Abstract
Background
Malnutrition is inevitable in patients with Coronavirus Disease 2019 (COVID-19) due to its effect on the gastrointestinal system, immune system, and high metabolic activity. However, the prevalence of malnutrition and its outcomes is uncertain. This study aimed to investigate the prevalence and outcome of malnutrition among patients with COVID-19.
Method
A comprehensive search was conducted in PubMed/Medline; Science direct and LILACS from December 29, 2019 to September, 2020 without language restriction. All observational studies reporting the prevalence of malnutrition were included while case reports and reviews were excluded. The data were extracted with two independent authors with a customized format and the disagreements were resolved by the other authors. The methodological quality of included studies was evaluated using a standardized critical appraisal tool.
Results
A total of 511 articles were identified from different databases and 27 articles were selected for evaluation after the successive screening. Fourteen articles with 4187 participants were included. The pooled prevalence of malnutrition among hospitalized patients with COVID-19 was 49.11% (95% CI: 31.67 to 66.54). The odd of mortality among patients COVID-19 with malnutrition was 10 times more likely as compared to those who were well-nourished.
Conclusion
The prevalence of malnutrition and mortality associated with malnutrition among COVID-19 hospitalized patients was very high which entails a mitigating strategy by different stakeholders to prevent and manage malnutrition and its outcomes.
Registration
This systematic review was registered in Prospero's international prospective register of systematic reviews (CRD42020215396).
Keywords: Malnutrition, Mortality, Prevalence, NUTRIC, COVID-19
1. Background
The Coronavirus Disease 2019 (COVID-19) pandemic which is caused by the severe acute respiratory syndrome virus-2 (SARS-CoV-2) infection was identified in Wuhan, Hubei province of China in December 2019 by the Chinese Center for Disease and Prevention from the throat swab of a patient [29]. Though the disease has emerged in China, it widespread worldwide unpredictably and it was declared as a global pandemic by the World Health Organization (WHO) as of March 11, 2020 [13].
The World Health Organization (WHO) situation report showed that there were approximately 50 million laboratory-confirmed cases and more than 1 million deaths globally as of November 6, 2020.
The Coronavirus Disease 2019 (COVID-19) was thought to affect mainly the respiratory system and is presented with fever, dry cough, and difficulty of breathing, and lately, the patient may deteriorate associated with pneumonia and acute respiratory distress syndrome [29,34,35,64]. However, recent evidence showed clinical manifestations on the gastrointestinal tract, immune, cardiovascular, dermatologic, and central nervous systems [3,6,21,24,31,43,59,60].
The Coronavirus Disease 2019 (COVID-19) causes significant economic, social, psychological chaos globally due to incompliant to preventive measures, unproven treatment, and the complexity of its transmission [17,45,48,57,62]. These impacts are thought to be disastrous for low-income countries because of very poor health care system, low awareness of the disease and its prevention, lack of skilled health personnel, scarce Intensive Care Unit, a limited number of mechanical ventilators, and prevalence of co-morbidities/infection along with high prevalent chronic malnutrition [8,14,49,62].
Different studies showed that patients with co-morbidities including (Asthma, COPD, Tuberculosis, Pneumonia, Acute respiratory distress syndrome (ARDS), Diabetes mellitus, hypertension, renal disease, hepatic disease, and cardiac disease), history of smoking, and history of substance use, male gender and age greater than 60 years were more likely to die or develop undesirable outcomes [22,44,52,65].
Different systemic reviews and observational studies showed that malnutrition among critically ill patients is as high as 70% which was strongly related to mortality, hospital length of stay, and duration of mechanical ventilation [6,14,20,25,28,31,[33], [34], [35], [36], [37], [38], [39]].
Malnutrition is inevitable in patients with Coronavirus Disease 2019 (COVID-19) due to its effect on the gastrointestinal disorder, immune system, high metabolic activity due to infection, fever, and less oral intake.
Malnutrition during COVID-19 is a ‘two-edged sword’ particularly in low-income countries where chronic malnutrition is very high. The disease is still very high and it is relapsing to the worst in some countries. However, the prevalence of malnutrition and its outcomes is uncertain and a topic of debate. Therefore, this systematic review and meta-analysis aimed to investigate the prevalence and outcome of malnutrition among patients with COVID-19.
2. Methods
2.1. Protocol and registration
The systematic review and meta-analysis was conducted based on the Preferred Reporting Items for Systematic and meta-analysis (PRISMA) protocols [46], and the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) checklist [58]. This systematic review and meta-analysis was registered in Prospero's international prospective register of systematic reviews (CRD42020215396) on October 23, 2020.
2.2. Eligibility criteria
All observational (case series, cross-sectional, cohort, and case–control) studies reporting the prevalence of malnutrition and outcomes among hospitalized patients with coronavirus disease (COVID-19) were included while studies that didn't report the prevalence of malnutrition among hospitalized patients with COVID-19, articles that didn't report full information for data extraction, articles with different outcomes of interest, and Systemic review study design were excluded. The methodological quality of included studies was evaluated with eight item appraisal tool adopted from Joanna Briggs institute as mentioned in methodological quality assessment section and studies with a methodological score less than fifty percent were also excluded. The primary outcomes of interest were the prevalence of malnutrition and mortality among hospitalized patients with COVID-19 worldwide. The prevalence of comorbidities and lengths of hospital stay were secondary outcomes.
2.3. Search strategy
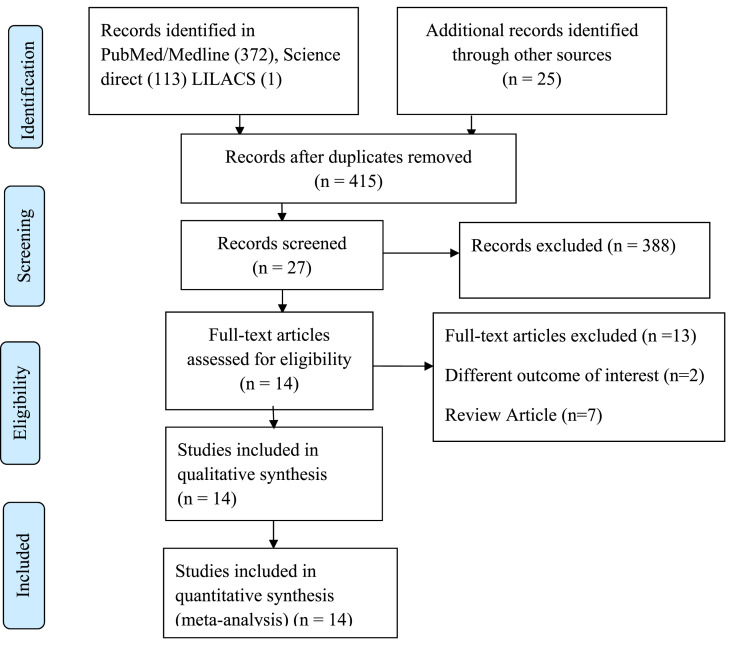
The search strategy was conducted to explore all available published and unpublished studies among surgical COVID-19 patients admitted to the hospital from December 2019 to September 2020 without language restrictions. A comprehensive search was employed in this review. An initial search on PubMed/Medline, Science Direct, and Cochrane Library was carried out followed by an analysis of the text words contained in Title/Abstract and indexed terms. A second search was undertaken by combining free text words and indexed terms with Boolean operators. The third search was conducted with the reference lists of all identified reports and articles for additional studies. Finally, an additional and grey literature search was conducted on Google scholars. The databases were searched with the following search terms using PICos (population, interest, context and design) strategy by combining with AND, OR Boolean operators as COVID-19 OR novel coronavirus OR SARS-CoV-2 AND malnutrition OR undernutrition OR deficiency OR hunger AND mortality OR death OR outcomes AND comorbidity OR complication AND prevalence OR incidence. The final search results were shown with the Prisma flow diagram (Fig. 1 ).
