Abstract
Purpose
In March 2020, the World Health Organization declared the SARS-CoV-2 infection-related coronavirus Disease (COVID-19) a pandemic. During the first and second waves of the pandemic spread, there have been several reports of COVID-19-associated neurological manifestations, including acute seizures and status epilepticus (SE). In this systematic review, we summarized the available data on clinical features, diagnosis, and therapy of COVID-19-related SE.
Methods
We performed a systematic search of the literature to identify data on demographics, clinical, neurophysiological, and neuroradiological data of patients with COVID-19-related SE. We used regression models (linear or logistic) with a stepwise forward method to identify features associated with mortality or severity of SE.
Results
Thirty-nine articles were included with a total of 47 cases of SE associated with COVID-19. Age, time between the acute respiratory phase of SARS-CoV-2 infection and SE onset, and hospitalization correlated with a higher SE severity as assessed by quantitative validated scales.
Conclusions
SE can be a neurological manifestation of SARS-CoV-2 infection. Although a possible association between SE and COVID-19 has been reported, the exact mechanisms are still not fully understood. Systemic inflammatory syndrome due to cytokine release could play a role in COVID-19-related SE.
Keywords: Epilepsy, Status epilepticus, SARS-CoV-2 infection, Pandemic
1. Introduction
Coronavirus disease 2019 (COVID-19) pandemic related to the infection by the novel coronavirus (SARS-CoV-2) is a challenging health emergency. Among the symptoms included in the COVID-19 disease spectrum, neurological manifestations have been frequently reported, including anosmia, ageusia, encephalopathies, stroke, epileptic seizures, and Status Epilepticus (SE) [1]. The neuroinvasive and neurotropic properties of SARS-CoV-2 have been questioned [2], and the neurologic picture is considered the consequence of an inflammatory response related to SARS-CoV-2 infection (“cytokine released syndrome” or “cytokine storm”). Increased levels of circulating cytokine and immune-cell hyperactivation could lead to secondary organ dysfunction and eventually to a life-threatening systemic inflammatory syndrome [3].
Acute symptomatic epileptic seizures and Status Epilepticus (SE) are two of the neurological conditions most frequently reported in association with SARS-CoV-2 infection and carry a high rate of mortality (between 5% and 39%) [4]. The management of SE during COVID-19 infection is particularly challenging, due to the unavailability of an electroencephalogram (EEG) in many COVID-19 units, the possible drug-to-drug interactions between antiviral treatments and anti-seizure medications (ASMs) [5], and the well-known respiratory suppression properties of benzodiazepines, which are the first-line treatment of SE.
In this systematic review, we summarize the available data on clinical features, diagnosis, and therapy of SE associated with COVID-19.
2. Methods
2.1. Searching strategy and review organization
Results of this systematic review have been reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The final study protocol was registered in the PROSPERO international prospective register of systematic reviews (https://www.crd.york.ac.uk/PROSPERO/, registration number CRD42020223305).
The following electronic databases and data sources were systematically searched: MEDLINE (accessed through PubMed), EMBASE, and Google Scholar (from December 2019 to January 2021). In all databases we used the following search strategy: ('epileptic state'/exp OR 'epileptic state') AND ('coronavirus disease 2019′/exp OR 'coronavirus disease 2019′). We included all studies reporting cases of SE in the context of COVID-19 syndrome in patients with or without a previous history of epilepsy, published in English, and reporting individual patient data. Non-peer reviewed papers were excluded.
The quality of studies included in the quantitative analysis was assessed using the Newcastle-Ottawa Quality Assessment Scale (NOS). This score ranges from 0 to 9, with studies getting scores ≥5 were regarded as good quality studies [6]. Nine reviewers (B.N., J.L., G.E., F.R., R.S., L.T., S.T., M.D.P., and M.R.) independently screened the retrieved articles for possible inclusion. Disagreements were discussed collegially and resolved through discussion. Data were extracted on a digital spreadsheet.
We extracted and collected the following individual patient data: age, gender, previous history of epilepsy, comorbidities, time between the onset of respiratory and/or gastrointestinal symptoms of COVID-19 and SE onset (time to SE, TtSE), intra-hospital (IHO), or extra-hospital (EHO) occurrence of SE, SE etiology (acute symptomatic, remote symptomatic, progressive symptomatic, unknown/not specified), brain computerized tomography (TC) and magnetic resonance image (MRI) findings, EEG findings, laboratory findings, COVID-19-specific treatments, SE treatments, SE duration, and outcome. Some categorical variables were additionally taken into account: use of steroids (Yes/No), use of anesthetics (Yes/No), and pathological CSF findings (Yes/No). Based on the clinical description, the Status Epilepticus Severity Score (STESS) and Epidemiology-based Mortality score in SE (EMSE) were calculated for each case by the reviewers. The full list of variables used for statistical analysis and missing data are reported in Supp.Tab.1.
3. Statistics
Statistical analysis was performed on the final dataset containing all information pooled from the included studies. Normality of continuous data was checked via Kolmogorov–Smirnov test, and a linear (Forward Stepwise) regression analysis was fitted to describe the relation of all clinical data with STESS and EMSE scores. We used logistic (Forward Stepwise) regression to describe how clinical variables modify the odds of survival and resolution of SE. To further confirm significant findings, we used an ANOVA to compare differences in clinical features between patients according to the number of ASMs and age group (0–25 years; 25–65 years; over 65 years), and t-test to compare clinical features between patients who survived and those who did not. Alpha level was set at 0.05 for statistical significance. Cases with insufficient information to calculate STESS and EMSE were not included in statistical analysis. Data were analyzed using IBM SPSS™.
