Abstract
Background:
Concomitant lesion of the medial collateral ligament (MCL) is associated with a greater risk of anterior cruciate ligament (ACL) graft failure.
Purpose:
The aim of this study was to compare two medial stabilization techniques in patients with revision ACL reconstruction (ACLR) and concomitant chronic medial knee instability.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
In a retrospective study, we included 53 patients with revision ACLR and chronic grade 2 medial knee instability to compare medial surgical techniques (MCL reconstruction [n = 17] vs repair [n = 36]). Postoperative failure of the revision ACLR (primary aim) was defined as side-to-side difference in Rolimeter testing ≥5 mm or pivot-shift grade ≥2. Clinical parameters and postoperative functional scores (secondary aim) were evaluated with a mean ± SD follow-up of 28.8 ± 9 months (range, 24-69 months).
Results:
Revision ACLR was performed in 53 patients with additional grade 2 medial instability (men, n = 33; women, n = 20; mean age, 31.3 ± 12 years). Failure occurred in 5.9% (n = 1) in the MCL reconstruction group, whereas 36.1% (n = 13) of patients with MCL repair showed a failed revision ACLR (P = .02). In the postoperative assessment, the anterior side-to-side difference in Rolimeter testing was significantly reduced (1.5 ± 1.9 mm vs 2.9 ± 2.3 mm; P = .037), and medial knee instability occurred significantly less (18% vs 50%; P = .025) in the MCL reconstruction group than in the MCL repair group. In the logistic regression, patients showed a 9-times elevated risk of failure when an MCL repair was performed (P = .043). Patient-reported outcomes were increased in the MCL reconstruction group as compared with MCL repair, but only the Lysholm score showed a significant difference (Tegner, 5.6 ± 1.9 vs 5.3 ± 1.6; International Knee Documentation Committee, 80.3 ± 16.6 vs 73.6 ± 16.4; Lysholm, 82.9 ± 13.6 vs 75.1 ± 21.1 [P = .047]).
Conclusion:
MCL reconstruction led to lower failure rates in patients with combined revision ACLR and chronic medial instability as compared with MCL repair. MCL reconstruction was superior to MCL repair, as lower postoperative anterior instability, an increased Lysholm score, and less medial instability were present after revision ACLR. MCL repair was associated with a 9-times greater risk of failure.
Keywords: chronic medial knee instability, revision ACLR, MCL repair, MCL reconstruction
Primary ACL surgery is a common procedure; however, long-term clinical failure occurs in approximately 10.3% of the cases, while rerupture rates for revision surgery can be as high as 33%.6,7 In recent years, revision ACLRs have become the focus of reconstructive surgery, as additional procedures have been recommended in certain cases of revision ACLR, such as slope-correction osteotomies or anterolateral reconstructions.7,8,29,30,32,33 Numerous studies have evaluated reasons for failure of primary and revision surgery, and patient- and surgery-related risk factors for ACLR failure have been identified.32,33 Common reasons for ACLR failure include technical errors (eg, malpositioning of the femoral tunnel), trauma, biological factors, untreated peripheral instabilities, and knee infection.2,12,31,34 Nevertheless, persistent or recurrent instability, impaired functional outcome, and pain have been repeatedly described after revision ACLR.13
Failure of revision anterior cruciate ligament reconstruction (ACLR) can be associated with a concomitant lesion of the medial collateral ligament (MCL) complex, as it can lead to a 13.6- to 16.8-times greater risk of failure.1,2 In addition, ACLR and medial anatomic reconstruction lead to significantly lower failure rates and improved patient-reported outcome in patients with chronic MCL and primary ACL ruptur.2,10 While some studies have analyzed the outcome of combined MCL reconstruction and primary ACLR, the influence of medial stabilization techniques in revision ACLR and its effect on patient outcomes have not yet been the focus.10,35
To the best of our knowledge, MCL reconstruction and repair in revision ACLR and chronic medial instability have not been compared before. The primary aim of this study was to compare MCL repair and MCL reconstruction in regard to failure rates in patients with revision ACLR and chronic medial knee instability. The secondary aim was to analyze the clinical outcome measures in these 2 groups (eg, side-to-side-difference, medial knee instability, functional scores). We hypothesized that reconstructing the MCL using autografts would lead to lower failure rates and improved patient-related outcome as compared with MCL suture repair techniques in patients with revision ACLR and chronic medial knee instability.