Fig. 1.
Prisma flow chart.
2.4. Data extraction
The data from each study were extracted by SA and YC independently with a customized format excel sheet. The disagreements between the two independent authors were resolved by the other authors. The extracted data included: Author names, country, date of publication, sample size, the prevalence of malnutrition, mortality, the number of days in the hospital, presence of co-morbidities, screening/diagnostic malnutrition tools, and determinants. Finally, the data were then imported for analysis in R software version 4.0.2 and STATA 16.
2.5. Assessment of methodological quality
Articles identified for retrieval were assessed by two independent Authors for methodological quality before inclusion in the review using a standardized critical appraisal Tool adapted from the Joanna Briggs Institute (Supplemental Table 1). The disagreements between the Authors appraising the articles were resolved through discussion. Articles with average scores greater than fifty percent were included for data extraction.
2.6. Data analysis
Data analysis was carried out in R statistical software version 4.0.2 and STATA 16. The pooled prevalence of malnutrition, mortality, and length of hospital stay among hospitalized patients with COVID-19 was determined with a random effect model with restricted maximum likely hood (REML) as there was substantial heterogeneity. The Heterogeneity among the included studies was checked with forest plot, χ2 test, I2 test, and the p-values. Substantial heterogeneity among the included studies was investigated with subgroup analysis for categorical moderators (nutritional status screening/assessment tools, setting, country, and age group) and meta-regression for continuous covariates (lengths of stay, mean age, and sample size) for outcomes extracted from more than ten studies.
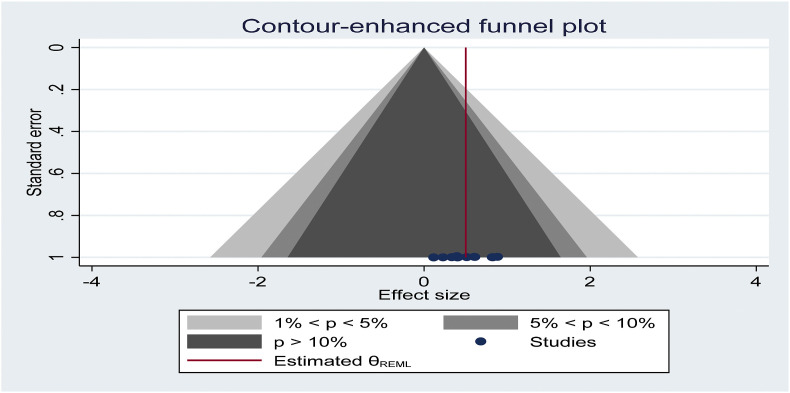
Publication bias was checked with a funnel plot and the objective diagnostic test was conducted with Egger's correlation, Begg's regression tests. Furthermore, factor analysis was carried out to identify the independent predictors of malnutrition among hospitalized patients with COVID-19.
3. Results
3.1. Selection of studies
A total of 511 articles were identified from different databases and 27 articles were selected for evaluation after the successive screening. Fourteen articles with 4187 participants were included and the rest were excluded with reasons [4,5,[9], [10], [11],19,20,23,26,32,53,55,56](Fig. 1).
3.2. Description of included studies
Fourteen Articles with 4187 participants were included in the review while thirteen studies were included in the meta-analysis for the prevalence of malnutrition and mortality. The Studies with the prevalence of malnutrition and/or prevalence of mortality among hospitalized patients with COVID-19 were included and the characteristics of each included studies were described in (Table 1 ) and the rest were excluded with reasons.
Table 1.
Description of included studies.
| Author | Study period | Country | Sample | Setting | Tools | Age group | P (95% CI) |
|---|---|---|---|---|---|---|---|
| Bedock et al., 2020 [7] | March 21 to April 24, 2020 | France | 144 | Hospital | GLIM | Adult | 82.81 [79.17,86.45] |
| Du et al., 2020 [16] | Jan 1 to Feb 29, 2020 | China | 155 | Hospital | CONUT | Adult | 41.13 [33.01,49.26] |
| Li et al., 2020 [38] | Jan 2 to Feb 15,2020 | China | 523 | Hospital | mNUTRIC | Adult | 61.03 [52.83,69.23] |
| Li et al., 2020 [37] | Jan to Feb, 2020 | China | 187 | Hospital | MNA | >65 | 82.13 [78.55,85.70] |
| Lin et al., 2020 [40] | Jan 20 to Feb 23, 2020 | China | 33 | Hospital | Albumin | Adult | 52.75 [45.49,60.00] |
| Liu et al., 2020 [41] | Jan 28 to March 5, 2020 | China | 141 | Hospital | MUST | >65 | 40.34 [36.14,44.55] |
| Luo et al., 2020 [42] | Feb to April,2020 | China | 1115 | Hospital | prealbumin | Adult | 88.39 [83.34,93.43] |
| Pironi et al., 2020 [50] | April 2020 | Italy | 268 | Hospital | NRS | Adult | 11.57 [9.69,13.45] |
| Recinella et al., 2020 [51] | March 30 to May 15, 2020 | Italy | 109 | Hospital | GNRI | >65 | 22.76 [17.74,27.78] |
| Rouget et al., 2020 [54] | March to April 2020 | France | 80 | Hospital | GLIM | Adult | 33.33 [25.63,41.03] |
| Wang et al., 2020 [63] | Jan to Feb, 2020 | China | 442 | Hospital | CONUT | Adult | 60.55 [51.38,69.73] |
| Zhang et al., 2020 [66] | Jan 28 to Feb 21, 2020 | China | 136 | ICU | mNUTRIC | Adult | 39.39 [22.72,56.07] |
| Zhao et al., 2020 [67] | Jan 29 to Feb 19, 2020 | China | 413 | Hospital | NRS | Adult | 37.50 [26.89,48.11] |
| Zuo et al., 2020 [68] | Jan 17 to Feb 17, 2020 | China | 446 | Hospital | prealbumin | >65 | 33.18 [28.81,37.55] |
The included studies were published from January 01 to May 15, 2020, with sample sizes, ranged from 33 to 1115. The mean (±SD) ages of the included studies varied from 54.2 ± 15.9 to 83.38 ± 3.9 years. The mean (±SD) length of hospital stay was varied from 7.63 ± 1.38 to 30.18 ± 11.06 days. The Majority of studies were conducted among hospitalized patients while one study was conducted among malnourished intensive care unit COVID-19 patients.
