Abstract
Objectives
All countries impacted by COVID-19 have had to change routine health service delivery. Although this has reversed some of the progress made in reducing the global burden of tuberculosis (TB) disease, there is an opportunity to incorporate lessons learned to improve TB programmes going forward.
Approach
We use Pakistan as a case study to discuss three important adaptations in light of COVID-19: bringing care closer to patients; strengthening primary health care systems; and proactively addressing stigma and fear.
Findings
COVID-19 control in Pakistan has restricted people’s ability to travel and this has forced the TB programme to reduce the need for in-person health facility visits and bring care closer to patients’ homes. Strategies that may be useful for providing more convenient care to patients in the future include: : remote treatment support using telemedicine; collaborating with private healthcare providers; and establishing community medicine collection points. As part of the response to COVID-19 in Pakistan, the out-patient departments of major tertiary and secondary care hospitals were closed, and this highlighted the importance of strengthening primary healthcare for both better pandemic and TB control. Finally, stigma associated with COVID-19 and TB can be addressed using trusted community-based health workers, such as Lady Health Workers in Pakistan.
Keywords: COVID-19, Tuberculosis, Primary health care, Community, Stigma, Pakistan
Introduction
The COVID-19 pandemic has within the time course of one year reversed the progress made in reducing the global burden of tuberculosis (TB). Globally, TB case notifications have declined by 25% and TB deaths are estimated to have increased by 0.2 to 0.4 million (Glaziou, 2020, World Health Organization, 2020). All countries impacted by COVID-19 have had to change the way they deliver routine services (World Health Organisation, 2020), and there is an opportunity to incorporate lessons learned to improve TB programmes going forward. We use Pakistan as a case study to discuss three important adaptations: bringing care closer to patients; strengthening primary care; and proactively addressing stigma and fear.
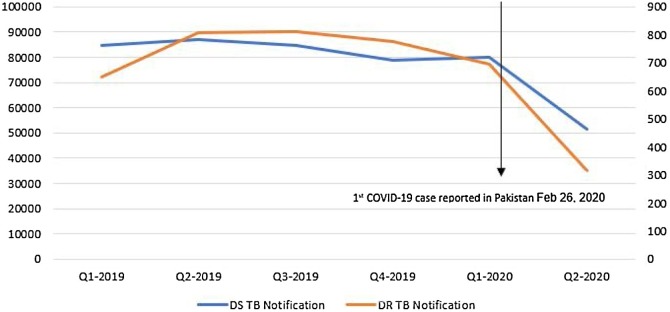
In response to COVID-19 in Pakistan, during the localised smart lockdown between March-June 2020, the out-patient departments of major tertiary and secondary care hospitals were closed to minimize disease transmission to other patients and health care professionals (HCP). To maintain uninterrupted services and improve patient access, out-patient services for illnesses other than COVID-19 were shifted to primary health care centres. Between February and April 2020, there were substantial declines in the case notification of drug-susceptible TB by 45% and of drug-resistant TB by 35%. Figure 1 shows Pakistan TB notifications before and during COVID-19.
Figure 1.
Pakistan TB notifications before and during COVID-19.
Bringing care closer to patients
COVID-19 control has involved restrictions on travel, which required the Pakistan National TB Programme (NTP) to introduce adaptations to bring care closer to patients’ homes. The NTP started providing medications for longer durations to reduce the number of health facility visits required (National TB Control Program, 2020a). Such efforts could be supplemented by bringing services closer to patients by establishing community medicine collection points (Shrinivasan et al., 2020), delivering medicines to homes (National TB Control Program, 2020b) and the use of telemedicine (Khan et al., 2020, Shrinivasan et al., 2020).
Private HCP, including doctors and drug sellers, are often located close to residential areas and they provide a convenient place to access healthcare in Pakistan. Improving the management and reporting of TB by private HCP, and developing partnerships with the NTP, is another way to bring care closer to patients. To engage HCP, a Mandatory TB Case Notification Act has been approved by three large provinces in Pakistan, namely Sindh, Khyber Pakhtunkhwa, & Punjab. Within this, an innovative strategy is being initiated to link private HCP with the NTP through an electronic on-line mandatory TB case notification system: evaluations of this initiative will be informative.
Furthermore, intensified TB case finding strategies can potentially narrow the gap between estimated TB incidence in communities and TB case notifications. Strategies used by the NTP include active TB screening as well as screening for both COVID-19 and TB in persons with cough and fever, especially in identified hot spot areas (Fatima and Yaqoob, 2020).
