Abstract
Objectives:
Rumination involves a repetitive, passive focus on one’s thoughts and feelings and has been hypothesized as a mechanism contributing to multiple psychopathologies. The current investigation explores secondary outcomes from a pilot study to examine whether rumination-focused cognitive behavior therapy (RFCBT) alleviates symptoms of anxiety, increases behavioral activation, or increases global functioning among adolescents with a history of Major Depressive Disorder (MDD).
Methods:
Thirty-three adolescents were randomized to receive either RFCBT (n = 17) or assessment only (AO; n = 16) over the course of eight weeks. Mixed effects regression models were used to conduct intent-to-treat (ITT) analyses.
Results:
The quadratic interaction for group-by-time-by-time was significant for anxiety. Adolescents in the RFCBT group experienced a significant decrease in anxiety across the first six weeks of intervention (F = 7.01, df = 108.49, p = .009). The group-by-time interaction was significant for the behavioral activation outcome (F = 4.28, df = 25.60, p = .049) with youth randomized to RFCBT demonstrating increasing activation compared to AO. Global functioning did not significantly differ between groups (F = .40, df = 1, p > .05).
Conclusions:
Preliminary evidence suggests that RFCBT may hold promise as an intervention that alleviates both depressive and anxiety symptoms when comorbid.
Keywords: major depressive disorder, anxiety, rumination, adolescence, treatment
Major Depressive Disorder (MDD) is a chronic and recurrent illness (Keller & Boland, 1998; Kessing et al., 2004) and the onset of MDD during adolescence places youth on a developmental trajectory of disrupted learning, poorer functioning, and increased disability during the transition to adulthood (Fergusson & Woodward, 2002). Even after the receipt of empirically supported treatments, risk for relapse remains high (Curry et al., 2011). Limited work (Kennard et al., 2014) examines whether and how interventions can maintain short- and long-term wellness among these youth. Thus, more research is needed to understand how to prevent or delay the onset of recurrent MDD.
Several factors increase the risk of relapse, such as the presence of residual symptoms following treatment and diagnostic comorbidity (Lewinsohn & Essau, 2002). Anxiety in particular occurs with high frequency in depressed adolescents, with up to 75% of depressed youth meeting criteria for a comorbid anxiety disorder (Angold et al., 1999). Comorbid anxiety is associated with more severe baseline depression, and higher levels of functional impairment (Ollendick et al., 2008; Rapee et al., 2013; Rohde et al., 2001). Comorbid anxiety and depression are associated with educational underperformance, social isolation, and family conflict (Rohde et al., 2001). Unfortunately, treatments that ameliorate depression do not always serve to similarly reduce anxiety, which can further contribute to ongoing functional impairment (Liber et al., 2010; Rapee et al., 2013). In sum, both depression and anxiety are associated with significant disability; and when combined, this phenotype can be particularly debilitating, as existing treatments do not adequately ameliorate these overlapping, yet distinct, symptomatologies.
Common mechanisms across both depression and anxiety disorders include thinking styles that are negative, passive, repetitive, perseverative, and avoidant, including both worry and rumination (Ehring & Watkins, 2008; Watkins, 2008; McLaughlin et al., 2007). Indeed, worry and rumination are highly correlated, both lead to the generation of a negative mood (Querstret & Cropley 2013), and both reflect repetitive negative thinking that is negatively reinforced through avoidance and associated with distress and negative emotion, whether anxiety or depression (Topper et al., 2010). As such, rumination and worry are habits hypothesized to represent underlying mechanisms that contribute to both depression and anxiety, respectively (Ehring & Watkins, 2008; Nolen-Hoeksema & Watkins, 2011; Watkins, 2008). Prior studies support these hypotheses when examining the two constructs in isolation. These hypotheses are supported by prior studies examining worry and rumination in isolation. For example, Chelminski and Zimmerman (2003) concluded worry occurs in MDD; and, Nolen-Hoeksema (2000) found that rumination predicts the onset of anxiety. Although the overlap between these two constructs is debatable (Topper et al., 2010), only temporal orientation has been replicated as a defining dissimilarity between worry and rumination; worry as future focused and rumination as past focused (Ehring & Watkins, 2008; Topper et al., 2010).
Further, worry and rumination maintain psychophysiological arousal (Querstret & Cropley, 2013), and appear to worsen negative emotional states (Morrow & Nolen-Hoeksema, 1990; Nolen-Hoeksema & Morrow, 1993). The relationship between worry and rumination may play a much broader role contributing to ill health as it prolongs the duration of the negative mood (Brosschot et al., 2006). Additionally, secondary analyses of the STAR*D trial revealed patients with anxious depression (scoring seven or higher on the anxiety/somatization factor from the Hamilton Depression Rating Scale) fared significantly worse than those without anxious depression (Fava et al., 2008). To date, limited work has examined whether interventions that target depressive rumination also function to ameliorate symptoms of anxiety.
Rumination-focused cognitive behavior therapy (RFCBT) is one such intervention designed to specifically target rumination among individuals with residual depression (Watkins, 2008). Among adults with treatment refractory depression, RFCBT was effective in reducing residual depression symptoms and relapse rates when compared to ongoing antidepressant medication alone (treatment as usual, TAU; Watkins et al., 2011). Of particular note, 11 participants met criteria for generalized anxiety disorder (GAD) at baseline, whereas only one met criteria for GAD following RFCBT, offering preliminary support for the utility of this specific intervention (Watkins et al., 2011), at least among adults.