The included studies used different types of malnutrition screening and diagnostic tools including Nutritional Risk Screening (NRS2000), Global Leadership Initiative on Malnutrition (GLIM), Controlling Nutritional status (CONUT), Mini Nutritional Assessment (MNA), modified Nutritional Risk in the critically Ill (MNUTRIC), Malnutrition Universal Screening Tool (MUST), Geriatric Nutritional Risk Index (GNRI), Anthropometric (Body Mass Index, Mid Upper arm circumference, Skinfolds), and Biological markers (albumin, prealbumin, globulin).
Ten of the included studies were conducted in China while the rest four studies were conducted in France and Italy, two studies in each country.
All of the included studies reported the prevalence of malnutrition among hospitalized patients with COVID-19 which varied from 11.57% to 88.39% while six of the included studies reported the prevalence of mortality among malnourished hospitalized COVID-19 patients. The prevalence of mortality among undernourished patients with COVID-19 from the included studies varied from 10% to 59.09%.
Six of the included studies with 1143 participants reported the prevalence of comorbidity including hypertension, diabetes mellitus, cardiovascular disease, cancer, COPD, and cerebrovascular disease as the major comorbidity among malnourished patients with COVID-19 while five studies with 961 participants reporting the prevalence of gastrointestinal symptoms including nausea, vomiting, diarrhea, anorexia, Anosmia, and dysgueusia.
4. Meta-analysis
4.1. Prevalence of malnutrition
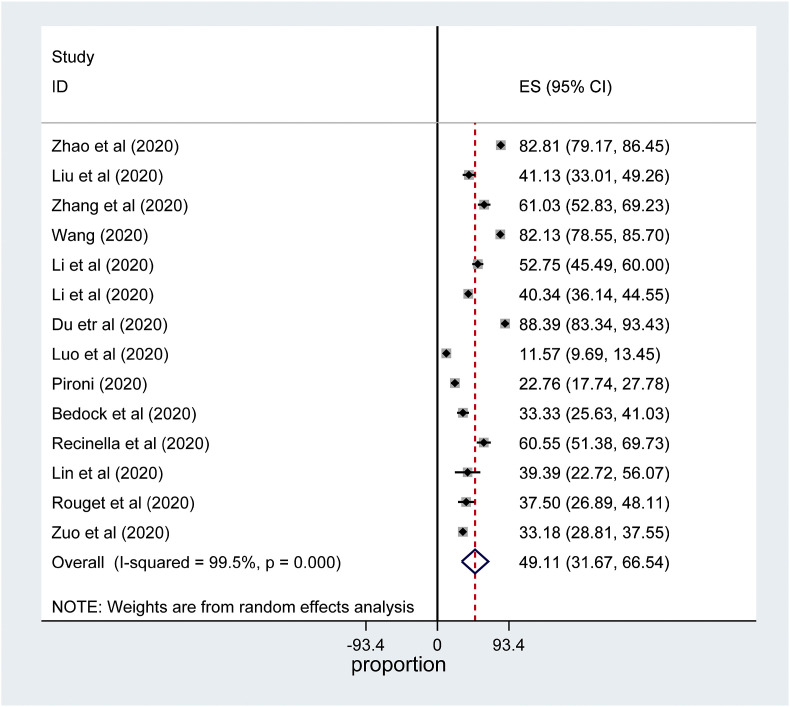
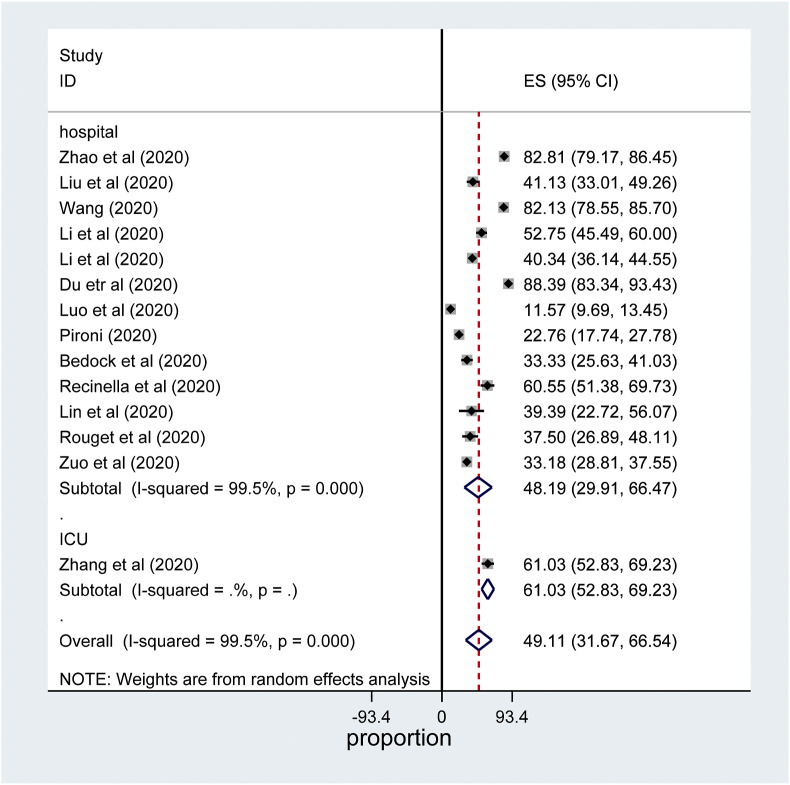
All of the included studies reported the prevalence of malnutrition among hospitalized patients with COVID-19. The pooled prevalence of malnutrition among hospitalized patients with COVID-19 was 49.11% (95% CI: 31.67 to 66.54, 14 studies, and 4187 participants) (Fig. 2 ).