Methods
Study Population
This retrospective cohort study analyzed all consecutive patients surgically treated between May 2013 and January 2018 with a minimum follow-up of 24 months (mean ± SD, 28.8 ± 9 months; range, 24-69 months). We included all patients (n = 59) with the diagnosis of persistent or recurrent instability after primary ACLR who were surgically treated between 2013 and January 2018 in our clinic. An additional inclusion criterion was that grade 2 medial knee instability, as diagnosed via clinical examination under anesthesia, must have been present at the time of revision surgery and must have been surgically addressed using MCL repair or MCL reconstruction. Medial knee instability was assessed clinically according to the classification of Hughston et al19 and the American Medical Association (grade 1, 0-5 mm; grade 2, 6-10 mm; grade 3, >10 mm).3 Exclusion criteria were grade 3 medial knee instability (n = 1), injury to the posterior cruciate ligament (n = 1), infection of the knee (n = 1), and signs of generalized hypermobility according to the Beighton score (≥5/9) (n = 1).29 Two patients were lost to follow up. Thus, 53 patients were included in the study. The primary aim was to evaluate the failure rates of revision ACLR between MCL repair and MCL reconstruction. Postoperative failure of revision ACLR was defined as a side-to-side difference in Rolimeter testing ≥5 mm or pivot-shift grade ≥2. The secondary aim was to analyze the clinical outcomes between these groups (eg, side-to-side difference, postoperative functional scores).
The treatment of MCL insufficiency was modified over time according to our clinical experience. Between 2013 and 2016, the standard treatment for grade 2 medial knee instability in revision ACLR was a suture repair with gathering of the medial structures, and this procedure was performed for 36 (67.9%) patients. From 2016 onward, the standard therapy for grade 2 medial instability in revision ACLR was a reconstruction using autologous tendon grafts. Thus, 17 (32.1%) patients received an additional MCL graft. The study design was approved by the local ethics committee, and informed consent was obtained from each patient in the study (No. 3293).
Surgical Technique of the Revision ACLR
Revision ACLR was performed via ipsi- or contralateral autografts using a single-bundle technique. The choice of revision ACL graft depended on previous graft removal, and hamstring tendon, bone–patellar tendon–bone, or quadriceps grafts were used. Femoral tunnel placement was performed via the anteromedial portal, and both tunnels (femoral and tibial) were controlled under fluoroscopy during revision surgery.
Surgical Technique of Suture Repair of the Medial Structures
A 4- to 6-cm longitudinal incision of the skin was placed over the medial epicondyle and adductor tubercle. After the sartorius fascia was split, the proximal superficial MCL (sMCL) and posterior oblique ligament (POL) were exposed.
The proximal sMCL and POL were inspected. If there was laxity at the femoral insertion, they were tightened via gathering stitches using suture anchors. The tibial sMCL insertion was inspected through access to the tibial ACL bone tunnel. If there was also laxity, it was tightened using suture anchors. If medial stability was not restored in this way, additional posteromedial advancement and reefing of the POL and adherent posterior capsule to the MCL were performed, according to the description of Jacobson and Chi.22 The interval between the sMCL and the POL was opened longitudinally, and the deep MCL and the medial meniscus were shown. The deep structures and deep MCL were tightened using sutures, and any lesion of the posteromedial meniscus complex was repaired and sutured to the deep MCL. Using a pants-over-vest suture technique, the POL was also sutured and tightened. Possible damage to the semimembranosus insertion was repaired, and the sMCL was tensioned and closed.
Surgical Technique of the Medial Reconstruction Using Autologous Tendon Grafts
The MCL reconstruction was performed according to the descriptions of Preiss et al.28 A 6-mm femoral bone tunnel was created at the intersection of an imaginary extension of the posterior edge of the tibia and the radiologic crossing with the Blumensaat line via a 1- to 2-cm skin insertion under strict fluoroscopic control of the medial knee (Figure 1).
Figure 1.