We adapted RFCBT for an adolescent population with the hope of changing ruminative thinking early in the illness. Prior research indicated rumination prospectively predicts the severity and duration of subsequent depressive episodes (Nolen-Hoeksema et al., 2008; Watkins, 2008). Thus, it is possible RFCBT may improve the overall trajectory of these youth with adolescent-onset depression. The primary outcome of this study revealed that eight weeks of RFCBT significantly changed resting state connectivity patterns and reduced rumination and depression compared to treatment as usual (Jacobs et al., 2016). The current, secondary, analyses are exploratory and examine whether RFCBT resulted in increases in behavioral activation, decreases in anxiety, and increases in global functioning. We hypothesized that RFCBT would lead to improvements in secondary outcome measures when compared to AO. Specifically, we hypothesized that RFCBT would result in reductions in anxiety, increases in behavioral activation, and increases in global functioning.
Method
Participants
Participants were 33 adolescents between the ages of 12 and 18 who met criteria for MDD in the past, but currently were in full or partial remission (rMDD). Eligibility was assessed using the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL; (Kaufman et al., 1997), in line with the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (American Psychiatric Association (APA), 2000). Full remission was defined as the absence of any significant depressive symptoms (i.e., a score of three on any KSADS-PL MDD item was exclusionary), however subthreshold symptoms were not exclusionary (i.e., a score of two on any KSADS-PL MDD item). Partial remission was defined as the absence of any clinically significant depressive symptoms in the past two weeks (i.e., no score of three on any KSADS-PL MDD item, and/or four or more scores of two on KSADS-PL MDD items). This study focused on a remitted sample to be consistent with the adult trial (Watkins et al., 2011). Given the unknown efficacy of the current intervention, participants, regardless of randomization, were permitted to continue all maintenance treatment regimens including maintenance psychotherapy and medication (selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) only). If on medication, adolescents were required to meet stabilization standards. Specifically, if currently taking an antidepressant, the adolescent was required to have adhered for a minimum of 12 weeks with no dose changes within the two weeks prior to enrollment. Comorbid anxiety and/or ADHD were not exclusionary, and adolescents were allowed to be on stimulant medication. Specifically, in the intervention group, two adolescents met criteria for social phobia; four met criteria for GAD; and, one-met criteria for post-traumatic stress disorder (PTSD). In the AO group, one adolescent met criteria for social phobia; four met criteria for GAD; and, one adolescent met criteria for both PTSD and panic disorder.
In addition to subthreshold or threshold MDD, adolescents were excluded if they received a Children’s Depression Rating Scale-Revised (CDRS-R) score greater than 45 or endorsed current suicidality with plan or intent, a Wechsler Abbreviated Scale of Intelligence (WASI) IQ < 70, or use of psychotropic medication other than stimulants or antidepressants. Comorbidities were exclusionary if they were considered primary (i.e., versus MDD as primary), and/or included: lifetime history of an autism spectrum disorder, psychotic disorder, mania, eating disorder, or alcohol/substance abuse or dependence within the previous six months.
Procedure
The University of Illinois at Chicago (UIC) Institutional Review Board (IRB) approved the current study and all adolescents signed assent with corresponding parent consent. Participants were recruited using flyers, postings on the Internet, and in-person through a treatment clinic. Active recruitment occurred between 2013 and 2015. Adolescents and their parent(s) were screened via telephone to confirm initial eligibility before they were scheduled for the baseline diagnostic interview. The baseline interview consisted of the KSADS-PL to confirm eligibility and self-report measures for parent and child. Adolescents also completed functional magnetic resonance image (fMRI) scans and these primary outcome data are described elsewhere (Jacobs et al., 2016). Once eligibility was confirmed, a baseline fMRI was scheduled. Adolescents and their families were notified of randomization assignment after completing the baseline fMRI. Randomization was generated using Research Randomizer stratified by sex and age (computer program, Version 4.02013).
Adolescents in both groups, RFCBT and AO, completed self-report questionnaires every 2 weeks throughout the 8-week intervention period. The family and, if applicable, outside clinician, were notified if the adolescent’s symptoms increased. At week 8, adolescents and their parents completed a clinical interview, self-report measures, and a follow-up fMRI. Figure 1 illustrates CONSORT criteria for the study. Of the 17 adolescents who received RFCBT, all but two completed the 8-week manualized intervention. Both participants were withdrawn due to safety concerns. One had worsening depression by the second intervention meeting and was endorsing suicidality and it was decided that a higher level of care was needed, and study participation may be too taxing. One adolescent ran away from home by week six of the intervention. Clinical Trials Registration: NCT01905267.
Figure 1.
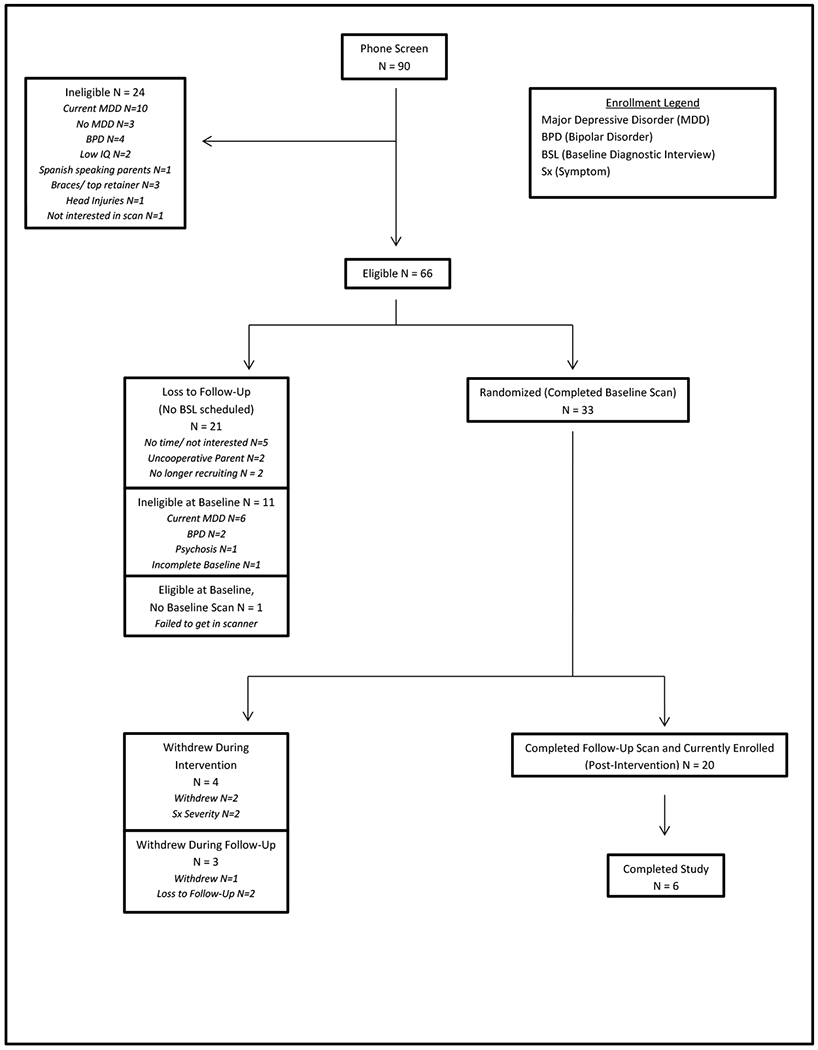
CONSORT.
