Abstract
Danzhen You and colleagues call for child health programming to take into consideration changing population sizes and dynamics
The world population reached 7.8 billion in 2020, tripling since 1950, and is expected to grow further in the next few decades.1 Population size, age structure, and geospatial distribution have changed over time and across regions and countries and will change further. Africa will continue to experience a surge in its child population, whereas Asia as a whole expects a declining child population. These changes pose challenges and opportunities for providing essential health services to children. Future health programming—the process of selecting interventions to improve health in a target population—must take into account demographic changes, including overall population trends and urbanisation, as they will contribute to health service needs.
A world with changing populations
The United Nations Population Division (UNPD) has a long history of estimating population sizes and projecting population changes for countries and territories.1 Although some academic institutions, most recently, the Institute for Health Metrics and Evaluation, produce their own population projections,2 we use the latest projections from UNPD1 to illustrate population changes over the next three decades because the methodology for constructing these is transparent and done in consultation with countries. Nonetheless, the population sizes and trends before 2050 are similar across the two sets of recent projections. Thus our conclusions are similar to those that other groups will observe in their projections.
The enormous growth of the world population in the past few decades, and expected to rise further,1 is not evenly distributed and will continue to differ by age groups and regions.
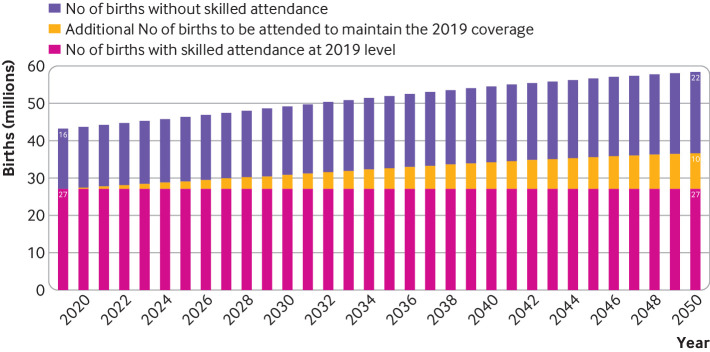
Asia is the continent with the largest population, but Africa is experiencing the fastest population growth and will almost double its population by mid-century. As of 2020, eight out of 10 people live in one of these two continents.1 With small changes in population sizes expected in the rest of the world, Asia and Africa drive global population trends. Both regions have an increasing total population, but differences in their patterns and trends of fertility and mortality lead to dissimilar demographic outcomes (fig 1; see also supplementary material for resulting differences in age structure, tables A1a and A1b and fig A4, and crude birth rate, fig A5).
Fig 1.
Population by age group in Africa and Asia, 1950-20501
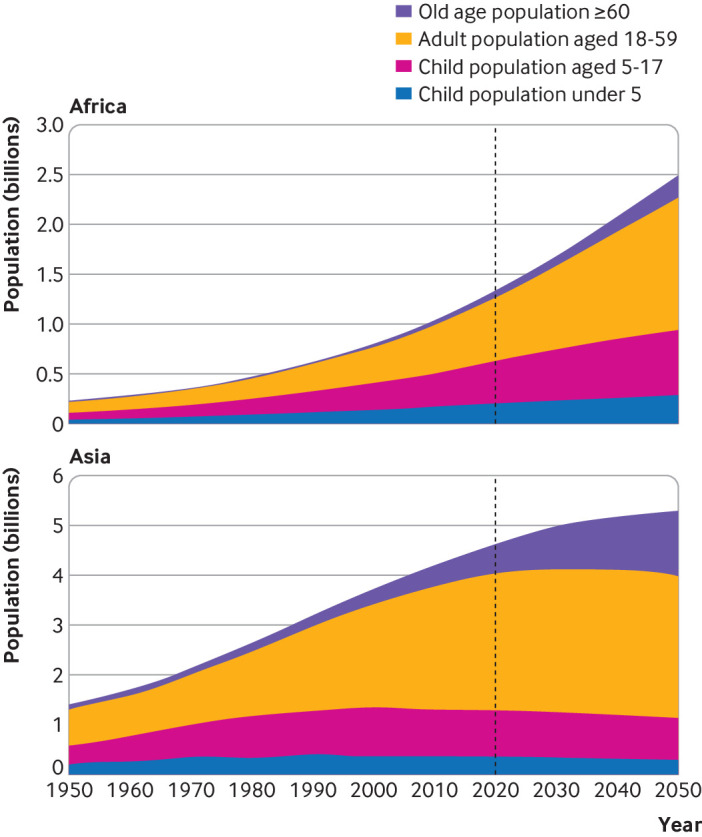
Africa is the only continent with substantial growth in the number of births and children (fig 2), expecting 1.6 billion births to occur in 2021-50—substantially higher than the 1.0 billion births in 1991-2020 (supplementary fig A1). A total of 43 countries, comprising 88% of the population in Africa will see an increase of annual births between now and 2050. In addition, Africa is projected to see a surge of around 315 million children and adolescents under age 18 from 626 million in 2020 to 942 million in 20501 (fig 2).
