, highly socially anxious drinkers are more likely to come in contact with university or community staff for problematic drinking (Buckner, et al., 2013), and early intervention protocols might not be as effective for this vulnerable group.
The Current Study
The current study sought to elucidate the interrelationship of problematic undergraduate drinking, social anxiety, PBS, and brief motivational intervention outcomes in several ways. Specifically, we sought to: (1) replicate pilot study findings that high social anxiety (HSA) drinkers do not benefit as much from a BMI relative to their low social anxiety (LSA) counterparts (Terlecki, et al., 2011); and extend those findings by (2) evaluating whether poorer BMI outcomes among the HSA group could be attributed to lower post-BMI PBS use. We hypothesized that social anxiety group would affect treatment outcomes, such that the HSA BMI group would not benefit as much from treatment relative to the LSA BMI group. Among the HSA BMI sample, we hypothesized that PBS use would mediate the relationship between social anxiety and alcohol treatment outcomes, such that HSA participants who reported lower PBS use would also report greater drinking and more alcohol problems post-treatment. The mediation models were designed to test the Protective Behavioral Strategies Survey (PBSS; Martens, et al., 2005) subscales as multiple parallel mediators to determine if HSA drinkers are vulnerable to underutilizing particular PBS.
METHOD
Participants
Participants were heavy drinking undergraduates aged 18 to 24 recruited to participate in a larger brief motivational intervention study (Terlecki, Buckner, Larimer & Copeland, 2015) at a large public university in the southern United States. The original trial inclusion criteria was: (1) drinking more than 5 drinks per occasion (4 drinks for women); (2) reporting at least three alcohol problems on three or more occasions in the past three years on the Rutgers Alcohol Problem Inventory (White & Labouvie, 1989), which is indicative of problematic drinking; (3) scoring six or greater on the Alcohol Use Disorder Identification Test (AUDIT; Saunders, Aasland, Babor & de la Fuente, 1993), which is indicative of risky drinking. The original treatment outcome study design included random assignment to a BMI-style intervention, which includes a PBS component, or to an assessment only control group. All study procedures were approved by the University Institutional Review Board. All participants provided informed consent prior to data collection.
The sub-sample for the planned secondary analysis reported herein was selected from the larger analytic sample (N = 225) and included students who completed the baseline, additional baseline social anxiety measures, and the 6-week post-test. This sub-sample was not recruited based on social anxiety characteristics. To increase generalizability to those with clinical levels of social anxiety, an empirically supported and validated clinical cut-off score was employed. Participants who scored at or above the clinical cut-off scores of 34 on the Social Interaction Anxiety Scale (SIAS) and Social Phobia Scale (SPS; Brown, et al., 1997; Mattick & Clarke, 1998) were pooled into a high social anxiety group (HSA; n = 49). The SIAS and SPS companion measures were used assess the primary presenting symptoms of social anxiety disorder including fears and anxiety related to social interaction (SIAS) and fears of being scrutinized by others (SPS). To compare HSA participants to those with more normative levels of social anxiety, a second group was created for those scoring one standard deviation below the community mean on both the SIAS and SPS (Brown, et al., 1997; Mattick & Clarke, 1998), which comprised the low social anxiety group (LSA; n = 71).
The sub-sample reported herein (N = 120; BMI, n = 63; control, n = 57) had a mean age of 20.28 years (SD = 1.59) and was 62.5% male. The racial/ethnic composition was 82.5% Non-Hispanic Caucasian, 10.0% Hispanic Caucasian, 4.2% non-Hispanic African American, 2.5% Asian American, and 0.8% “other”. About half (53.3%) volunteered to participate via the university’s research participation pool and 46.7% were referred from the university’s Office of Judicial Affairs following an alcohol policy violation.
Procedures
Baseline Assessment.
Participants met individually with the study interventionist to complete consent forms. Participants were provided with a secure link to online self-report measures (www.hostedsurvey.com). Eligible participants were randomized to study condition after baseline assessment. Study interventionists were blind to study condition until the baseline assessment was completed.
Intervention.
The BMI group was conducted as per the Brief Alcohol Screening and Intervention for College Students (BASICS) manual (Dimeff, et al., 1999). BMI participants were asked to monitor their drinking during the two-week period between baseline and BMI. Paper-based drinking monitoring cards were provided and returned to researchers just prior to the feedback interview and included as intervention content. The BMI group received an in-person feedback interview two weeks after completing the baseline assessment. The 50-minute in-person BMI included written personalized feedback for each participant using self-reported baseline data and drinking monitoring card data. The intervention included a PBS component. The feedback form was used to elicit an open-ended conversation about the participant’s self-reported drinking behavior and self-reported PBS use including suggestions for how to decrease drinking and increase PBS use. For example, participants were prompted to identify PBS that they were likely to use and additional strategies that would be helpful or useful. This content was then integrated into the motivational intervention to help build confidence and motivation for using such PBS strategies. BMI participants were provided with a take home leaflet of PBS strategies to consider for future use. The strategies were derived from the PBSS measure.
The control group completed the baseline assessment and did not receive any feedback regarding their drinking behaviour until after the 6-week post-test.
Post-test assessment.
Participants completed online post-test measures 6-weeks after completing baseline assessments.
Measures
Participants completed online self-assessment measures including demographic information (age, gender, ethnicity, Greek-system involvement), alcohol use, alcohol problems, social anxiety, and PBS online at baseline and again at a 6-week post-test assessment.
Alcohol use.
The Daily Drinking Questionnaire (DDQ; Collins, Parks & Marlatt, 1985) assessed average past-month weekly drinking frequency and drinking quantity. Using a 7-day grid, students were asked to self-report the typical number of drinks consumed each day during a typical week (weekly quantity) and the number of typical drinking days (weekly frequency) over the past month.
The Quantity/Frequency Index (QFI; Dimeff, et al., 1999) assessed average alcohol consumption on typical (typical drinks) and heavy drinking (peak drinks) occasions during the past month. Each item is scored 1 (0 drink), 2 (1–2 drinks), 3 (3–4 drinks), 4 (5–6 drinks), and so on through 11 (more than 19 drinks). Alcohol use measures were administered at baseline and the 6-week post-test.
Alcohol-related problems.
Past-month alcohol problems were assessed with the past-month version of the 23-item Rutgers Alcohol Problems Index (RAPI; White & Labouvie, 1989). Both the original and the past-month versions of the RAPI have demonstrated adequate psychometric properties (Buckner, Eggleston, et al., 2006; White & Labouvie, 1989). Each item is scored on a Likert scale ranging from 0 (never) to 4 (more than 10 times), with a maximum score of 92. In our sample, the RAPI demonstrated good internal consistency (α =.87).
Protective Strategies.
The Protective Behavioral Strategies Survey (Martens, et al., 2005) measured cognitive and behavioral strategies used to prevent harms associated with heavy drinking using a total score and also across three distinct subscales: stopping/limiting drinking (e.g., stopping drinking at a certain time), manner of drinking (e.g., avoid gulping or chugging); and serious harm reduction (e.g., using a designated driver). The PBSS demonstrated acceptable internal consistency in the current sample for total use (α = .79), Stopping/Liming (α = .79), Manner of Drinking (α = .76), and Serious Harm Reduction (α = .71). The PBSS was administered at baseline and the 6-week post-test.
Social Anxiety.