Intervention.
RFCBT for adolescents was modified from the RFCBT studied among adult populations (Watkins et al., 2011; Watkins, 2016). Adolescents randomized to RFCBT met one-on-one with a therapist, the second author, on a weekly basis for 45-60 minutes for 8 weeks. RFCBT directly teaches adolescents to recognize rumination or “when you get stuck in your head” and to notice the influence this has on their mood (Watkins et al., 2011). This psychoeducation component includes noticing personal triggers to ruminate, as well as opportunities to shift or change any situations that tend to increase the likelihood of rumination, to reduce habitual rumination (Watkins & Nolen-Hoeksema, 2014). Adolescents were taught to be Active, Specific, and Kind (ASK) when thinking about oneself, rather than ruminative, which tends to be passive, abstract, and a critical form of thinking. Adolescents learn about their cycle of emotions and that the habit of rumination gets them stuck at thinking and feeling, which can make it harder to take action and has consequences. At each session, adolescents participated in a mindfulness exercise to show how to use your attention to shift into a different way of being. Mindfulness exercises included three-part breath, the body scan, progressive muscle relaxation, lovingkindness, the wave exercise, and others as appropriate. Another key skill taught is to change “Why?” questions to “How?” questions because abstract “Why?” questions lead to impaired problem solving, greater negative overgeneralization, and greater emotional reactivity (Watkins, 2008; Watkins et al., 2008).
Although it could be argued that RFCBT is similar to mindfulness-based CBT interventions, a hallmark difference is that first adolescents (patients) are educated on what rumination is and how to recognize it (identify triggers). Psychoeducation regarding rumination and recognizing one’s own pattern, offers a foundation for utilizing skills such as mindfulness, problem solving, distraction, or other coping strategies to reduce rumination. Adolescents also learn strategies to prevent rumination from beginning in the first place. The adolescent intervention differed from the adult treatment in that exercises were shorter, and language was modified to be applicable to a younger, primarily inner-city population.
Assessment Only.
Adolescents randomized to AO completed the same assessment schedule, which included baseline, self-report questionnaires every two weeks during the intervention period, and the eight-week follow-up interview and fMRI scan.
Measures
Behavioral Activation of Depression Scale - Adolescent (BADS-A; Skriner et al., 2015).
BADS-A is an adaptation of the BADS used with adult populations (Kanter et al., 2007) that assesses behavioral activation and avoidance. Psychometric evaluation of the BADS-A indicates a five-factor solution (18-items; Skriner et al., 2015). The total score was used in the current study with higher scores indicating greater activation. Adolescents completed this self-report at baseline and week 8.
Children’s Depression Rating Scale – Revised (CDRS-R; (Poznanski & Mokros, 1996).
The CDRS-R is a well-validated 17-item clinician-rated depression severity measure. The reliability, validity, and sensitivity to change of the CDRS-R are well documented (Brooks & Kutcher, 2001). Inter-rater reliability (intraclass correlations, ICC = 98%) was excellent. The Independent Evaluator (IE), blind to randomization, completed the CDRS-R after the baseline and week 8 KSADS-PL interview with both adolescent and parent.
Global Assessment Scale for Children (CGAS; (Shaffer et al., 1983).
CGAS provides a measure of global impairment and functioning over the previous month. The scale ranges from 1 (lowest) to 100 (highest). Of note, CGAS scores obtained in clinical contexts are hypothesized to reflect functional competence rather than symptom severity (Green et al., 1994). The IE used information collected from the parent and adolescent to assign a CGAS score at baseline and week 8.
Multidimensional Anxiety Scale for Children (MASC; (March, Parker, Sullivan, Stallings, & Conners, 1997).
The MASC is a 39 item 4-point Likert self-report rating scale that has shown robust psychometric properties in clinical, epidemiological and intervention studies. Three-week test-retest reliability for the MASC is .79 in clinical samples (March et al., 1997). Adolescents completed the MASC at baseline and every two weeks over the eight-week intervention period.
Reynolds Adolescent Depression Scale (RADS; Reynolds, 1987).
The RADS is a 30-item self- report measure of current depressive symptomatology. This measure utilizes a 4-point Likert scale and has excellent internal consistency and good test-retest reliability (Reynolds, 1987). Adolescents completed the RADS at baseline and every two weeks over the eight-week intervention period.
Rumination Response Scale (RRS; (Treynor et al., 2003).
The RRS was used to assess self-report ruminative tendencies. The RRS is valid and reliable even among young adolescent populations (Burwell & Shirk, 2007). Adolescents completed the RRS at baseline and every two weeks over the eight-week intervention period.
Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (KSADS-PL; (Kaufman et al., 1997).
