Abstract
Background:
Anterior cruciate ligament (ACL) tears are frequently associated with meniscal injury. Risk factors for concomitant meniscal injuries have been studied in the adult population but less so in pediatric patients.
Purpose:
To evaluate the relationship between age and body mass index (BMI) and the presence of a concomitant meniscal tear at the time of ACL reconstruction (ACLR) in pediatric patients.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A single-institution retrospective review was performed of patients aged <19 years who underwent primary ACLR over a 3.5-year period. Revision ACLR and multiligament knee reconstructions were excluded. Logistic regression was used to identify risk factors associated with having a meniscal tear at the time of surgery. Subgroup analysis was performed for medial and lateral meniscal tears.
Results:
Included in this study were 453 patients (230 males, 223 females; median age, 15 years). Of these, 265 patients (58%) had a meniscal tear, including 150 isolated lateral meniscal tears, 53 isolated medial meniscal tears, and 62 patients with both lateral and medial meniscal tears. Median time from injury to surgery was 48 days. For every 1-year increase in age, there was a 16% increase in the adjusted odds of having any meniscal tear (odds ratio [OR], 1.16; 95% confidence interval [CI], 1.05-1.27; P = .002), with a 20% increase in the odds of having a medial meniscal tear (OR, 1.20; 95% CI, 1.07-1.35; P = .002) and a 16% increase in the odds of having a lateral meniscal tear (OR, 1.16; 95% CI, 1.05-1.27; P = .003). For every 2-point increase in BMI, there was a 12% increase in the odds of having any meniscal tear (OR, 1.12; 95% CI, 1.02-1.22; P = .016) and a 10% increase in the odds of having a lateral meniscal tear (OR, 1.10; 95% CI, 1.01-1.19; P = .028).
Conclusion:
Pediatric patients undergoing ACLR had a 58% incidence of concomitant meniscal pathology. Increasing age and BMI were independent risk factors for these injuries, while no association was found between time to surgery and meniscal pathology.
Keywords: ACL tear, BMI, meniscus tear, pediatric, risk factors
The rate of anterior cruciate ligament (ACL) injuries continues to rise in the pediatric and adolescent population.11,29 To minimize the risk of additional intra-articular damage secondary to altered knee mechanics in ACL-deficient knees, ACL reconstruction (ACLR) in a timely fashion is the preferred treatment modality for these patients.22 Pediatric ACL injuries are often associated with concomitant meniscal or chondral injuries, and these concomitant injuries are being treated with increasing frequency.7 Concurrent meniscal pathology has been noted to be as high as 60% to 70% in large primary ACLR studies including both adults and adolescents.8,24,32,34 Both the lateral and medial menisci may sustain injury at the time of the ACL tear. Classically, lateral meniscal tears are thought to be created at the time of the ACL injury due to compressive and shear forces during the pivot shift phenomenon. These tears are frequently seen in patients undergoing acute ACLR.3 On the contrary, medial meniscal tears have been shown to be more frequent in patients with chronic ACL injuries undergoing delayed reconstruction. This may be related to the role of the medial meniscus as a secondary stabilizer in an ACL-deficient knee, although medial meniscal tears result from acute injury as well.5,6
To optimize results after ACLR, it is critical to recognize and address concomitant injuries. Meniscal tears are particularly important to appreciate as the menisci function not only in shock absorption but also as secondary stabilizers of the knee.1,27 Meniscal deficiency has also been shown to be an independent risk factor for the development of radiographic osteoarthritis after ACLR.19 Advanced imaging such as magnetic resonance imaging (MRI) is good, but not perfect, in detecting meniscal lesions, so a thorough and systematic arthroscopic evaluation is routinely performed.13,18
Risk factors for meniscal injuries in association with ACL tears have been extensively studied in the adult population, but they have been less so in pediatric patients.4,28 Among pediatric and adolescent patients with ACL tears, there is limited evidence to elucidate independent relationships between age, BMI, time from injury to surgery, and the presence of meniscal pathology.8,24,26,31 The purpose of this study was to evaluate the relationship between age, BMI, time from injury to surgery, and the presence of a meniscal tear at the time of ACLR in children and adolescents. We hypothesized that there would be a direct relationship between increasing age and BMI and the presence of concomitant meniscal injury.
