Abstract
Advances in information and communication technology (ICT) are having an increasing impact on the practice of ophthalmology. Successive generations of 4G networks have provided continued improvements in bandwidth and download speeds. Fibre-optic networks were promised as the next step in the development of a faster and more reliable network. However, due to considerable delays in their widespread implementation, original expectations have not been met. Currently, the new 5G network is on the verge of widespread release and aims to offer previously unparalleled bandwidth, speed, reliability and access. This review aims to highlight the potential profound impact near instantaneous communication (the 5G network) may have on ophthalmology and the delivery of eyecare to the global population. Conversely, if the new network fails to deliver as intended, the wireless network itself may become yet another obstacle to adopting next-generation technologies in eyecare.
Subject terms: Health services, Medical research
5G通信技术对眼科的潜在影响
摘要
信息和通信技术 (ICT) 的进步对眼科临床产生了越来越大的影响。连续几代的4G网络在带宽和下载速度方面都有了持续性的提高。光纤网络将成为下一代发展更快、更可靠的网络通讯技术。然而, 由于广泛普及中的严重拖延, 该技术未能达到最初的预期。目前, 新的5G网络技术即将广泛发布, 旨在提供空前未有的频宽、速度、可靠性和接入能力。本综述旨在强调瞬时通信技术 (5G网络) 对眼科学和全球范围内眼科医疗活动潜在的、深远的影响。相反, 如果新的网络技术的普及未能达到预期目标, 那么无线网络本身就可能成为在眼科医疗活动中采用下一代技术的另一个障碍。
Introduction
The current landscape of ophthalmology and medicine is rapidly transforming as a direct result of exponential advancements in information and communication technology (ICT). One of the major advances in ICT over the last two decades has been the development of broadband cellular networks. The widespread roll out of 4G networks has, with each successive generation, provided improved bandwidth and download speeds. Fibre-optic networks were promised as the next step in the development of a faster and more reliable network. However, due to considerable delays in the widespread implementation of these networks, original expectations have not been met. Currently, the new 5G network is on the verge of widespread release and promises unparalleled bandwidth, speed, reliability and access. If the 5G network delivers as promised, the potential exists for an increased focus on the development of virtual reality (VR), artificial intelligence (AI), teleophthalmology and telesurgery. In order to reliably develop and successfully implement this new ICT within healthcare, a substantially improved network than what is currently available worldwide is required. If this does not occur, the potential exists for the network itself to be a major barrier to healthcare. This review aims to highlight the potential profound impact near instantaneous communication (the 5G network) may have on ophthalmology and the delivery and adoption of next-generation technologies worldwide.
Main text
Overview of the current networks worldwide
Presently there are up to five main categories of networks available worldwide: ADSL (asymmetric digital subscriber line), wireless cellular, cable, fibre optic and less commonly satellite [1, 2]. The ADSL is a type of broadband that allows the transferring of data over existing copper telephone lines, 4G is a wireless broadband network, cable employs a combination of fibre optic and coaxial cables for data delivery and fibre optic delivers data via a cluster of fibre optic cables [3, 4]. Literature from 2017 demonstrates South Korea (KOR), Norway (NOR), Sweden (SWE), Hong Kong (HKG) and Switzerland (CHE) had the top five average connection speeds globally [5]. Interestingly, the report also demonstrated that the United States of America (USA) ranked 10th with 18.7 Mbps, the United Kingdom (UK) placed 16th, Australia (AUS) was ranked 50th and China (CHN) ranked 74th with an average speed of just 7.4 Mbps. These statistics highlight the failure of current generation networks to provide a uniformly fast and reliable service in even some of the more economically developed countries.
In terms of access to the internet, there were ~4.5 billion internet users in the world at the end of 2019, with Asia and Europe having the greatest proportion of internet users (50.3% and 15.9%, respectively) [6]. In 2016, 88% of people aged 55–64 used the internet recently in the United Kingdom, this decreased slightly to 74% for those aged 65–74 and was 39% for those aged 75+ [7]. Similarly, in the United States, 67% of those aged over 65+ used broadband internet, with the highest usages in the 65–69 and 70–74 brackets (82% and 75%, respectively) [8]. In the Southern hemisphere, an Australian study examining internet usage by those over 50 found 82% of respondents had internet access and 93% actively used the technology [9]. A report from Opensignal found users in KOR, JPN, NOR, HKG and the United States consistently had access to 4G 90% of the time [10]. In comparison, Australian users had 4G access in 86% of cases and UK users were able to access the 4G network services 77% of the time. These statistics highlight a major proportion of the world’s population has access to and is comfortable using the internet. If the new 5G network is able to deliver as promised, the integration of technologies to assist in the eyecare of patients is promising.
What is 5G?
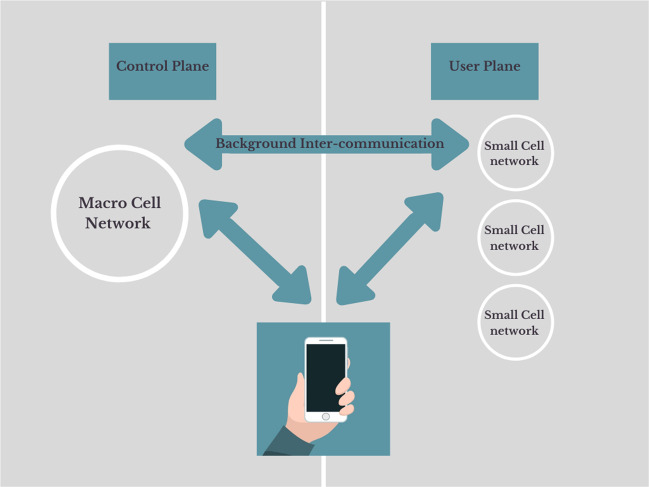
The 5G network is the fifth generation of wireless broadband networks, offering speeds and reliability that surpass its 2G, 3G and 4G predecessors. 5G is based on the use of an architectural structure incorporating the conventional macrocellular network with an overlay of small cell networks [11]. As shown in Fig. 1, this allows users to connect to two networks simultaneously. The dual connectivity allows the macrocellular network to act as the control plane and the small cells to act as the user plane. The control plane is responsible for signalling between networks and the user plane is assigned for data services (e.g. video streaming or calls). The use of two separate (yet intercommunicating) networks intends to create a higher performing network.