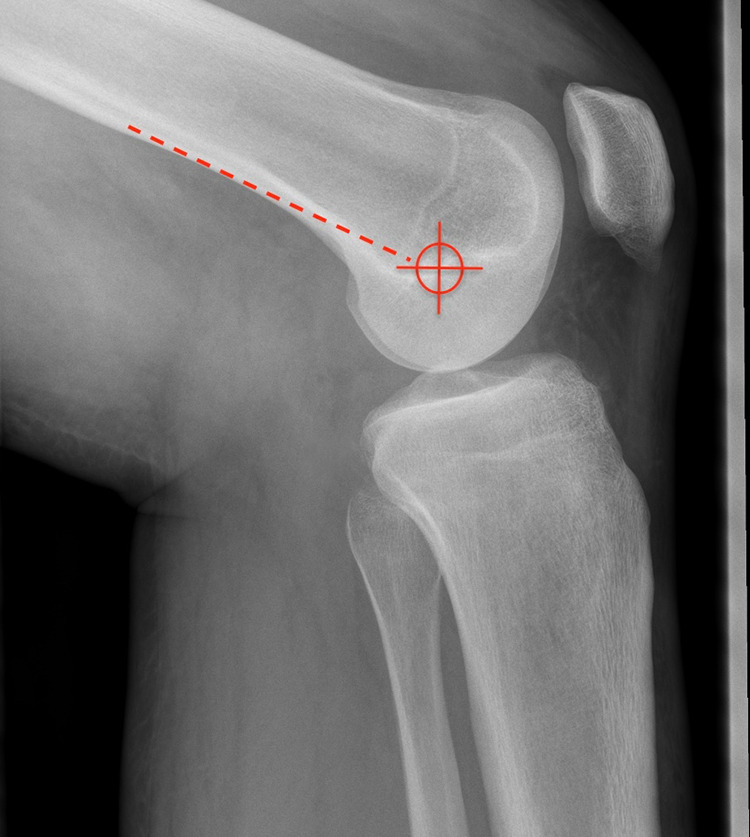
An imaginary extension of the posterior edge of the tibia and the radiologic crossing with the Blumensaat line was used to find the femoral bone tunnel for the medial collateral ligament reconstruction.
A gracilis tendon autograft sutured at both ends was placed in the femoral tunnel and fixed using an interference screw. Thus, 1 branch of the femoral tunnel could be used for the sMCL, and the second could be used for the POL reconstruction. A 5-mm bone tunnel was created above the pes anserinus centrally to the sMCL insertion and above the insertion of the distal arm of the semimembranosus muscle. The sMCL and POL branches were inserted into the tibial bone tunnels below the sartorius fascia and fixed using interference screws at 30° of knee flexion (Figure 2).
Figure 2.

The superficial medial collateral ligament and posterior oblique ligament branches were inserted into the tibial bone tunnels below the sartorius fascia and fixed using an interference screw.
Postoperative Protocol
Mobilization and passive range of motion were started on the first postoperative day, and partial weightbearing (20 kg) was recommended for 6 weeks. A brace was applied, and passive motion was limited to 0°/30° for 2 weeks (extension/flexion), 0°/60° for 2 weeks, 0°/90° for 2 weeks, and then unlimited range of motion. Pivoting or contact sports (eg, football, basketball) were allowed after 12 months. The same postoperative protocol was used for the group with MCL repair and the group with MCL reconstruction.
Patient Outcomes
All patients were clinically examined at follow-up. The pivot-shift test was pre- and postoperatively measured and divided into grade 1 (glide), grade 2 (clunk), and grade 3 (gross). The Lachman test was evaluated using the 2000 IKDC Knee Examination Form (International Knee Documentation Committee) as follows: grade 1 (2-5 mm), grade 2 (6-10 mm), grade 3 (>10 mm).20 To confirm medial knee instability during revision surgery, we looked at the medial meniscus when applying valgus stress to identify a “medial drive-through sign.”