Fig. 2.
Forest plot for the prevalence of malnutrition among hospitalized patients with COVID-19: The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval, and the diamond shows the pooled prevalence.
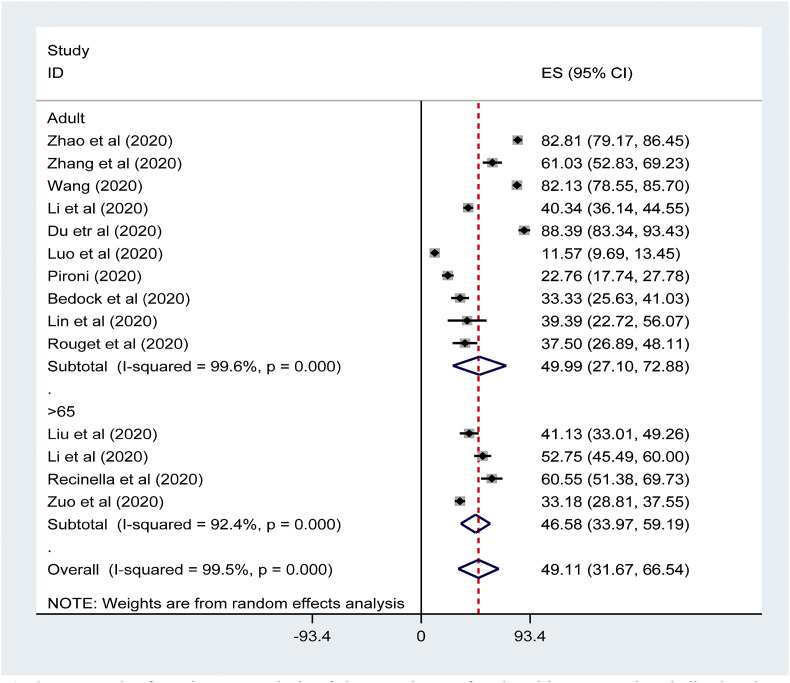
The sub-group analysis was conducted by country, setting, Nutritional assessment and screening tools, and age group. The sub-group analysis revealed that prevalence of malnutrition was comparable among elderly patients (>65 years) as compared to adult patients (18–65 years), 46.5% (95% confidence interval (CI):33.97–59.19%) and 49.99% (95% confidence interval (CI):27.10–72.88%) respectively (Fig. 3 ). The prevalence of malnutrition among hospitalized patients with COVID-19 was found to be higher in China followed by Italy, 53.34% (95% confidence interval (CI): 31.17–75.50%) and 41.45% % (95% confidence interval (CI):4.42 to 78.48) respectively (Supplemental Fig. 1).
Fig. 3.
Forest plot for subgroup analysis of the prevalence of malnutrition among hospitalized patients with COVID-19 by age group: The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval, and the diamond shows the pooled prevalence.
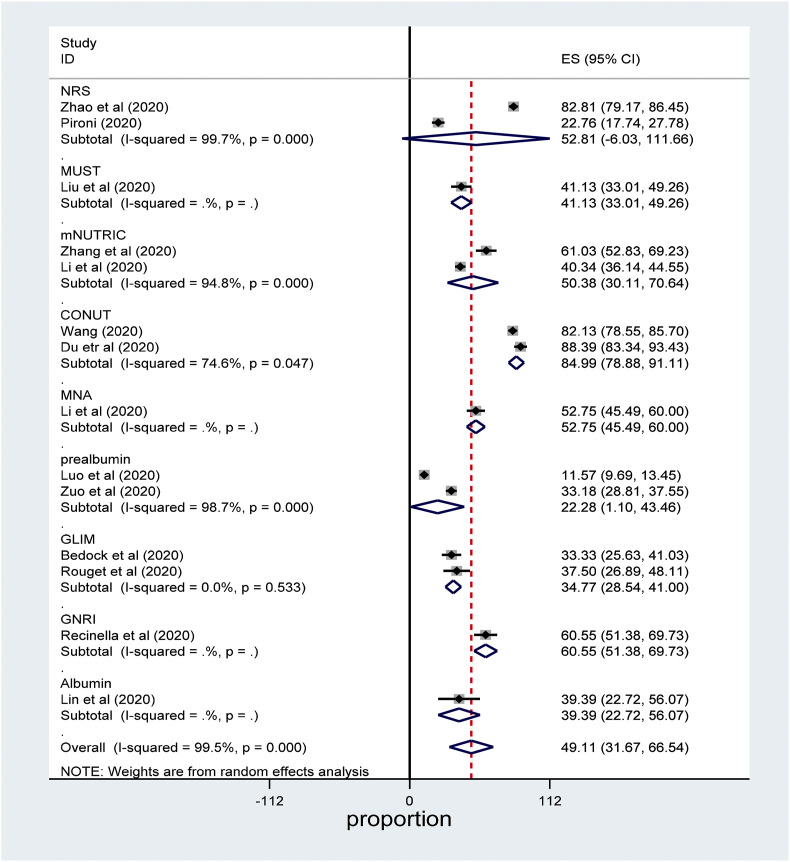
The meta-analysis also revealed that the prevalence of malnutrition among hospitalized patients with COVID-19 was the highest with CONUT, GNRI, NRS2000 nutritional status screening, and assessment tools while the prevalence of malnutrition was the lowest with GLIM, albumin, and prealbumin (Fig. 4 ).
Fig. 4.
Forest plot for subgroup analysis of the prevalence of malnutrition among hospitalized patients with COVID-19 by country: The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval, and the diamond shows the pooled prevalence.
The subgroup analysis showed that the pooled prevalence of malnutrition was the highest among critically ill patients as compared to general ward patients; 61.03% (95% confidence interval (CI):52.83–69.23%) and 48.19% (95% confidence interval (CI): 29.91–66.47%) respectively (Fig. 5 ).
Fig. 5.
Forest plot for the prevalence of perioperative complication among surgical patients with COVID-19: The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval, and the diamond shows the pooled prevalence.