Methods
A retrospective chart review of consecutive pediatric patients aged <19 years who underwent ACLR between August 2012 and April 2016 at a single institution by 1 of 3 fellowship-trained pediatric orthopaedic surgeons (M.T.B., S.C.W., and M.A.C.). The patient cohort was created by querying the electronic medical record using the Current Procedural Code (CPT) code 29888 (ACL reconstruction). Patients with multiligament knee reconstructions and revision ACLRs were excluded. Approval for this study was received from an institutional review board.
Demographic information (age, sex, BMI, and time from injury to surgery) was obtained from the medical chart. Meniscal tears were identified based on intraoperative findings, as documented in the operative report. Meniscal tears were noted to be medial, lateral, or both medial and lateral, but more detailed information about tear location or pattern was not evaluated in this study. Time from injury to surgery was defined as the patient’s reported date of injury and the date of surgery.
Statistical analyses were performed using SAS Version 9.4 (SAS Institute), and statistical significance was assessed at the 0.05 level. Descriptive statistics were calculated for all variables of interest and included medians and interquartile ranges as well as counts and percentages, when appropriate. Categorical variables were compared between patients who had a meniscal tear versus those who did not have a meniscal tear using the chi-square test. Normality of continuous variables was assessed using histograms and normal probability plots in addition to through the Anderson-Darling test for normality. The distribution of continuous variables was compared between groups using Wilcoxon rank-sum tests. Logistic regression was used to identify independent risk factors associated with having a meniscal tear. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were constructed for each independent risk factor (age and BMI). Two subgroup analyses were performed, those who had had a medial meniscal tear and those who had had a lateral meniscal tear using similar procedures as for the overall cohort.
Results
A total of 453 patients were included: 230 male patients (51%) and 223 female patients (49%) with a median age of 15 years (range, 7-18 years). The right (49%) and left (51%) knees were affected nearly equally. In total, 265 patients (58%) had a meniscal tear, including 150 isolated lateral meniscal tears (57%), 53 isolated medial meniscal tears (20%), and 62 patients (23%) with both lateral and medial meniscal tears. There were no statistically significant differences in sex with regard to meniscal tears, with 54% of meniscal tears occurring in male patients and 46% in female patients (P = .16). Demographic data for the cohort is provided in Table 1. Among patients aged 13 years and younger (n = 90), 47% had a meniscal tear. In contrast, of patients aged 14 to 18 years (n = 363), 61% had a meniscal tear, which was significantly greater compared to the younger age group (P = .01).
Table 1.
Demographic and Clinical Characteristics (n = 453 Patients)a
| Value | |
|---|---|
| Sex | |
| Male | 230 (51) |
| Female | 223 (49) |
| Age, y | 15 (14-16) |
| Knee | |
| Right | 223 (49) |
| Left | 230 (51) |
| Any meniscal tear | 265 (58) |
| LM | 150 (57) |
| MM | 53 (20) |
| LM, MM | 62 (23) |
aValues are shown as n (%) or median (interquartile range). LM, lateral meniscus; MM, medial meniscus.
Age at surgery was found to be a statistically significant independent predictor of the presence of a meniscal tear. For every 1-year increase in age, there was a 16% increase in the odds of having any meniscal tear (OR, 1.16; 95% CI, 1.05-1.27; P = .002), depicted in Figure 1. Age at surgery was also a statistically significant independent predictor following subgroup analysis of medial and lateral meniscal tears. For every 1-year increase in age at surgery, there was a 20% increase in the odds of having a medial meniscal tear (OR, 1.20; 95% CI, 1.07-1.35; P = .002) and a 16% increase in the odds of having a lateral meniscal tear (OR, 1.16, 95% CI, 1.05-1.27; P = .003).
Figure 1.
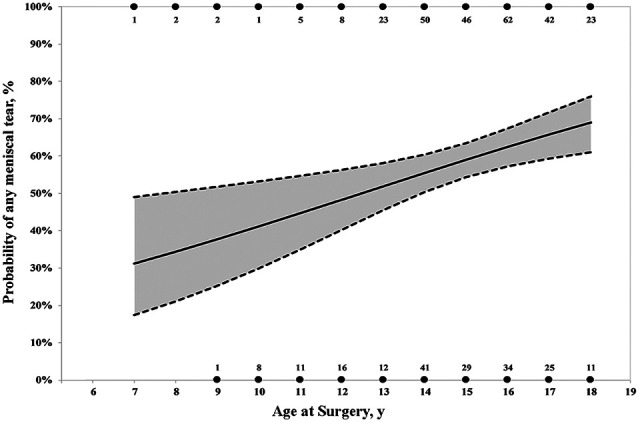
Predicted probability plot of any meniscal tear by age. Circles represent the number of patients who did have a meniscus tear (at the top of chart along 100% line) and did not have a meniscus tear (numbers along 0% line). The solid line represents the predicted probability of any meniscus tear for each given age. The dashed lines represent the standard error of the predicted probability.