Fig. 1. A schematic representation of the 5G network.
The control plane represents the division of 5G responsible for background communication between networks. The user plane represents the networks responsible for data services. The user, macrocellular and small cell nextworks all intercommunicate (double-sided arrows) and work in synergy.
Peak data rates for the new 5G network have been reported to be in the range of 5.8–10 Gbps, with Vodafone UK reporting average speeds of 150–200 Mbps [12, 13]. Theoretically, at peak rates, the new network will be at least two orders of magnitude faster. According to Lifewire, in order to stream 4K Ultra HD content on YouTube, a speed of at least 15 Mbps is needed to stream without interruptions [14]. As the current generation network’s average speed in many countries is below this requirement, more people are forced to stream at lower resolutions. Though this difference may be minor when watching video streams for entertainment, the difference in resolution and latency is considerably more important in medical applications, such as remote surgery. While data on the minimum resolution requirements for remote surgery are not available, the impact of resolution on performance during endoscopic and laparoscopic procedures is more well established. One study of 11 expert laparoscopic surgeons reported a 2D/4K monitor resulted in better surgical performance amongst participants compared to a 2D/HD monitor. Furthermore, surgical performance using 2D/4K monitor while operating in narrow spaces was comparable to a 3D/HD monitor [15]. Another study evaluating the impact of resolution on trans-spheroidal pituitary surgery found that the 4K endoscope enhanced the reliability of intraoperative judgement on the extent of resection when compared with its HD counterpart, thereby minimising unexpected residuals post-operatively [16].
Though the prospect of 5G is promising, there are some challenges in its implementation. 5G is reliant on different waveforms to its predecessors, many current devices are not compatible and thus new compatible devices will need to be purchased in order to experience the benefit of the new network. In addition, the widespread distribution of the population and the large geographics of nations will also create challenges with regard to implementing adequate infrastructure for the new 5G network. The importance of addressing these infrastructural and coverage limitations is paramount to allow the world population to entirely experience the potential profound impact 5G may have on ophthalmic care.
Wireless cellular networks, such as 5G have historically been optimised for on-the-go connectivity, whereas the other networks (e.g. cable, fibre optic) offer more stable connectivity needed in permanent structures. Whilst the new generation 5G offers unparalleled bandwidth and wireless connectivity, the networks ability to offer reliable connectivity indoors remains a challenge. The new 5G operates at millimetre wave bands (24, 28, 37 and 39 GHz) and mid-spectrum bands (2–3 GHz) in addition to 1–2-GHz spectrum used by current generation wireless networks [17]. The most notable challenge with millimetre wave frequencies is that they have difficulty penetrating dense building structures or foliage. This is due to these wave bands being of a shorter wavelength and thus unable to propagate through high-density structures [18]. Telecom providers are aiming to overcome the challenges of indoor reliable connectivity through the use of small cells, with providers aiming to increase the number of small cells by 900% from 2018 to 2026 [19]. The major benefit of multiple small cells compared to traditional large cells is considerably less land space is required, overcoming the challenges associated with acquiring land in high-density metropolitan regions. Furthermore, the likely lower costs and increased efficiency of establishing 5G makes the wireless network preferred over dedicated fixed-line communication for widespread use.
Demographics of the world population
According to the World Health Organisation, at least 2.2 billion people suffer from a vision impairment (best eye presenting < 6/12) or blindness [20]. The World Bank estimated ~45% of the world population was based in rural areas [21]. This average is a direct result of countries, such as Trinidad and Tobago, Burundi, Papua New Guinea and Liechtenstein have at least 85% of their citizens inhabiting rural areas [22]. Conversely, countries, such as AUS, UK and USA having a predominantly urban population, with no more than 40% of the citizens in these countries residing in rural areas [23–25]. While literature is not available on the rural vs urban distribution of ophthalmologists in countries, such as the UK and USA, data from AUS and Africa does suggest the majority of ophthalmologists are based in capital cities [26, 27]. Assuming the same applies globally, in its current state, the ability of those in rural or remote areas to access specialised eyecare is limited by the distribution of readily available ophthalmic care. In addition, non-urgent referrals to some ophthalmology departments can result in prolonged wait times for outpatient visits and elective surgery. Given the large geographic of the global populous and the disproportional distribution of ophthalmic workforce, instantaneous communication promised by 5G may be key in improving the delivery of eyecare.
The potential of the 5G network
Virtual reality
VR technology has the potential to enhance eye healthcare via a number of avenues, including improved patient communication and education, and its incorporation into ophthalmic surgical training. Language barriers may compromise the eye healthcare of many patients due to challenges in information communication. A more efficient network carries with it the potential to further improve the quality of translation services provided, particularly at centres in less multicultural towns/cities. The proposed new network offers the opportunity to increase both the number of languages/dialects available for translation and quantity of remote translators available from other geographical regions (e.g. overseas). The VR technology can be used to provide real-time translation services, while considerably reducing the impact of lack of translator availability in providing a high standard of healthcare. Furthermore, some languages are heavily reliant on non-verbal cues and the translator being able to “virtually” interact with a patient face to face would likely help to improve communication.
Emerging evidence is demonstrating the utility of VR technology as a patient education tool [28, 29]. The “image intensive” nature of ophthalmic practice is highly suited to this technology. In order to play a VR video at 240p (very low equivalent TV resolution), a bandwidth of 25 Mbps is required, with an increase in required bandwidth to 1 Gbps for the equivalent of 4K resolution (very high definition) [30]. The current average bandwidth in many developed countries is currently well below this [5, 12]. However, the 5G network makes the incorporation of VR into ophthalmic practice a real possibility.