Fig 2.
Number of births and children under age 18, 1950-20501
In contrast, the number of births in Asia has declined since the late 1980s and is expected to decline further. The population of children and adolescents aged under 18 has also declined since 2000, and the trend is expected to continue in the next few decades. Asia, however, will still see 2.1 billion births in 2021-50 and a large child population of 1.1 billion in 2050. It will also have a rapidly ageing population with the number of people aged 60 or older increasing from 607 million (13.1%) in 2020 to 1.29 billion (24.4%) in 2050 (supplementary tables A1a and A1b).1
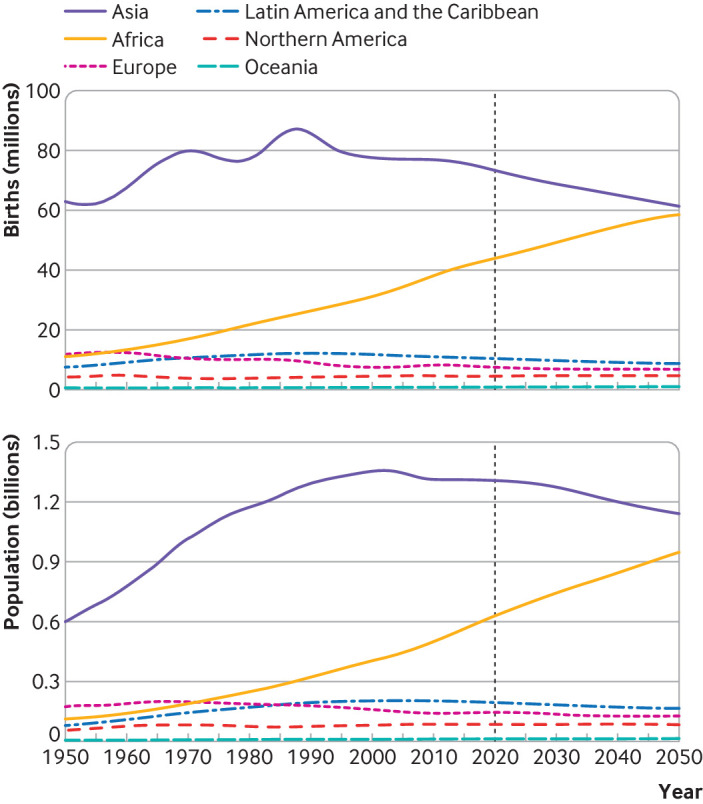
Asia is currently, and will continue to be, the region with the largest absolute number of births and total population, but the distribution of the world population will shift towards Africa, which will have an increasing share of births and children over the next few decades (fig 3). By 2050, four in 10 children and adolescents under age 18 will be Africans, an increase from three in 10 in 2020. More children are expected to live in Africa than in Asia from the mid-2060s onwards.1
Fig 3.