The K-SADS-PL is a well-established, structured diagnostic interview and was completed by the IE with the adolescent and the parent at baseline and week 8 upon adolescent and parent interview. Inter-rater reliability was good (kappa = .78).
Data Analyses
Intent to treat (ITT) analyses were conducted using mixed-effects regression models (MRMs) using SPSS MIXED (Version 19, Chicago: SPSS Inc.). MRMs allow for the dependencies inherent in repeated assessments, are robust to missing data, and can be used to estimate scores using group trajectories. MRMs were used to assess the effects of treatment and treatment-by-time for behavioral activation (BADS-A) at baseline and week 8. The quadratic treatment-by-time-by-time interaction was also evaluated for anxiety symptoms (MASC), as five assessment points were available. Effect size for the MASC was calculated using Cohen’s f2 (f2 = R2 / 1 – R2; Selya et al., 2012). A general linear model (GLM) was used to evaluate global functioning (CGAS) given the restriction of range in available data. All other effect sizes were calculated using Cohen’s d (d = (M1 – M2) / √[(s12 + s22) / 2]); Cohen, 1988; Rosnow & Rosenthal, 1996). Secondary completers analyses were conducted using a GLM with completed measures for behavioral activation (BADS-A), anxiety symptoms (MASC), and global functioning (CGAS; n = 15 RFCBT, n = 14 AO).
Results
Youth randomized to RFCBT did not differ from those randomized to the AO group on demographic characteristics or clinical features (Table 1). The presence of a current comorbid anxiety disorder, as well as current psychiatric medication use were common in the total sample, 39% and 52%, respectively. Additionally, 24% of the total sample reported taking a stimulant for comorbid ADHD. Ten adolescents experienced a change in outside treatment during the eight-week intervention period (4 = RFCBT and 6 = AO). Changes included tapering down or discontinuing maintenance psychotherapy (n = 3), stopping medication (n = 2), increasing SSRI (n = 3), new ADHD medication (n = 1), and change in ADHD medication (n = 1). Time in remission was approximately one-year across groups, although residual symptoms (i.e., a score of two on any KSADS-PL MDD item) were present at baseline.
Table 1.
Demographics and clinical characteristics of intent-to-treat sample
| RFCBT (n=17) | Assessment Only (n=16) | |
|---|---|---|
| M(SD) | M(SD) | |
| Age | 15.41(1.97) | 15.69(1.89) |
| IQ Estimate | 108.94(13.27) | 108.13(12.60) |
| Days Since Last Episode | 469(692.25) | 251(337.50) |
| RADS Baseline | 64.41(12.12) | 63.50(12.42) |
| CDRS-R Baseline | 27.47(3.94) | 28.00(6.82) |
| RRS Baseline | 52.88(12.62) | 50.69(12.77) |
| BADS-A Baseline | 68.60(16.28) | 65.25(11.50) |
| MASC Baseline | 50.00(16.06) | 46.63(12.53) |
| CGAS Baseline | 73.94(7.43) | 75.81 (10.10) |
| N(%) | N(%) | |
| Female | 9(53%) | 10(63%) |
| Racial/Ethnic Minority | 9(53%) | 7(44%) |
| Current Comorbid Anxiety | 7(41%) | 6(38%) |
| Current ADHD Medication | 5(29%) | 3(19%) |
| Current Psychiatric Medication |
7(41%) |
10(63%) |
Note. RADS = Reynolds Adolescent Depression Scale; CDRS-R = Children Depression Rating Scale; RRS = Ruminative Response Scale; BADS-A = Behavior Activation of Depression Scale – Adolescent; MASC = Multidimensional Anxiety Scale for Children; CGAS = Global Assessment Scale for Children
Figure 2 illustrates change in anxiety within the ITT sample. Among the ITT sample, the quadratic group-by-time-by-time interaction was significant for anxiety (F = 7.01, df = 108.49, p = .009) with a small effect size (f2 = .19), such that adolescents who received RFCBT demonstrated significantly decreasing anxiety compared to AO through week 6. As illustrated in Figures 3 and 4, the ITT sample of adolescents receiving RFCBT also demonstrated significant increases in behavior activation (BADS-A; (F = 4.28, df = 25.60, p = .049, d = .97), but did not demonstrate a significant increase in global functioning (CGAS; F = .40, df = 1, p > .05, d = .02). Table 2 details main and interaction effects for all outcomes in the ITT sample. Diagnostically, six adolescents randomized to AO and 10 adolescents randomized to RFCBT met criteria for an anxiety disorder at baseline. At week eight, two adolescents in the AO group and zero adolescents in the RFCBT group met criteria for an anxiety disorder.
Figure 2.
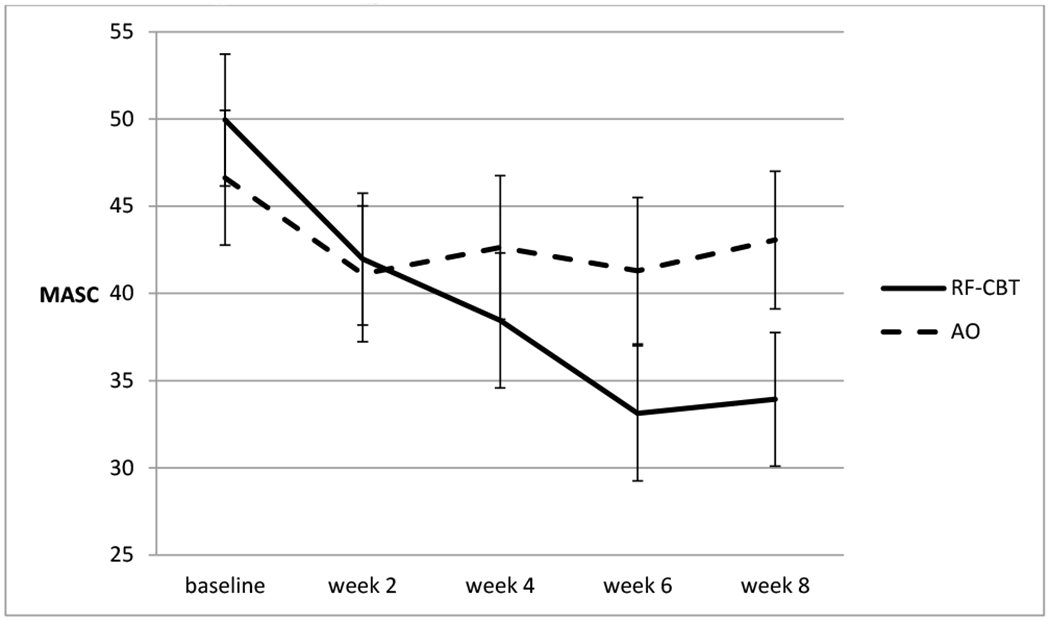
Mixed-Effects Regression Models: Predicted scores for anxiety symptoms among intent-to-treat sample across eight weeks
Note. MASC = Multidimensional Anxiety Scale for Children
Figure 3.