Scores such as visual analog scale for pain, Lysholm, and Tegner rating were collected before and after revision surgery, and the subjective IKDC score was evaluated only postoperatively.6,21,26,31 The Lysholm score was divided into excellent (>94 points), good (84-94 points), fair (65-83 points), and poor (<65 points). Preoperative long-leg standing radiographs were used to determine leg alignment, and the posterior tibial slope was measured on the lateral knee radiograph and calculated by defining the angle between a line drawn tangentially to the tibial plateau and the proximal anatomic axis of the tibia.33 A normal posterior tibial slope was defined as 8° ± 3°.24
Statistical Analysis
Data were presented as mean and SD for continuous variables. A subgroup analysis was performed to determine correlations between patients with revision ACLR and MCL repair and patients with revision ACLR and MCL graft. Mean differences between these groups were calculated using an unpaired Student t test for parametric parameters and a Kruskal-Wallis test for nonparametric parameters, and differences in categorical parameters were compared using a chi-square test. Additionally, multivariable conditional logistic regression analysis was performed to identify predictors for failure of revision ACLR, including the medial stabilization technique (MCL repair vs reconstruction) and sex. A post hoc power analysis was performed using G*Power Version 3.1.9.6 for Mac (HHU Düsseldorf) to assess the validity of the proportions of revision ACLR failure in patients with MCL repair or reconstruction. Statistical analysis was performed using SPSS Statistics Version 22 (IBM Corp), and a P value <.05 was considered significant.
Results
Revision ACLR was performed in 53 patients (men, n = 33; women, n = 20) with grade 2 medial instability, and the mean age at revision surgery was 31.3 ± 12 years (range, 18-61 years). In total, revision ACLR failed in 14 patients (26.4%). An MCL reconstruction was associated with significantly lower failure rates than was MCL repair. Thus, failure occurred in 5.9% (1/17) of patients in the MCL reconstruction group, whereas 36.1% (13/36) of patients had a failed revision ACLR in the MCL repair group (P = .02). Based on our proportions of failure (0.361/0.059) in 53 patients, a post hoc power of 0.778 was achieved at a significance level of 5%. In the preoperative assessment, there was no difference between the groups. Descriptive data were similar between the MCL repair and MCL reconstruction groups. Patient characteristics and preoperative clinical findings are displayed in Tables 1 and 2.
TABLE 1.
Patient Characteristics According to MCL Repair and MCL Reconstructiona (N = 53)
| Characteristic | MCL Repair (n = 36) | MCL Reconstruction (n = 17) | P Value |
|---|---|---|---|
| Sex: female | 13 (36.1) | 7 (41.2) | .79 |
| Age, y | 29.8 ± 11.2 (18-61) | 34.6 ± 13.2 (18-61) | .15 |
| Affected knee: left | 15 (41.7) | 3 (17.6) | .13 |
| Revision ACL reconstruction failure | 13 (36.1) | 1 (5.9) | .02 |
| Follow-up, mo | 29.6 ± 10.7 (24-69) | 27.2 ± 2.8 (24-34) | .85 |
| Body mass index | 25.3 ± 3.5 (18-32) | 24.5 ± 3.3 (18-30) | .47 |
| Revision ACL graft choice | .16 | ||
| Bone–patellar bone–tendon | 13 (36.1) | 3 (17.6) | |
| Hamstring tendon | 11 (30.6) | 2 (11.8) | |
| Quadriceps tendon | 12 (33.3) | 12 (70.6) | |
| Malalignment, deg | |||
| Varus | 0 | 1 (5.9) | .09 |
| Valgus | 1 (2.8) | 0 | .21 |
| Posterior tibial slope, deg | 9.6 ± 1.9 (5-15) | 9.3 ± 2.1 (6-13) | .62 |
aValues are presented as No. (%) or mean ± SD (range). Bold indicates P < .05. ACL, anterior cruciate ligament; MCL, medial collateral ligament.
TABLE 2.
Preoperative Clinical Assessment According to MCL Repair and Reconstructiona (N = 53)
| Characteristic | MCL Repair (n = 36) | MCL Reconstruction (n = 17) | P Value |
|---|---|---|---|
| Limited range of motionb | 3 (8.3) | 0 | .14 |
| Grade of Lachman test | .73 | ||
| 1: 2-5 mm | 6 (16.7) | 0 | |
| 2: 5-10 mm | 18 (50) | 8 (47.1) | |
| 3: >10 mm | 12 (33.3) | 9 (52.9) | |
| Grade of pivot-shift test | .16 | ||
| 1: glide | 7 (19.4) | 0 | |
| 2: clunk | 13 (36.1) | 10 (58.8) | |
| 3: gross | 16 (44.4) | 7 (41.2) | |
| Rolimeter side-to-side difference, mm | 6.9 ± 2 (4-10) | 7.5 ± 1.8 (4-10) | .25 |
aValues are presented as No. (%) or mean ± SD (range). MCL, medial collateral ligament.
b>5° of flexion and extension deficit.