4. Results
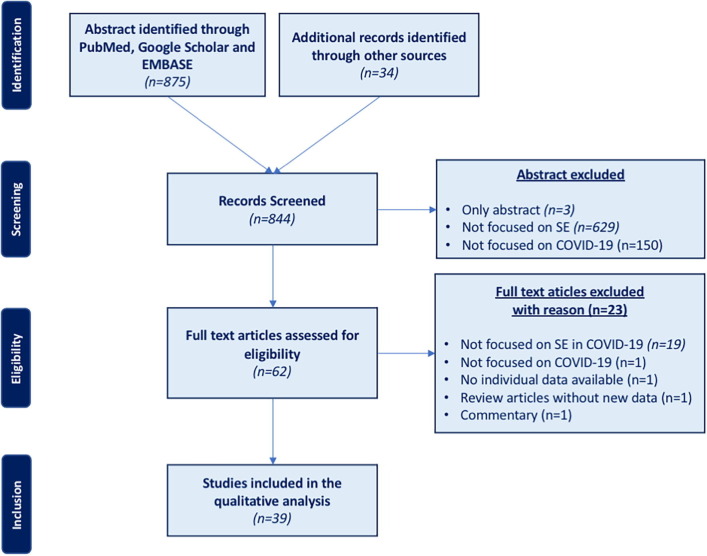
The literature search reported above yielded 909 articles (MEDLINE: 63; Google Scholar: 797; EMBASE: 15; other sources: 34). Sixty-five duplicated abstracts and titles were identified through our electronic search. Of the 844 records screened, the full texts of 62 articles were reviewed for eligibility. Twenty-three articles initially considered for possible inclusion were eventually excluded (excluded articles with reasons for exclusion and number of patients for each excluded study are reported in Supp.Tab.2). Thirty-nine articles (24 case reports and 15 case series, with individual patient data available for 47 patients) fulfilling the selection criteria were finally included (Fig. 1 ) [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44]. According to Newcastle-Ottawa Quality Assessment Scale (NOS), six papers (6/39) were scored 2, sixteen papers (13/39) were scored 3, twenty-two papers (19/38) were scored 4, and one paper (1/38) was scored 5 (score results for each study are provided in Supp.Tab.3).
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram describing the search from literature; 844 records were screened, from which 39 articles (24 case reports and 15 retrospective studies) were selected. SE: status epilepticus.
5. Demographics and past medical history
Forty-seven patients (25 males; 53.2%) were included (median age: 57 years, range: 2–86). Three patients (6.4%) had a prior history of epilepsy, with 2 (4.3%) taking ASM before hospitalization. Hypertension (n = 7; 14.9%), diabetes mellitus type II (n = 6; 12.8%), chronic renal disease (n = 5; 10.6%) and chronic obstructive pulmonary disease (COPD) (n = 2; 4.3%) were the most commonly reported comorbidities. Demographics and data on past medical history are summarized in Table 1 .
Table 1.
Demographics and clinical data.
| Sex | Male | 25 | (53.2%) | |
| Female | 22 | (46.8%) | ||
| Age | Median (range) | 57 y (2–86) | ||
| Range | 2–86 | |||
| age < 18 y | 8 | (17.4%) | ||
| Epilepsy history | Yes | 3 | (6.4%) | |
| No | 30 | (63.8%) | ||
| NA | 14 | (29.8%) | ||
| Comorbidities | Yes | 22 | (46.8%) | |
| No | 2 | (4.3%) | ||
| NA | 23 | (48.9%) | ||
| COVID-19 associated symptoms | Respiratory symptoms | |||
| Yes | 33 | (70.2%) | ||
| NA | 14 | (29.8%) | ||
| Gastrointestinal symptoms | ||||
| Yes | 9 | (19.1%) | ||
| NA | 38 | (81.9%) | ||
| Other symptoms | ||||
| Yes | 15 | (31.9%) | ||
| NA | 32 | (69.1%) | ||
| COVID-19 associated treatment | Steroids | |||
| Yes | 15 | (31.9%) | ||
| No | 2 | (4.3%) | ||
| NA | 30 | (63.8%) | ||
| Hydroxychloroquine | ||||
| Yes | 13 | (27.7%) | ||
| NA | 34 | (72.3%) | ||
| Heparin | ||||
| Yes | 10 | (21.3%) | ||
| NA | 37 | (78.7%) | ||
| Antibiotics | ||||
| Yes | 18 | (38.3%) | ||
| NA | 29 | (61.7%) | ||
| Remdesevir | ||||
| Yes | 2 | (4.3%) | ||
| NA | 45 | (95.7%) | ||
| Plasma | ||||
| Yes | 1 | (2,1%) | ||
| NA | 46 | (97,9%) | ||
| Intubation | Yes | 28 | (59.6%) | |
|
24 | |||
|
4 | |||
| NA | 19 | (40.4%) | ||
| Laboratory findings | Arterial-blood gas (ABG) | |||
| Performed | 7 | (14.9%) | ||
|
61.1 ± 17.4 | |||
|
26.7 ± 5.5 | |||
|
7.5 ± 1.1 | |||
| NA | 40 | (85.1%) | ||
| Blood samples | ||||
| Performed | 24 | (51.1%) | ||
|
13 | (27.7%) | ||
|
4 | (8.5%) | ||
|
7 | (14.9%) | ||
| No | 23 | (48.9%) | ||
| Lumbar punction | ||||
| Performed | 23 | (48.9%) | ||
|
1–26 | |||
| 4 | (8.5%) | |||
|
7 | (14.9%) | ||
| (51.1%) | ||||
|
1 | (2,1%) | ||
| ○ Ab-NMDAR + | ||||
| NA | 24 | (51.1%) | ||
| Neuroradiological findings | Brain CT scan | |||
| Performed | 28 | (59.6%) | ||
|
4 | (8.5%) | ||
|
3 | (6.4%) | ||
|
1 | (2.1%) | ||
|
1 | (2.1%) | ||
|
1 | (2.1%) | ||
|
1 | (2.1%) | ||
|
1 | (2.1%) | ||
|
2 | (4.3%) | ||
| NA | 19 | (40.4%) | ||
| Brain MRI scan | ||||
| Performed | 27 | (57.4%) | ||
|
8 | (17%) | ||
|
4 | (8.5%) | ||
|
2 | (4.3%) | ||
|
2 | (4.3%) | ||
|
1 | (2.1%) | ||
|
2 | (4.3%) | ||
|
10 | (21.3%) | ||
| NA | 10 | (21.3%) | ||
NA: not available.
6. Symptoms related to SARS-CoV-2 infection and therapy
Respiratory or gastrointestinal symptoms occurred in 33 (70.2%) and 9 (19.1%) patients, respectively. Other frequently reported symptoms were fever (n = 7; 14.9%), hypo/anosmia and ageusia (n = 2; 4.3%), asthenia/weakness (n = 2; 4.3%), myalgia (n = 2; 4.3%) and confusion (n = 2; 4.3%). Twenty-eight (59.6%) patients underwent intubation, whether for respiratory symptoms (n = 24; 51.1%) or for SE (n = 4; 8.5%). SARS-CoV-2 infection-related symptoms and therapy are summarized in Table 1.