After adjusting for age, body mass index (BMI) was also identified to be an independent predictor of a meniscal tear. For every 2 point increase in BMI, there was a 12% increase in the odds of having any meniscal tear (OR, 1.12; 95% CI, 1.02-1.22; P = .016), depicted in Figure 2, and a 10% increase in the odds of having a lateral meniscal tear (OR, 1.10; 95% CI, 1.01-1.19; P = .028). Mean BMI for patients with a meniscal tear 24.2 kg/m2 and for patients without a meniscal tear was 23.0 kg/m2 (P = .01). BMI did not predict the presence of an isolated medial meniscal tear (OR, 1.04; 95% CI, 1.00-1.09; P = .07).
Figure 2.
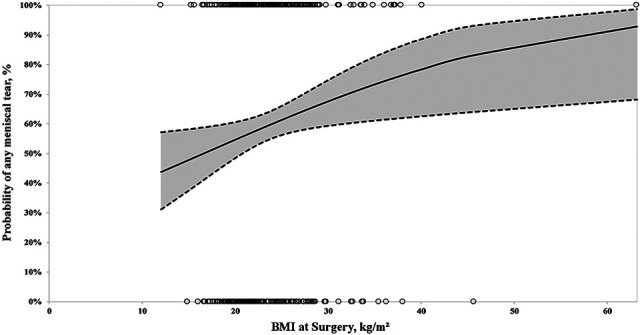
Predicted probability plot of any meniscal tear by body mass index (BMI). Circles represent the BMIs of individual patients who did have a meniscus tear (circles along 100% line) and did not have a meniscus tear (circles along 0% line). The solid line represents the predicted probability of any meniscus tear for each given BMI. The dashed lines represent the standard error of the predicted probability.
The date of injury was available for 417 patients (92%), and time from injury to surgery was calculated and ranged from 1 to 338 weeks. Median time from injury to surgery and corresponding interquartile ranges are presented in Table 2. Surgery was performed within 6 weeks of injury in 43% of patients and within 12 weeks of injury in 72% of patients. Of the patients, 6% had surgery more than 1 year after their initial injury. Time from injury to surgery was not a predictor of a lateral meniscal tear (P = .839) or a medial meniscal tear (P = .083).
Table 2.
Time From Injury to Surgery (Days)a
| n | Median (IQR) | |
|---|---|---|
| Overall | 417 | 48 (32-91) |
| LM tear | 141 | 47 (32-84) |
| MM tear | 51 | 47 (31-94) |
| LM and MM tears | 44 | 58 (37-131) |
| No meniscal tear | 170 | 47 (31-95) |
aIQR, interquartile range; LM, lateral meniscus; MM, medial meniscus.
Discussion
This study sought to evaluate the relationship between age and BMI and the presence of a meniscal tear in pediatric patients undergoing ACLR. It was observed that age was a risk factor for a meniscal tear, with a 16% increase in the risk of having any meniscal tear per 1-year increase in age from 9 to 18 years. Subgroup analysis among these patients undergoing ACLR revealed there was a 20% increase in the odds of having a medial meniscal tear and 16% increase in the odds of having a lateral meniscal tear for each 1-year increase in age. Furthermore, every 2 point increase in BMI was associated with a 12% increase in the odds of having any meniscal tear and 10% increase in the odds of having a lateral meniscal tear. Time from injury to surgery was not identified as having a statistically significant association with meniscal tears, with a median time to surgery of 48 days.
Studies including patients of all ages have shown that older age, male sex, increased body weight, and increased time from injury to surgery have all been associated with an increased risk of meniscal tears in patients undergoing ACLR. In a large prospective cohort of patients undergoing ACLR, the Multicenter Orthopaedic Outcomes Network (MOON) noted an incidence of concomitant meniscal injury slightly higher than our overall study population, with 66% of their patients identified as having meniscal tears.32 This series included a wide range in patient ages (11-63 years), with a mean of 24 years. However, if we compare our older patients (aged 17-18 years) to the MOON cohort, we have very similar rates of concomitant meniscal injuries (60%-70%). Other large cohorts including patients aged 14 to 78 years have reported similar rates of meniscal pathology in ACL-deficient knees.5,28,30 In a retrospective review of 764 patients (mean age, 27 years; range, 14-59 years) with ACL tears undergoing arthroscopy, Tandogan et al28 noted a significant relationship between age and the presence of a medial meniscal tear. This relationship has been noted in other studies, all with a wide range of patient ages in the cohorts.9,14,23 Neither study demonstrated age or BMI to be independent risk factors.