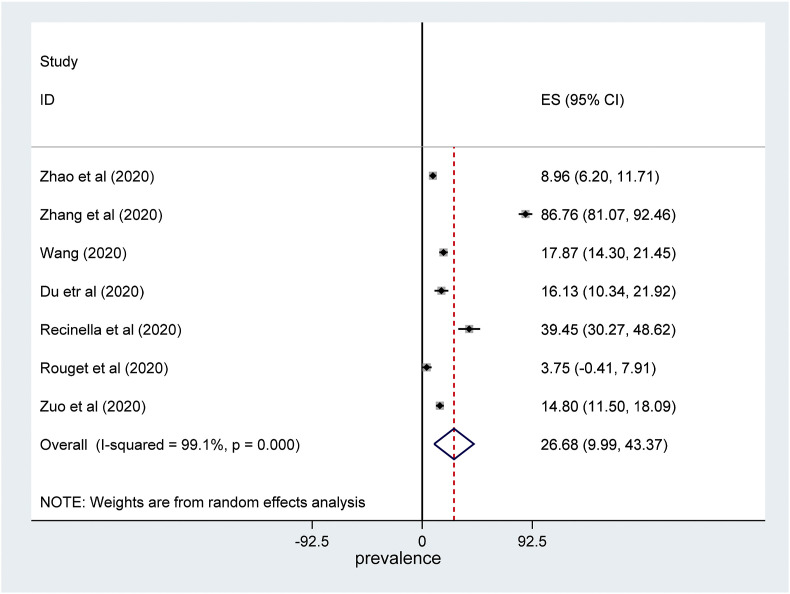
4.2. Mortality and morbidity
The meta-analysis showed that the prevalence of malnutrition was 26.68% (95% confidence interval (CI): 9.99 to 43.37, 6 studies, 1781 participants) (Fig. 6 ). The odd of mortality among patients with hospitalized malnutrition patients with COVID-19 was 10 times more likely as compared to those who were not malnourished (Supplemental Fig. 2). The prevalence of individual comorbidity including hypertension, diabetes mellitus, cardiovascular disease were the most common comorbidities respectively but we didn't perform overall prevalence of comorbidity as the included studies didn't report the overall prevalence of comorbidity.
Fig. 6.
Forest plot for the prevalence of mortality among hospitalized malnourished patients with COVID-19: The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval, and the diamond shows the pooled prevalence.
4.3. Mean duration of hospitalization
The pooled mean duration of hospitalization was estimated from the included studies mean duration of hospitalization. The meta-analysis revealed that the mean duration of Hospitalization was 12.18 (95% confidence interval (CI): 8.57–15.79) days (Supplemental Fig. 3).
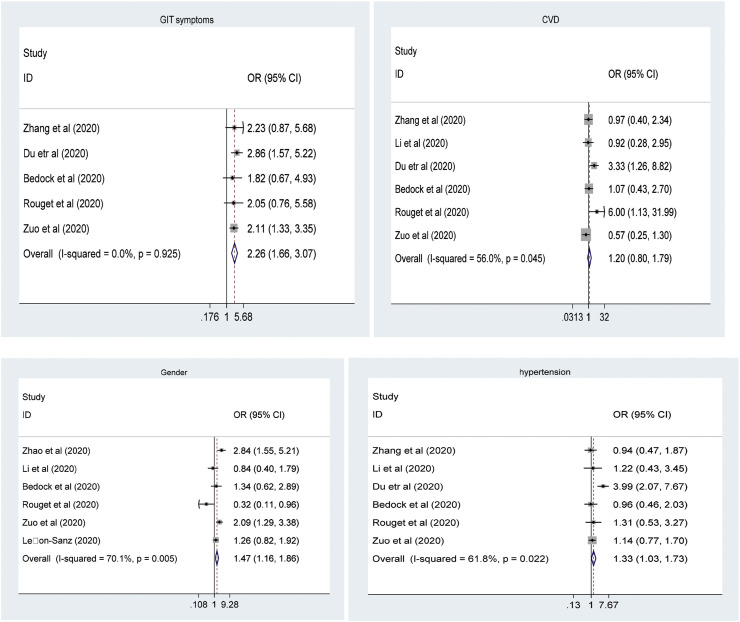
4.4. Determinants of malnutrition
This study identified different independent predictors of malnutrition including gastrointestinal symptoms (nausea, vomiting, and anorexia), comorbidity (hypertension, cardiovascular disease), and being male gender. The meta-analysis revealed that patients with gastrointestinal symptoms were more than 2 times more likely to develop malnutrition compared to their counterparts (Fig. 7 ).
Fig. 7.
Forest plot showing pooled odds ratio (log scale) of the associations between malnutrition and its determinants (GIT symptoms; Gender; CVD; Hypertension).
4.5. Meta-regression
The meta-analysis showed a substantial heterogeneity between the included studies which entails subgroup analysis and/or meta-regression to identify the sources of heterogeneity. Regression Analysis was run for the prevalence of malnutrition with the only length of hospital stay covariates because the other covariates were reported in less than ten included studies where the meta-regression model fit couldn't be certain. However, it was not possible to explain the source of heterogeneity (I2 = 99.22, tau2 = 687, p = 0.000). The model revealed that 99.22% of the residual variation was due to real heterogeneity while only 0.78% of the variation may be due to within-study sampling variability.
4.6. Sensitivity analysis and publication bias
Sensitivity analysis was conducted to identify the most influential study on the pooled summary effect by removing each study at a time and we didn't find a significant influencing summary effect. The funnel plot didn't show significant publication bias. Besides, egger's regression and Begg's correlation rank correlation failed to show a significant difference (p = 0.7634 and p = 1.1733) respectively (Fig. 8 ).
Fig. 8.
Funnel plot to assess publication bias. The vertical line indicates the effect size whereas the diagonal line indicates the precision of individual studies with a 95% confidence interval.
5. Discussion
This meta-analysis was intended to provide evidence on prevalence, independent predictors, and outcomes of malnutrition among hospitalized patients with COVID-19 for prevention and early intervention in compliance with local guidelines.
The meta-analysis revealed that the prevalence of malnutrition was 49.11% (95% CI: 31.67–66.54) which was comparable with the included studies. However, studies conducted among hospitalized patients before the COVID-19 era showed that the prevalence of malnutrition was lower than this meta-analysis which varied from 22 to 40% [1,15,30,61]. This discrepancy might be explained by the impact of COVID-19 disease on the gastrointestinal tract and immunity besides high metabolic rate and decreased oral intake.
Body of evidence showed that malnutrition is very high among elderly hospitalized patients [1,12,25,27,28,33,39], unlike this systematic review and meta-analysis where the prevalence of malnutrition between elderly and adult patients is comparable. The possible explanation might be because of the inclusion of a small number of studies conducted on the elderly; only four studies were conducted on the elderly from a total of 14 studies.
The meta-analysis showed that the prevalence of malnutrition among hospitalized patients with COVID-19 was the highest with CONUT, GNRI, and NRS2000 nutritional status screening and assessment tools while the prevalence of malnutrition was the lowest with GLIM, albumin, and prealbumin which is in line with studies conducted on the predictability of nutritional screening and assessment tools. Studies showed that biological markers are a poor predictor of nutritional status as these indices might be affected by critical illness, infection, liver, and renal disease in which case albumin and prealbumin will rise irrespective of nutritional status [2,18,47].