7. SE presentation and semiology
Twenty-seven out of 47 (57.4%) patients developed SE after COVID-19 respiratory/gastrointestinal symptoms (median: 168 hours, IQR 96-276), whereas 7 patients (14.9%) before (median: 24 hours, IQR 11-72). SE etiology was mainly unknown, though acute symptomatic and multifactorial have been reported. Seventeen patients (36.2%) met the diagnostic criteria for New-onset Refractory Status Epilepticus (NORSE) [45]. Although motor symptoms represented the most frequent manifestation of SE, several nonconvulsive SE were reported. Salzburg criteria for the diagnosis of Non-convulsive Status Epilepticus (NCSE) [46] were mentioned only in 3/8 cases. The details of SE presentation and semiology are summarized in Table 2
Table 2.
Status Epilepticus clinical features.
| Onset | Intra-hospital onset (IHO) | 30 | (63.8%) |
| Extra-hospital onset (EHO) | 12 | (25.5%) | |
| NA | 5 | (10.6%) | |
| Etiology | Acute | 19 | |
|
7 | (14.9%) | |
|
5 | (10.6%) | |
|
4 | (8.6%) | |
|
3 | (6.4%) | |
| Unknown | 26 | (55.3%) | |
| NA | 2 | (4.3%) | |
| Semiology | Motor onset | ||
|
11 | (23.4%) | |
|
2 | (4.3%) | |
|
2 | (4.3%) | |
|
6 | (12.8%) | |
|
1 | (2.1%) | |
| Non-motor onset | |||
|
8 | (17%) | |
| Unknown | 17 | (36.2%) | |
| Pattern EEG | GPDs | 5 | (10.6%) |
| LPDs | 2 | (4.3%) | |
| LPDs PLUS | 2 | (4.3%) | |
| BILPD | 2 | (4.3%) | |
| GRDA | 2 | (4.3%) | |
| NA | 34 | (72.3%) | |
| SE duration | <1h | 15 | (31.9%) |
| 1–6 h | 0 | (0%) | |
| 6–12 h | 1 | (2.1%) | |
| 12–24 h | 0 | (0%) | |
| >24 h | 3 | (6.4%) | |
| Unknown | 28 | (59.6%) | |
| Total STESS score | 0–3 | 34 | (72.3%) |
| 4–6 | 13 | (27.7%) | |
| Total EMSE score | 0–33 | 27 | (57.4%) |
| ≥34 | 20 | (42.6%) |
BILPDs: bilateral independent periodic discharges; FMSE: focal motor status epilepticus; GCSE: generalized convulsive status epilepticus; GPDs: generalized periodic discharges; GRDA: generalized rhythmic delta activity; MSE: motor status epilepticus; NCSE: non-convulsive status epilepticus; LPDs: lateralized periodic discharges; NA: not available.
8. EEG findings
EEG data were available for 33 (70.2%) patients. EEG abnormalities mainly consisted in continuous epileptiform activity (n = 24; 51.1%), although EEG slow-wave continuous activity was also reported (n = 8; 17%). EEG abnormalities were mostly localized in the frontal lobe (n = 13; 27.7%), followed by temporal lobe (n = 6; 12.8%). Twelve patients (25,5%) showed lateralized abnormalities, with 8 (17%) in the right hemisphere and 4 (8.7%) in the left hemisphere. Bifrontal localization was described in 4 (8.5%) patients, while diffuse epileptiform abnormalities were described in 9 (19.1%). A specific EEG pattern was described in 14 patients (30.4%), consisting in Generalized Periodic Discharges (GPDs) (n = 5; 10.6%), Lateralized Periodic Discharges (LPDs) (n = 2; 4.3%), Generalized Rhythmic Delta Activity (GRDA) (n = 2; 4.3%), Bilateral Independent Lateralized Periodic Discharges (BiLPD) (n = 2; 4.3%), Lateralized Periodic Discharges with superimposed fast activity (LPDs + F) (n = 2; 4.3%), and Generalized Spike-&-Wave/Sharp-and-Wave (GSW) (n = 1; 2.1%).
A follow-up EEG was performed in 5 patients (10.6%). EEG findings were normal in 2 patients, whereas the others showed “GRDA” [26], “GRDA and GPDs” [26], or “transitioning to moderate background, slowing with intermittent left temporal sharp waves” [37].
EEG findings are summarized in Table 2.
9. Neuroradiological findings
Information regarding computerized tomography (CT) scans of the head were reported in 28 (59.6%) cases, and 14 (29.8%) patients had abnormal findings. Twenty-seven (54.7%) patients underwent brain magnetic resonance image (MRI), with abnormal findings in 20 (42.6%). These included: inflammatory lesions (n = 8; 17%), posterior reversible encephalopathy syndrome (PRES) (n = 4; 8.5%), brain atrophy (n = 2; 4.3%), cerebral hemorrhage (n = 2; 4.3%), brain tumor and cerebral hemorrhage (n = 1; 2.1%), and nonspecific changes (n = 2; 4.3%). In most of the cases, inflammatory lesions did not show a specific lateralization neither a specific cortical lobe involvement (n = 5; 10.6%), even though orbito-frontal (n = 2; 4.3%) and limbic localization were reported.
Data on follow-up were reported for 16 patients (34%). The median follow-up duration was 21 days (range 4–1080). Four patients underwent a follow-up brain MRI, showing abnormalities in 2 cases, that were located in the “bilateral mesial temporal lobe” in one patient, and the “bilateral olfactive bulbs, head of caudate nucleus, posterior commissural fibers of the fornix, hippocampus, and left temporal lobe” in the other.
Neuroradiological findings are summarized in Table 1.
10. Laboratory findings
Arterial-blood gas sampling was reported in 7 patients (14.9 %). Data regarding blood samples were reported in 24 patients (51.1%), showing increased C-reactive protein (n = 13; 27.7%), procalcitonin (n = 4; 8.5%) and D-dimer (n = 7; 14.9%).