The question remains as to whether these risk factors are similar in the pediatric population. In the largest pediatric study to assess the association of age and meniscal tears, Dumont et al8 identified that among 370 patients, 57% had lateral meniscal tears and 43% had medial meniscal tears at the time of ACL surgery. Patients aged >15 years had a significantly higher rate of medial meniscal tears at the time of ACL surgery as well as a trend for increasing meniscal tear rate with age. In other pediatric studies, Samora et al24 evaluated 142 patients with ACL tears with a mean age of 14 years and found that 69% had a meniscal tear at the time of surgery, while Anderson and Anderson2 noted meniscal tears in 83% of 135 adolescents with ACL-deficient knees. In a similar but smaller study, Vavken et al31 described the presence of concomitant injuries in 208 pediatric patients undergoing ACLR. The authors identified 59% of patients as having a concomitant injury (meniscal tear or chondral injury), but identified no association with age. In cohorts of pediatric and adult patients, male sex was a predictor for a higher rate of both medial and lateral meniscal tears.4 We did not find that to be true in our pediatric cohort.
Increasing BMI has been correlated to increased rates of concomitant meniscal pathology. In adolescents with ACL tears, Raad et al21 showed a positive correlation between BMI and concomitant meniscal lesions, and Dumont et al8 noted that a weight >65 kg led to an increased risk of both medial and lateral meniscal tears. Vavken et al31 noted an 8% increased risk of a medial meniscal tear per 1 unit increase in BMI, but no association between lateral meniscal tears. Similarly, Patel et al20 found that children with an elevated BMI had a higher rate of concurrent meniscal tears compared with normal BMI (76% vs 70%). Among our pediatric patients, we demonstrated a significantly increased risk of concomitant medial and lateral meniscal pathology with increasing BMI, even within healthy ranges.
Multiple studies have evaluated timing from injury to surgery as a risk factor for meniscal injury.12,14,15,17 Specific to pediatric patients, Millet et al16 noted a 25% increase in medial meniscal tears among patients undergoing surgery more than 6 weeks after injury. Vavken et al31 noted a 6% increased risk of medial meniscal tears per month delay to surgery but no increased risk of lateral meniscal pathology with delay. Guenther et al10 noted that a longer interval between injury and surgery was associated with not only an increased likelihood of a medial meniscal tear but also of a higher severity grade tear. Likewise, Anderson and Anderson2 evaluated the impact of subacute (6-12 weeks) and delayed (>12 weeks) ACLR in patients aged <17 years and found increasing rates and severity of medial and lateral meniscal tears and chondral pathology as compared to acute reconstruction. Unlike these studies, we identified no association between time from injury to surgery and the presence of medial or lateral meniscal tears in our large pediatric cohort. It is important to note, however, that 75% of patients in our series had surgery within 3 months of injury, and the effects of longer delays to surgery may not be fully elucidated in this study. The increased risk of meniscal tears reported in other studies suggests that increasing time to surgery is associated with a return to cutting and pivoting activities in an ACL-deficient knee. With increased awareness of ACL injuries and a larger presence of certified athletic trainers in schools in our region, we are hopeful that our finding represents improvements in return-to-play guidance and safety offered by the certified athletic trainers in our local schools as well as educational efforts in our community.
Advancements in MRI quality have helped surgeons in the preoperative detection of meniscal tears, but MRI is still not perfect, and intra-articular injuries may be missed.18 Laundre et al13 evaluated MRI reports of 120 patients who underwent ACLR and found MRI was correct in detecting a meniscal tear in 76% of cases. The majority of missed tears were found in the posterior horn of the lateral meniscus, a finding which has also been seen in other similar studies.25,33 In a pediatric population, MRI had a sensitivity of 59% and specificity of 91% in characterizing meniscal tears compared to what was identified at arthroscopy.24 Given the high rate of concomitant meniscal pathology identified among our pediatric cohort, it is vital for the surgeon to critically inspect and probe the meniscus, especially in older adolescent patients, regardless of the MRI findings.