Share of births and children under age 18 by continent, 1950-20501
Global population growth is a distinctively urban phenomenon, with an increasing urban population but a stable rural population3 (supplementary figs A2 and A3). In 2007, half of the world’s population was living in urban areas. In 2020, this percentage had increased to 56%—that is, an urban population of 4.4 billion. Over a quarter of them are children and adolescents under 18 years of age. During 2020-30, the urban population is projected to expand on average by 24 million a year in Africa (20 million a year in sub-Saharan Africa), and by 45 million a year in Asia. The number of children living in urban areas will rise from 256 million to 342 million in Africa, and from 588 million to 645 million in Asia. By 2050, it is estimated that 59% of the African population will live in urban areas, increasing from 44% in 2020. In Asia, the percentage will rise from 51% to 66%.3
Current status of health services and outcomes
Timely and quality health services are essential to improve child survival and ensure healthy lives, but there are large gaps in healthcare provision in many African and Asian countries. Many children in these countries do not have essential healthcare because of a range of complex interrelated factors, including poverty, insufficient investments in health, and a lack of political will, leadership, and supportive policies.4 Sub-Saharan Africa has the greatest gaps in trained staff for health and the lowest coverage of key lifesaving interventions, such as antenatal care, skilled attendants at birth, caesarian sections when needed to save a mother and baby, postnatal care for mothers and babies, and immunisation against common childhood illnesses.4 5 In 2019, only 73% of infants in sub-Saharan Africa received the third dose of the diphtheria, tetanus, and pertussis vaccine—lower than the estimated global coverage of 85%.6 7 And only about six out of every 10 babies in sub-Saharan Africa were delivered by a skilled birth attendant. Furthermore, in sub-Saharan Africa, where most deaths from pneumonia occur, only 47% of children with pneumonia symptoms are taken for care, with the lowest proportions in western and central Africa. In South Asia, less than half of pregnant women received four antenatal care visits and 24% of babies were delivered without a skilled birth attendant.8 9
As a result of poor availability of quality healthcare, lack of clean water and sanitation, malnutrition, poverty, and other contributing factors, Africa remains the continent with the highest mortality rate in children under 5 years, with one child in 14 dying before his or her fifth birthday. This mortality rate is substantially higher than the average ratio of one in 199 in high income countries. Asia has the second highest rate, with one child in 37 dying under age 5. Africa and Asia together accounted for 95% of all deaths in children under 5 in 2019.10 The leading causes of child deaths in the two regions are infectious diseases and neonatal complications,10 all of which require essential health services and access to life saving treatments. In the past few decades, many African and Asian countries made progress in preventing child deaths and improving child health, but the progress is insufficient to meet the sustainable development goal 3, which calls for efforts to ensure healthy lives and promote wellbeing for everyone at all ages.11 In addition, service disruptions caused by the covid-19 pandemic may reverse the progress achieved, and therefore extra attention is needed to ensure that no one is left behind.4 10 12
Implications of population changes for health programming
The massive increase in population expected in many African countries will place additional burdens on the provision of essential services (eg, antenatal care, delivery care, postnatal care, immunisation services, and case management of childhood illnesses) to prevent maternal and child deaths and ensure healthy lives. Rapid population growth means that in the years to come more mothers and children will need essential health services, and substantially more resources will be required just to maintain current levels of key lifesaving interventions. If the trends towards urbanisation continue, African countries will need to invest in more urban health centres, including centres in slum areas, to avoid an increase in inequality among the urban poor.