The SPS and SIAS (Mattick & Clarke, 1998) assessed baseline social anxiety. Each measure included 20 items scored on a 5-point Likert scale ranging from 0 (not at all characteristic or true of me) to 4 (extremely characteristic or true of me). Total scores on both the SIAS and SPS range from 0 to 60, with clinical cut-off scores at or exceeding 34 (Mattick & Clarke, 1998). These measures have good internal consistency across community and student samples (Heimberg, Mueller, Holt, Hope & Liebowitz, 1992; Mattick & Clarke, 1998; Weeks, et al., 2005) and demonstrate specificity for social anxiety (Brown, et al., 1997). In the current sample, the internal consistencies of the SIAS (α = .90), SPS (α = .92), and the combined SIAS-SPS (α = .91) were excellent.
RESULTS
Sample Characteristics
Means and standard deviations of descriptive variables (Table 1) and outcome variables at baseline and post-test are presented by group (Table 2). There were no observed demographic differences by study group (see Table 1). Referral group served as a co-variate in all analyses to control for any confounding influence.
Table 1.
Baseline significance tests of participant demographics by condition, social anxiety group, and the condition by group interaction
| BMI Condition | Control Condition | Significance tests | |||||
|---|---|---|---|---|---|---|---|
| Variable | LSA (n = 33) | HSA (n = 30) | LSA (n = 38) | HSA (n = 19) | Condition F/χ2 | SA F/χ2 | Condition*SA F/χ2 |
| Demographic variables | |||||||
| Age (years) | 20.12 (1.29) | 20.27 (1.68) | 20.34 (1.60) | 20.68 (1.92) | 1.120 | 0.653 | 0.106 |
| Referral (% volunteer) | 19 (57.6%) | 15 (50.0%) | 17 (44.7%) | 13 (68.4%) | 0.515 | 0.306 | 0.326 |
| Gender (% male) | 22 (66.7%) | 18 (60.0%) | 23 (60.5%) | 12 (63.2%) | 0.481 | 0.480 | 0.475 |
| Greek (% member) | 10 (30.3%) | 11 (36.7%) | 15 (39.5%) | 8 (42.1%) | 0.821 | 0.567 | 0.822 |
| Race (% White) | 26 (78.8%) | 26 (86.7%) | 31 (82.3%) | 16 (84.2%) | 0.122 | 0.170 | 0.157 |
Notes. N = 120. BMI = Brief Motivational Intervention. LSA = low social anxiety group. HSA = high social anxiety group. Values represent either mean scores and standard deviations of continuous variables or within group counts and percentages for categorical variables.
p < .001
p < .01
p < .05.
Table 2.
Means, standard deviations, and results of multivariate analysis of covariance significance tests of baseline and post-test drinking variables and protective strategies scores by condition and social anxiety group
| BMI Condition | Control Condition | Significance tests | |||||
|---|---|---|---|---|---|---|---|
| Variable | LSA (n = 33) | HSA (n = 30) | LSA (n = 38) | HSA (n = 19) | Condition F | SA F | Condition*SA F |
| Social anxiety | 26.61 (14.95) | 64.07 (13.59) | 26.29 (12.27) | 69.05 (11.52) | 0.87 | 262.99*** | 1.67 |
| Drinking variables | |||||||
| Peak drinks | |||||||
| Baseline | 5.36 (1.48) | 6.73 (2.45) | 5.61 (1.98) | 6.16 (1.54) | 0.22 | 7.18** | 2.33 |
| Post-test | 3.55 (1.39) | 4.30 (2.14) | 4.61 (1.82) | 6.21 (1.62) | 19.60*** | 4.11* | 3.45* |
| Typical drinks | |||||||
| Baseline | 3.67 (1.34) | 5.40 (2.36) | 4.21 (1.51) | 4.49 (1.83) | 0.07 | 15.28*** | 3.75* |
| Post-test | 2.55 (0.94) | 3.20 (1.42) | 3.63 (1.48) | 4.37 (1.46) | 15.85*** | 3.88* | 3.40* |
| Drinking frequency | |||||||
| Baseline | 3.88 (0.55) | 4.10 (0.48) | 3.79 (0.78) | 4.05 (0.71) | 0.45 | 3.30ǂ | 0.11 |
| Post-test | 3.09 (0.68) | 3.13 (1.07) | 3.37 (1.00) | 3.51 (0.98) | 7.46** | 2.73ǂ | 2.69ǂ |
| Weekly drinking | |||||||
| Baseline | 14.21 (7.54) | 19.90 (9.07) | 14.53 (7.97) | 18.74 (8.25) | 0.09 | 10.43** | 0.88 |
| Post-test | 8.70 (7.30) | 8.90 (7.97) | 12.00 (8.44) | 15.58 (8.28) | 13.63*** | 0.01 | 4.57* |
| Alcohol problems | |||||||
| Baseline | 11.89 (9.08) | 16.19 (13.28) | 13.74 (9.17) | 16.80 (12.25) | 2.32 | 11.43*** | 5.14* |
| Post-test | 4.21 (4.07) | 7.87 (8.76) | 14.10 (8.43) | 13.53 (11.15) | 19.69*** | 10.03*** | 2.57 |
| Protective Strategies | |||||||
| Stopping/Limiting | |||||||
| Baseline | 18.21 (10.76) | 18.07 (11.99) | 17.13 (8.28) | 16.78 (7.83) | 1.36 | 5.43* | 2.11 |
| Post-test | 20.39 (6.20) | 16.67 (5.74) | 17.18 (3.98) | 16.37 (4.63) | 3.63* | 3.00ǂ | 1.32 |
| Manner of Drinking | |||||||
| Baseline | 18.27 (4.19) | 17.37 (3.98) | 16.32 (3.43) | 15.74 (4.74) | 3.66* | 5.36** | 5.22* |
| Post-test | 19.24 (1.79) | 18.37 (2.33) | 18.53 (2.40) | 16.16 (4.18) | 5.23** | 8.52** | 6.33* |
| Consequences | |||||||
| Baseline | 7.42 (1.92) | 6.27 (2.15) | 6.97 (1.98) | 6.00 (2.56) | 0.79 | 6.99** | 0.05 |
| Post-test | 8.15 (1.79) | 6.40 (2.55) | 7.50 (2.50) | 7.26 (2.70) | 3.01* | 5.44* | 3.04ǂ |
Notes. N = 120. BMI = Brief Motivational Intervention. Values represent means scores and standard deviations. Covariates included gender and referral group. Baseline scores served as additional covariates in post-test analyses.
p < .001
p < .01
p < .05
p < .10
Baseline Analyses
A multivariate analysis of covariance (MANCOVA) was conducted to evaluate baseline group differences among baseline BMI treatment outcome variables (typical drinks, peak drinks, weekly drinking quantity, drinking frequency, and alcohol problems) and baseline PBSS subscale scores (Stopping/Limiting, Manner of Drinking, Serious Harm Reduction) by condition (BMI, control), social anxiety group (LSA, HSA) and the condition*SA group interaction. Covariates included gender and participant referral group. A priori significance was α = .05. The overall baseline MANCOVA was not significant, Wilks’ λ = 1.45, p = .18, partial η2 = .10. No significant baseline main effect of condition was observed, F(8,107) = 1.45, p = .18, partial η2 = .10 (Table 2), indicating successful randomization. However, a significant main effect of social anxiety group was observed, F(8,107) = 3.69, p < .001, partial η2 = .22, such that the HSA group reported significantly more drinking, greater alcohol problems and lower PBSS use at baseline relative to the LSA group (see Table 2).