Presently, ophthalmology training programmes face considerable challenges in ensuring all trainees receive a consistent and uniform experience through the duration of their training. Worldwide, the challenges associated with ensuring a consistent trainee experience include an unstructured curriculum, financial costs, human costs and time constraints [31]. The widespread use of VR technology to assist in trainee education may play a key role in addressing some of the aforementioned barriers to surgical training. In its current form, VR technology is available through the use of simulators for trainee education. The EYESI surgical simulation system has been used to develop a training curriculum for phacoemulsification surgery and the MicroVisTouch surgical simulator has been used to simulate components of vitreoretinal surgery [32, 33]. Furthermore, the use of such technology as an objective measure of a trainees ability is encouraging. A study from Denmark reported a high correlation between performance on the EYESI surgical simulator and real-life surgical performance in cataract surgery [34]. Another study from Germany reported the use of EYESI simulator as a warm-up improved average performance during vitreoretinal surgery and had a positive correlation with performance on the simulator versus in theatre [35]. Though these results are encouraging, the availability and cost of these simulators as well as expert demonstrators have likely limited their implementation worldwide.
The arrival of the 5G network holds the potential address these barriers and improve the provision of VR education to trainees. The high speeds and considerable increase in bandwidth offered by the new 5G network create the possibility for the use of digitally assisted virtual surgery (DAVS) e.g. NGENUITY by Alcon or Artevo 800 by Zeiss in surgical education. DAVS systems compared to analogue microscopes offer higher-performance magnification, improved depth of field, operating at lower levels of illumination, no use of chemical dyes for image enhancement and better ergonomics for surgeons [36, 37]. Increasingly, surgeons are finding features of DAVS that could not be achieved on traditional microscopes, such as on-screen integration with overlays of other intraoperative image modalities, e.g. toric marking, endoscopic or intraoperative optical coherence tomography (OCT) views and fluidics parameters [38]. The viewing on a 4K display screen allows the opportunity for not only the surgeon but also any trainees in the room to view the same images simultaneously. The streaming of these 4K feeds live to trainees in other geographical regions would potentially allow for a means of real-time surgical training. This 4K streaming technology may also be greatly beneficial to overseas fellows as it would assist in eliminating several challenges faced by fellows in order to receive specialist training including regulations, language differences and costs associated with travel. Furthermore, implementation of DAVS may assist in reducing the impact of limited availability of local surgeons to make dedicated teaching trips to other geographical locations. An additional benefit of DAVS is that it holds the potential to allow retired surgeons no longer suited to surgical work to act as dedicated educators in remote supervising roles and could allow instant access to expert advice regarding more complex cases. The use of 5G for the implementation of DAVS is exciting. The new network could allow surgery occurring in tertiary/quaternary centres to be live streamed to overseas trainees with full depth perception and augmented overlays, offering a learning experience comparable to that of being physically present within the operating theatre.
The integration of VR in medicine demonstrates a great deal of promise; there are however several factors requiring consideration prior to its widespread implementation. According to current reports, a bandwidth of 100 Mbps is required in order to live-stream sub-4K resolutions with full immersion for more than 15 min without nausea [39]. This speed requirement far exceeds what is available on the current generation of networks; however, the new 5G network carries with it the potential to address this major barrier limiting the widespread implementation of VR. In addition to inadequate bandwidth, a major limitation of the VR technology is its design; devices tend to be bulky, have cumbersome wiring and limited battery life [40]. Furthermore, the cost of VR simulators can exceed $170,000 AUD and decreasing this cost will also assist in increased its integration into ophthalmology [41]. The live streaming of VR feeds over large distances also creates an issue of confidentiality. Ensuring confidentiality regarding a patient’s medical condition is one of the key underpinning principles of medical practice. Encryption of transmissions would greatly assist in reducing the risk of cyber hijacking, it would also be important to convey this added risk to patients participating in VR communication.
Artificial intelligence
AI is a generalised term used to describe a system that displays properties of human intelligence [42]. Deep learning refers to the inputting of a large amount of raw data in multiple layers of representation, with each subsequent input allowing the system to improve its ability to discriminate between data and classify the information presented [42]. The implementation of AI into the clinical care of patients presents an opportunity to significantly impact the efficiency of workflow, whilst maintaining a high standard of care. The large volumes of image-based data, particularly in the medical retina subspecialty, are well-suited to “AI training”. A Taiwanese study reported that the sensitivity and specificity of a cloud-based AI utilising OCT for the detection and classification of aged-related macular degeneration (AMD) was similar to experienced retinal specialists [43]. This study also reported that the AI made appropriate management recommendations [43]. Another study from Germany, which trained the AI on 1.2 million OCT images demonstrated over 95% sensitivity and specificity to detect exudative AMD [44]. Similar results have been shown with the use of AI for the diagnosis of diabetic retinopathy (DR) [45, 46]. Having near-instantaneous communication with aforementioned trained networks can herald an age of “instant” triaging where primary care workers can upload high-resolution scans and receive instant “specialist equivalent” triaging feedback. This will significantly short-circuit the traditional referral pathway and hopefully allow urgent cases to be accurately triaged and referred.
AI is also conceivably a tool that could overcome language barriers. Theoretically, an AI translator could “speak” an indefinite number of languages facilitating clinician–patient communication. Although limited data is currently available, companies, such as Google and Baidu, are showing great progress in this area and the arrival of highly proficient AI translators may be on the horizon [47, 48].
While AI technologies are available offline, it may not be feasible (in terms of cost or technician availability) to place all of the infrastructure necessary in smaller or more remote centres. An efficient 5G network could allow for the use of cloud-based technologies as discussed above and also allow for instantaneous transmission of data required for AI analysis from smaller hospitals to larger centres with access to AI infrastructure.