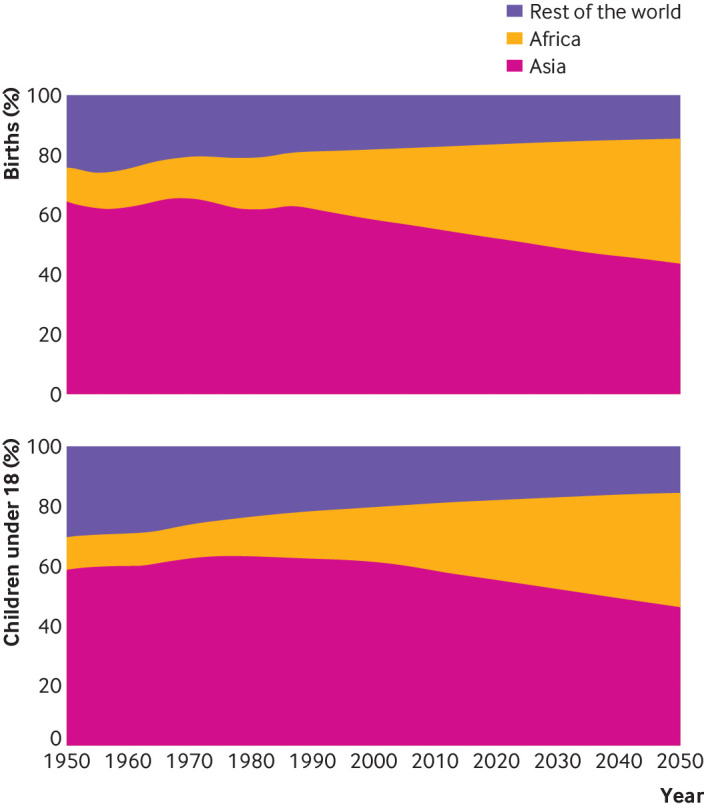
Africa had the highest neonatal mortality rate in the world in 2019 at 26 deaths per 1000 live births.10 A large proportion of neonatal deaths are caused by lack of skilled delivery care and treatment immediately after birth and in the first days of life. Figure 4 shows an example of the implication of Africa’s increase in births on the resources needed to ensure these births are attended by a skilled provider to prevent deaths (method shown in supplementary data). In 2019, Africa had 43 million births,1 of which 27 million (about 63%), were assisted by a skilled birth attendant and the rest were not.8 It is projected that the annual number of births in Africa will rise, and reach around 49 million in 2030 and 58 million by 2050.1 In order to maintain the 63% coverage level each year, a total of 22 million more births will need a skilled provider during 2020-30 and 164 million more in 2020-50. Achieving a higher coverage of skilled birth attendance and reducing the number of unassisted births will require even more intense efforts—to reach 90% coverage, a total of 173 million more births need a skilled birth attendant in 2020-30 (611 million more in 2020-50). Governments, international organisations, public health communities, and other key stakeholders need to train a large number of skilled birth attendants to meet the demand from the increasing numbers of births in Africa.
Fig 4.
Total number of births without skilled attendance, additional number of births to be attended to maintain the 2019 coverage, number of births with skilled attendance at 2019 level.1 Authors’ calculations based on United Nations Population Division1 and joint Unicef and World Health Organization database on skilled birth attendants, February 2020 (www.data.unicef.org)
A similar analysis of the required number of health service providers in Africa shows the gaps in service provision caused by population growth. The World Health Organization calls for a minimum of 44.5 doctors, nurses, and midwives per 10 000 inhabitants.13 Only five African countries reached this minimum standard (table 1). For Africa as a whole, this ratio in 2018 was 14.8 doctors, nurses, and midwives per 10 000 inhabitants, much lower than the global average of 53.2 health service providers per 10 000 inhabitants.14
Table 1.