Twenty-three patients (48.9%) underwent a lumbar puncture, with a median of 9 white cell/mm3 (range 1–26) and increased protein and glucose mean concentrations. SARS-CoV-2 protein chain reaction (PCR) was positive in the cerebrospinal fluid (CSF) of 4 (8.5%) patients, and in 1 patient antibodies against N-methyl-D-aspartate receptor (NMDAr) were detected. Laboratory findings are summarized in Table 2
11. SE treatment
Treatment was reported in 38 (80.9%) patients. The most frequently used first-line IV ASMs were levetiracetam (LEV) (n = 14; 29.8%) and lorazepam (n = 10; 21.3%), while the most frequent second-line therapy were LEV (n = 11; 23.4%), valproic acid (n = 5; 10.6%), phenytoin (n = 4; 8.5%), and lacosamide (n = 4; 8.5%). The median number of ASMs used was 2 (IQR 1–3). Thirteen patients (27.7 %) received also an anesthetic medication, the most frequent being midazolam (n = 10; 21.3%) and propofol (n = 2; 4,3%). The median number of anesthetic medications used was 1 (IQR 0.75–1.5). Thirteen patients (27.7%) received further therapies, including steroid treatment (n = 7; 14.9%) or Ig IV (n = 5; 10.6%). In 25 patients (53.2 %) the treatment outcome was reported, which was favorable in the majority of cases (96%). There was no discernible difference in outcomes with various ASMs. The details of ASMs/anesthetic medications are summarized in Table 3 .
Table 3.
Anti-seizure (ASM) and Anesthetic (An) treatments of status epilepticus.
| Anti-seizure medication (ASMs) | Median number of ASMs associated (IQR) | Route of administration | N° of cases as first medication | N° of patients treated | Median dosage (IQR) |
|---|---|---|---|---|---|
| Lorazepam | 1 (1–2) | i.v. | 10 | 10 | 2 mg (1.25–6.5) |
| Levetiracetam | 1 (1–2) | i.v. | 14 | 23 | 2000 mg (1625–3500) |
| Clonazepam | 2 (1–3) | i.v. | 3 | 5 | NA |
| Diazepam | 3 (0–4) | i.v. | 2 | 3 | 20 mg |
| Clobazam | 2 (1–3) | i.v. | 1 | 2 | NA |
| Phenobarbital | 2 (1–3) | i.v. | 1 | 3 | NA |
| Valproic Acid | 1.5 (1–3) | i.v. | 4 | 10 | NA |
| Phenytoin | 2 (1–2) | i.v. | 0 | 4 | NA |
| Lacosamide | 2.5 (1.75–3.25) | i.v. | 1 | 11 | 200 mg (100–200) |
| Perampanel | 4 (3–4) | o.s. | 0 | 2 | 20 mg |
| Anesthetics (An) | Median number of An associated (IQR) | Route of administration | N° of cases as first medication | N° of patients treated | Median dosage (IQR) |
| Midazolam | 1 (0–2) | i.v. | 8 | 10 | NA |
| Propofol | 2 (0–2) | i.v. | 2 | 3 | NA |
| Tiopental | 1 (0–2) | i.v. | 1 | 2 | NA |
| Ketamine | 2 (1–2) | i.v. | 1 | 2 | NA |
i.v.: intra-venous; NA: not available.
Regardless of treatment, resolution of SE was reported in 40 patients (85.1%). Among these, 37 (78.7%) had a resolution of SE with a median of 48 hours (range: 0–1344) after the start of SE and with a median of 12 hours (range: 0–720) after the initiation of antiseizure treatment. Outcome was reported in 42 patients (89.3%): although it was mostly favorable, 10 patients (21%) died after a median of 21 days (IQR 13.5–25).
12. SE severity scales
Even though none of the studies reported the most commonly used outcome scales for SE, based on the information reported in the articles, we calculated STESS and EMSE scores for every patient. The median STESS score was 3 (IQR 2–4), while the mean EMSE score was 19 (IQR 14–49).
13. Statistical analysis of pooled data
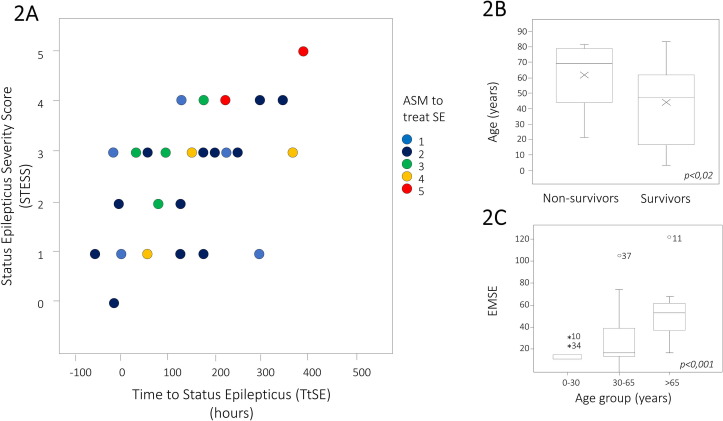
Logistic regression carried out using “SE resolution” as outcome variable did not show significant predictors of SE resolution. U Mann–Whitney test showed that patients who survived were younger (median age = 49.5, IQR 35–63) than those who did not (median age = 71, IQR 50–69, p < 0.02) (Fig. 2 B). A multiple linear regression model showed that severity of STESS score was influenced by the number of ASMs (p = 0.007), IHO of SE (p = 0.001), age (p = 0.048), TtSE (p = 0.005) (Fig. 2A). The relation between EMSE and age was confirmed using an ANOVA comparing the variance of EMSE score among age groups (0–30 years, 30–65 years, over 65 years), with higher mean EMSE scores in the older group (p < 0.001) (Fig. 2C). Post hoc analysis showed significant differences between the 0–30 years (mean EMSE = 16,33) and the over 65 years (mean EMSE = 56,83) groups and between the 30–65 years (mean EMSE = 29,48) and the over 65 years (mean EMSE = 56,83) groups.
Fig. 2.
A) A multiple linear regression model showed that severity of STESS score was influenced by the number of ASMs (p = 0.007), IHO of SE (p = 0.001), age (p = 0.048), TtSE (p = 0.005). B) U Mann–Whitney test showed that patients who survived were younger (median age = 49,5, IQR 35–63) than those who did not (median age = 71, IQR 50–69) (p < 0.02). C) The relation between EMSE and age was further confirmed using an ANOVA comparing the variance of EMSE score among age groups (0–30 years, 30–65 years, over 65 years), with higher mean EMSE scores in the older group (p < 0.001).
14. Outcomes
Thirteen patients had complete recovery at follow-up, whereas one patient had a persisting dysexecutive syndrome [36], and a moderate persistent cognitive deficit with bilateral proximal weakness in a further patient [37].