Teleophthalmology
In recent times, videoconferencing for ophthalmology patients has been explored as a potential solution for the challenges created by the urban-centric distribution of ophthalmologists. The data available thus far does suggest that teleophthalmology may be a viable method of patient care, particularly for those in rural or remote areas. An audit of 709 patients consulted through the use of teleophthalmology by Lions Outback vision in AUS found they were able to successfully diagnose 95% of patients [49]. Furthermore, teleophthalmology was able to provide access to surgical interventions more efficiently. Over this 1-year period, the use of teleophthalmology saved over 10 days of outreach clinic, based solely on the 287 cataract patients seen and managed [49]. This highlights the potential for teleophthalmology programmes to not only reduce the impact of geographic distribution on patient care but also to reduce waiting times for elective surgery. A meta-analysis from Canada reported that teleophthalmology was equivocal to face-to-face consultations for detection of age-related macular degeneration and DR [50]. This further supports the use of teleophthalmology for the eyecare of patients in the future. A teleophthalmology screening system used for ophthalmic triaging in remote Brazil, reported 85% accuracy and a negative predictive value of ~97% when compared to an onsite local ophthalmologist [51]. This study involved the use of a single mobile phone for image and patient information collection. A similar system could be deployed for those patients in more remote regions.
The patient response to the use of teleophthalmology has also been encouraging. A study of 109 patients who used the service in rural Western AUS found 69.1% of patients were “very satisfied” and 24.5% were “satisfied”, with no patients reporting they were dissatisfied or worse [52]. The study also found older patients felt they could easily explain their medical issues over conferencing, the service was time-saving and saved them significant costs that would be associated with travelling to appointments. Similarly, a Spanish study reported that ~94% of patients gave a score of at least 8 out of 10 for general satisfaction when partaking in a teleophthalmology-based screening programme for DR [53]. An American study assessing the patient-perceived value of teleophthalmology in an urban, low-income population with diabetes also found 87% of patients were open to a teleophthalmology exam if it were recommended by their primary care physician [54]. Another major potential benefit of increased implementation of telehealth is improved social and emotional well-being for rural patients. This is likely due to a reduction in need for patients to travel and subsequent sense of alienation they may experience due to their isolation from family and local community [55].
The arrival of the 5G network may create the potential for the concurrent use of AI (e.g. automated OCT) with teleophthalmology. Similarly, the concurrent use of teleophthalmology with remote operated stereo slit lamps may be a possibility. Nankavil et al. have demonstrated remote operation of a slit lamp while acquiring high-resolution live video to and from America, Canada and the Netherlands [56]. A review of telehealth interventions found that image-based triage was twice as effective in reducing the need for appointments when compared with non-image-based [57]. This could have a profound impact on the efficiency of workflow for ophthalmologists and considerably reduce the cost of attending hospital or office-based appointments. The use of teleophthalmology may also reduce the number of missed appointments, reducing the resource wastage of the already-strained public healthcare system. Teleophthalmology could additionally be beneficial for metropolitan patients with physical disabilities, the elderly and those with busy schedules.
The Covid-19 pandemic has had a considerable impact on ophthalmic practice and altered the landscape in which eyecare is delivered worldwide. Due to government-imposed social distancing restrictions, concerns regarding patient and staff safety, there has been a surge in the use of telehealth platforms to deliver healthcare [58].
Restrictions have extended to the point of complete lockdowns in countries, such as China, Italy, France, UK and India [59]. A survey of 1260 ophthalmologists in India reported that 77.5% were using telemedicine in some capacity to deliver eyecare [60]. The majority of specialists used phone consultations, whilst ~10% employed video calls. A survey of American neuro-ophthalmologists noted a 64.4% increase in telehealth video consults [61]. This survey identified ease of access, continuity and efficiency of care as benefits and specifically highlighted the challenges in the detection and management of conditions requiring funduscopic examination as a barrier. In the UK, oculoplastics subspecialists reported video consultation software was most notably helpful for follow-up and post-operative patients [62]. They reported video quality was sufficient for history-taking, external ocular examination and could be supplemented by patients providing close-up pictures as necessary. In addition, 62% of patients included in the study preferred virtual consults over face-to-face due to better safety and convenience. Teleophthalmology has also demonstrated great promise in paediatric and strabismus patients during the Covid-19 period [63].
Covid-19 has also created many challenges surrounding medical education, with many students being withdrawn from placements as a direct result of the pandemic. An additional benefit of the increased implementation of telemedicine technologies in ophthalmology is medical student education. The highly visual nature of ophthalmology lends well to the delivery of virtual didactic lectures, online cases and “attending” virtual consultations with patients [64].
The Covid-19 pandemic appears to have further accelerated the integration of telemedicine into ophthalmology. While the data is limited, teleophthalmology is proving to a viable alternative to face-to-face consultations. In the future, there is a strong possibility video consultations will become the norm and increasing bandwidth will be required to support this shift towards virtual practice. Though in building WiFi and fixed connections may be sufficient for use by clinicians in hospitals, true teleophthalmology will require a widespread wireless cellular network. If 5G delivers as promised and barriers, such as the inability to carry out funduscopic examinations can be overcome, teleophthalmology will likely become a key aspect of practice in the post-pandemic future.