This study is the largest pediatric ACLR cohort to quantify the risk of meniscal injury by age and BMI. The main limitations of this study relate to the retrospective review of intraoperative findings. The presence of a meniscal tear was obtained from the operative report with the intraoperative assessment subject to the operating surgeon. It is conceivable that some small and superficial meniscal tears had healed between the time of injury and surgery, perhaps slightly underestimating the true incidence of concomitant meniscal tears. This study only evaluated age, sex, time from injury to surgery, and BMI as potential risk factors, but other variables such as sport and injury mechanism could also be risk factors of concomitant meniscal injuries. Larger cohort size studies are needed to evaluate which risk factors are correlated with different tear locations, patterns, and treatments.
Conclusion
The presence of a concomitant meniscal injury is quite common in pediatric patients with an ACL tear, found in our series to be 58%. In this population, the presence of a concomitant meniscal tear was associated with increasing age and BMI but not time from injury to surgery. Meniscal pathology at the time of ACLR is present at a significantly greater rate in adolescents aged >13 years compared to those aged 13 years and younger. For every 1-year increase in age from 7 to 18 years, there is a 16% increase in the odds of having a meniscal tear. Furthermore, each 2.0-unit increase in BMI is associated with a 12% increase in the odds of having a meniscal tear. Patient and family preoperative education should include a discussion regarding potential meniscal treatment, implications for rehabilitation, and long-term sequela. In the pediatric population, there should be a high index of suspicion and careful arthroscopic assessment for meniscal injuries at the time of ACLR.
Footnotes
Final revision submitted August 26, 2020; accepted September 25, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: C.A.P. has received research funding from DJO and OrthoPediatrics and education payments from Smith & Nephew and Arthrex. M.A.C. has received research funding from DJO and OrthoPediatrics and education payments Smith & Nephew. M.T.B. has received research support from OrthoPediatrics and education payments and nonconsulting fees from Arthrex. S.C.W. has received research support from OrthoPediatrics, education payments from Arthrex, and nonconsulting fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Children’s Healthcare of Atlanta Institutional Review Board.
References
- 1. Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH. Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med. 2011;39(10):2187–2193. [DOI] [PubMed] [Google Scholar]
- 2. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):275–281. [DOI] [PubMed] [Google Scholar]
- 3. Bellabarba C, Bush-Joseph CA, Bach BR, Jr. Patterns of meniscal injury in the anterior cruciate-deficient knee: a review of the literature. Am J Orthop (Belle Mead NJ). 1997;26(1):18–23. [PubMed] [Google Scholar]
- 4. Brambilla L, Pulici L, Carimati G, et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med. 2015;43(12):2966–2973. [DOI] [PubMed] [Google Scholar]
- 5. Chhadia AM, Inacio MC, Maletis GB, et al. Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med. 2011;39(9):1894–1899. [DOI] [PubMed] [Google Scholar]
- 6. Church S, Keating JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87(12):1639–1642. [DOI] [PubMed] [Google Scholar]
- 7. Cruz AI, Jr, Gao B, Ganley TJ, et al. Trends in concomitant meniscal surgery among pediatric patients undergoing ACL reconstruction: an analysis of ABOS Part II candidates from 2000 to 2016. Orthop J Sports Med. 2019;7(9):2325967119869848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med. 2012;40(9):2128–2133. [DOI] [PubMed] [Google Scholar]
- 9. Ghodadra N, Mall NA, Karas V, et al. Articular and meniscal pathology associated with primary anterior cruciate ligament reconstruction. J Knee Surg. 2013;26(3):185–193. [DOI] [PubMed] [Google Scholar]
- 10. Guenther ZD, Swami V, Dhillon SS, Jaremko JL. Meniscal injury after adolescent anterior cruciate ligament injury: how long are patients at risk? Clin Orthop Relat Res. 2014;472(3):990–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Herzog MM, Marshall SW, Lund JL, et al. Trends in incidence of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States, 2002-2014. Sports Health. 2018;10(6):523–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kay J, Memon M, Shah A, et al. Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3738–3753. [DOI] [PubMed] [Google Scholar]