In the postoperative assessment, there was a significant difference between the MCL reconstruction group and the MCL repair group in regard to side-to-side difference. At the latest follow-up, patients with an MCL reconstruction showed a side-to-side difference of 1.5 ± 1.9 mm compared with 2.9 ± 2.3 mm (P = .037) for those with an MCL repair. Medial knee instability occurred significantly less in the MCL reconstruction group than in the MCL repair group (18% vs 50%; P = .025) (Table 3).
TABLE 3.
Postoperative Clinical Findings According to MCL Repair and Reconstructiona (N = 53)
| Characteristic | MCL Repair (n = 36) | MCL Reconstruction (n = 17) | P Value |
|---|---|---|---|
| Limited range of motionb | 1 (2.8) | 0 | .47 |
| Grade of Lachman test | .29 | ||
| Absent | 19 (52.8) | 14 (82.4) | |
| 1: 2-5 mm | 10 (27.8) | 2 (11.8) | |
| 2: 5-10 mm | 7 (19.4) | 1 (5.9) | |
| 3: >10 mm | 0 | 0 | |
| Grade of pivot-shift test | .43 | ||
| Absent | 27 (75) | 16 (94.1) | |
| 1: glide | 3 (8.3) | 0 | |
| 2: clunk | 5 (13.9) | 1 (5.9) | |
| 3: gross | 1 (2.8) | 0 | |
| Rolimeter SSD, mm | 2.9 ± 2.3 (0-9) | 1.5 ± 1.9 (0-8) | .04 |
| Failure of the revision ACLRc | 13 (36.1) | 1 (5.9) | .02 |
| Medial knee instability | 18 (50) | 3 (17.6) | .03 |
| Grade 1 | 11 (30.6) | 2 (11.8) | .08 |
| Grade 2 | 7 (19.4) | 1 (5.9) |
aValues are presented as No. (%) or mean ± SD (range). Bold indicates P < .05. ACLR, anterior cruciate ligament reconstruction; MCL, medial collateral ligament; SSD, side-to-side difference.
b>5° of flexion and extension deficit.
cSSD >5 mm or pivot shift >2.
Overall, 29 patients (54.7%) reported a good to excellent clinical outcome, and 24 (45.3%) showed fair to poor outcome measures according to the Lysholm score. Functional scores, including Tegner (2.8 ± 1.4 to 5.4 ± 1.7; P < .001) and Lysholm (50.9 ± 24.7 to 77.6 ± 19.2; P < .001), significantly improved in comparison with preoperative values, and IKDC showed a postoperative mean of 75.7 ± 16.6 points. Pain according to the visual analog scale was significantly reduced after revision surgery (4.2 ± 2.8 to 1.6 ± 1.9; P < .001). Only the Lysholm score showed a significant difference between the groups, with higher scores for the MCL reconstruction group (Lysholm, 82.9 ± 13.6 vs 75.1 ± 21.1; P = .047) (Table 4).
TABLE 4.
Postoperative Functional Results According to MCL Repair and Reconstructiona (N = 53)
| Characteristic | MCL Repair (n = 36) | MCL Reconstruction (n = 17) | P Value |
|---|---|---|---|
| VAS for pain | 1.9 ± 2.1 (0-9) | 1.1 ± 1.4 (0-3) | .19 |
| Lysholm | 75.1 ± 21.1 (6-100) | 82.9 ± 13.6 (41-100) | .047 |
| Excellent: >94 | 8 (22.2) | 5 (29.4) | .42 |
| Good: 84-94 | 11 (30.6) | 5 (29.4) | |
| Fair: 65-83 | 7 (19.4) | 6 (35.3) | |
| Poor: <65 | 10 (27.8) | 1 (5.9) | |
| Tegner | 5.3 ± 1.6 (1-9) | 5.6 ± 1.9 (3-9) | .19 |
| IKDC | 73.6 ± 16.4 (13.8-96.7) | 80.3 ± 16.6 (32-100) | .12 |
aValues are presented as No. (%) or mean ± SD (range). Bold indicates P < .05. IKDC, International Knee Documentation Committee; MCL, medial collateral ligament; VAS, visual analog scale.