A systematic review of barriers to the worldwide adoption of telemedicine found cost, concerns regarding reimbursement, issues surrounding confidentiality, legal liability and security of data were the most frequent barriers reported by organisations [65]. This study also reported age, level of education, computer literacy and bandwidth were some of the more frequent barriers reported by patients. In relation to the minimum bandwidth required to successfully carry out telehealth consultations, speeds as low as 318–512 kbps have been reported to be sufficient [66, 67]. Whilst the vast majority of nations’ average internet speeds far exceed the minimum speed requirements, the issue appears to stem from an inability to maintain consistent bandwidth over an extended period of time. In alignment with this, a UK-based Whole System Demonstrator Action Network briefing paper reported connectivity problems were severely restrictive for the provision of seamless care using telehealth [68]. These findings are also consistent with a telehealth study of 287 participants which revealed only 73.5% of patients were satisfied with their internet connectivity for videoconferencing for the 1-year duration of the trial [69]. Only eight patients were unable to participate in the trial due to not being able to connect to the internet and two withdrew due to issues with repeatedly disconnecting. Similarly, another paper from the UK stressed the importance of reliable bandwidth in order to minimise loss of sound and/or picture and ensure a high quality of healthcare is provided to patients [70]. The new 5G network carries with it the potential to address this issue of bandwidth reliability and overcome a major barrier to the provision of teleophthalmology to the global population, particularly those in rural or remote regions.
The integration of telemedicine using 5G into eyecare is very promising, however much like in the case of VR, ensuring transmissions are heavily encrypted and secure from cyber attacks is an additional major barrier for the provision of improved eyecare to patients.
Telesurgery
The development of remote surgery technology in the future holds the potential to not only revolutionise patient care of those in rural and remote areas, but also improves access to specialist teaching for trainees and general ophthalmologists [71]. Currently, data on the incorporation of real-time telementoring in ophthalmology is limited. An early example of its use involved the transmission of a live feed of an endoscopic dacryocystorhinostomy with interactive questions and answers format from a hospital in Hawaii to the Philippines [72]. Similarly, the use of real-time telementoring was demonstrated to be beneficial in the removal of an orbital tumour, where an orbital specialist mentored a general ophthalmologist over 200 miles away through the procedure without incidence [73]. The potential benefit of real-time telementoring has been demonstrated in Orthopaedic Surgery and General Surgery. A pilot study from Canada, used real-time telementoring by an orthopaedic surgeon to guide four physicians through leg fasciotomies on cadavers. The study concluded surgical telementoring may enable physicians to safely perform two-incision leg fasciotomy in remote environments [74]. Another study from California reported telementoring for guidance of surgical trainees through sleeve gastrectomy procedures was a highly rated learning tool by both mentors and mentees [75]. Recently a case report of two patients successfully undergoing laparoscopic high-anterior and low-anterior resections, respectively, using telementoring has demonstrated the potential of the 5G network [76]. In both cases a connection speed of at least 98 Mbs was achieved and both procedures reported a score greater than 9.5/10 for image quality. In addition, verbal communication during both procedures was rated 10/10. A German study reported the 5G network achieved the minimum requirements for data volume, rate and latency needed for video transmission during telesurgery [77]. These studies highlight the potential that exists for the incorporation of telementoring into ophthalmology for the training of future specialists and guidance of generalists through procedures requiring specialist input.
The dawn of the new 5G network has made the concept of telesurgery for patients requiring surgery a realistic possibility in the next 10 years. The concept of telesurgery refers to the use of a high-powered internet network and robotics in order to conduct surgical procedures where the patient and surgeon are not within the same hospital [78]. The major limitation to the development of telesurgery thus far has been the limitation in network speeds. The insufficient network speeds result in increased and inconsistent latency times, this results in a considerable delay in time between a surgeon’s movement and the robotic arm’s replication of the action. One experiment qualitatively reported an average latency of 10.4 ms was suitable to carry out the endonasal telesurgery with a distance of 800 km between the robot and the surgeon [79]. Another study evaluating the effect of latency on surgical performance reported that surgical time, motion and errors were directly proportional to latency [80]. These studies highlight the need for a reliable and high-speed network in order for telesurgery to become a realistic option for patient management. There is evidence that a latency of ≤200 ms optimises telesurgery in terms of difficulty, security, precision and fluidity of manipulation [80]. This latency can be achieved with current networks, but requires over 40 technicians to be present, a dedicated network and high-speed fibre optic cables [78]. Additional benefits of robot-assisted surgery include elimination of tremors, unprecedented levels of manoeuvrability and visualisation [81]. The use of the Da Vinci Xi Surgical System has demonstrated feasibility in penetrating keratoplasty. One study evaluated 12 procedures with robot assistance and reported an average procedure duration of 43.9 min with no intraoperative adverse events [82]. Remote surgery holds the potential to considerably reduce the impact of geography, population and specialist distribution on the ability to deliver quality eyecare to patients. If the new 5G network delivers on ultrafast speed and reliable connectivity, telesurgery could revolutionise patient care. Telesurgery also presents an opportunity for patients to make previously unseen choices in regard to selecting their surgeons. Furthermore, telementoring could be combined with telesurgery to offer an additional educational method for the education of trainees or foreign doctors unable to be trained conventionally by specialists.
The concepts of remote surgery and telementoring are hopeful solutions to address many of the major barriers to the delivery of eyecare to patients. Prior to the widespread implementation of these technologies, there are considerable ethical dilemmas and liability concerns that require consideration. The practice of having sub-specialised ophthalmologists guiding general specialists through complicated procedures digitally creates an issue of whether ophthalmologists would be doing more harm than good. During these procedures, a very realistic possibility exists that the general ophthalmologist may have difficulty interpreting a mentor’s instructions or make an error, thereby a complication may occur which they are not trained to manage. Furthermore, in case of complications or poor patient outcomes who would legally be responsible in this situation would need to be clearly defined. Similarly, while remote surgery could potentially revolutionise eyecare, if a loss of signal was to occur and any subsequent complications ensued, clearly defining who would be liable out of the hospital, surgeon or internet provider will be essential.
Conclusion
The dawn of the 5G network presents the opportunity for the development and implementation of technologies that hold the potential to address many of the current barriers for the delivery of specialist eyecare to the global population. These technologies are particularly suited to ophthalmic practice. The technologies developed may play a key role in addressing current challenges, including waiting times, costs associated with care, cultural appropriateness, geographic population and specialist distribution. If the 5G network delivers as promised, technologies including VR, AI, teleophthalmology and telesurgery may be key assistive components in the delivery of improved healthcare to the global population.