The subgroup analysis revealed that malnutrition is the highest among ICU critically ill patients when compared to general ward patients which are comparable with studies conducted in ICU among non-COVID-19 patients [12,30,36]. These patients are critically ill with a high metabolic rate due to the inflammatory process, fever, prolonged length of stay, inadequate calorie intake.
The systematic review found out independent predictors of malnutrition among hospitalized patients with COVID-19 including hypertension, gastrointestinal symptoms, being male, and cardiovascular disease. This study showed that patients having gastrointestinal symptoms were 2.26 times more likely to be malnourished as compared to their counterparts.
5.1. Quality of evidence
The methodological quality of included studies was moderate to high quality as illustrated with the Joanna Briggs Institute assessment tool for meta-analysis of observational studies. However, substantial heterogeneity associated with dissimilarities of included studies in nutritional screening/assessment tools, study setting, age group, and sample size, could affect the allover quality of evidence.
5.2. Implication for policy
Body of evidence revealed that the prevalence of malnutrition and its outcomes was very high among hospitalized patients with COVID-19. Hospital malnutrition in patients with COVID-19 is a huge challenge particularly in low and middle-income countries because of prevalent chronic malnutrition, poverty, inadequate and or no nutritional support at all in some countries, and lack of local nutritional support protocol. Therefore, a mitigating strategy is required by different stakeholders to prevent and manage malnutrition and its and its consequences by screening/assessing nutritional status, involving the nutritionist/dietitian, and adopting nutritional support guidelines.
5.3. The implication for further research
The meta-analysis revealed that the prevalence of malnutrition and its outcomes was very high among hospitalized COVD-19. However, the included studies were too heterogeneous, low powered and cross-sectional studies also don't show a temporal relationship between malnutrition, mortality, and its determinants. Therefore, further observational and randomized controlled trials with more validated nutritional status screening and assessment tools are required.
5.4. Limitation of the study
The meta-analysis included studies with moderate to high methodological quality. However, some of the included studies were low-powered and the majority of studies included in this review didn't report data on outcomes of malnutrition, comorbidity, and risk factors to investigate the independent predictors. Besides, the included studies used different types of screening and assessment nutritional tools and it would be difficult to provide conclusive evidence.
6. Conclusion
This meta-analysis showed that the prevalence of malnutrition was very high among hospitalized patients with COVID-19. The meta-analysis showed that mortality among hospitalized patients with COVID-19 was more than 10 times more likely as compared to those who were well-nourished. This entails a mitigating strategy by different stakeholders to prevent and manage malnutrition and its outcomes.
Ethics approval and consent to participate
Ethical clearance and approval were obtained from the ethical review board of the College of Health Science and Medicine.
Consent for publication
Not applicable.
Availability of data and materials
Data and material can be available where appropriate.
Funding
No funding was obtained from any organization.
Authors' contributions
SA and MB conceived the idea design of the project. SA, YC, HA, RH, and KH were involved in searching strategy, data extraction, quality assessment, analysis, and manuscript preparation. All authors read and approved the manuscript.
Declaration of competing interest
The authors declare that there are no competing interests.
Acknowledgments
The authors would like to acknowledge Dali University for technical support and encouragement to carry out the project.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.clnesp.2021.03.002.
Abbreviations
- ARDS
Acute Respiratory Distress Syndrome
- CI
Confidence Interval
- CONUT
Controlling Nutritional status
- COPD
Chronic Obstructive Pulmonary Disease
- CVD
Cardiovascular Disease
- GIT
Gastrointestinal Tract
- GLIM
Global Leadership Initiative on Malnutrition
- GNRI
Geriatric Nutritional Risk Index
- ICU
Intensive care Unit
- MNA
Mini Nutritional Assessment
- mNUTRIC
modified Nutritional Risk in the critically Ill
- MOOSE
Meta-Analysis of Observational Studies in Epidemiology
- MUST
Malnutrition Universal Screening Tool
- NRS2000
Nutritional Risk Screening 2000
- OR
odds Ratio
- PRISMA
Preferred Reporting Items for Systematic and meta-analysis
- SD
Standard Deviation
- WHO
World Health Organization
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Alzahrani S.H., Alamri S.H. Prevalence of malnutrition and associated factors among hospitalized elderly patients in King Abdulaziz University Hospital, Jeddah, Saudi Arabia. BMC Geriatr. 2017;17:136. doi: 10.1186/s12877-017-0527-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arbab K., Majid H., Jafri L., Akram B., Raheem A., Jamil B. Assessing nutritional status of critically ill patients using serum Prealbumin levels. J Ayub Med Coll Abbottabad. 2019;31:178–181. [PubMed] [Google Scholar]
- 3.Asadi-Pooya A.A., Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020:116832. doi: 10.1016/j.jns.2020.116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azzolino D., Saporiti E., Proietti M., Cesari M. Nutritional considerations in frail older patients with COVID-19. J Nutr Health Aging. 2020;1 doi: 10.1007/s12603-020-1400-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barazzoni R., Bischoff S.C., Breda J., Wickramasinghe K., Krznaric Z., Nitzan D. Elsevier; 2020. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Basu-Ray I., Soos M.P. StatPearls Publishing; 2020. Cardiac manifestations of coronavirus (COVID-19). StatPearls [Internet] [PubMed] [Google Scholar]
- 7.Bedock D., Lassen P.B., Mathian A., Moreau P., Couffignal J., Ciangura C. Prevalence and severity of malnutrition in hospitalized COVID-19 patients. Clinical Nutrition ESPEN. 2020;40:214–219. doi: 10.1016/j.clnesp.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bong C.-L., Brasher C., Chikumba E., Mcdougall R., Mellin-Olsen J., Enright A. The COVID-19 pandemic: effects on low-and middle-income countries. Anesth Analg. 2020 doi: 10.1213/ANE.0000000000004846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caccialanza R., Laviano A., Lobascio F., Montagna E., Bruno R., Ludovisi S. Early nutritional supplementation in non-critically ill patients hospitalized for the 2019 novel coronavirus disease (COVID-19): rationale and feasibility of a shared pragmatic protocol. Nutrition. 2020:110835. doi: 10.1016/j.nut.2020.110835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cena H., Maffoni S., Braschi V., Brazzo S., Pallavicini C., Vietti I. Position paper of the Italian association of medical specialists in dietetics and clinical nutrition (ANSISA) on nutritional management of patients with COVID-19 disease. Mediterr J Nutr Metabol. 2020:1–5. [Google Scholar]