Number of doctors, nurses, and midwives in Africa per 10 000 population, by country (2014-18)
| Country | No per 10 000 | Country | No per 10 000 | Country | No per 10 000 |
|---|---|---|---|---|---|
| Seychelles | 102.0 | Gambia | 16.5 | Congo* | 7.7 |
| Libya | 86.2 | Nigeria | 15.6 | Angola | 6.2 |
| Mauritius | 60.4 | Eritrea | 15.0 | United Republic of Tanzania | 6.0 |
| Botswana | 59.1 | Uganda | 14.0 | Liberia | 5.7 |
| Eswatini | 44.6 | Rwanda | 13.4 | Togo | 4.9 |
| Ghana | 43.3 | Kenya | 13.2 | Mali | 4.9 |
| Tunisia | 38.2 | Democratic Republic of the Congo | 11.8 | Malawi | 4.7 |
| Gabon | 36.3 | Mauritania | 11.1 | Benin | 4.7 |
| Lesotho* | 33.2 | Burkina Faso | 9.7 | Senegal | 3.8 |
| Algeria | 32.7 | Sudan | 9.6 | Niger | 3.1 |
| Zambia | 25.2 | Burundi | 9.5 | Madagascar | 3.1 |
| Egypt | 23.8 | Djibouti | 9.5 | Central African Republic | 2.8 |
| Namibia | 23.7 | Equatorial Guinea | 9.0 | Chad | 2.8 |
| South Africa | 22.1 | Comoros | 9.0 | Sierra Leone* | 2.5 |
| Zimbabwe | 21.4 | Côte d’Ivoire | 8.1 | Guinea | 2.1 |
| Morocco | 21.2 | Guinea-Bissau | 8.1 | Somalia | 1.3 |
| Cabo Verde | 20.5 | Ethiopia | 7.9 | Cameroon* | 0.9 |
| Sao Tome and Principe | 19.8 | Mozambique | 7.7 |
Countries with latest data available in 2009 to 2013. Note that countries or areas with data older than 2009 or without data are not listed in the table.
Source: Analysis based on WHO Global Health Observatory, https://apps.who.int/gho/data/node.main.SDG3C?lang=en, accessed on 26 October 2020.
In 2018, Africa had around 1.9 million primary health service providers (doctors, nurses, and midwives).14 If the number per population in each country listed in table 1 is kept constant up to 2030, the continent will have to add more than 517 000 skilled health professionals by 2030, for a total of 2.4 million, to compensate for the projected population growth. On top of this, an additional 5.1 million professionals will be needed for the continent to reach the WHO minimum standard of 44.5 skilled health professionals per 10 000 population, for a total of 7.5 million professionals in 2030. To reach the minimum standard by 2050, Africa would require a total health work force of 11.1 million—almost six times as many as the current number (fig 5). This ratio is smallest in northern Africa (1.4) and ranges in sub-Saharan Africa from 4.2 in southern Africa to 8.6 in eastern Africa (method used shown in supplementary data, results by subregion shown in supplementary fig A6).
Fig 5.
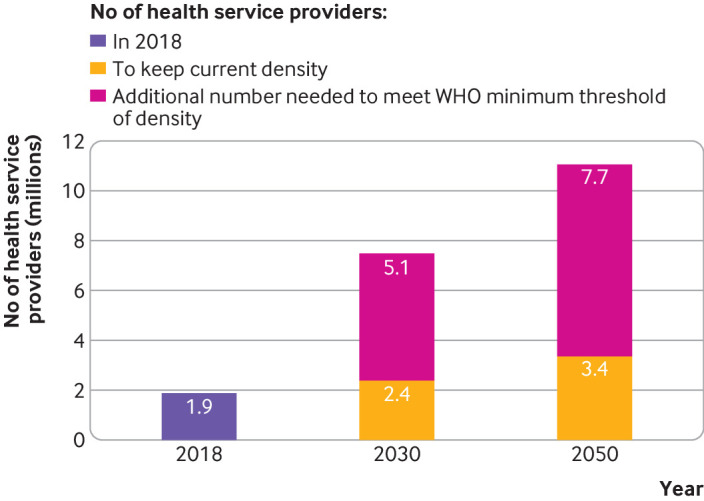
Number of health service providers (doctors, nurses, and midwives) in 2018 (purple bar) and required in 2030 and 2050 when maintaining current density (yellow) and additional number needed for meeting World Health Organization minimum threshold of density (deep pink), Africa. Analysis based on countries with available data for doctors, nurses, and midwives from 2014 or later. Regional aggregates were calculated using weighted averages. The WHO minimum threshold of density is 44.5 skilled health professionals per 10 000 population. Unicef analysis based on WHO Global Health Observatory (https://apps.who.int/gho/data/node.main.SDG3C?lang=en).