15. Discussion
The management of patients with SE in the context of COVID-19 pandemic is both a diagnostic and therapeutic challenge. Due to the highly contagious nature of the disease, these patients have usually limited access to diagnostic investigations, including the EEG [47]. This could seriously underestimate the incidence of SE, particularly in patients with non-convulsive SE or SE with minor motor phenomena. According to our data, only 70% of SE patients underwent an EEG recording. Several EEG patterns have been reported in SE associated with COVID-19, including periodic (LPDs, LPDs “plus”, BiLPDs, and GPDs) and rhythmic (GRDA) patterns. However, based on the available evidence, no single EEG pattern appears to be specific for SE related to this viral infection. Concerning SE semiology, a greater percentage of patients presented a Convulsive Status Epilepticus (CSE), focal or generalized. Remarkably, the Salzburg criteria for NCSE [46] were rarely applied for the diagnosis of NCSE. Hence, although the available data suggest that SE with prominent motor semiology is the most frequent SE type associated with COVID-19, the difficulties in recording an EEG in this clinical setting as well as the lack of use of specific diagnostic criteria could have led to an underestimation of NCSE or SE with mild clinical seizure activity.
Several conditions can lead to SE in patients with COVID-19. Acute seizures and SE can arise from the febrile status, hypoxia, or metabolic derangements. Nevertheless, according to the available data, such etiologies are infrequent, and generally associated with a milder form of SE, as shown by lower STESS and EMSE scores. Consequently, these patients generally show a good response to treatment and a positive outcome. In our systematic review, however, most cases of SE had an unknown etiology. In this subgroup of patients, SE started some days after the onset of systemic symptoms was associated with higher STESS and EMSE scores, and showed a worse response to treatment.
Several hypotheses have been proposed to explain the possible underlying causes of SE associated with COVID-19. According to a controversial hypothesis, a direct invasion of SARS-CoV-2 in the CNS represents the mechanism underlying these cases of SE, as suggested by experimental and clinical studies [48], [49], showing the neuroinvasive and neurotropic properties of the virus. The exact route through which SARS-CoV-2 enters the CNS is still unclear. It has been hypothesized that a viral involvement of the peripheral nerve is later followed by a spread to the CNS. However, in our review, only 4 cases showed the presence of the virus in the CSF as confirmed by polymerase chain reaction (PCR). Hence, a direct invasion of the CNS cannot be demonstrated in every case of SE associated with SARS-CoV-2 infection. In the literature, there are several reports of SE associated with COVID-19 possibly due to neuroinvasive or neuroinflammatory mechanisms. However, mere association does not necessarily imply causality, and the overall clinical evidence supporting these explanations is rather weak. Although some criteria such as temporality, plausibility, and coherence [50] may support the association between COVID-19 and SE, the strength of association (i.e., the larger an association between exposure and disease, the more likely it is to be causally related) and consistency needs to be thoroughly evaluated in the assessment of causality. A recent epidemiological study in Salzburg [51] has shown that the incidence of SE during the pandemic was not different compared to the general SE incidence recorded in the previous 5 years. However, it is plausible that the aforementioned difficulties in using adequate diagnostic tools led to a considerable underestimation of SE, and particularly NCSE. Regarding consistency, most studies differed greatly in terms of diagnostic investigations performed to rule out other causes of SE, hence impairing an accurate assessment of the causal relationship. Of note, only approximately half of the patients underwent a brain MRI (58.7%), CFS analysis (50%), or extensive laboratory workup including inflammatory markers (49.9%); serum and CSF autoimmune antibodies panel were performed in a minority of patients (15.2%). Hence, at least in some cases, the underlying cause of SE in COVID-19 may be unrelated to the viral infection or its systemic consequences. The association between SE and COVID-19 could therefore be spurious, or there may be a third underlying condition that could explain both SE and COVID-19. With this regard, at least in some cases, a concomitant immunodepression could have independently increased the risk of SARS-CoV-2 infection and SE due to immunological impairment (e.g., autoimmune or infective encephalitis).
According to a further hypothesis [52], SE could arise from the SARS-CoV-2-induced systemic inflammatory response. Remarkably, most cases of SE with SARS-CoV-2 infection described in the literature can be classified as cryptogenic New-Onset Refractory Status Epilepticus (NORSE), which are thought to be the clinical manifestation of a pro-inflammatory state in the CNS. However, although systemic inflammatory markers, such as erythrocytes sedimentation rate (ESR), C-reactive protein (CPR), and fibrin degradation product (D-dimer) were often increased, only very few studies provided data on levels of circulating cytokines (i.e. IL-6 and IL-1). Furthermore, no reports describing SE resolution following therapy with anti-interleukin drugs (i.e. Anakinra, Tocilizumab) have been published yet. Hence, although systemic inflammation and cytokine storm are frequently referred to as a possible underlying cause of SE associated with SARS-CoV-2, the evidence supporting this hypothesis is scarce.
The treatment of SE in patients with SARS-CoV-2 infection poses several challenges. The first-line treatment of SE in these patients should take into account the possible drug-to-drug interactions between antiviral treatments and anti-seizure medications (ASMs), along with the well-known respiratory depressive effect of BDZs. International guidelines for SE treatment recommend the use of i.v. BDZ as first-line treatment. However, our data show that LEV was the most frequently used medication. This can be due to the concerns for desaturation associated with BDZ use in patients with respiratory involvement. Interestingly, we did not observe any differences in SE resolution, number of ASMs, short- and long-term outcomes between patients initially treated with intravenous BDZs or ASMs.
Although none of the studies provided data on STESS and EMSE scores, we were able to calculate these scores for every patient. Based on recent studies, we assumed STESS ≥ 4 and EMSE ≥ 34 to be optimized cutoff points for mortality prediction. Accordingly, 28.3% of patients had a STESS score >4 and 45.7% an EMSE score >34. STESS score was related to mortality but not to SE resolution. Older patients had more severe SE, as reflected by higher values on EMSE and STESS scores. The presence of multiple comorbidities was also associated with a poorer outcome, as shown by the higher EMSE values. Furthermore, tTSE, age, number of ASMs, and IHO onset appear to be associated with more severe SE outcomes. These findings suggest that a delayed SE onset, probably sustained by inflammatory storm, is related to more severe SE, whereas early SE, possibly related to acute febrile reaction, is less severe.
16. Conclusion
SE can represent a neurological manifestation of SARS-CoV-2 infection; it can occur before any other symptom of respiratory or systemic involvement of COVID-19, although more frequently it occurs within the context of a clinically overt respiratory infection. The lack of prompt access to EEG recordings may lead to an underestimate of its incidence, particularly for NCSE. The etiology of SARS-CoV-2-related SE remains mostly unknown. A direct role of SARS-CoV-2 invasion in the CNS or the systemic inflammatory syndrome due to cytokine release has been proposed as possible explanations. However, the association between SE and COVID-19 could be spurious, and there may be other underlying conditions causally and independently related to both SE and COVID-19.