- 11.Chimera B., Potani I., Daniel A.I., Chatenga H. Clinical nutrition care challenges in low-resource settings during the COVID-19 pandemic: a focus on Malawi. J Global Health. 2020;10 doi: 10.7189/jogh.10.020363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Correia M.I.T., Perman M.I., Waitzberg D.L. Hospital malnutrition in Latin America: a systematic review. Clin Nutr. 2017;36:958–967. doi: 10.1016/j.clnu.2016.06.025. [DOI] [PubMed] [Google Scholar]
- 13.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed: Atenei Parmensis. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Da’ar O.B., Haji M., Jradi H. Coronavirus Disease 2019 (COVID-19): potential implications for weak health systems and conflict zones in the Middle East and North Africa region. Int J Health Plann Manag. 2020;35:1240–1245. doi: 10.1002/hpm.2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Delgado A.F. Hospital malnutrition and inflammatory response in critically ill children and adolescents admitted to a tertiary intensive care unit. Clinics. 1980;63(3):357–362. doi: 10.1590/S1807-59322008000300012. ISSN, 5322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Du X., Liu Y., Chen J., Peng L., Cheng Z., Wang H.H. Comparison of the clinical implications among two different nutritional indices in hospitalized patients with COVID-19. medRxiv. 2020 doi: 10.1101/2020.04.28.20082644. [DOI] [Google Scholar]
- 17.Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A. Fair allocation of scarce medical resources in the time of Covid-19. Mass Medical Soc. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 18.Espahbodi F., Khoddad T., Esmaeili L. Evaluation of malnutrition and its association with biochemical parameters in patients with end stage renal disease undergoing hemodialysis using subjective global assessment. Nephro-Urol Mon. 2014;6 doi: 10.5812/numonthly.16385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fedele D., De francesco A., Riso S., Collo A. Obesity, malnutrition, and trace element deficiency in the coronavirus disease (COVID-19) pandemic: an overview. Nutrition. 2020;81:111016. doi: 10.1016/j.nut.2020.111016. 111016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fernández-Quintela A., Milton-Laskibar I., Trepiana J., Gómez-Zorita S., Kajarabille N., Léniz A. Key aspects in nutritional management of COVID-19 patients. J Clin Med. 2020;9:2589. doi: 10.3390/jcm9082589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gu J., Han B., Wang J. COVID-19: gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology. 2020;158:1518–1519. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guan W.-J., Liang W.-H., Zhao Y., Liang H.-R., Chen Z.-S., Li Y.-M. Comorbidity and its impact on 1590 patients with covid-19 in China: a nationwide analysis. Eur Respir J. 2020;55 doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guerra R.S., Fonseca I., Sousa A.S., Jesus A., Pichel F., Amaral T.F. ESPEN diagnostic criteria for malnutrition–a validation study in hospitalized patients. Clin Nutr. 2017;36:1326–1332. doi: 10.1016/j.clnu.2016.08.022. [DOI] [PubMed] [Google Scholar]
- 24.Hajifathalian K., Krisko T., Mehta A., Kumar S., Schwartz R., Fortune B. Gastrointestinal and hepatic manifestations of 2019 novel coronavirus disease in a large cohort of infected patients from New York: clinical implications. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holst M., Yifter-Lindgren E., Surowiak M., Nielsen K., Mowe M., Carlsson M. Nutritional screening and risk factors in elderly hospitalized patients: association to clinical outcome? Scand J Caring Sci. 2013;27:953–961. doi: 10.1111/scs.12010. [DOI] [PubMed] [Google Scholar]
- 26.Huizar M.I., Arena R., Laddu D.R. The global food syndemic: the impact of food insecurity, malnutrition and obesity on the healthspan amid the COVID-19 pandemic. Prog Cardiovasc Dis. 2020;82(4):784–791. doi: 10.1016/j.pcad.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kagansky N., Berner Y., Koren-Morag N., Perelman L., Knobler H., Levy S. Poor nutritional habits are predictors of poor outcome in very old hospitalized patients. Am J Clin Nutr. 2005;82:784–791. doi: 10.1093/ajcn/82.4.784. [DOI] [PubMed] [Google Scholar]
- 28.Kaiser M.J., Bauer J.M., Rämsch C., Uter W., Guigoz Y., Cederholm T. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010;58:1734–1738. doi: 10.1111/j.1532-5415.2010.03016.x. [DOI] [PubMed] [Google Scholar]
- 29.Kakodkar P., Kaka N., Baig M. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19) Cureus. 2020;12 doi: 10.7759/cureus.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kang M.C., Kim J.H., Ryu S.-W., Moon J.Y., Park J.H., Park J.K. Prevalence of malnutrition in hospitalized patients: a multicenter cross-sectional study. J Kor Med Sci. 2017;33 doi: 10.3346/jkms.2018.33.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kumar A., Arora A., Sharma P., Anikhindi S.A., Bansal N., Singla V. Gastrointestinal and hepatic manifestations of Corona Virus Disease-19 and their relationship to severe clinical course: a systematic review and meta-analysis. Indian J Gastroenterol. 2020:1–17. doi: 10.1007/s12664-020-01058-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.kyle U.G., Genton L., Heidegger C.P., Maisonneuve N., Karsegard V.L., Huber O. Hospitalized mechanically ventilated patients are at higher risk of enteral underfeeding than non-ventilated patients. Clin Nutr. 2006;25:727–735. doi: 10.1016/j.clnu.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 33.Lara-Pulido A., Guevara-Cruz M. Malnutrition and associated factors in elderly hospitalized. Nutr Hosp. 2012;27:652–655. doi: 10.1590/S0212-16112012000200044. [DOI] [PubMed] [Google Scholar]
- 34.lechien J.R., Chiesa-Estomba C.M., De Siati D.R., Horoi M., Le Bon S.D., Rodriguez A. European Archives of Oto-Rhino-Laryngology; 2020. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study; pp. 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lechien J.R., Chiesa-Estomba C.M., Place S., Van laethem Y., Cabaraux P., Mat Q. Clinical and epidemiological characteristics of 1,420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 2020;288(3):335–344. doi: 10.1111/joim.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lew C.C.H., Yandell R., Fraser R.J., Chua A.P., Chong M.F.F., Miller M. Association between malnutrition and clinical outcomes in the intensive care unit: a systematic review. J Parenter Enteral Nutr. 2017;41:744–758. doi: 10.1177/0148607115625638. [DOI] [PubMed] [Google Scholar]