Logistic regression revealed that MCL repair was an independent risk factor for an increased failure rate, as patients were 9 times more likely to have a failed revision ACLR (odds ratio, 9.043; 95% CI, 1.07-76.23; P = .043) (Table 5).
TABLE 5.
Logistic Regression According to Failurea
| Variable | β | SE | Wald | df | P Value | Exp (β) |
|---|---|---|---|---|---|---|
| MCL repair | 2.202 | 0.011 | 4.099 | 1 | .043 | 9.043 |
| Sex: female | 0.063 | 6.940 | 0.011 | 1 | .917 | 1.065 |
aBold indicates P < .05. MCL, medial collateral ligament.
Discussion
The most important finding of our study was that MCL reconstruction leads to lower failure rates in patients with revision ACLR and chronic medial knee instability as compared with MCL repair. MCL reconstruction was superior to MCL repair, as lower postoperative anterior instability, increased Lysholm scores, and less incidence of medial instability after revision ACLR occurred. Also, logistic regression revealed that MCL repair was associated with a 9-times greater risk of failure.
Previous studies have revealed that medial instability increases the force on the ACL graft and that both the ACL and the MCL benefit from a surgical intervention of the MCL.4,37 Ahn and Lee1 found that concomitant grade 2 MCL instability was a significant risk factor for recurrent knee instability after ACLR, as patients with grade 2 medial instability had a 13.6-times greater risk of having a failed ACLR. Moreover, Hamrin Senorski et al17 demonstrated that concomitant MCL instability was a strong negative predictor of return to knee-strenuous sports within the first year after ACLR. Also, Alm et al2 showed that failure of revision ACLR was associated with preoperative medial knee instability and that medial stabilizing techniques reduced the risk of failure by a factor of 13. Thus, medial knee instability of grade ≥2 severity should be surgically addressed during revision surgery. This study proved that functional scores can be significantly improved by addressing the medial knee instability.
While some clinical studies have recommended a nonsurgical approach, others have shown a benefit in reconstructing the ACL and MCL in acute combined injuries.9,14,36 However, numerous techniques for the surgical treatment of the MCL instability, including MCL repair and MCL reconstruction, have been described and reported to lead to successful outcomes, even in ACL-deficient knees.12,14–16 In a prospective randomized controlled study, Funchal et al11 demonstrated significantly lower failure rates (3.4% vs 29.6%) and improved clinical outcomes (Lysholm, 90 vs 78 points) when patients with combined chronic MCL grade II and primary ACL rupture were treated with ACLR and MCL reconstruction.
Dong et al9 analyzed the effect of MCL repair and MCL reconstruction on primary ACL tears and acute grade 3 MCL instability in combination with primary ACLR. They found no major differences between MCL repair and MCL reconstruction based on postoperative IKDC scores and medial opening evaluations. Nevertheless, it was shown that MCL reconstruction restored better anteromedial rotatory stability than did MCL repair. In this study, MCL reconstruction was also associated with better restoration of anterior displacement of the tibia according to the side-to-side difference (1.5 ± 1.9 mm vs 2.9 ± 2.3 mm) and medial knee instability (18% vs 50%) in comparison with MCL repair. Nevertheless, a comparison between MCL reconstruction and repair in patients with revision ACLR and chronic medial instability has not been published to date. This study represents the first to show this difference.
Previous studies have considered MCL repair as an option for treatment in the acute phase; in the subacute or chronic phase, the MCL graft may be the preferred treatment option, as scarring is difficult to repair.5,9,25 Our findings support these studies, as chronic medial instability, especially grade ≥2, in combination with revision ACLR should be surgically addressed using MCL reconstruction at the time of revision surgery. The good clinical results of anatomic MCL reconstruction suggest that it may be superior to MCL repair in the chronic setting: Funchal et al11 demonstrated as much in combined MCL and primary ACLR, and Dong et al9 achieved better rotary stability in anatomic MCL reconstruction than MCL repair.9,11,25
Using MCL allografts is a suitable option for MCL reconstructions.18,27 An advantage is that harvesting more tendons would not be necessary and that the hamstring tendons (the medial dynamic stabilizer) could be preserved, in case they were still intact. A disadvantage of using allografts could be that they are not commonly available, they incur higher costs, and they are associated with increased failure rates.23
To the best of our knowledge, this is the first study on revision ACLR and surgical treatment of chronic medial instability. Although the study size and subgroups were small, MCL reconstruction led to lower failure rates in revision ACLR and chronic medial instability as compared with MCL repair. This study revealed that MCL reconstruction was superior to MCL repair, as lower postoperative anterior instability, improved Lysholm score, and less medial instability were present after revision ACLR.