BMI Treatment Effects
A second multivariate analysis of covariance (MANCOVA) was conducted to evaluate group differences among post-test alcohol outcome variables (typical drinks, peak drinks, weekly drinking quantity, drinking frequency, and alcohol problems) and post-test PBSS subscale scores (PBSS Stopping/Limiting, PBSS Manner of Drinking; PBSS Serious Harm Reduction) by condition (BMI, control), SA group (LSA, HSA) and the condition*SA group interaction. Covariates included baseline alcohol outcomes, baseline protective behavioral strategies, gender and participant referral group. Greek system membership was not related to outcomes (p = .83) and was not employed as a covariate. The overall MANCOVA was significant Wilks’ λ = 5.39, p < .001, partial η2 = .30. Results revealed a significant main effect of condition, F(8,99) = 5.39, p < .001, partial η2 = .30, social anxiety group, F(8,99) = 2.14, p = .039, partial η2 = .15, and a significant condition*SA group interaction, F(8,99) = 2.53, p = .015, partial η2 = .17.
Pairwise tests revealed that participants assigned to the BMI reported significantly lower typical drinks (BMI, M = 2.91; control, M = 3.89, p < .001), peak drinks (BMI, M = 3.87; control, M = 5.38, p < .001), weekly drinks (BMI, M = 8.87; control, M = 13.51, p = .002), alcohol problems (BMI, M = 4.36; control, M = 10.17, p < .001), and greater use of PBSS manner of drinking (BMI, M = 18.50; control, M = 17.65, p = .037), and PBSS Stopping/Limiting (BMI, M = 20.87; control, M = 19.71, p = .041) use relative to the control group. Regarding drinking frequency, there was a trend for the BMI group to drink less frequently relative to controls (BMI, M = 2.53; control, M = 2.92, p = .083), but this effect was not significant. There was no significant treatment effect for PBSS Serious Harm Reduction.
Regardless of treatment condition, pairwise comparisons showed that the HSA group reported significantly greater post-test peak drinking (HSA, M = 4.94; LSA, M = 4.31, p = .048), more alcohol problems (HSA, M = 7.98; LSA, M = 6.51, p = .043), lower PBSS Stopping/Limiting (HSA, M = 19.29; LSA, M = 21.27, p = .024) use, and lower PBSS Manner of Drinking (HSA, M = 17.32; LSA, M = 18.88, p = .003) at post-test relative to the LSA group.
The significant SA*BMI interaction revealed that HSA BMI participants reported greater peak drinks (p = .038), greater typical drinks (p = .035), greater alcohol problems (p = .021) lower PBSS Stopping/Limiting (p = .008), lower PBSS Manner of Drinking (p = .048), use at post-test relative to the LSA BMI group (see Table 2).
Mediation
Bivariate correlations of study variables (see Table 3) among those assigned to the BMI (n = 63) revealed that social anxiety was significantly positively associated with post-test peak drinks, typical drinks, and drinking problems and significantly negatively related to PBSS subscale use. Given that a significant SA*BMI interaction was observed in the treatment outcome analyses (see Table 1) for typical drinking, peak drinking, drinking problems, we tested whether post-treatment protective behavioral strategies subscales mediated the relationship between social anxiety and post-treatment drinking among those receiving the BMI.
Table 3.
Bivariate correlations of social anxiety, alcohol use, alcohol problems, and protective behavioral strategies at baseline and post-test among participants randomized to the BMI
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Social anxiety | - | .217* | .205* | .280** | .099 | .264*** | −.222** | −.438*** | −.226** | −.221** |
| 2. Peak drinks | .235** | - | .760*** | .628*** | .524** | .248** | −.242** | −.260*** | −.261*** | −.228** |
| 3. Typical drinks | .064 | .609*** | - | .722*** | .504*** | .248** | −.383*** | −.324*** | −.308*** | −.274*** |
| 4. Weekly quantity | .147 | .486*** | .526*** | - | .520*** | .185* | −.347*** | −.345*** | −.264*** | −.363*** |
| 5. Drinking frequency | .238** | .292*** | .292*** | .381*** | - | .139 | −.201 | −.177 | −.283*** | −.117 |
| 6. Drinking problems | .318*** | .201* | .208* | .171ǂ | .148 | - | .023 | .037 | −.162 | .014 |
| 7. PBSS total | −.390*** | −.376*** | −.319*** | −.411*** | −.448*** | −.135 | - | .474*** | .417*** | .318*** |
| 8. PBSS Stopping/Limiting | −.205** | −.173ǂ | −.195* | −.272** | −.153 | −.080 | .466*** | - | .379*** | .621*** |
| 9. PBSS Manner of Drinking | −.275** | −.158ǂ | −.188* | −.244** | −.249** | −.043 | .391*** | .515*** | - | .105 |
| 10. PBSS Consequences | −.252** | −.167ǂ | −.120 | −.266** | −.205** | .023 | .325*** | .460*** | .229** | - |
Note. n = 63. BMI = Brief Motivational Intervention. Correlations for baseline variables are presented below the diagonal. Correlations for post-test variables are presented above the diagonal. PBSS = Protective Behavioral Strategies Survey. Social anxiety was assessed at baseline only.
p < .001
p < .01
p < .05
p < .07.
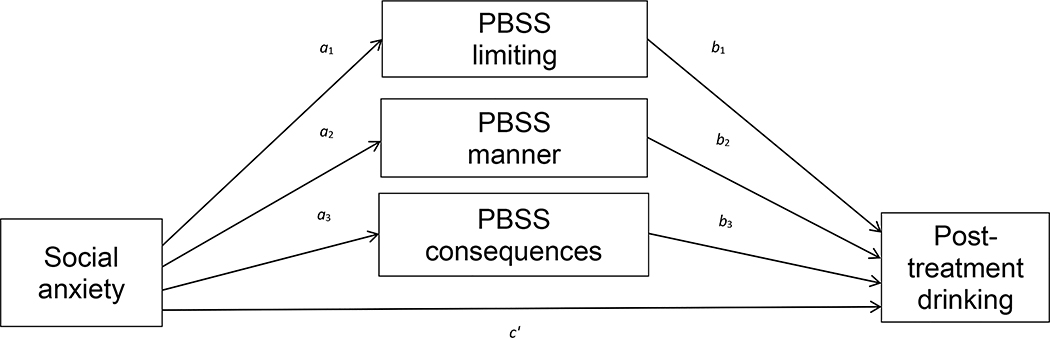
A series of parallel multiple mediator models (see Figure 1) were tested with SPSS 26 using PROCESS macro 3.4, Model 4 (Hayes, 2017). The PROCESS macro tests mediation using an ordinary least squares regression-based model. Effects were estimated using 5,000 bootstrapped samples and standard errors were estimated with 95% confidence intervals for direct and indirect effects. Bootstrapped mediation methods such as PROCESS are now preferred methods of testing mediation (MacKinnon, Fairchild & Fritz, 2007; Williams & MacKinnon, 2008).
Figure 1.
Conceptual diagram of the parallel multiple mediator model for the effect of social anxiety on post-treatment drinking via Protective Behavioural Strategies Scale (PBSS) subscales.
Each parallel multiple mediator model was conducted using a unique post-test alcohol outcome as the dependent variable (i.e., peak drinks, typical drinks, alcohol problems) with gender and referral group as covariates. For each model, continuous social anxiety scores served as the predictor variable and the three PBSS subscales (Stopping/Limiting, Manner of Drinking, and Serious Harm Reduction) served as multiple mediator variables. Regression coefficients, standard errors, and model summary information are presented in Table 4. Results from multiple mediation models indicate that among those assigned to BMI, PBSS Manner of Drinking uniquely mediated the relationship between SA and peak drinking (p = .049) as well as SA and typical drinking (p = .044), whereas PBSS Stopping/Limiting and PBSS Consequences did not significantly mediate these relationships. Among those assigned to BMI, PBSS Serious Negative Consequences (p = .029) and PBSS Manner of Drinking (p = .015) jointly mediated the relationship between SA and alcohol problems, whereas PBSS Stopping/Limiting did not mediate this relation. Table 5 contains estimates of indirect effects and bootstrapped 95% confidence intervals for significant mediation results1.