Author contributions
F.D. contributed to the conception and design of the study. B.N., J.L., G.E., F.R., R.S., L.T., S.T., M.D.P., M.R. applied eligibility criteria and selected studies for inclusion in the systematic review. J.L. performed statistical analysis. F.D., B.N., J.L., G.E., F.R., and S.T. wrote the manuscript and supervised all the data. All authors contributed to manuscript revisions, read, and approved the submitted version.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.yebeh.2021.107887.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Romoli M, Jelcic I, Bernard-Valnet R, García Azorín D, Mancinelli L, Akhvlediani T, et al. Infectious Disease Panel of the European Academy of Neurology. A systematic review of neurological manifestations of SARS-CoV-2 infection: the devil is hidden in the details. Eur J Neurol. 2020 Sep;27(9):1712-1726. 10.1111/ene.14382. Epub 2020 Jun 30. PMID: 32503088; PMCID: PMC7300895. [DOI] [PMC free article] [PubMed]
- 2.Solomon T. Neurological infection with SARS-CoV-2 — the story so far. Nat Rev Neurol. 2021 doi: 10.1038/s41582-020-00453-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fajgenbaum D.C., June C.H. Cytokine Storm. N Engl J Med. 2020;383(23):2255–2273. doi: 10.1056/NEJMra2026131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boggs J.G. Mortality associated with status epilepticus. Epilepsy Curr. 2004;4(1):25–27. doi: 10.1111/j.1535-7597.2004.04110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fırat O., Yalçın N., Demirkan K. COVID-19 & antiepileptic drugs: Should we pay attention? Seizure. 2020;80:240–241. doi: 10.1016/j.seizure.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available from: URL: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm.
- 7.Dono F, Carrarini C, Russo M, De Angelis MV, Anzellotti F, Onofrj M, et al. New-onset refractory status epilepticus (NORSE) in post SARS-CoV-2 autoimmune encephalitis: a case report. Neurol Sci. 2020 Nov 3:1–4. 10.1007/s10072-020-04846-z. Epub ahead of print. PMID: 33145624; PMCID: PMC7608104. [DOI] [PMC free article] [PubMed]
- 8.Skorin I, Carrillo R, Perez CP, Sanchez N, Parra J, Troncoso P, et al. EEG findings and clinical prognostic factors associated with mortality in a prospective cohort of inpatients with COVID-19. Seizure. 2020 Dec;83:1-4. 10.1016/j.seizure.2020.10.007. Epub 2020 Oct 13. PMID: 33075670; PMCID: PMC7553125. [DOI] [PMC free article] [PubMed]
- 9.Sokolov E., Hadavi S., Mantoan Ritter L., Brunnhuber F. Non-convulsive status epilepticus: COVID-19 or clozapine induced? BMJ Case Rep. 2020;13(10) doi: 10.1136/bcr-2020-239015. PMID: 33012721; PMCID: PMC7536775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chegondi M., Kothari H., Chacham S., Badheka A. Coronavirus Disease 2019 (COVID-19) associated with febrile status epilepticus in a child. Cureus. 2020 Aug 18;12(8) doi: 10.7759/cureus.9840. PMID: 32953347; PMCID: PMC7497292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balloy G, Leclair-Visonneau L, Péréon Y, Magot A, Peyre A, Mahé PJ, et al.. Non-lesional status epilepticus in a patient with coronavirus disease 2019. Clin Neurophysiol. 2020 Aug;131(8):2059-2061. 10.1016/j.clinph.2020.05.005. Epub 2020 May 13. PMID: 32405258; PMCID: PMC7217773. [DOI] [PMC free article] [PubMed]
- 12.Swarz JA, Daily S, Niemi E, Hilbert SG, Ibrahim HA, Gaitanis JN. COVID-19 Infection Presenting as Acute-Onset Focal Status Epilepticus. Pediatr Neurol. 2020 Nov;112:7. 10.1016/j.pediatrneurol.2020.07.012. Epub 2020 Jul 31. PMID: 32823139; PMCID: PMC7392878. [DOI] [PMC free article] [PubMed]
- 13.Neumann B, Schmidbauer ML, Dimitriadis K, Otto S, Knier B, Niesen WD, et al. PANDEMIC and the IGNITE study groups. Cerebrospinal fluid findings in COVID-19 patients with neurological symptoms. J Neurol Sci. 2020 Nov 15;418:117090. 10.1016/j.jns.2020.117090. Epub 2020 Aug 11. PMID: 32805440; PMCID: PMC7417278. [DOI] [PMC free article] [PubMed]
- 14.Werner C, Scullen T, Mathkour M, Zeoli T, Beighley A, Kilgore MD, et al. Neurological Impact of Coronavirus Disease of 2019: Practical Considerations for the Neuroscience Community. World Neurosurg. 2020 Jul;139:344-354. 10.1016/j.wneu.2020.04.222. Epub 2020 May 6. PMID: 32387786; PMCID: PMC7202815. [DOI] [PMC free article] [PubMed]
- 15.Carroll E, Neumann H, Aguero-Rosenfeld ME, Lighter J, Czeisler BM, Melmed K, et al. Post-COVID-19 inflammatory syndrome manifesting as refractory status epilepticus. Epilepsia. 2020 Oct;61(10):e135-e139. 10.1111/epi.16683. Epub 2020 Sep 18. PMID: 32944946; PMCID: PMC7537028. [DOI] [PMC free article] [PubMed]
- 16.Abdulsalam M.A., Abdulsalam A.J., Shehab D. Generalized status epilepticus as a possible manifestation of COVID-19. Acta Neurol Scand. 2020;142(4):297–298. doi: 10.1111/ane.133217. PMID: 32779768; PMCID: PMC740532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Somani S, Pati S, Gaston T, Chitlangia A, Agnihotri S. De Novo Status Epilepticus in patients with COVID-19. Ann Clin Transl Neurol. 2020 Jul;7(7):1240-1244. 10.1002/acn3.51071. Epub 2020 Jun 10. PMID: 32407609; PMCID: PMC7273010. [DOI] [PMC free article] [PubMed]
- 18.Emami A, Fadakar N, Akbari A, Lotfi M, Farazdaghi M, Javanmardi F, et al. Seizure in patients with COVID-19. Neurol Sci. 2020 Nov;41(11):3057-3061. 10.1007/s10072-020-04731-9. Epub 2020 Sep 19. PMID: 32949289; PMCID: PMC7501768. [DOI] [PMC free article] [PubMed]
- 19.Atakla HG, Noudohounsi ACWH, Barry LF, Noudohounsi MMUD, Legba LD, Souare IS, et al. COVID-19 infection in known epileptic and non-epileptic children: what is the place of chloroquine sulfate? (a case report). Pan Afr Med J. 2020 Oct 22;37:177. 10.11604/pamj.2020.37.177.26066. PMID: 33447332; PMCID: PMC7778175. [DOI] [PMC free article] [PubMed]
- 20.Parauda SC, Gao V, Gewirtz AN, Parikh NS, Merkler AE, Lantos J, et al. Posterior reversible encephalopathy syndrome in patients with COVID-19. J Neurol Sci. 2020 Sep 15;416:117019. 10.1016/j.jns.2020.117019. Epub 2020 Jul 9. PMID: 32679347; PMCID: PMC7347314. [DOI] [PMC free article] [PubMed]
- 21.Doo FX, Kassim G, Lefton DR, Patterson S, Pham H, Belani P. Rare presentations of COVID-19: PRES-like leukoencephalopathy and carotid thrombosis. Clin Imaging. 2021 Jan;69:94-101. 10.1016/j.clinimag.2020.07.007. Epub 2020 Jul 16. PMID: 32707411; PMCID: PMC7365057. [DOI] [PMC free article] [PubMed]
- 22.Derly Andrade Molina, Juan Fernández-Cadena, Telmo Fernández-Cadena et al. A suspected case of SARS-CoV-2 persistence with reactivation, 26 October 2020, PREPRINT (Version 1) available at Research Square [ 10.21203/rs.3.rs-92286/v1].