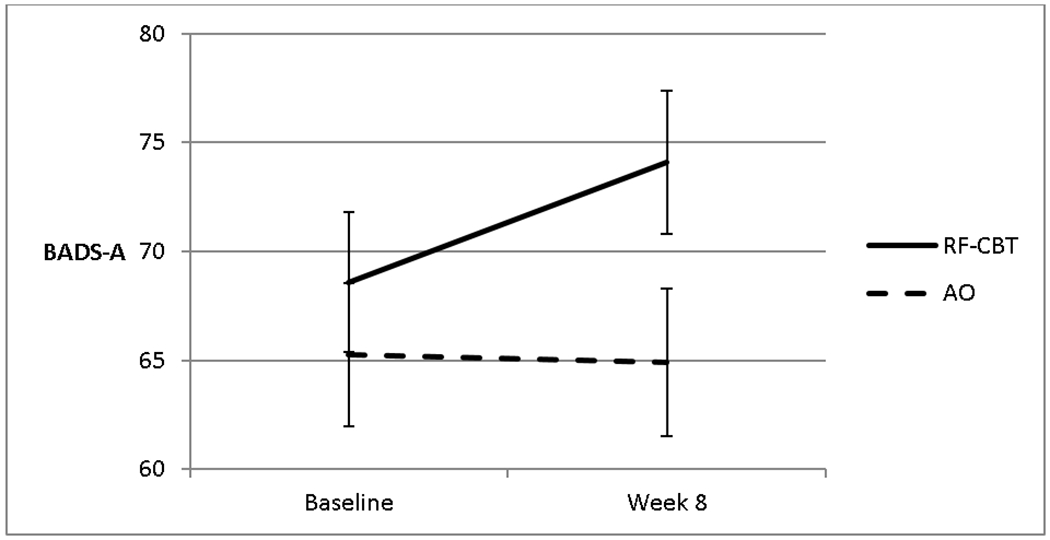
Mixed-Effects Regression Models: Predicted scores for behavioral activation among intent-to-treat sample
Note. BADS-A = Behavior Activation Depression Scale – Adolescent
Figure 4.
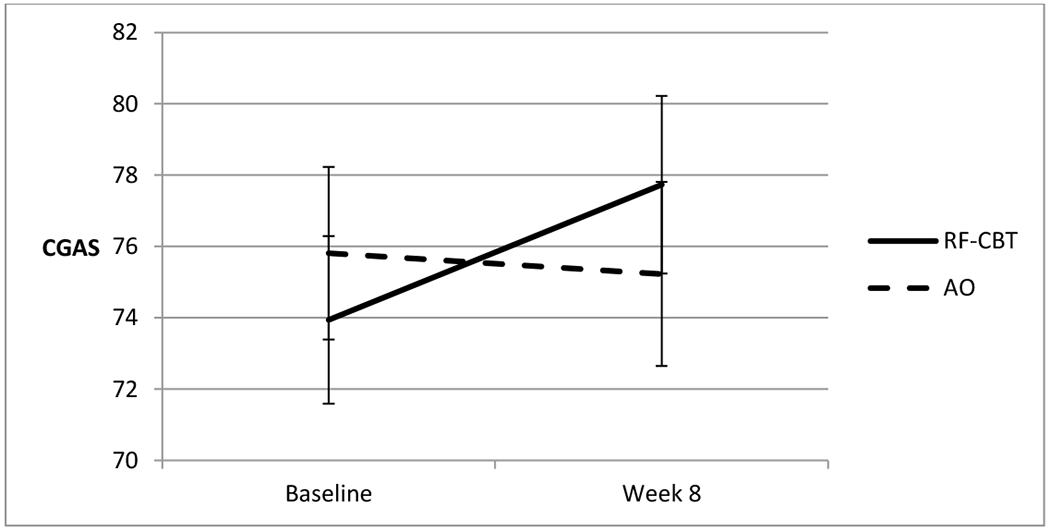
Change in global functioning across 8 weeks among completers sample
Note. CGAS = Global Assessment Scale for Children
Table 2.