Table 4.
Regression Coefficients, Standard Errors, and Model Summary Information for Protective Behavioral Strategies Subscales (PBSS) as Parallel Multiple Mediators of the Social Anxiety and Post-Treatment Drinking Relationship
| Consequent | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (PBSS Stopping/Limiting) | M2 (PBSS Manner of Drinking) | M3 (PBSS Consequences) | Y (Alcohol Outcome) | |||||||||||||
| Antecedent | Coeff. | SE | p | Coeff. | SE | p | Coeff. | SE | p | Coeff. | SE | p | ||||
| Peak Drinks | ||||||||||||||||
| X (SA) | a1 | 1.750 | 0.517 | <.001 | a2 | −5.465 | 1.221 | <.001 | a3 | −2.042 | 0.523 | <.001 | c′ | 0.281 | 0.572 | .625 |
| M1 | - | - | - | - | - | - | - | - | - | b1 | 0.096 | 0.070 | .177 | |||
| M2 | - | - | - | - | - | - | - | - | - | b2 | −0.285 | 0.142 | .049 | |||
| M3 | - | - | - | - | - | - | - | - | - | b3 | −0.132 | 0.504 | .334 | |||
| Constant | iM1 | 16.729 | 1.446 | <.001 | iM2 | 21.335 | 3.222 | <.001 | iM3 | 13.548 | 1.381 | <.001 | iY | 7.910 | 2.833 | .007 |
| R2 = 0.201 | R2 = 0.345 | R2 = 0.419 | R2 = 0.255 | |||||||||||||
| F(4,58) = 3.643, p = .010 | F(4,58) = 7.65, p <.001 | F(4,58) = 10.443, p <.001 | F(7,55) = 2.694, p = .018 | |||||||||||||
| Typical Drinks | ||||||||||||||||
| X (SA) | a1 | 1.911 | 0.496 | <.001 | a2 | −5.158 | 1.268 | <.001 | a3 | −2.131 | 0.552 | <.001 | c′ | 0.005 | 0.006 | .393 |
| M1 | - | - | - | - | - | - | - | - | - | b1 | 0.060 | 0.046 | .203 | |||
| M2 | - | - | - | - | - | - | - | - | - | b2 | −0.191 | 0.093 | .044 | |||
| M3 | - | - | - | - | - | - | - | - | - | b3 | −0.112 | 0.092 | .229 | |||
| Constant | iM1 | 17.009 | 1.342 | <.001 | iM2 | 21.073 | 3.102 | <.001 | 13.177 | 1.350 | <.001 | iY | 5.712 | 1.885 | .004 | |
| R2 = 0.266 | R2 = 0.353 | R2 = 0.408 | R2 = 0.302 | |||||||||||||
| F(4,58) = 5.26, p <.001 | F(4,58) = 7.91, p <.001 | F(4,58) = 9.99, p <.001 | F(7,55) = 3.407, p = .004 | |||||||||||||
| Alcohol Problems | ||||||||||||||||
| X (SA) | a1 | 1.509 | 0.509 | .004 | a2 | −5.763 | 1.096 | <.001 | a3 | −2.260 | 0.493 | <.001 | c′ | −2.042 | 1.392 | .148 |
| M1 | - | - | - | - | - | - | - | - | - | b1 | −0.201 | 0.218 | .358 | |||
| M2 | - | - | - | - | - | - | - | - | - | b2 | −0.625 | 0.283 | .029 | |||
| M3 | - | - | - | - | - | - | - | - | - | b3 | −0.974 | 0.395 | .015 | |||
| Constant | iM1 | 17.928 | 1.485 | <.001 | iM2 | 23.872 | 3.315 | <.001 | 13.195 | 1.491 | <.001 | iY | 35.995 | 7.538 | <.001 | |
| R2 = 0.261 | R2 = 0.393 | R2 = 0.405 | R2 = 0.193 | |||||||||||||
| F(4,58) = 5.117, p <.001 | F(4,58) = 9.369, p <.001 | F(4,58) = 9.886, p <.001 | F(7,55) = 4.49, p <.001 | |||||||||||||
Note. n = 63. Covariates include gender, referral group, and baseline measure scores.
Table 5.
Bootstrap estimates, standard errors, and 95% confidence intervals for the indirect effects of social anxiety predicting past-month typical drinks, peak drinks, and alcohol problems
| Coeff. | SE | CI (lower) | CI (upper) | |
|---|---|---|---|---|
| Social anxiety → PBSS Manner of Drinking → Peak drinks | 1.557 | .255 | 1.107 | 2.067 |
| Social anxiety → PBSS Manner of Drinking → Typical drinks | 0.985 | .236 | 0.513 | 1.457 |
| Social anxiety → PBSS Manner of Drinking → Alcohol problems | 3.602 | .296 | 3.010 | 4.194 |
| Social anxiety → PBSS Serious Consequences → Alcohol problems | 2.201 | .264 | 1.673 | 2.729 |
Note. PBSS = Protective Behavioral Strategies Survey. n = 63.
DISCUSSION
The current study evaluated social anxiety as an individual difference variable hypothesized to negatively affect BMI treatment outcomes among heavy drinking undergraduates. PBS underutilization was examined as a mechanism underlying the relationship between social anxiety and poorer BMI outcomes. The HSA group reported significantly more drinking (typical drinks, peak drinks, weekly drinking), more alcohol problems, and lower PBS use relative to the LSA group. These findings support a growing body of literature that social anxiety serves as risk factor for problematic drinking (Torvik, et al., 2019).
Results from the BMI outcome analyses supported the hypothesis that social anxiety would negatively affect BMI treatment outcomes. Specifically, highly socially anxious drinkers who received a BMI did not experience the same treatment outcomes as did their peers with more normative levels of social anxiety, which is consistent with our pilot study findings (Terlecki, et al., 2011). BMI treatment outcome analyses revealed that HSA drinkers continued to engage in heavier post-treatment drinking (typical and peak drinks) and experienced more alcohol problems relative to their peers with more normative levels of social anxiety. Therefore, HSA drinkers who voluntarily seek (or are referred to) a BMI alcohol treatment may continue to drink heavily, experience negative health effects (e.g., liver damage), and other alcohol-related problems such as poor health and lower grades, even after receiving treatment. This outcome is worrying because approximately one-quarter (23%) of individuals seeking alcohol treatment also meet criteria for social anxiety disorder (Thomas, Thevos & Randall, 1999) and social anxiety disorder appears to onset before problematic alcohol use (Buckner, Schmidt, et al., 2008). Similarly, in the present sample, nearly 22% of participants exceeded the clinical cut-off scores on both the SIAS and SPS, suggesting that about one-quarter of individuals who engaged in a BMI for alcohol use were at risk for comorbidity and may continue to experience some level of alcohol-related harms after receiving treatment.
The present study’s second aim was to evaluate PBS underutilization as a mechanism underlying poorer BMI treatment outcomes among HSA drinkers in an effort to improve treatment outcomes. The research has shown that greater PBS use is associated with reduced drinking and fewer alcohol problems among undergraduates (Araas & Adams, 2008; D’Lima, et al., 2012; Labrie, et al., 2011; Patrick, Lee & Larimer, 2011; Ray, et al., 2009). Further research shows that HSA drinkers may underutilize PBS strategies (Terlecki, et al., 2019; Villarosa-Hurlocker, et al., 2018; Villarosa, et al., 2014), which in turn, may render them vulnerable to experiencing more alcohol problems. Given that PBS are considered an ‘active ingredient’ in BMI-style interventions (Martens, et al., 2013) and that greater PBS use are associated with better intervention outcomes (Barnett, et al., 2007; Larimer, et al., 2007; Murphy, et al., 2012), PBS were isolated as a potential mediator in the SA and poorer drinking outcomes relationship.