- 23.Hung E.C., Chim S.S., Chan P.K., Tong Y.K., Ng E.K., Chiu R.W., et al. Detection of SARS coronavirus RNA in the cerebrospinal fluid of a patient with severe acute respiratory syndrome. Clin Chem. 2003;49(12):2108–2109. doi: 10.1373/clinchem.2003.025437. PMID: 14633896; PMCID: PMC7108123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M, et al. Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection. Eur J Neurol. 2020 Sep;27(9):e43-e44. 10.1111/ene.14298. Epub 2020 May 30. PMID: 32383343; PMCID: PMC7267660. [DOI] [PMC free article] [PubMed]
- 25.Farley M, Zuberi J. COVID-19 Precipitating Status Epilepticus in a Pediatric Patient. Am J Case Rep. 2020 Jul 30;21:e925776. 10.12659/AJCR.925776. PMID: 32730234; PMCID: PMC7414829. [DOI] [PMC free article] [PubMed]
- 26.Chen W, Toprani S, Werbaneth K, Falco-Walter J. Status epilepticus and other EEG findings in patients with COVID-19: A case series. Seizure. 2020 Oct;81:198-200. 10.1016/j.seizure.2020.08.022. Epub 2020 Aug 21. PMID: 32861152; PMCID: PMC7441944. [DOI] [PMC free article] [PubMed]
- 27.Bolaji P., Kukoyi B., Ahmad N., Wharton C. Extensive cerebral venous sinus thrombosis: a potential complication in a patient with COVID-19 disease. BMJ Case Rep. 2020;13(8) doi: 10.1136/bcr-2020-236820. PMID: 32784243; PMCID: PMC7418679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Monti G, Giovannini G, Marudi A, Bedin R, Melegari A, Simone AM, et al. Anti-NMDA receptor encephalitis presenting as new onset refractory status epilepticus in COVID-19. Seizure. 2020 Oct;81:18-20. 10.1016/j.seizure.2020.07.006. Epub 2020 Jul 15. PMID: 32688169; PMCID: PMC7362825. [DOI] [PMC free article] [PubMed]
- 29.Abdi S, Ghorbani A, Fatehi F. The association of SARS-CoV-2 infection and acute disseminated encephalomyelitis without prominent clinical pulmonary symptoms. J Neurol Sci. 2020 Sep 15;416:117001. 10.1016/j.jns.2020.117001. Epub 2020 Jun 18. PMID: 32590204; PMCID: PMC7301801. [DOI] [PMC free article] [PubMed]
- 30.McAbee GN, Brosgol Y, Pavlakis S, Agha R, Gaffoor M. Encephalitis Associated with COVID-19 Infection in an 11-Year-Old Child. Pediatr Neurol. 2020 Aug;109:94. 10.1016/j.pediatrneurol.2020.04.013. Epub 2020 Apr 24. PMID: 32586676; PMCID: PMC7180343. [DOI] [PMC free article] [PubMed]
- 31.Gómez-Enjuto S, Hernando-Requejo V, Lapeña-Motilva J, Ogando-Durán G, Fouz-Ruiz D, Domingo-García J, et al. Verapamil as treatment for refractory status epilepticus secondary to PRES syndrome on a SARS-Cov-2 infected patient. Seizure. 2020 Aug;80:157-158. 10.1016/j.seizure.2020.06.008. Epub 2020 Jun 6. PMID: 32574838; PMCID: PMC7275169. [DOI] [PMC free article] [PubMed]
- 32.Hosseini AA, Shetty AK, Sprigg N, Auer DP, Constantinescu CS. Delirium as a presenting feature in COVID-19: Neuroinvasive infection or autoimmune encephalopathy? Brain Behav Immun. 2020 Aug;88:68-70. 10.1016/j.bbi.2020.06.012. Epub 2020 Jun 9. PMID: 32531427; PMCID: PMC7282789. [DOI] [PMC free article] [PubMed]
- 33.Hepburn M, Mullaguri N, George P, Hantus S, Punia V, Bhimraj A, et al. Acute Symptomatic Seizures in Critically Ill Patients with COVID-19: Is There an Association? Neurocrit Care. 2020 May 28:1–5. 10.1007/s12028-020-01006-1. Epub ahead of print. PMID: 32462412; PMCID: PMC7253233. [DOI] [PMC free article] [PubMed]
- 34.Rodrigo-Armenteros P, Uterga-Valiente JM, Zabala-Del-Arco J, Taramundi-Argüeso S, Erburu-Iriarte M, Antón-Méndez L, et al. Non-convulsive status epilepticus in a patient with COVID-19 infection. Clin Neurophysiol. 2020 Nov;131(11):2588-2590. 10.1016/j.clinph.2020.08.005. Epub 2020 Aug 26. PMID: 32927214; PMCID: PMC7449119. [DOI] [PMC free article] [PubMed]
- 35.Saeed A, Shorafa E. Status epilepticus as a first presentation of COVID-19 infection in a 3 years old boy; Case report and review the literature. IDCases. 2020;22:e00942. 10.1016/j.idcr.2020.e00942. Epub 2020 Sep 3. PMID: 32895630; PMCID: PMC7468313. [DOI] [PMC free article] [PubMed]
- 36.Delorme C, Paccoud O, Kas A, Hesters A, Bombois S, Shambrook P, et al. CoCo-Neurosciences study group and COVID SMIT PSL study group. COVID-19-related encephalopathy: a case series with brain FDG-positron-emission tomography/computed tomography findings. Eur J Neurol. 2020 Dec;27(12):2651-2657. 10.1111/ene.14478. Epub 2020 Sep 22. PMID: 32881133; PMCID: PMC7461074. [DOI] [PMC free article] [PubMed]