Author contributions
WC and RC conceptualised the review topic. GS conducted the search for literature, extracted relevant points of discussion, analysed currently reported statistics, updated reference lists and contributed to writing of the report. WC and RC were also involved with drafting and contributed to writing of the review. WC, RC and GS, all approved of the review being submitted for publication.
Compliance with ethical standards
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Strover S. Reaching rural America with broadband internet service. Prakville (VIC): The Conversation; 2018. https://theconversation.com/reaching-rural-america-with-broadband-internet-service-82488.
- 2.Roser M, Ritchie H, Ortiz-Ospina E. Internet. Oxford (UK): Our World in Data; 2020. https://ourworldindata.org/internet#citation.
- 3.Choros A. ADSL2+ internet: everything you need to know. Crows Nest (NSW): WhistleOut; 2016. https://www.whistleout.com.au/Broadband/Guides/adsl2-plus-everything-you-need-to-know.
- 4.Ofcom. Broadband basics. London (UK): Ofcom; n.d.. https://www.ofcom.org.uk/__data/assets/pdf_file/0019/16354/bb-guide-combined.pdf.
- 5.Akamai. Akamai’s state of the internet] Q1 2017 report. Cambridge (Massachusetts, USA): Akamai; 2017. https://www.akamai.com/us/en/multimedia/documents/state-of-the-internet/q1-2017-state-of-the-internet-connectivity-report.pdf.
- 6.Stats IW. World Internet Users and 2020 Population Stats. Bogota (Colombia): Miniwatts Marketing Group; 2020. https://www.internetworldstats.com/stats.htm.
- 7.AgeUK. The internet and older people in the UK—key statistics. London (UK): Age UK; 2016. https://www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/active-communities/rb_july16_older_people_and_internet_use_stats.pdf.
- 8.Anderson M, Perrin A. Technology use among seniors. Washington DC (USA): Pew Research Center; 2017. https://www.pewresearch.org/internet/2017/05/17/technology-use-among-seniors/.
- 9.Zajac IT, Flight IHK, Wilson C, Turnbull D, Cole S, Young G. Internet usage and openness to internet-delivered health information among Australian adults aged over 50 years. Australas Med J. 2012;5:262–7. doi: 10.4066/AMJ.2012.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Opensignal. The state of LTE(February 2018). London (UK): Opensignal; 2018. https://www.opensignal.com/reports/2018/02/state-of-lte.
- 11.Okasaka S, Weiler RJ, Keusgen W, Pudeyev A, Maltsev A, Karls I, et al. Proof-of-Concept of a millimeter-wave integrated heterogeneous network for 5G cellular. Sens (Basel) 2016;16:1362. doi: 10.3390/s16091362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Authority ACaM. 5G and mobile network developements—emerging issues. Melbourne (VIC): Australian Communications and Media Authority; 2016. https://www.acma.gov.au/theACMA/5g-and-mobile-network-developments.
- 13.Vodafone. 5G: how fast is 5G? Newbury(UK): Vodafone UK; 2020.
- 14.Lifewire. Internet speed requirements for video streaming. New York City (New York, USA): Dotdash; 2019. https://www.lifewire.com/internet-speed-requirements-for-movie-viewing-1847401.
- 15.Harada H, Kanaji S, Hasegawa H, Yamamoto M, Matsuda Y, Yamashita K, et al. The effect on surgical skills of expert surgeons using 3D/HD and 2D/4K resolution monitors in laparoscopic phantom tasks. Surg Endosc. 2018;32:4228–34. doi: 10.1007/s00464-018-6169-1. [DOI] [PubMed] [Google Scholar]
- 16.D’Alessandris QG, Rigante M, Mattogno PP, La Rocca G, Romanello M, Auricchio AM, et al. Impact of 4K ultra-high definition endoscope in pituitary surgery: analysis of a comparative institutional case series. J Neurosurg Sci. 2020. [DOI] [PubMed]
- 17.National Academies of Sciences Engineering, and Medicine; Policy and Global Affairs; Government-University-Industry Research Roundtable; Saunders J. The transformational impact of 5G. In: Proceedings of a workshop—in brief. Washington DC (USA): National Academies Press (US); 2019 https://www.ncbi.nlm.nih.gov/books/NBK547761/. [PubMed]
- 18.Wallace C. Bringing 5G networks indoors. Stockholm (SWE): Ericsson; 2019. https://www.ericsson.com/en/reports-and-papers/white-papers/bringing-5g-networks-indoors.
- 19.Marek S. Marek’s Take: making 5G work indoors is a huge task for operators. New York (USA): Fierce Wireless; 2019. https://www.fiercewireless.com/wireless/marek-s-take-making-5g-work-indoors-a-huge-task-for-operators.
- 20.Organization WH. Blindness and vision impairment. Geneva (CHE); 2019. https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment.
- 21.Bank TW. Urban population (% of total population). Washington DC (USA): World Bank Group; 2018. https://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS.
- 22.Dillinger J. Rural population by country. Saint-Laurent (CAN): Reunion Tech Inc; 2017. https://www.worldatlas.com/articles/working-on-the-land-the-world-s-major-rural-populations.html.
- 23.Statistics ABo. Geographic distribution of the population. Canberra (AUS): Australian Bureau of Statistics; 2012. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/1301.0~2012~Main%20Features~Geographic%20distribution%20of%20the%20population~49.
- 24.Affairs DfEFR. Rural population 2014/15. London (UK): Department for Environment Food & Rural affairs; 2020. https://www.gov.uk/government/organisations/department-for-environment-food-rural-affairs.
- 25.Bureau USC. One in five Americans live in rural areas. Maryland (USA): United States Census Bureau; 2017. https://www.census.gov/library/stories/2017/08/rural-america.html.