Estimates of Fixed Effects of Group, Time, and Their Interaction on Activation, Anxiety, and Functioning of the Intent to Treat Sample
| Dependent Variable | Estimate | Standard Error | df | 95% Confidence Interval | |
|---|---|---|---|---|---|
| BADS-A | |||||
| Intercept | 61.91** | 7.29 | 36.96 | 47.14 | 76.68 |
| Treatment | 3.34 | 4.59 | 37.64 | −5.96 | 12.65 |
| Time | −1.55 | 1.11 | 25.37 | −3.82 | .73 |
| Time x Treatment | 1.46* | .71 | 25.60 | .01 | 2.91 |
| MASC | |||||
| Intercept | 41.24** | 8.25 | 41.24 | 24.59 | 57.89 |
| Treatment | 3.25 | 5.17 | 41.40 | −7.19 | 13.70 |
| Time | 2.66 | 1.48 | 109.28 | −.28 | 5.60 |
| Time x Treatment | −3.38*** | .93 | 109.29 | −5.22 | −1.54 |
| Treatment x Time x Time | .63** | .24 | 108.49 | .16 | 1.11 |
| CGAS | |||||
| Intercept | 77.68** | 5.39 | 57.49 | 66.90 | 88.47 |
| Treatment | −1.87 | 3.38 | 57.49 | −8.63 | 4.89 |
| Time | −1.24 | 1.68 | 30.90 | −4.67 | 2.19 |
| Treatment x Time | 1.09 | 1.05 | 30.87 | −1.05 | 3.24 |
Note. BADS-A = Behavior Activation of Depression Scale for – Adolescent, MASC = Multidimensional Anxiety Scale for Children, CGAS = Global Assessment Scale for Children, df = degrees of freedom
p < .05
p < .01.
p < .001
Results among completers were parallel in that adolescents who received RFCBT reported significantly decreasing anxiety compared to AO controls (MASC; F = 8.57, df = 1, p = .007, d = .13). However, groups did not differ on behavioral activation (F = 3.41, df = 1, p = .078, d = .24) or global functioning (CGAS; F = .40, df = 1, p = .530, d = .02).
Discussion
Youth randomized to RFCBT demonstrated significant decreases in anxiety across six of the eight-week intervention period in both the ITT and completer samples relative to AO. Across both AO and RFCBT, the number of adolescents who met full diagnostic criteria for an anxiety disorder was reduced (66% versus 100% reduction). RFCBT also led to a significant increase in behavioral activation within the ITT sample; however, this did not meet criteria for significance among completers. The change in global functioning was not significant across either sample. In sum, RFCBT not only improved residual depressive symptoms (Jacobs et al., 2016), but also appears to have broader utility in reducing anxiety symptoms. This supports our hypothesis that rumination may serve to reduce avoidance, as observed through reductions in anxiety and increases in behavioral activation.
Indeed, these results lend evidence to the notion that rumination, or repetitive negative thought, may be an underlying mechanism across both depression and anxiety disorders (Ehring & Watkins, 2008). Given that these illnesses together account for almost half of the global cost of mental illness (WHO Global Burden of Disease, 2008), examinations of whether and how interventions can target dual symptom presentation are warranted. Until recently, the majority of evaluated interventions have been disorder-specific (Topper et al., 2010) and targeting underlying mechanisms shared between disorders offers a fruitful avenue forward for intervention researchers. There is growing agreement that dual treatment for depression and anxiety may be necessary to treat these disorders more effectively (Barlow et al., 2004).
Certainly most disorder-specific treatments for depression can successfully alleviate symptoms of depression, but do not address symptoms of anxiety (Barlow et al., 2004; Rapee et al., 2013; Titov et al., 2015; Topper et al., 2010). In studies of psychosocial treatments for depression, adolescents with comorbid depression and anxiety do not improve at the same rate as peers who meet criteria for one diagnosis (Brent & Kolko, 1998; Rohde et al., 2001; Young et al., 2006). In addition, these comorbid adolescents showed less improvement in anxiety symptomology (Young et al., 2006) or no improvement in the recurrence of anxiety disorders during follow-up (Rohde et al., 2001).
These studies demonstrate that depression-specific treatments often do not effectively ameliorate comorbid anxiety symptoms during acute illness. In contrast, the current study suggests that significant reductions in anxiety can occur in tandem with reductions in residual depression. Reductions of these comorbid symptoms during the critical period of adolescence may prevent a recurrence and pathway towards ongoing psychopathology in adulthood (Kolaitis, 2012). It remains to be seen whether RFCBT can reduce depression and anxiety symptoms concurrently during the acute phase of depressive illness. Future research can explore this possibility.
Limitations and Future Directions
There are several limitations of the current investigation. First, this pilot study was designed to examine feasibility and preliminary efficacy. Thus, future examinations should include larger samples, an active control, and a larger proportion of unmedicated adolescents. However, it is worth noting that the current design paralleled that of the clinical trial conducted with adults (Watkins et al., 2011) in that the majority of adolescents in the AO group were engaged in ongoing maintenance treatment (including antidepressant medications; see Table 1). In addition, the current eligibility criteria focused on adolescents with a history of depression, whereas including adolescents with various dimensions of psychopathology including anxiety and depression would allow for a more thorough test of the efficacy of RFCBT in reducing both symptomologies. Further, there is less certainty that changes were specifically due to RFCBT versus another ongoing intervention. However, engagement across both arms of this study was parallel, so this offers some control for this possibility. Second, only one clinician administered the intervention. Future studies should include more than one therapist blind to study hypotheses in order to remove potential bias as well as compare efficacy across providers. However, the pre- and post-intervention evaluators were blind to study condition, potentially attenuating the effects of this limitation.
Third, the significance of the quadratic term for the anxiety outcome suggests that anxiety symptoms may be variable, particularly as the end of intervention approaches. Data collection for longitudinal follow-up is currently ongoing and future analyses can examine the stability of symptoms over the course of two-years following intervention. Fourth, the extent to which the current intervention overlaps with interventions such as Acceptance and Commitment Therapy (ACT), Mindfulness Based Stress Reduction (MBSR) is unknown. RFCBT specifically targets the mechanism of rumination, teaching skills for self-monitoring of cognitive habits and techniques for shifting attention to more productive habits. As such the adolescent receives a fair amount of psychoeducation regarding rumination, which is specific to RFCBT. Future research could attempt to dismantle effective ingredients of these treatments or directly compare them to one another. Finally, we did not find a significant improvement in global functioning across eight weeks. Indeed, we have found evidence of a delay between intervention and improvement in global functioning within a large sample of adolescents (Peters et al., 2015) and it remains to be seen whether or not global functioning will improve within this sample subsequent to the intervention period.