- 37.Li G., Zhou C.-L., Ba Y.-M., Wang Y.-M., Song B., Cheng X.-B. Nutritional risk and therapy for severe and critical COVID-19 patients: a multicenter retrospective observational study. Clin Nutr. 2020 doi: 10.1016/j.clnu.2020.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li T., Zhang Y., Gong C., Wang J., Liu B., Shi L. Prevalence of malnutrition and analysis of related factors in elderly patients with COVID-19 in Wuhan, China. Eur J Clin Nutr. 2020:1–5. doi: 10.1038/s41430-020-0642-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ligthart-Melis G.C., Luiking Y.C., Kakourou A., Cederholm T., Maier A.B., De Van Der Schueren M.A. Frailty, sarcopenia, and malnutrition frequently (Co-) occur in hospitalized older adults: a systematic review and meta-analysis. J Am Med Dir Assoc. 2020 doi: 10.1016/j.clnu.2020.09.040. [DOI] [PubMed] [Google Scholar]
- 40.Lin L., Hu K., Cai S., Deng X., Shao X., Liang Y. Hypoproteinemia is an independent risk factor for the prognosis of severe COVID-19 patients. J Clin Biochem Nutr. 2020:20–75. doi: 10.3164/jcbn.20-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu G., Zhang S., Mao Z., Wang W., Hu H. Clinical significance of nutritional risk screening for older adult patients with COVID-19. Eur J Clin Nutr. 2020:1–8. doi: 10.1038/s41430-020-0659-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luo Y., Xue Y., Mao L., Yuan X., Lin Q., Tang G. Prealbumin as a predictor of prognosis in patients with coronavirus disease 2019. Front Med. 2020;7 doi: 10.3389/fmed.2020.00374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA neurology. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mao R., Liang J., Shen J., Ghosh S., Zhu L.-R., Yang H. Implications of COVID-19 for patients with pre-existing digestive diseases. Lancet Gastroenterol & hepatol. 2020;5:426–428. doi: 10.1016/S2468-1253(20)30076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mckibbin W.J., Fernando R. 2020. The global macroeconomic impacts of COVID-19: seven scenarios. [Google Scholar]
- 46.Moher D., Liberati A., tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 47.Morey V.M., Song Y.D., Whang J.S., Kang Y.G., Kim T.K. Can serum albumin level and total lymphocyte count be surrogates for malnutrition to predict wound complications after total knee arthroplasty? J Arthroplasty. 2016;31:1317–1321. doi: 10.1016/j.arth.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 48.Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Paintsil E. COVID-19 threatens health systems in sub-Saharan Africa: the eye of the crocodile. J Clin Invest. 2020;130 doi: 10.1172/JCI138493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pironi L., Sasdelli A.S., Ravaioli F., Baracco B., Battaiola C., Bocedi G. Malnutrition and nutritional therapy in patients with SARS-CoV-2 disease. Clin Nutr. 2020;32:2695–2701. doi: 10.1016/j.clnu.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Recinella G., Marasco G., Serafini G., Maestri L., Bianchi G., Forti P. Prognostic role of nutritional status in elderly patients hospitalized for COVID-19: a monocentric study. Aging Clin Exp Res. 2020:1–7. doi: 10.1007/s40520-020-01727-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., Mcginn T., Davidson K.W. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. Jama. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Romano L., Bilotta F., Dauri M., Macheda S., Pujia A., De Santis G. Short Report–Medical nutrition therapy for critically ill patients with COVID-19. Eur Rev Med Pharmacol Sci. 2020;24:4035–4039. doi: 10.26355/eurrev_202004_20874. [DOI] [PubMed] [Google Scholar]
- 54.Rouget A., Vardon-Bounes F., Lorber P., Vavasseur A., Marion O., Marcheix B. 2020. Prevalence of malnutrition in COVID-19 inpatients: the Nutricov study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Silva D.F.O., Lima S.C.V.C., Sena-Evangelista K.C.M., Marchioni D.M., Cobucci R.N., Andrade F.B.D. Nutritional risk screening tools for older adults with COVID-19: a systematic review. Nutrients. 2020;12:2956. doi: 10.3390/nu12102956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Silverio R., Gonçalves D.C., Andrade M.F., Seelaender M. Coronavirus disease 2019 (COVID-19) and nutritional status: the missing link? Adv Nutr. 2020:1–11. doi: 10.1093/advances/nmaa125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Spinelli A., Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg. 2020;107(7):785–787. doi: 10.1002/bjs.11627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Jama. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 59.Tang K., Wang Y., Zhang H., Zheng Q., Fang R., Sun Q. Dermatologic therapy; 2020. Cutaneous manifestations of the Coronavirus Disease 2019 (COVID-19): a brief review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thakkar S., Arora S., Kumar A., Jaswaney R., Faisaluddin M., Din M.A.U. medRxiv; 2020. A systematic review of the cardiovascular manifestations and outcomes in the setting of coronavirus-19 disease. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Waitzberg D.L., Caiaffa W.T., Correia M.I.T. Hospital malnutrition: the Brazilian national survey (IBRANUTRI): a study of 4000 patients. Nutrition. 2001;17:573–580. doi: 10.1016/s0899-9007(01)00573-1. [DOI] [PubMed] [Google Scholar]
- 62.Walker P.G., Whittaker C., Watson O.J., Baguelin M., Winskill P., Hamlet A. The impact of COVID-19 and strategies for mitigation and suppression in low-and middle-income countries. Science. 2020;369:413–422. doi: 10.1126/science.abc0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang R., He M., Yue J., Bai L., Liu D., Huang Z. 2020. CONUT score is associated with mortality in patients with COVID-19: a retrospective study in Wuhan. [Google Scholar]
- 64.Woelfel R., Corman V.M., Guggemos W., Seilmaier M., Zange S., Mueller M.A. MedRxiv; 2020. Clinical presentation and virological assessment of hospitalized cases of coronavirus disease 2019 in a travel-associated transmission cluster. [Google Scholar]
- 65.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang P., He Z., Yu G., Peng D., Feng Y., Ling J. The modified NUTRIC score can be used for nutritional risk assessment as well as prognosis prediction in critically ill COVID-19 patients. Clin Nutr. 2020;40(2):534–541. doi: 10.1016/j.clnu.2020.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhao X., Li Y., Ge Y., Shi Y., Lv P., Zhang J. Evaluation of nutrition risk and its association with mortality risk in severely and critically ill COVID-19 patients. J Parenter Enteral Nutr. 2020;78:110930. doi: 10.1002/jpen.1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zuo P., Tong S., Yan Q., Cheng L., Li Y., Song K. Burbank; Los Angeles County, Calif: 2020. Decreased prealbumin level is associated with increased risk of mortality in hospitalized elderly patients with COVID-19. Nutrition. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and material can be available where appropriate.