There are a few limitations in this study. First, no preoperative randomization was performed, and the study was based on a small study size (53 patients) and a small subgroup with MCL reconstruction (17 patients). Second, a strong limitation was that no preoperative valgus or varus stress radiographs were performed at pre- and postoperative assessment. The degree of medial instability was only clinically evaluated and confirmed using the medial drive-through sign during revision surgery. Third, given the retrospective study design, important data, such as preoperative side-to-side difference in Rolimeter testing or meniscal or chondral lesions, could not be collected. Fourth, because we changed the procedures from repair to reconstruction during the study period, a possible bias could have occurred. Fifth, the follow-up period was limited, and postoperative long-term complications, such as osteoarthritis or subsequent procedures, could not be observed.
Conclusion
MCL reconstruction led to lower failure rates in patients with revision ACLR and chronic medial instability compared with MCL repair. MCL reconstruction was superior to MCL repair, as lower postoperative anterior instability, increased Lysholm scores, and less medial instability were present after revision ACLR. MCL repair was associated with a 9-times greater risk of failure.
Footnotes
Final revision submitted August 24, 2020; accepted September 21, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: K.H.F. has received educational payments and royalties from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hamburg Medical Association (No. 3293, Ärztekammer Hamburg).
References
- 1. Ahn JH, Lee SH. Risk factors for knee instability after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2936–2942. [DOI] [PubMed] [Google Scholar]
- 2. Alm L, Krause M, Frosch KH, Akoto R. Preoperative medial knee instability is an underestimated risk factor for failure of revision ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2458–2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. American Medical Association. Standard Nomenclature of Athletic Injuries; 1968. [Google Scholar]
- 4. Battaglia MJ, II, Lenhoff MW, Ehteshami JR, et al. Medial collateral ligament injuries and subsequent load on the anterior cruciate ligament: a biomechanical evaluation in a cadaveric model. Am J Sports Med. 2009;37(2):305–311. [DOI] [PubMed] [Google Scholar]
- 5. Borden PS, Kantaras AT, Caborn DN. Medial collateral ligament reconstruction with allograft using a double-bundle technique. Arthroscopy. 2002;18(4):E19. [DOI] [PubMed] [Google Scholar]
- 6. Collins NJ, Prinsen CA, Christensen R, Bartels EM, Terwee CB, Roos EM. Knee injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage. 2016;24(8):1317–1329. [DOI] [PubMed] [Google Scholar]
- 7. Crawford SN, Waterman BR, Lubowitz JH. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29(9):1566–1571. [DOI] [PubMed] [Google Scholar]
- 8. Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2846–2852. [DOI] [PubMed] [Google Scholar]
- 9. Dong J, Wang XF, Men X, et al. Surgical treatment of acute grade III medial collateral ligament injury combined with anterior cruciate ligament injury: anatomic ligament repair versus triangular ligament reconstruction. Arthroscopy. 2015;31(6):1108–1116. [DOI] [PubMed] [Google Scholar]
- 10. Erickson BJ, Cvetanovich GL, Frank RM, Riff AJ, Bach BR, Jr. Revision ACL reconstruction: a critical analysis review. JBJS Rev. 2017;5(6):e1. [DOI] [PubMed] [Google Scholar]
- 11. Funchal LFZ, Astur DC, Ortiz R, Cohen M. The presence of the arthroscopic “floating meniscus” sign as an indicator for surgical intervention in patients with combined anterior cruciate ligament and grade II medial collateral ligament injury. Arthroscopy. 2019;35(3):930–937. [DOI] [PubMed] [Google Scholar]
- 12. Gallo RA, Kozlansky G, Bonazza N, Warren RF. Combined anterior cruciate ligament and medial collateral ligament reconstruction using a single Achilles tendon allograft. Arthrosc Tech. 2017;6(5):e1821–e1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. George MS, Dunn WR, Spindler KP. Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34(12):2026–2037. [DOI] [PubMed] [Google Scholar]
- 14. Grant JA, Tannenbaum E, Miller BS, Bedi A. Treatment of combined complete tears of the anterior cruciate and medial collateral ligaments. Arthroscopy. 2012;28(1):110–122. [DOI] [PubMed] [Google Scholar]