In summary, the current preliminary investigation contributes to a growing body of literature suggesting that interventions targeting underlying mechanisms may offer further amelioration of mental illness. Disorder-specific treatments in adolescence may tend to overlook overlapping features of depression and anxiety (Angold et al., 1999), despite large similarities in cognitive, affective, interpersonal, and biological mechanisms in symptomology and etiology of these disorders (Newby et al., 2015; Queen et al., 2014). Repetitive negative thought, such as worry and rumination, is associated with depression and anxiety in adolescence and represents an important underlying mechanism for further intervention research. Future work can also examine whether the gains made during this treatment are maintained over time to promote long-term wellbeing during a critical developmental window.
Footnotes
The authors report no conflicts of interest.
Ethics Approval Statement
Research was conducted at University of Illinois at Chicago with approval from the Institutional Review Board and all parents and adolescents signed consent and assent, respectively.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. American Psychiatric Association, 2000. [Google Scholar]
- Angold A, Costello EJ, & Erkanli A (1999). Comorbidity. Journal of Child Psychology and Psychiatry, 40, 57–87. [PubMed] [Google Scholar]
- Barlow DH, Allen LB, & Choate ML (2004). Toward a unified treatment for emotional disorders. Behavior Therapy, 35(2), 205–230. [DOI] [PubMed] [Google Scholar]
- Brent DA, & Kolko DJ (1998). Psychotherapy: Definitions, mechanisms of action, and relationship to etiological models. Journal of Abnormal Child Psychology, 26(1), 17–25. [DOI] [PubMed] [Google Scholar]
- Brooks SJ, & Kutcher S (2001). Diagnosis and measurement of adolescent depression: a review of commonly utilized instruments. Journal of Child and Adolescent Psychopharmacology, 11(4), 341–376. [DOI] [PubMed] [Google Scholar]
- Brosschot JF, Gerin W, & Thayer JF (2006). The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychometric Research, 60, 113–124. [DOI] [PubMed] [Google Scholar]
- Burwell RA, & Shirk SR (2007). Subtypes of rumination in adolescence: Associations between brooding, reflection, depressive symptoms, and coping. Journal of Clinical Child and Adolescent Psychology, 36(1), 56–65. [DOI] [PubMed] [Google Scholar]
- Chelminski I, & Zimmerman M (2003). Pathological worry in depressed and anxious patients. Journal of Anxiety Disorders, 17(5), 533–546. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Earlbaum Associates. [Google Scholar]
- Curry J, Silva S, Rohde P, Ginsburg G, Kratochvil C, Simons A, Krichner J, May D, Kennard B, Mayes T, Feeny N, Albano AM, Lavanier S, Reinecke M, Jacobs RH, Becker-Weidman E, Weller E, Emslie G, Walkup J, Kastelic E, . . . March J (2011). Recovery and recurrence following treatment for adolescent major depression. Archives of General Psychiatry, 68(3), 263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T, & Watkins ER (2008). Repetitive negative thinking as a transdiagnostic process. International Journal of Cognitive Therapy, 1(3), 192–205. [Google Scholar]
- Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, Carmin CN, Biggs MM, Zisook S, Leuchter A, Howland R, Warden D, & Trivedi MH (2008). Difference in treatment outcome in outpatients with anxious versus nonanxious depression: A STAR*D Report. American Journal of Psychiatry, 165, 342–351. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, & Woodward LJ (2002). Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry, 59(3), 225–231. [DOI] [PubMed] [Google Scholar]
- Green B, Shirk S, Hanze D, & Wanstrath J (1994). The Children’s Global Assessment Scale in clinical practice: An empirical evaluation. Journal of the American Academy of Child & Adolescent Psychiatry, 33(8), 1158–1164. [DOI] [PubMed] [Google Scholar]
- Jacobs RH, Watkins ER, Peters AT, Feldhaus CG, Barba A, Carbray J, & Langenecker SA (2016). Targeting ruminative thinking in adolescents at risk for depressive relapse: Rumination-focused cognitive behavior therapy in a pilot randomized controlled trial with resting state fMRI. PLoS ONE, 11,(11): e0163952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanter JW, Mulick PS, Busch AM, Berlin KS, & Martell CR (2007). The Behavioral Activation for Depression Scale (BADS): psychometric properties and factor structure. Journal of Psychopathology and Behavioral Assessment, 29(3), 191–202. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, & Ryan N (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 980–988. [DOI] [PubMed] [Google Scholar]
- Keller MB, & Boland RJ (1998). Implications of failing to achieve successful long-term maintenance treatment of recurrent unipolar major depression. Biological Psychiatry, 44(5), 348–360. [DOI] [PubMed] [Google Scholar]
- Kennard BD, Emslie GJ, Mayes TL, Nakonezny PA, Jones JM, Foxwell AA, & King J (2014). Sequential treatment with fluoxetine and relapse-prevention CBT to improve outcomes in pediatric depression. American Journal of Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessing LV, Hansen MG, Andersen PK, & Angst J (2004). The predictive effect of episodes on the risk of recurrence in depressive and bipolar disorders–a life-long perspective. Acta Psychiatrica Scandinavica, 109(5), 339–344. [DOI] [PubMed] [Google Scholar]
- Kolaitis G (2012). Mood disorders in childhood and adolescence: Continuities and discontinuities to adulthood. Psychiatrike, 23, 94–100. [PubMed] [Google Scholar]
- Lewinsohn PM, & Essau CA (2002). Depression in adolescents. In: Gotlib IH & Hammen CL (Eds.), Handbook of depression. Guilford; 2002: 541–559. [Google Scholar]