Strengthening primary care and supporting HCP
Primary health care represents the core of Pakistan’s health delivery system and is essential for delivery of care in epidemics and pandemics around the world. An assessment of HCP carried out between May-June 2020 and primary level health care facilities throughout Pakistan revealed poor knowledge regarding infection and prevention control (IPC), inadequate logistics to ensure uninterrupted supplies of drugs and consumables and low adherence to IPC measures (National TB Control Program, 2020c). To better implement TB infection control measures at each facility, the NTP trained HCP on proper use of personal protective equipment and this was supplemented by comprehensive educational modules on infection control which were prepared and delivered through online training to field staff.
Proactively addressing stigma and fears
The similarity of symptoms of TB and COVID-19 (cough, fever and shortness of breath) poses the risk of increased stigma for people with TB or respiratory symptoms. The NTP has been urging the TB control community to quickly adapt and strengthen TB service provision to maximise the health and safety of vulnerable TB patients and TB HCP during these unprecedented times. Since Lady Health Workers (LHWs) in Pakistan are closely embedded and trusted health care workers in rural communities (Hafeez et al., 2011) and have the capacity to learn additional skills, the NTP has recently taken steps to engage this cadre for effective delivery of key TB interventions at the community level. This new paradigm of engagement has the potential to strengthen the district health system and at the same time provides an opportunity to integrate primary health centre services within the NTP with the aim of increasing TB case detection.
Conclusion
COVID-19 has provided an opportunity to introduce some TB service adaptations and move ahead on long-standing goals, such as bringing care closer to communities, investing in human resources and addressing stigma. We believe that a multi-pronged approach is essential, and, as always, progress relies on political commitment, strategic planning, community engagement and research & development.
Funding Source
No specific funding was available or obtained from any organization for this study.
Ethical Approval
Local ethical was also waived off from IRB, ethics committee, common management unit (HIV, TB and Malaria).
Conflict of Interest
The current “Instructions to Authors” have been read by all authors, thereby indicating compliance with those instructions and acceptance of the conditions posed. Authors have seen and agreed to the submitted version of the paper, all who have been acknowledged as contributors or as providers of personal communications have agreed to their inclusion, the material is original and it has been neither published nor submitted for publication and is not under consideration for publication elsewhere. If accepted, the paper will not be published elsewhere in the same form, in English or in any other language, without written consent of the copyright holder.
There are no conflicts of interest.
Transparency declaration
This article is part of a supplement entitled Commemorating World Tuberculosis Day March 24th, 2021: “The Clock is Ticking” published with support from an unrestricted educational grant from QIAGEN Sciences Inc.
References
- Fatima R., Yaqoob A. In Reply: How TB and COVID-19 compare: An opportunity to integrate both control programmes. Int J Tuberc Lung Dis. 2020;24:1227–1228. doi: 10.5588/ijtld.20.0571. [DOI] [PubMed] [Google Scholar]
- Glaziou P. Predicted impact of the COVID-19 pandemic on global tuberculosis deaths in 2020. MedRxiv. 2020 2020.04.28.20079582. [Google Scholar]
- Hafeez A., Mohamud B.K., Shiekh M.R., Shah S.A.I., Jooma R. Lady health workers programme in Pakistan: Challenges, achievements and the way forward. J Pak Med Assoc. 2011;61:210–215. [PubMed] [Google Scholar]
- Khan M., Rego S., Rajal J.B., Bond V., Fatima R.K. Mitigating the impact of COVID-19 on tuberculosis and HIV services: a cross-sectional survey of 669 health professionals in 64 low and middle-income countries. MedRxiv. 2020 doi: 10.1371/journal.pone.0244936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National TB Control Program . Ministry of Health; Islamabad, Pakistan: 2020. TB Advosiry during COVID-19 Outbreak. [Google Scholar]
- National TB Control Program . Ministry of Health; Islamabad, Pakistan: 2020. TB Advisory during COVID-19 Outbreak. [Google Scholar]
- National TB Control Program . Ministry of Health; Islamabad, Pakistan: 2020. RAPID ASSESSMENT OF INFECTION PREVENTION & CONTROL AMID COVID-19 CRISIS AT PHC LEVEL TB CARE FACILITIES ACROSS PAKISTAN. [Google Scholar]
- Shrinivasan R., Rane S., Pai M. India’s syndemic of tuberculosis and COVID-19. BMJ Glob Heal. 2020;5 doi: 10.1136/bmjgh-2020-003979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation . WHO; Geneva, Switzerland: 2020. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report. [Google Scholar]
- World Health Organization . WHO; Geneva, Switzerland: 2020. Global Tuberculosis Report 2020. [Google Scholar]