Results of the parallel mediation models showed that PBSS Manner of Drinking uniquely mediated the relationship between social anxiety and peak and typical drinking (i.e., was the only significant mediator). This finding is consistent with cross-sectional data showing that PBSS Manner of Drinking may be implicated in heavy drinking amongst those with elevated social anxiety (Terlecki, et al., 2019). Specifically, highly socially anxious students who underutilized PBSS Manner of Drinking strategies (e.g., avoiding participating in drinking games, avoiding pre-gaming, avoiding drinking to keep up with others) remained vulnerable to heavier post-treatment drinking (typical drinks and peak drinks). PBSS Manner of Drinking and PBSS Serious Harm Reduction subscales jointly mediated the relationship between social anxiety and greater post-treatment alcohol problems (i.e., both mediators were significant), which is consistent with findings from earlier cross-sectional research that PBSS Serious Harm Reduction mediated the relationship between social anxiety and drinking problems (Villarosa-Hurlocker, et al., 2018; Villarosa, et al., 2014).
Taken together, underutilization of particular PBS strategies may be a key reason why highly socially anxious drinkers remain vulnerable to poorer BMI treatment outcomes. In partial support of this contention, PBS may be used less frequently or less effectively due to competing cognitive demands due to the nature of social anxiety disorder itself such as monitoring of physiological anxiety symptoms (e.g., sweating, blushing), over-attending to social cues (e.g., monitoring for disapproval or social threats), maintaining a self-critical internal dialogue (Clark & McManus, 2002; Clark & Wells, 1995), and avoiding practicing new social skills. Additional alcohol-related cognitive impairment may render PBS even more difficult to effectively implement in certain evaluative social drinking situations (e.g., meeting new people at parties), which is concerning given that high social anxiety drinkers are vulnerable to heavy solitary drinking before they go out (Keough, et al., 2016) and therefore may be too intoxicated to practice or implement new PBS that require social interaction (e.g., drink or drinking games refusal). Socially anxious drinkers who are under the influence of alcohol may also be less willing or less capable of engaging in particular PBS that are feared to result in social scrutiny (e.g., avoid drinking games, avoid drinking to “keep up;” as per the PBSS Manner of Drinking subscale) as opposed to less obvious PBS (e.g., putting extra ice in your drink; as per the PBSS Stopping/Limiting subscale). In summary, high social anxiety drinkers under the influence of alcohol may not possess the additional cognitive resources required to activate novel coping skills in situ and also might avoid using strategies that require practicing new social skills (e.g., refusing drinks or declining drinking games participation) rendering them vulnerable to not effectively using PBS strategies.
Clinical Implications
The present findings have important clinical implications. First, our findings show that socially anxious drinkers do not benefit as much from BMI treatment and continue to underutilize PBS strategies after receiving treatment. Underutilization of a particular type of PBS mediated the relation between social anxiety and both heavier drinking and more problems.
Taken together, these findings suggest BMI protocols with a PBS component may be insufficient and may require adaptation for co-occurring social anxiety and heavy drinking. Our data suggest that PBSS Manner of Drinking items may be particularly salient in the feedback interview, such as avoiding drinking to “keep up with others” and “avoiding pre-gaming”. During the BMI feedback interview, those with elevated social anxiety may require more PBS coverage. For example, participants might be asked to list some acceptable novel PBS strategies while also identifying PBS strategies that they would be reluctant to use, and a discussion of barriers to employing novel PBS. Study interventionists may then use motivational interviewing techniques to help to increase confidence for attempting PBSS Manner of Drinking items via cognitive restructuring and role play. Among those who seem particularly vulnerable to PBS underutilization, offering dedicated PBS follow-ups, group sessions, or ‘booster’ sessions may be beneficial. Alternatively, a brief cognitive behavioral component addressing faulty cognitions about the likelihood of experiencing social ridicule when employing certain PBS strategies (e.g., drinking game refusal) may be helpful. Screening students for social anxiety related symptoms pre-BMI might be useful to further tailor intervention content. Finally, referrals to student mental health or community mental health providers for social anxiety disorder psychotherapy treatment focusing on improved social skills, increasing coping skills, and decreasing cognitive rumination may be beneficial alongside the BMI.
Limitations and Future Directions
The present findings should be interpreted considering the limitations discussed below, which can be used to inform future directions on this important topic. First, the sample was a group of homogenous undergraduates. Our heavy drinking inclusion criteria likely excluded some minority students who have been shown to not drink as heavily as do Caucasian students (O’Malley & Johnston, 2002). Further research is required to test whether these results generalize to more diverse samples, including non-undergraduates. Second, our sample size was somewhat limited and future work would benefit from larger sample sizes. Third, the data consist of retrospective self-report methods. Multi-method (e.g., biological data, ecological momentary assessment) and multi-informant (e.g., collateral or peer reports of participant drinking) methods will be an important next step in this line of research. Fourth, socially anxious participants may have responded to study questionnaires in a socially favourable way, either by underreporting drinking or problems to avoid social scrutiny or not admitting to changing their drinking behaviors post-treatment. Therefore, it may be useful to study this relationship using methods such as ecological momentary assessment to provide a better assessment of when particular PBS are employed and whether or not PBS use had an immediate effect on alcohol use or the experience of alcohol problems. Finally, due to the natural distribution of anxiety characteristics, equal sample sizes were not achieved among MANCOVA group variables, which may have affected the error rate.
Conclusions
Despite these limitations, this study represents an important step in the identification of social anxiety as an individual differences variable that negatively affects BMI treatment outcomes and links those poorer treatment outcomes to PBSS Manner of Drinking underutilization. The study’s findings suggest that highly socially anxious drinkers comprise a group who are not only vulnerable to experiencing greater alcohol problems (for review see, Buckner, et al., 2013), but for whom existing standard BMI treatments may not offer the same benefit relative to peers with more normative social anxiety. As such, these at-risk drinkers may concerningly continue to drink heavily and experience elevated alcohol problems even after receiving treatment, therefore increasing the risk of developing a lifetime alcohol use disorder. Future work is needed to identify ways to help this vulnerable group of students learn to manage their drinking to reduce future alcohol problems during their undergraduate years and beyond.
Acknowledgments
This investigation was supported in part by National Institute on Alcohol Abuse and Alcoholism (NIAAA) Grant F31AA017565. NIAAA had no role in the study design, collection, analysis, or interpretation of the data; the writing of the manuscript; or the decision to submit the paper for publication.
Footnotes
Bootstrap estimates, standard errors, and 95% confidence intervals for the indirect effects of non-significant mediation pathways are available on request.