- 26.Welfare AIoHa. Eye health workforce in Australia. Canberra (AUS): Welfare AIoHa; 2016. https://www.aihw.gov.au/getmedia/82b0922e-0744-459b-9b9e-5c019bdf6b3f/19296.pdf.aspx?inline=true.
- 27.Palmer JJ, Chinanayi F, Gilbert A, Pillay D, Fox S, Jaggernath J, et al. Mapping human resources for eye health in 21 countries of sub-Saharan Africa: current progress towards VISION 2020. Hum Resour Health. 2014;12:44. doi: 10.1186/1478-4491-12-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pandrangi VC, Gaston B, Appelbaum NP, Albuquerque FC, Jr., Levy MM, Larson RA. The application of virtual reality in patient education. Ann Vasc Surg. 2019;59:184–9. [DOI] [PubMed]
- 29.Thompson-Butel AG, Shiner CT, McGhee J, Bailey BJ, Bou-Haidar P, McCorriston M, et al. The role of personalized virtual reality in education for patients post stroke-a qualitative case series. J Stroke Cerebrovasc Dis. 2019;28:450–7. doi: 10.1016/j.jstrokecerebrovasdis.2018.10.018. [DOI] [PubMed] [Google Scholar]
- 30.Mangiante S, Klas G, Navon A, Zhuang G, Ran J, Dias Silva M. VR is on the edge: how to deliver 360° videos in mobile networks. Newbury (UK): Vodafone R&D; 2017. https://www.researchgate.net/publication/319049968_VR_is_on_the_Edge_How_to_Deliver_360_Videos_in_Mobile_Networks.
- 31.Khalifa YM, Bogorad D, Gibson V, Peifer J, Nussbaum J. Virtual reality in ophthalmology training. Surv Ophthalmol. 2006;51:259–73. doi: 10.1016/j.survophthal.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 32.Spiteri AV, Aggarwal R, Kersey TL, Sira M, Benjamin L, Darzi AW, et al. Development of a virtual reality training curriculum for phacoemulsification surgery. Eye. 2014;28:78–84. doi: 10.1038/eye.2013.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kozak I, Banerjee P, Luo J, Luciano C. Virtual reality simulator for vitreoretinal surgery using integrated OCT data. Clin Ophthalmol. 2014;8:669–72. doi: 10.2147/OPTH.S58614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thomsen AS, Smith P, Subhi Y, Cour M, Tang L, Saleh GM, et al. High correlation between performance on a virtual-reality simulator and real-life cataract surgery. Acta Ophthalmologica. 2017;95:307–11. doi: 10.1111/aos.13275. [DOI] [PubMed] [Google Scholar]
- 35.Deuchler S, Wagner C, Singh P, Müller M, Al-Dwairi R, Benjilali R, et al. Clinical efficacy of simulated vitreoretinal surgery to prepare surgeons for the upcoming intervention in the operating room. PLoS One. 2016;11:e0150690–e. doi: 10.1371/journal.pone.0150690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alcon. Digitally assisted vitreoretinal surgery: a new perspective. Texas (USA): Novartis; 2018. https://alconscience.com/wp-content/uploads/2018/10/DIGITALLY-ASSISTED-SURGERY-WHITE-PAPER.pdf.
- 37.Freeman WR, Chen KC, Ho J, Chao DL, Ferreyra HA, Tripathi AB, et al. Resolution, depth of field, and physician satisfaction during digitally assisted vitreoretinal surgery. Retina. 2018;39:1768–71. doi: 10.1097/IAE.0000000000002236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kita M, Mori Y, Hama S. Hybrid wide-angle viewing-endoscopic vitrectomy using a 3D visualization system. Clin Ophthalmol. 2018;12:313–7. doi: 10.2147/OPTH.S156497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Charles. C, Bugajksi M, Luthra A, McCarthy S, Moroney P, Wirick K. Virtual and augmented reality—how do they affect the current service delivery and home and network architectures? Adelaide (SA): ARRIS; 2016. https://www.commscope.com/globalassets/digizuite/1733-exec-paper-virtual-and-augmented-reality-final.pdf?utm_source=arris&utm_medium=redirect.
- 40.Khor WS, Baker B, Amin K, Chan A, Patel K, Wong J. Augmented and virtual reality in surgery-the digital surgical environment: applications, limitations and legal pitfalls. Ann Transl Med. 2016;4:454. doi: 10.21037/atm.2016.12.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parham G, Bing EG, Cuevas A, Fisher B, Skinner J, Mwanahamuntu M, et al. Creating a low-cost virtual reality surgical simulation to increase surgical oncology capacity and capability. Ecancermedicalscience. 2019;13:910. doi: 10.3332/ecancer.2019.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Panch T, Szolovits P, Atun R. Artificial intelligence, machine learning and health systems. J Glob Health. 2018;8:020303. doi: 10.7189/jogh.08.020303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hwang D-K, Hsu C-C, Chang K-J, Chao D, Sun C-H, Jheng Y-C, et al. Artificial intelligence-based decision-making for age-related macular degeneration. Theranostics. 2019;9:232–45. doi: 10.7150/thno.28447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Treder M, Lauermann JL, Eter N. Automated detection of exudative age-related macular degeneration in spectral domain optical coherence tomography using deep learning. Graefe’s Arch Clin Exp Ophthalmol. 2018;256:259–65. doi: 10.1007/s00417-017-3850-3. [DOI] [PubMed] [Google Scholar]
- 45.Gargeya R, Leng T. Automated identification of diabetic retinopathy using deep learning. Ophthalmology. 2017;124:962–9. doi: 10.1016/j.ophtha.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 46.Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. Jama. 2016;316:2402–10. doi: 10.1001/jama.2016.17216. [DOI] [PubMed] [Google Scholar]
- 47.Wu Y, Schuster M, Zhifeng Chen, Quoc V. Le, Mohammad Norouzi, Wolfgang Macherey, et al. Google’s neural machine translation system: bridging the gap between human and machine translation. Ithaca, NY (USA): Cornell University; 2016. https://arxiv.org/abs/1609.08144.