- 37.Hwang S.T., Ballout A.A., Mirza U., Sonti A.N., Husain A., Kirsch C., et al. Acute seizures occurring in association with SARS-CoV-2. Front Neurol. 2020;5(11) doi: 10.3389/fneur.2020.576329. PMID: 33224090; PMCID: PMC7674622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Najjar S., Najjar A., Chong D.J., Pramanik B.K., Kirsch C., Kuzniecky R.I., et al. Central nervous system complications associated with SARS-CoV-2 infection: integrative concepts of pathophysiology and case reports. J Neuroinflammation. 2020;17(1):231. doi: 10.1186/s12974-020-01896-0. PMID: 32758257; PMCID: PMC7406702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davide Silvagni, Pietro Soloni, Francesca Darra et al. Self-limited focal epilepsy in a young child with SARS-CoV-2: serendipity or causal association?, 22 May 2020, PREPRINT (Version 1) available at Research Square [ 10.21203/rs.3.rs-30907/v1]. [DOI] [PubMed]
- 40.Roy-Gash F., De Mesmay M., Devys J.M., Vespignani H., Blanc R., Engrand N. Correction to: COVID-19-associated acute cerebral venous thrombosis: clinical, CT, MRI and EEG features. Crit Care. 2020;24(1):528. doi: 10.1186/s13054-020-03225-6. Erratum for: Crit Care. 2020 Jul 11;24(1):419. PMID: 32859261; PMCID: PMC7453364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Santos de Lima F, Issa N, Seibert K, Davis J, Wlodarski R, Klein S, et al. Epileptiform activity and seizures in patients with COVID-19. J Neurol Neurosurg Psychiatry. 2020 Nov 6:jnnp-2020-324337. 10.1136/jnnp-2020-324337. Epub ahead of print. PMID: 33158913. [DOI] [PubMed]
- 42.Vollono C, Rollo E, Romozzi M, Frisullo G, Servidei S, Borghetti A, et al. Focal status epilepticus as unique clinical feature of COVID-19: A case report. Seizure. 2020 May;78:109-112. 10.1016/j.seizure.2020.04.009. Epub 2020 Apr 21. PMID: 32344366; PMCID: PMC7172719. [DOI] [PMC free article] [PubMed]
- 43.Flamand M, Perron A, Buron Y, Szurhaj W. Pay more attention to EEG in COVID-19 pandemic. Clin Neurophysiol. 2020 Aug;131(8):2062-2064. 10.1016/j.clinph.2020.05.011. Epub 2020 May 22. PMID: 32482439; PMCID: PMC7242207. [DOI] [PMC free article] [PubMed]
- 44.Le Guennec L, Devianne J, Jalin L, Cao A, Galanaud D, Navarro V, et al. Orbitofrontal involvement in a neuroCOVID-19 patient. Epilepsia. 2020 Aug;61(8):e90-e94. 10.1111/epi.16612. Epub 2020 Jul 23. PMID: 32589794; PMCID: PMC7361605. [DOI] [PMC free article] [PubMed]
- 45.Gaspard N., Hirsch L.J., Sculier C., Loddenkemper T., van Baalen A., Lancrenon J., et al. New-onset refractory status epilepticus (NORSE) and febrile infection-related epilepsy syndrome (FIRES): State of the art and perspectives. Epilepsia. 2018;59(4):745–752. doi: 10.1111/epi.14022. Epub 2018 Feb 24 PMID: 29476535. [DOI] [PubMed] [Google Scholar]
- 46.Leitinger M., Beniczky S., Rohracher A., Gardella E., Kalss G., Qerama E., et al. Salzburg consensus criteria for non-convulsive status epilepticus–approach to clinical application. Epilepsy Behav. 2015;49:158–163. doi: 10.1016/j.yebeh.2015.05.007. Epub 2015 Jun 17 PMID: 26092326. [DOI] [PubMed] [Google Scholar]
- 47.Assenza G., Lanzone J., Ricci L., et al. Electroencephalography at the time of Covid-19 pandemic in Italy. Neurol Sci. 2020;41:1999–2004. doi: 10.1007/s10072-020-04546-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Meinhardt J., Radke J., Dittmayer C., et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat Neurosci. 2020 doi: 10.1038/s41593-020-00758-5. [DOI] [PubMed] [Google Scholar]
- 49.DosSantos MF, Devalle S, Aran V, Capra D, Roque NR, Coelho-Aguiar JM, et al. Neuromechanisms of SARS-CoV-2: A Review. Front Neuroanat. 2020 Jun 16;14:37. 10.3389/fnana.2020.00037. PMID: 32612515; PMCID: PMC7308495. [DOI] [PMC free article] [PubMed]
- 50.Hill A.B. The environment and disease: association or causation? Proc R Soc Med. 1965;58(5):295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leitinger M., Poppert K.N., Mauritz M., Rossini F., Zimmermann G., Rohracher A., et al. Status epilepticus admissions during the COVID-19 pandemic in Salzburg-A population-based study. Epilepsia. 2020;61(12):e198–e203. doi: 10.1111/epi.16737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.F. Nikbakht, A. Mohammadkhanizadeh, E. Mohammadi. How does the COVID-19 cause seizure and epilepsy in patients? The potential mechanisms. Multiple Sclerosis and Related Disorders. Volume 46,2020,102535. ISSN 2211-0348. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.