References
- APA. (2013). The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Association. [Google Scholar]
- Araas TE, & Adams TB (2008). Protective behavioral strategies and negative alcohol-related consequences in college students. Journal of Drug Education, 38(3), 211–224. doi: 10.2190/DE.38.3.b [DOI] [PubMed] [Google Scholar]
- Barnett NP, Goldstein AL, Murphy JG, Colby SM, & Monti PM (2006). “I’ll Never Drink Like That Again”: Characteristics of Alcohol-Related Incidents and Predictors of Motivation to Change in College Students. Journal of Studies on Alcohol, 67(5), 754–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Murphy JG, Colby SM, & Monti PM (2007). Efficacy of counselor vs. computer-delivered intervention with mandated college students. Addictive Behaviors, 32(11), 2529–2548. doi: 10.1016/j.addbeh.2007.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, & Read JP (2005). Mandatory alcohol intervention for alcohol-abusing college students: a systematic review. Journal of Substance Abuse Treatment, 29(2), 147–158. doi: 10.1016/j.jsat.2005.05.007 [DOI] [PubMed] [Google Scholar]
- Barnett NP, et al. (2004). Brief alcohol interventions with mandated or adjudicated college students. Alcoholism: Clinical & Experimental Research, 28(6), 966–975. doi: 10.1097/01.alc.0000128231.97817.c7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boniface S, et al. (2017). The Effect of Brief Interventions for Alcohol Among People with Comorbid Mental Health Conditions: A Systematic Review of Randomized Trials and Narrative Synthesis. Alcohol and Alcoholism, 53(3), 282–293. doi: 10.1093/alcalc/agx111 [DOI] [PubMed] [Google Scholar]
- Brown EJ, et al. (1997). Validation of the Social Interaction Anxiety Scale and the Social Phobia Scale across the anxiety disorders. Psychological Assessment, 9(1), 21–27. doi: 10.1037/1040-3590.9.1.21 [DOI] [Google Scholar]
- Bruch MA, Heimberg RG, Harvey C, & McCann M (1992). Shyness, alcohol expectancies, and alcohol use: Discovery of a suppressor effect. Journal of Research in Personality, 26(2), 137–149. doi: 10.1016/0092-6566(92)90050-e [DOI] [Google Scholar]
- Bruch MA, Rivet KM, Heimberg RG, & Levin MA (1997). Shyness, alcohol expectancies, and drinking behavior: Replication and extension of a suppressor effect. Personality and Individual Differences, 22(2), 193–200. doi: 10.1016/s0191-8869(96)00190-0 [DOI] [Google Scholar]
- Buckner JD, Ecker AH, & Proctor SL (2011). Social anxiety and alcohol problems: The roles of perceived descriptive and injunctive peer norms. Journal of Anxiety Disorders, 25(5), 631–638. doi: 10.1016/j.janxdis.2011.02.003 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Eggleston AM, & Schmidt NB (2006). Social anxiety and problematic alcohol consumption: the mediating role of drinking motives and situations. Behavior Therapy, 37(4), 381–391. doi: 10.1016/j.beth.2006.02.007 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG, Ecker AH, & Vinci C (2013). A biopsychosocial model of social anxiety and substance use. Depression & Anxiety, 30(3), 276–284. doi: 10.1002/da.22032 [DOI] [PubMed] [Google Scholar]
- Buckner JD, Lewis EM, Terlecki MA, Albery IP, & Moss AC (2020). Context-specific drinking and social anxiety: The roles of anticipatory anxiety and post-event processing. Addictive Behaviors, 102, 106184. doi: 10.1016/j.addbeh.2019.106184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Mallott MA, Schmidt NB, & Taylor J (2006). Peer influence and gender differences in problematic cannabis use among individuals with social anxiety. Journal of Anxiety Disorders, 20(8), 1087–1102. doi: 10.1016/j.janxdis.2006.03.002 [DOI] [PubMed] [Google Scholar]
- Buckner JD, et al. (2008). Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. Journal of Psychiatric Research, 42(3), 230–239. doi: 10.1016/j.jpsychires.2007.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, & Shah SM (2015). Fitting in and feeling fine: Conformity and coping motives differentially mediate the relationship between social anxiety and drinking problems for men and women. Addiction Research & Theory, 23(3), 231–237. doi: 10.3109/16066359.2014.978304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, & Terlecki MA (2016). Social anxiety and alcohol-related impairment: The mediational impact of solitary drinking. Addictive Behaviors, 58, 7–11. doi: 10.1016/j.addbeh.2016.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Timpano KR, Zvolensky MJ, Sachs-Ericsson N, & Schmidt NB (2008). Implications of comorbid alcohol dependence among individuals with social anxiety disorder. Depression & Anxiety, 25(12), 1028–1037. doi: 10.1002/da.20442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, & Maisto SA (2007). Which Heavy Drinking College Students Benefit From a Brief Motivational Intervention? Journal of Consulting & Clinical Psychology, 75(4), 663–669. doi: 10.103710022-006x.75.4.663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Elliott JC, Garey L, & Carey MP (2012). Face-to-face versus computer-delivered alcohol interventions for college drinkers: a meta-analytic review, 1998 to 2010. Clinical Psychology Review, 32(8), 690–703. doi: 10.1016/j.cpr.2012.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DM, & McManus F (2002). Information processing in social phobia. Biological Psychiatry, 51(1), 92–100. doi: 10.1016/S0006-3223(01)01296-3 [DOI] [PubMed] [Google Scholar]
- Clark DM, & Wells A (1995). A cognitive model of social anxiety. In Heimberg RG, Leibowitz MR, Hope DA & Schneier FR (Eds.), Social phobia: Diagnosis, assessment, and treatment (pp. 69–93). New York: Guilford Press. [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. doi: 10.1037/0022-006x.53.2.189 [DOI] [PubMed] [Google Scholar]
- D’Lima GM, Pearson MR, & Kelley ML (2012). Protective behavioral strategies as a mediator and moderator of the relationship between self-regulation and alcohol-related consequences in first-year college students. Psychology of Addictive Behaviors, 26(2), 330–337. doi: 10.1037/a0026942 [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan D, & Marlatt GA (1999). Brief Alcohol Screening and Intervention for College Students (BASICS): A harm reduction approach. New York: Guilford Press. [Google Scholar]
- Eisenberg D, Gollust SE, Golberstein E, & Hefner JL (2007). Prevalence and Correlates of Depression, Anxiety, and Suicidality Among University Students. American Journal of Orthopsychiatry, 77(4), 534–542. doi: 10.1037/0002-9432.77.4.534 [DOI] [PubMed] [Google Scholar]
- Geisner IM, Varvil-Weld L, Mittmann AJ, Mallett K, & Turrisi R (2015). Brief web-based intervention for college students with comorbid risky alcohol use and depressed mood: Does it work and for whom? Addictive Behaviors, 42, 36–43. doi: 10.1016/j.addbeh.2014.10.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, et al. (2015). Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions IIIEpidemiology of DSM-5 Alcohol Use DisorderEpidemiology of DSM-5 Alcohol Use Disorder. JAMA Psychiatry, 72(8), 757–766. doi: 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ham LS (2009). Positive Social Alcohol Outcome Expectancies, Social Anxiety, and Hazardous Drinking in College Students. Cognitive Therapy and Research, 33(6), 615–623. doi: 10.1007/s10608-009-9248-8 [DOI] [Google Scholar]
- Ham LS, Bacon AK, Carrigan MH, Zamboanga BL, & Casner HG (2016). Social anxiety and alcohol use: The role of alcohol expectancies about social outcomes. Addiction Research & Theory, 24(1), 9–16. doi: 10.3109/16066359.2015.1036242 [DOI] [Google Scholar]
- Ham LS, Bonin M, & Hope DA (2007). The role of drinking motives in social anxiety and alcohol use. Journal of Anxiety Disorders, 21(8), 991–1003. doi: 10.1016/j.janxdis.2006.10.014 [DOI] [PubMed] [Google Scholar]