In contrast to Africa, Asia is experiencing a decline in the number of births and the child population. Around 68 million births are expected in 2030, about five million less than in 2020. Over the same period, the child and adolescent population under age 18 will shrink by 38 million. Forty out of 51 countries or territories in Asia will see a decline in the number of births. In addition, 25 countries or territories are projected to have a smaller child population.1 Nevertheless, Asia has the largest number of births and child population in the world and a gap in many health interventions, therefore supportive policies and programmes need to be strengthened to maintain and improve essential services for all children.
Taking the population into account in planning and programming is not only about population size, but also other factors, including population distribution in urban and rural areas. Rapid urbanisation is occurring in many African and Asian countries.3 Urbanisation has a positive effect if it is accompanied by advancements in technology and infrastructure, the construction of sufficient quality educational and medical facilities, and improved living standards. Extensive and unplanned urbanisation often results in adverse effects, leading to greater poverty, with local governments unable to provide services for all people. Poor air quality, insufficient water availability, and waste disposal problems, already prevalent in many urban centres, are exacerbated by increasing populations, taking a toll on human health.15 Informal settlements and insecure residential status exclude many urban households from services provided by the government. Today, approximately one billion people live in slums,11 the worst form of informal settlement, and hundreds of millions of them are children. The quality of urban services for marginalised and disadvantaged people is poor. Studies show glaring disparities in health outcomes in urban areas and that many of the poorest urban children fare worse than children in rural areas.16 17 A Unicef study of over 70 countries found that in almost 30% of these countries analysed, the poorest urban children have lower diphtheria, tetanus, and pertussis immunisation coverage than the poorest children in rural areas.17 In the absence of strategies favouring the poor, inequity in child health may widen, and an increasing number of urban children may be left behind. Programming for children must take into account the particular conditions in urban settings in Asia and Africa, where over 80% of the world’s children and adolescents are living and where urbanisation is happening rapidly.
A renewed approach
Health programming must consider population characteristics and trends. Population data can be used to quantify the need and target locations for specific programmes and services. Countries with a growing population, many of those situated in sub-Saharan Africa, can use information on population size, density, and geospatial distribution to determine how many health workers need to be trained and where they should be deployed, the number of healthcare facilities, including hospitals, needed and where they should be located across the country, and the volume of supplies needed, including the number of vaccines. These decisions are crucial for delivery of high quality, essential services.
The projected rapid population growth in most African countries will pose immense challenges to the continent’s ability to reach all in need with essential health services, but also presents opportunities if properly harnessed. Numerous studies have shown the transformative power of investment in essential services for children, adolescents, and youth.18 19 20 21 22 23 24 Urgent efforts and investments by governments, the United Nations and its agencies, public health communities, and donors are required to ensure that African countries, particularly those in sub-Saharan Africa, have sufficient health facilities and health workers to provide preventive and curative health services for their growing populations. Inaction now will result in an unprecedented burden, and millions of children could grow up underserved or die from preventable causes.
Many countries in Africa and Asia are facing rapid urbanisation with challenges to increase the extent of urban programming for essential services. In Africa, urbanisation is occurring among countries with a lower level of per capita national income than in other regions.17 In particular, in sub-Saharan Africa, urbanisation has not coincided with economic growth. Between 1970 and 2000 the urbanisation level in sub-Saharan Africa increased from approximately 20% to 30%, while gross domestic product per capita decreased over the same period.25 Urbanisation without shared economic growth has the danger of creating a whole class of urban poor deprived of necessary services and security, living in slums at the margins of urban centres.26 As more and more children live in cities and towns with many of them living in poverty, it is becoming increasingly critical to scale up urban programming, provide services to all mothers and children including the urban poor, and reduce intra-urban inequity. To do so, the urban setting has to become an integral part of programming for mothers and children; capacities of inclusive urban planning must be further developed at all levels of government—national, regional, and local; and solutions must be found for the lack of financial resources needed to improve urban systems and to increase equity within urban areas.17
Consideration of population characteristics and trends shows that Africa and Asia need a blend of political will, evidence based strategies, innovation, enhanced implementation capacity, and adequate financing to ensure that mothers survive, and children and young people can grow up to become healthy and productive members of society. Large heterogeneity exists across countries. The majority of the 54 African countries will continue to have an increase of births, but 11 countries will see a decline between now and 2050.1 Coverage of the diphtheria, tetanus, and pertussis vaccine was 80% or more in 35 African countries, between 50% and 80% in 15 countries, and lower than 50% in 4.6 The coverage of skilled birth attendance ranged from 24.3% in Chad to 99.8% in Botswana and Mauritius.8 These examples highlight the need for countries to take actions according to the current status of health services and outcomes and future population changes.27
Key messages.