- Liber JM, van Widenfelt BM, van der Leeden AJ, Goedhart AW, Utens EM, & Treffers PD (2010). The relation of severity and comorbidity to treatment outcome with cognitive behavioral therapy for childhood anxiety disorders. Journal of Abnormal Child Psychology, 38(5), 683–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, & Conners CK (1997). The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 554–565. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Borkovec TD, & Sibrava NJ (2007). The effects of worry and rumination on affect states and cognitive activity. Behavior Therapy, 38(1), 23–38. [DOI] [PubMed] [Google Scholar]
- Morrow J, & Nolen-Hoeksema S (1990). Effects of responses to depression on the remediation of depressive affect. Journal of Personality and Social Psychology, 58(3), 519–527. [DOI] [PubMed] [Google Scholar]
- Newby JM, McKinnon A, Kuyken W, Gilbody S, & Dalgleish T (2015). Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clinical Psychology Review, 40, 91–110. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S (2000). The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology, 100, 569–582. [PubMed] [Google Scholar]
- Nolen-Hoeksema S, & Morrow J (1993). Effects of rumination and distraction on naturally occurring depressed mood. Cognition and Emotion, 7, 561–570. [Google Scholar]
- Nolen-Hoeksema S, & Watkins ER (2011). A heuristic for developing transdiagnostic models of psychopathology explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6(6), 589–609. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S (2008). Rethinking rumination. Perspectives on Psychological Science, 3, 400–424. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Jarrett MA, Grills-Taquechel AE, Hovey LD, & Wolff JC (2008). Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention deficit/hyperactivity disorder, and oppositional/conduct disorders. Clinical Psychology Review, 28(8), 1447–1471. [DOI] [PubMed] [Google Scholar]
- Peters AT, Jacobs RH, Feldhaus C, Henry DB, Albano AM, Langenecker SA, Reinecke MA, Silva SG, & Curry JF (2015). Trajectories of functioning into emerging adulthood following treatment for adolescent depression. Journal of Adolescent Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poznanski EO, & Mokros HB (1996). Children’s Depression Rating Scale-Revised, Manual. Western Psychological Services. [Second printing 1999]. [Google Scholar]
- Queen AH, Barlow DH, & Ehrenreich-May J (2014). The trajectories of adolescent anxiety and depressive symptoms over the course of a transdiagnostic treatment. Journal of Anxiety Disorders, 28(6), 511–521. [DOI] [PubMed] [Google Scholar]
- Querstret D, & Cropley M (2013). Assessing treatments used to reduce rumination and/or worry: A systematic review. Clinical Psychology Review, 33(8), 996–1009. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Lyneham HJ, Hudson JL, Kangas M, Wuthrich VM, & Schniering CA (2013). Effect of comorbidity on treatment of anxious children and adolescents: results from a large, combined sample. Journal of the American Academy of Child & Adolescent Psychiatry, 52(1), 47–56. [DOI] [PubMed] [Google Scholar]
- Reynolds WM Reynolds Adolescent Depression Scale, (RADS-2). 1987.
- Rohde P, Clarke GN, Lewinsohn PM, Seeley JR, & Kaufman NK (2001). Impact of comorbidity on a cognitive-behavioral group treatment for adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry, 40(7), 795–802. [DOI] [PubMed] [Google Scholar]
- Rosnow RL, & Rosenthal R (1996). Computing contrasts, effect sizes, and counternulls on other people’s published data: General procedures for research consumers. Psychological Methods, 1, 331–340 [Google Scholar]
- Selya AS, Rose JS, Dierker LC, Hedeker D, & Mermelstein RJ (2012). A practical guide to calculating Cohen’s f2, a measure of local effect size, from PROC MIXED. Frontiers in Psychology, 3(111), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, & Aluwahlia S (1983). A children’s global assessment scale (CGAS). Archives of General Psychiatry, 40(11), 1228. [DOI] [PubMed] [Google Scholar]
- Titov N, Dear B, Staples L, Terides M, Karin E, Sheehan J, … Wootton B (2015). Disorder-specific versus transdiagnostic and clinician-guided versus self-guided treatment for major depressive disorder and comorbid anxiety disorders: A randomized controlled trial. Journal of Anxiety Disorders, 35, 88–102. [DOI] [PubMed] [Google Scholar]
- Topper M, Emmelkamp PM, & Ehring T (2010). Improving prevention of depression and anxiety disorders: Repetitive negative thinking as a promising target. Applied and Preventive Psychology, 14(1), 57–71. [Google Scholar]
- Treynor W, Gonzalez R, & Nolen-Hoeksema S (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research, 27(3), 247–259. [Google Scholar]
- Watkins ER (2008). Constructive and unconstructive repetitive thought. Psychological bulletin, 134(2), 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins ER (2016). Rumination-focused cognitive-behavioural therapy for depression. Guilford Press. [Google Scholar]
- Watkins ER, Moberly NJ, & Moulds ML (2008). Processing mode causally influences emotional reactivity. Emotion, 8(3), 364–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins ER, Mullan E, Wingrove J, Rimes K, Steiner H, Bathurst N, Eastman R, & Scott J (2011). Rumination-focused cognitive-behavioural therapy for residual depression: phase II randomised controlled trial. The British Journal of Psychiatry, 199(4), 317–322. [DOI] [PubMed] [Google Scholar]
- Watkins ER & Nolen-Hoeksema S (2014). A habit-goal framework of depressive rumination. Journal of Abnormal Psychology, 123(1), 24–34. [DOI] [PubMed] [Google Scholar]
- World Health Organizaton, (2008). World Health Organization: The global burden of disease: 2004 update. WHO Press, Geneva, Switzerland. [Google Scholar]
- Young JF, Mufson L, & Davies M (2006). Impact of comorbid anxiety in an effectiveness study of interpersonal psychotherapy for depressed adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 45(8), 904–912. [DOI] [PubMed] [Google Scholar]