- Ham LS, & Hope DA (2005). Incorporating social anxiety into a model of college student problematic drinking. Addictive Behaviors, 30(1), 127–150. doi: 10.1016/j.addbeh.2004.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ham LS, & Hope DA (2006). Incorporating social anxiety into a model of college problem drinking: Replication and extension. Psychology of Addictive Behaviors, 20(3), 348–355. doi: 10.1037/0893-164X.20.3.348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ham LS, Zamboanga BL, Bacon AK, & Garcia TA (2009). Drinking motives as mediators of social anxiety and hazardous drinking among college students. Cognitive Behavior Therapy, 38(3), 133–145. doi: 10.1080/16506070802610889 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. (2nd ed.): Guilford Press. [Google Scholar]
- Heimberg RG, Mueller GP, Holt CS, Hope DA, & Liebowitz MR (1992). Assessment of anxiety in social interaction and being observed by others: The social interaction anxiety scale and the Social Phobia Scale. Behavior Therapy, 23(1), 53–73. doi: 10.1016/s0005-7894(05)80308-9 [DOI] [Google Scholar]
- Hennessy EA, Tanner-Smith EE, Mavridis D, & Grant SP (2019). Comparative Effectiveness of Brief Alcohol Interventions for College Students: Results from a Network Meta-Analysis. Prevention Science, 20(5), 715–740. doi: 10.1007/s11121-018-0960-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R, Zha W, & Smyth D (2017). Magnitude and Trends in Heavy Episodic Drinking, Alcohol-Impaired Driving, and Alcohol-Related Mortality and Overdose Hospitalizations Among Emerging Adults of College Ages 18–24 in the United States, 1998–2014. Journal of Studies on Alcohol and Drugs, 78(4), 540–548. doi: 10.15288/jsad.2017.78.540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt J, & Eisenberg D (2010). Mental Health Problems and Help-Seeking Behavior Among College Students. Journal of Adolescent Health, 46(1), 3–10. doi: 10.1016/j.jadohealth.2009.08.008 [DOI] [PubMed] [Google Scholar]
- Keough MT, Battista SR, O’Connor RM, Sherry SB, & Stewart SH (2016). Getting the party started — Alone: Solitary predrinking mediates the effect of social anxiety on alcohol-related problems. Addictive Behaviors, 55, 19–24. doi: 10.1016/j.addbeh.2015.12.013 [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, & Borchardt C (2000). The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clinical Psychology Review, 20(2), 149–171. doi: 10.1016/s0272-7358(99)00027-6 [DOI] [PubMed] [Google Scholar]
- Kypri K, et al. (2009). Randomized controlled trial of proactive web-based alcohol screening and brief intervention for university students. Archives of Internal Medicine, 169(16), 1508–1514. doi: 10.1001/archinternmed.2009.249 [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, & Lac A (2010). The use of protective behavioral strategies is related to reduced risk in heavy drinking college students with poorer mental and physical health. Journal of Drug Education, 40(4), 361–378. doi: 10.2190/DE.40.4.c [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Lac A, Garcia JA, & Ferraiolo P (2009). Mental and social health impacts the use of protective behavioral strategies in reducing risky drinking and alcohol consequences. Journal of College Student Development, 50(1), 35–49. doi: 10.1353/csd.0.0050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrie JW, Lac A, Kenney SR, & Mirza T (2011). Protective behavioral strategies mediate the effect of drinking motives on alcohol use among heavy drinking college students: Gender and race differences. Addictive Behaviors, 36(4), 354–361. doi: 10.1016/j.addbeh.2010.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, & Cronce JM (2002). Identification, prevention and treatment: a review of individual-focused strategies to reduce problematic alcohol consumption by college students. Journal of Studies on Alcohol(14), 148–163. [DOI] [PubMed] [Google Scholar]
- Larimer ME, & Cronce JM (2007). Identification, prevention, and treatment revisited: individual-focused college drinking prevention strategies 1999–2006. Addictive Behaviors, 32(11), 2439–2468. doi: 10.1016/j.addbeh.2007.05.006 [DOI] [PubMed] [Google Scholar]
- Larimer ME, et al. (2007). Personalized mailed feedback for college drinking prevention: A randomized clinical trial. Journal of Consulting & Clinical Psychology, 75(2), 285–293. doi: 10.1037/0022-006X.75.2.285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenk KM, Erickson DJ, Winters KC, Nelson TF, & Toomey TL (2012). Screening services for alcohol misuse and abuse at four-year colleges in the U.S. Journal of Substance Abuse Treatment, 43(3), 352–358. doi: 10.1016/j.jsat.2012.01.001 [DOI] [PubMed] [Google Scholar]
- Linden AN, Lau-Barraco C, & Milletich RJ (2013). The role of protective behavioral strategies and anxiety in problematic drinking among college students. Journal of Studies on Alcohol Drugs, 74(3), 413–422. doi: 10.15288/jsad.2013.74.413 [DOI] [PubMed] [Google Scholar]
- Litt DM, Stock ML, & Lewis MA (2012). Drinking to Fit in: Examining the Need to Belong as a Moderator of Perceptions of Best Friends’ Alcohol Use and Related Risk Cognitions Among College Students. Basic and Applied Social Psychology, 34(4), 313–321. doi: 10.1080/01973533.2012.693357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation analysis. Annual Review of Psychology, 58(1), 593–614. doi: 10.1146/annurev.psych.58.110405.085542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, & Larimer ME (Eds.). (1995). Preventing alcohol abuse in college students: A harm reduction approach. Northvale, NJ: Erlbaum. [Google Scholar]
- Martens MP, et al. (2005). Development of the Protective Behavioral Strategies Survey. Journal of Studies on Alcohol and Drugs, 66(5), 698–705. doi: 10.15288/jsa.2005.66.698 [DOI] [PubMed] [Google Scholar]
- Martens MP, et al. (2008). Protective behavioral strategies and the relationship between depressive symptoms and alcohol-related negative consequences among college students. Journal of Counselling Psychology, 55(4), 535–541. doi: 10.1037/a0013588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, et al. (2008). The Roles of Negative Affect and Coping Motives in the Relationship Between Alcohol Use and Alcohol-Related Problems Among College Students. Journal of Studies on Alcohol & Drugs, 69(3), 412–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Smith AE, & Murphy JG (2013). The efficacy of single-component brief motivational interventions among at-risk college drinkers. Journal of Consulting & Clinical Psychology, 81(4), 691–701. doi: 10.1037/a0032235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, & Clarke JC (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behavior Research and Therapy, 36(4), 455–470. doi: 10.1016/s0005-7967(97)10031-6 [DOI] [PubMed] [Google Scholar]
- Meade Eggleston A, Woolaway-Bickel K, & Schmidt NB (2004). Social anxiety and alcohol use: evaluation of the moderating and mediating effects of alcohol expectancies. Journal of Anxiety Disorders, 18(1), 33–49. doi: 10.1016/j.janxdis.2003.07.005 [DOI] [PubMed] [Google Scholar]
- Merrill JE, Reid AE, Carey MP, & Carey KB (2014). Gender and depression moderate response to brief motivational intervention for alcohol misuse among college students. Journal of Consulting and Clinical Psychology, 82(6), 984–992. doi: 10.1037/a0037039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, et al. (2012). A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting & Clinical Psychology, 80(5), 876–886. doi: 10.1037/a0028763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, et al. (2007). Social anxiety as a moderator of the relationship between perceived norms and drinking. Journal of Studies on Alcohol and Drugs, 68(1), 91–96. doi: 10.15288/jsad.2007.68.91 [DOI] [PubMed] [Google Scholar]