- 13. Laundre BJ, Collins MS, Bond JR, et al. MRI accuracy for tears of the posterior horn of the lateral meniscus in patients with acute anterior cruciate ligament injury and the clinical relevance of missed tears. AJR Am J Roentgenol. 2009;193(2):515–523. [DOI] [PubMed] [Google Scholar]
- 14. Mansori AE, Lording T, Schneider A, et al. Incidence and patterns of meniscal tears accompanying the anterior cruciate ligament injury: possible local and generalized risk factors. Int Orthop. 2018;42(9):2113–2121. [DOI] [PubMed] [Google Scholar]
- 15. Michalitsis S, Vlychou M, Malizos KN, Thriskos P, Hantes ME. Meniscal and articular cartilage lesions in the anterior cruciate ligament-deficient knee: correlation between time from injury and knee scores. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):232–239. [DOI] [PubMed] [Google Scholar]
- 16. Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18(9):955–959. [DOI] [PubMed] [Google Scholar]
- 17. Mok YR, Wong KL, Panjwani T, et al. Anterior cruciate ligament reconstruction performed within 12 months of the index injury is associated with a lower rate of medial meniscus tears. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):117–123. [DOI] [PubMed] [Google Scholar]
- 18. Munger AM, Gonsalves NR, Sarkisova N, et al. Confirming the presence of unrecognized meniscal injuries on magnetic resonance imaging in pediatric and adolescent patients with anterior cruciate ligament tears. J Pediatr Orthop. 2019;39(9):e661–e667. [DOI] [PubMed] [Google Scholar]
- 19. Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. [DOI] [PubMed] [Google Scholar]
- 20. Patel NM, Talathi NS, Bram JT, DeFrancesco CJ, Ganley TJ. How does obesity impact pediatric anterior cruciate ligament reconstruction? Arthroscopy. 2019;35(1):130–135. [DOI] [PubMed] [Google Scholar]
- 21. Raad M, Thevenin Lemoine C, Berard E, et al. Delayed reconstruction and high BMI z score increase the risk of meniscal tear in paediatric and adolescent anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):905–911. [DOI] [PubMed] [Google Scholar]
- 22. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42(11):2769–2776. [DOI] [PubMed] [Google Scholar]
- 23. Ridley TJ, McCarthy MA, Bollier MJ, Wolf BR, Amendola A. Age differences in the prevalence of isolated medial and lateral meniscal tears in surgically treated patients. Iowa Orthop J. 2017;37:91–94. [PMC free article] [PubMed] [Google Scholar]
- 24. Samora WP, 3rd, Palmer R, Klingele KE. Meniscal pathology associated with acute anterior cruciate ligament tears in patients with open physes. J Pediatr Orthop. 2011;31(3):272–276. [DOI] [PubMed] [Google Scholar]
- 25. Sharifah MI, Lee CL, Suraya A, et al. Accuracy of MRI in the diagnosis of meniscal tears in patients with chronic ACL tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):826–830. [DOI] [PubMed] [Google Scholar]
- 26. Shieh A, Bastrom T, Roocroft J, Edmonds EW, Pennock AT. Meniscus tear patterns in relation to skeletal immaturity: children versus adolescents. Am J Sports Med. 2013;41(12):2779–2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shybut TB, Vega CE, Haddad J, et al. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2015;43(4):905–911. [DOI] [PubMed] [Google Scholar]
- 28. Tandogan RN, Taser O, Kayaalp A, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12(4):262–270. [DOI] [PubMed] [Google Scholar]
- 29. Tepolt FA, Feldman L, Kocher MS. Trends in pediatric ACL reconstruction from the PHIS database. J Pediatr Orthop. 2018;38(9):e490–e494. [DOI] [PubMed] [Google Scholar]
- 30. Unay K, Akcal MA, Gokcen B, et al. The relationship between intra-articular meniscal, chondral, and ACL lesions: finding from 1,774 knee arthroscopy patients and evaluation by gender. Eur J Orthop Surg Traumatol. 2014;24(7):1255–1262. [DOI] [PubMed] [Google Scholar]
- 31. Vavken P, Tepolt FA, Kocher MS. Concurrent meniscal and chondral injuries in pediatric and adolescent patients undergoing ACL reconstruction. J Pediatr Orthop. 2018;38(2):105–109. [DOI] [PubMed] [Google Scholar]
- 32. Westermann RW, Wright RW, Spindler KP, et al. Meniscal repair with concurrent anterior cruciate ligament reconstruction: operative success and patient outcomes at 6-year follow-up. Am J Sports Med. 2014;42:2184–2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wong KP, Han AX, Wong JL, Lee DY. Reliability of magnetic resonance imaging in evaluating meniscal and cartilage injuries in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):411–417. [DOI] [PubMed] [Google Scholar]
- 34. Wyatt RW, Inacio MC, Liddle KD, Maletis GB. Factors associated with meniscus repair in patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(12):2766–2771. [DOI] [PubMed] [Google Scholar]