Rapid population growth in Africa will place considerable pressure on health systems with resource constraints
Rapid urbanisation is occurring in many African and Asian countries, leading to greater poverty and taking a large toll on human health
Urban programming needs to increase to service all children and particularly the urban poor.
Health programming must take into consideration population characteristics and the current status of health services and outcomes to meet service needs equitably
Prioritising investments in children’s health to reap the demographic dividend is critical in many countries in Africa and Asia
Acknowledgments
We thank Liliana Carvajal, Mamadou Saliou Diallo, Lauren Francis, Lucia Hug, Padraic Murphy, and David Sharrow from Unicef for providing data on intervention coverage and mortality. Special thanks to Amiya Bhatia and Shripad Tuljapurkar for useful review comments.
Web extra.
Extra material supplied by authors
Details of data and methods
.Contributors and sources:. DY conceived the paper and drafted the first version. JB and SL conducted the data analysis. JB, JR, and KS contributed to drafting and editing. The population data used in the analysis come from the United Nations Population Division. Health intervention coverage data are from household surveys. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated. DY is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no conflict of interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of a series proposed by WHO and Unicef and commissioned by The BMJ, which peer reviewed, edited, and made the decision to publish. Article handling fees, including open access are funded by WHO and Unicef.
References
- 1.United Nations, Department of Economic and Social Affairs, Population Division. World population prospects 2019. Online edition, revision 1, 2019. https://population.un.org/wpp/
- 2. Vollset SE, Goren E, Yuan CW, et al. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. Lancet 2020;396:1285-306. 10.1016/S0140-6736(20)30677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United Nations, Department of Economic and Social Affairs, Population Division. 2018 Revision of world urbanization prospects. 2018. https://population.un.org/wup/
- 4.World Health Organization and the United Nations Children’s Fund. Protect the progress: rise, refocus, recover. Progress report on the every woman every child global strategy for women’s, children’s and adolescents’ health (2016-2030). Geneva: World Health Organization and the United Nations Children’s Fund, 2020. https://protect.everywomaneverychild.org/assets/img/2020-Progress-Report-on-the-EWEC-Global-Strategy-Final.pdf
- 5.Unicef. The state of the world’s children. 2019. https://www.unicef.org/reports/state-of-worlds-children-2019
- 6.WHO and Unicef estimates of national immunization coverage 2019 revision. https://data.unicef.org/topic/child-health/immunization/
- 7.Immunization coverage: are we losing ground? UNICEF and WHO. 2020. https://data.unicef.org/resources/immunization-coverage-are-we-losing-ground/
- 8.Joint Unicef and WHO database on skilled birth attendant, February 2020 www.data.unicef.org
- 9.Unicef global databases, August 2020 based on Demographic and Health Surveys, Multiple Indicator Cluster Surveys and other national surveys. www.data.unicef.org
- 10.United Nations Inter-agency Group for Child Mortality Estimation. Levels and trends in child mortality: report 2020. 2020. https://childmortality.org/wp-content/uploads/2019/10/UN-IGME-Child-Mortality-Report-2019.pdf
- 11.United Nations, Department of Economic and Social Affairs, Statistical Division. The sustainable development goals report 2019 . 2019. https://unstats.un.org/sdgs/report/2019/#sdg-goals