- Nelson TF, Toomey TL, Lenk KM, Erickson DJ, & Winters KC (2010). Implementation of NIAAA College Drinking Task Force Recommendations: How Are Colleges Doing 6 Years Later? Alcoholism: Clinical and Experimental Research, 34(10), 1687–1693. doi: 10.1111/j.1530-0277.2010.01268.x [DOI] [PubMed] [Google Scholar]
- Norberg MM, Norton AR, Olivier J, & Zvolensky MJ (2010). Social anxiety, reasons for drinking, and college students. Behavior Therapy, 41(4), 555–566. doi: 10.1016/j.beth.2010.03.002 [DOI] [PubMed] [Google Scholar]
- O’Grady MA, Cullum J, Armeli S, & Tennan H (2011). Putting the relationship between social anxiety and alcohol use into context: A daily diary investigation of drinking in response to embarrassing events. Journal of Social and Clinical Psychology, 30(6), 599–615. doi: 10.1521/jscp.2011.30.6.599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley PM, & Johnston LD (2002). Epidemiology of alcohol and other drug use among American college students. Journal of Studies on Alcohol Supplement, 63, 23. [DOI] [PubMed] [Google Scholar]
- Patrick ME, Lee CM, & Larimer ME (2011). Drinking motives, protective behavioral strategies, and experienced consequences: Identifying students at risk. Addictive Behaviors, 36(3), 270–273. doi: 10.1016/j.addbeh.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR, D’Lima GM, & Kelley ML (2013). Daily use of protective behavioral strategies and alcohol-related outcomes among college students. Psychology of Addictive Behaviors, 27(3), 826–831. doi: 10.1037/a0032516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray AE, Turrisi R, Abar B, & Peters KE (2009). Social-cognitive correlates of protective drinking behaviors and alcohol-related consequences in college students. Addictive Behaviors, 34(11), 911–917. doi: 10.1016/j.addbeh.2009.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samson JE, & Tanner-Smith EE (2015). Single-Session Alcohol Interventions for Heavy Drinking College Students: A Systematic Review and Meta-Analysis. Journal of Studies on Alcohol and Drugs, 76(4), 530–543. doi: 10.15288/jsad.2015.76.530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, & de la Fuente JR (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, et al. (2017). Monitoring the future national survey results on drug use, 1975–2016: Volume II, college students and adults ages 19–55 . Ann Arbor: Insitute for Social Research, The University of Michigan: Retrieved from http://monitoringthefuture.org/pubs.html#monographs. [Google Scholar]
- Spokas M, & Heimberg RG (2009). Overprotective parenting, social anxiety, and external locus of control: Cross-sectional and longitudinal relationships. Cognitive Therapy and Research, 33(6), 543–551. doi: 10.1007/s10608-008-9227-5 [DOI] [Google Scholar]
- Stewart SH, Morris E, Mellings T, & Komar J (2006). Relations of social anxiety variables to drinking motives, drinking quantity and frequency, and alcohol-related problems in undergraduates. Journal of Mental Health, 15(6), 671–682. doi: 10.1080/09638230600998904 [DOI] [Google Scholar]
- Sullivan LE, Fiellin DA, & O’Connor PG (2005). The prevalence and impact of alcohol problems in major depression: A systematic review. The American Journal of Medicine, 118(4), 330–341. doi: 10.1016/j.amjmed.2005.01.007 [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2015). Brief Alcohol Interventions for Adolescents and Young Adults: A Systematic Review and Meta-Analysis. Journal of Substance Abuse Treatment, 51, 1–18. doi: 10.1016/j.jsat.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terlecki MA, & Buckner JD (2015). Social anxiety and heavy situational drinking: Coping and conformity motives as multiple mediators. Addictive Behaviors, 40, 77–83. doi: 10.1016/j.addbeh.2014.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terlecki MA, Buckner JD, Larimer ME, & Copeland AL (2011). The role of social anxiety in a brief alcohol intervention for heavy-drinking college students. Journal of Cognitive Psychotherapy, 25(1), 7–21. doi: 10.1891/0889-8391.24.4.5 [DOI] [Google Scholar]
- Terlecki MA, Buckner JD, Larimer ME, & Copeland AL (2012). Brief motivational intervention for college drinking: The synergistic impact of social anxiety and perceived drinking norms. Psychology of Addictive Behaviors, 26(4), 917–923. doi: 10.1037/a0027982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terlecki MA, Buckner JD, Larimer ME, & Copeland AL (2015). Randomized controlled trial of brief alcohol screening and intervention for college students for heavy-drinking mandated and volunteer undergraduates: 12-month outcomes. Psychology of Addictive Behaviors, 29(1), 2–16. doi: 10.1037/adb0000056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terlecki MA, Ecker AH, & Buckner JD (2014). College drinking problems and social anxiety: The importance of drinking context. Psychology of Addictive Behaviors, 28(2), 545–552. doi: 10.1037/a0035770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terlecki MA, Ecker AH, & Buckner JD (2019). The Role of Underutilization of Protective Behavioral Strategies in the Relation of Social Anxiety with Risky Drinking. Addictive Behaviors. doi: 10.1016/j.addbeh.2019.106122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas SE, Thevos AK, & Randall CL (1999). Alcoholics with and without social phobia: A comparison of substance use and psychitatric variables. Journal of Studies on Alcohol, 60(472–479). [DOI] [PubMed] [Google Scholar]
- Torvik FA, et al. (2019). Explaining the association between anxiety disorders and alcohol use disorder: A twin study. Depression and Anxiety, 36(6), 522–532. doi: 10.1002/da.22886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarosa-Hurlocker MC, Madson MB, Mohn RS, Zeigler-Hill V, & Nicholson BC (2018). Social anxiety and alcohol-related outcomes: the mediating role of drinking context and protective strategies. Addiction Research & Theory, 26(5), 396–404. doi: 10.1080/16066359.2018.1424834 [DOI] [Google Scholar]
- Villarosa MC, Moorer KD, Madson MB, Zeigler-Hill V, & Noble JJ (2014). Social anxiety and alcohol-related negative consequences among college drinkers: Do protective behavioral strategies mediate the association? Psychology of Addictive Behaviors, 28(3), 887–892. doi: 10.1037/a0037628 [DOI] [PubMed] [Google Scholar]
- Wechsler H (1994). Health and behavioral consequences of binge drinking in college. A national survey of students at 140 campuses. JAMA: The Journal of the American Medical Association, 272(21), 1672–1677. doi: 10.1001/jama.272.21.1672 [DOI] [PubMed] [Google Scholar]
- Wechsler H, Dowdall GW, Maenner G, Gledhill-Hoyt J, & Lee H (1998). Changes in binge drinking and related problems among American college students between 1993 and 1997. Results of the Harvard School of Public Health College Alcohol Study. Journal of American College Health, 47(2), 57–68. doi: 10.1080/07448489809595621 [DOI] [PubMed] [Google Scholar]
- Weeks JW, et al. (2005). Empirical validation and psychometric evaluation of the Brief Fear of Negative Evaluation Scale in patients with social anxiety disorder. Psychological Assessment, 17(2), 179–190. doi: 10.1037/1040-3590.17.2.179 [DOI] [PubMed] [Google Scholar]
- White HR, & Labouvie EW (1989). Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol, 50(1), 30–37. doi: 10.15288/jsa.1989.50.30 [DOI] [PubMed] [Google Scholar]
- Williams J, & MacKinnon DP (2008). Resampling and distribution of the product methods for testing indirect effects in complex models. Structural Equation Modeling: A Multidisciplinary Journal, 15(1), 23–51. doi: 10.1080/10705510701758166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zivin K, Eisenberg D, Gollust SE, & Golberstein E (2009). Persistence of mental health problems and needs in a college student population. Journal of Affective Disorders, 117(3), 180–185. doi: 10.1016/j.jad.2009.01.001 [DOI] [PubMed] [Google Scholar]