- 15. Halinen J, Lindahl J, Hirvensalo E. Range of motion and quadriceps muscle power after early surgical treatment of acute combined anterior cruciate and grade-III medial collateral ligament injuries: a prospective randomized study. J Bone Joint Surg Am. 2009;91(6):1305–1312. [DOI] [PubMed] [Google Scholar]
- 16. Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. 2006;34(7):1134–1140. [DOI] [PubMed] [Google Scholar]
- 17. Hamrin Senorski E, Svantesson E, Beischer S, et al. Low 1-year return-to-sport rate after anterior cruciate ligament reconstruction regardless of patient and surgical factors: a prospective cohort study of 272 patients. Am J Sports Med. 2018;46(7):1551–1558. [DOI] [PubMed] [Google Scholar]
- 18. Hanley JM, Anthony CA, DeMik D, et al. Patient-reported outcomes after multiligament knee injury: MCL repair versus reconstruction. Orthop J Sports Med. 2017;5(3):2325967117694818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities, part I: the medial compartment and cruciate ligaments. J Bone Joint Surg Am. 1976;58(2):159–172. [PubMed] [Google Scholar]
- 20. Irrgang JJ, Anderson AF. Development and validation of health-related quality of life measures for the knee. Clin Orthop Relat Res. 2002;402:95–109. [DOI] [PubMed] [Google Scholar]
- 21. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 22. Jacobson KE, Chi FS. Evaluation and treatment of medial collateral ligament and medial-sided injuries of the knee. Sports Med Arthrosc Rev. 2006;14(2):58–66. [DOI] [PubMed] [Google Scholar]
- 23. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3(1):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Krause M, Drenck TC, Korthaus A, Preiss A, Frosch KH, Akoto R. Patella height is not altered by descending medial open-wedge high tibial osteotomy (HTO) compared to ascending HTO. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1859–1866. [DOI] [PubMed] [Google Scholar]
- 25. Lind M, Jakobsen BW, Lund B, Hansen MS, Abdallah O, Christiansen SE. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med. 2009;37(6):1116–1122. [DOI] [PubMed] [Google Scholar]
- 26. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. [DOI] [PubMed] [Google Scholar]
- 27. Marx RG, Hetsroni I. Surgical technique: medial collateral ligament reconstruction using Achilles allograft for combined knee ligament injury. Clin Orthop Relat Res. 2012;470(3):798–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Preiss A, Giannakos A, Frosch KH. Minimally invasive augmentation of the medial collateral ligament with autologous hamstring tendons in chronic knee instability. Article in German. Oper Orthop Traumatol. 2012;24(4-5):335–347. [DOI] [PubMed] [Google Scholar]
- 29. Smits-Engelsman B, Klerks M, Kirby A. Beighton score: a valid measure for generalized hypermobility in children. J Pediatr. 2011;158(1):119–123, e111-e114. [DOI] [PubMed] [Google Scholar]
- 30. Southam BR, Colosimo AJ, Grawe B. Underappreciated factors to consider in revision anterior cruciate ligament reconstruction: a current concepts review. Orthop J Sports Med. 2018;6(1):2325967117751689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 32. Trojani C, Sbihi A, Djian P, et al. Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):196–201. [DOI] [PubMed] [Google Scholar]
- 33. Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament–reconstructed patient. Am J Sports Med. 2013;41(12):2800–2804. [DOI] [PubMed] [Google Scholar]
- 34. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(6):531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wright RW, Huston LJ, Spindler KP, et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38(10):1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zaffagnini S, Bonanzinga T, Marcheggiani Muccioli GM, et al. Does chronic medial collateral ligament laxity influence the outcome of anterior cruciate ligament reconstruction? A prospective evaluation with a minimum three-year follow-up. J Bone Joint Surg Br. 2011;93(8):1060–1064. [DOI] [PubMed] [Google Scholar]
- 37. Zhu J, Dong J, Marshall B, Linde MA, Smolinski P, Fu FH. Medial collateral ligament reconstruction is necessary to restore anterior stability with anterior cruciate and medial collateral ligament injury. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):550–557. [DOI] [PubMed] [Google Scholar]