- 12. Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health 2020;8:e901-8. 10.1016/S2214-109X(20)30229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scheffler R, Cometto G, Tulenko K, et al. Health workforce requirements for universal health coverage and the sustainable development goals—background paper n.1 to the WHO global strategy on human resources for health: workforce 2030. World Health Organization, 2016. https://www.who.int/hrh/resources/health-observer17/en/
- 14.World Health Organization. World health statistics 2020: monitoring health for the SDGs. 2020. https://apps.who.int/iris/bitstream/handle/10665/332070/9789240005105-eng.pdf?ua=1
- 15.UN-Habitat. World cities report 2016: urbanization and development – emerging futures. 2016. https://unhabitat.org/sites/default/files/download-manager-files/WCR-2016-WEB.pdf
- 16.Save the Children. The urban disadvantage: state of the world’s mothers. 2015. https://www.savethechildren.org/content/dam/usa/reports/advocacy/sowm/sowm-2015.pdf
- 17.Unicef. Advantage or paradox: the challenge for children and young people of growing up urban. 2018. https://data.unicef.org/wp-content/uploads/2018/11/AdvantageOrParadox_rev1_web.pdf
- 18.Katz B, Tilchin R. Investing in the next generation: a bottom-up approach to creating better outcomes for children and youth. Brookings Institute. August 2017. https://www.brookings.edu/research/investing-in-the-next-generation-a-bottom-up-approach-to-creating-better-outcomes-for-children-and-youth/.
- 19.Huebner G, Boothby N, Aber JL, et al. Beyond survival: the case for investing in young children globally. Discussion Paper. National Academy of Medicine. June 2016. https://nam.edu/beyond-survival-the-case-for-investing-in-young-children-globally/
- 20.United Nations Children’s Fund. Right in principle and in practice: A review of the social and economic returns to investing in children. UNICEF. June 2012. https://www.unicef.org/socialpolicy/files/Investing_in_Children.pdf
- 21. Belli PC, Bustreo F, Preker A. Investing in children’s health: what are the economic benefits? Bull World Health Organ 2005;83:777-84. [PMC free article] [PubMed] [Google Scholar]
- 22.Hempel K, Cunningham W. Investing in your country’s children and youth today: good policy, smart economics. Child & Youth Development Notes. World Bank, 2010:IV(1). http://documents1.worldbank.org/curated/en/360861468314362308/pdf/806420NEWS0Inv00Box379809B00PUBLIC0.pdf
- 23.Hempel K, Wuermli A, Lundberg M. Adolescence: protecting and promoting human development in times of economic shocks, social protection and labor. Policy Note: Labor Market and Youth. World Bank, 2012:13. http://documents1.worldbank.org/curated/en/290641468181465405/pdf/699950BRI00PUB0icy0Note01300PUBLIC0.pdf
- 24.Unicef. Generation 2030 Africa 2.0: prioritizing investments in children to reap the demographic dividend. November 2017. https://data.unicef.org/resources/generation-2030-africa-2-0/
- 25.United Nations. Department of Economic and Social Affairs, World Economic and Social Survey 2013: sustainable development challenges. 2013:60. https://www.un.org/en/development/desa/policy/wess/wess_current/wess2013/WESS2013.pdf
- 26.Dudwick N, Hull K, Katayama R, Shilpi F, Simler K. From farm to firm rural - urban transition in developing countries. 2011. https://documents.worldbank.org/curated/en/547481468330918163/pdf/622590PUB0farm0476B0extop0id0186230.pdf
- 27. Wehrmeister FC, Fayé CM, da Silva ICM, et al. on the behalf of the Countdown to 2030 for Women’s, Children’s and Adolescents’ Health regional collaboration in sub-Saharan Africa . Wealth-related inequalities in the coverage of reproductive, maternal, newborn and child health interventions in 36 countries in the African Region. Bull World Health Organ 2020;98:394-405. https://www.who.int/bulletin/volumes/98/6/19-249078/en/. 10.2471/BLT.19.249078 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Details of data and methods