- 48.Research B. Baidu research announces breakthrough in simultaneous translation. California (USA): Baidu Research; 2018.
- 49.Bartnik SE, Copeland SP, Aicken AJ, Turner AW. Optometry-facilitated teleophthalmology: an audit of the first year in Western Australia. Clin Exp Optom. 2018;101:700–3. doi: 10.1111/cxo.12658. [DOI] [PubMed] [Google Scholar]
- 50.Kawaguchi A, Sharafeldin N, Sundaram A, Campbell S, Tennant M, Rudnisky C, et al. Tele-ophthalmology for age-related macular degeneration and diabetic retinopathy screening: a systematic review and meta-analysis. Telemed J E Health. 2018;24:301–8. doi: 10.1089/tmj.2017.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ribeiro AG, Rodrigues RA, Guerreiro AM, Regatieri CV. A teleophthalmology system for the diagnosis of ocular urgency in remote areas of Brazil. Arq Bras Oftalmol. 2014;77:214–8. doi: 10.5935/0004-2749.20140055. [DOI] [PubMed] [Google Scholar]
- 52.Host BK, Turner AW, Muir J. Real-time teleophthalmology video consultation: an analysis of patient satisfaction in rural Western Australia. Clin Exp Optom. 2018;101:129–34. doi: 10.1111/cxo.12535. [DOI] [PubMed] [Google Scholar]
- 53.Valpuesta Martin Y, Pacheco Callirgos GE, Maroto Martin TM, Piriz Veloso M, Hernandez Santamaria S, Lopez Galvez MI. Satisfaction of patients and primary care professionals with a teleophthalmology-based screening programme for diabetic retinopathy in a rural area in Castilla y Leon, Spain. Rural Remote Health. 2020;20:5180. doi: 10.22605/RRH5180. [DOI] [PubMed] [Google Scholar]
- 54.Ramchandran RS, Yilmaz S, Greaux E, Dozier A. Patient perceived value of teleophthalmology in an urban, low income US population with diabetes. PLoS One. 2020;15:e0225300–e. doi: 10.1371/journal.pone.0225300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Caffery LJ, Bradford NK, Wickramasinghe SI, Hayman N, Smith AC. Outcomes of using telehealth for the provision of healthcare to Aboriginal and Torres Strait Islander people: a systematic review. Aust NZ J Public Health. 2017;41:48–53. doi: 10.1111/1753-6405.12600. [DOI] [PubMed] [Google Scholar]
- 56.Nankivil D, Gonzalez A, Rowaan C, Lee W, Aguilar MC, Parel J-MA. Robotic remote controlled stereo slit lamp. Transl Vis Sci Technol. 2018;7:1. doi: 10.1167/tvst.7.4.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J Telemed telecare. 2016;22:504–12. doi: 10.1177/1357633X16670495. [DOI] [PubMed] [Google Scholar]
- 58.Saleem SM, Pasquale LR, Sidoti PA, Tsai JC. Virtual ophthalmology: telemedicine in a COVID-19 Era. Am J Ophthalmol. 2020;216:237–42. doi: 10.1016/j.ajo.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Koh D. COVID-19 lockdowns throughout the world. Occup Med. 2020. 10.1093/occmed/kqaa073.
- 60.Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: results of a survey. Indian J Ophthalmol. 2020;68:725–30. doi: 10.4103/ijo.IJO_797_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moss HE, Lai KE, Ko MW. Survey of telehealth adoption by neuro-ophthalmologists during the COVID-19 pandemic: benefits, barriers, and utility. J Neuroophthalmol. 2020;40:346–55. doi: 10.1097/WNO.0000000000001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kang S, Thomas PBM, Sim DA, Parker RT, Daniel C, Uddin JM. Oculoplastic video-based telemedicine consultations: Covid-19 and beyond. Eye. 2020;34:1193–5. doi: 10.1038/s41433-020-0953-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Deshmukh AV, Badakere A, Sheth J, Bhate M, Kulkarni S, Kekunnaya R. Pivoting to teleconsultation for paediatric ophthalmology and strabismus: our experience during COVID-19 times. Indian J Ophthalmol. 2020;68:1387–91. doi: 10.4103/ijo.IJO_1675_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wendt S, Abdullah Z, Barrett S, Daruwalla C, Go JA, Le B, et al. A virtual COVID-19 ophthalmology rotation. Surv Ophthalmol. 2020. [DOI] [PMC free article] [PubMed]
- 65.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24:4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schulz TR, Richards M, Gasko H, Lohrey J, Hibbert ME, Biggs BA. Telehealth: experience of the first 120 consultations delivered from a new refugee telehealth clinic. Intern Med J. 2014;44:981–5. doi: 10.1111/imj.12537. [DOI] [PubMed] [Google Scholar]
- 67.Smith AC. Telemedicine: challenges and opportunities. Expert Rev Med Devices. 2007;4:5–7. doi: 10.1586/17434440.4.1.5. [DOI] [PubMed] [Google Scholar]
- 68.Giordano R, Clark M, Goodwin N. Perspectives on telehealth and telecare. London (UK): The King’s Fund; 2011. https://www.kingsfund.org.uk/sites/default/files/Perspectives-telehealth-telecare-wsdan-paper.pdf.
- 69.Celler B, Varnfield M, Sparks R, Li J, Nepal S, Jang-Jaccard J, et al. Home monitoring of chronic disease for aged care. Canberra (ACT): CSIRO; 2016.
- 70.Williams OE, Elghenzai S, Subbe C, Wyatt JC, Williams J. The use of telemedicine to enhance secondary care: some lessons from the front line. Future Health J. 2017;4:109–14. doi: 10.7861/futurehosp.4-2-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hung AJ, Chen J, Shah A, Gill IS. Telementoring and Telesurgery for Minimally Invasive Procedures. J Urol. 2018;199:355–69. doi: 10.1016/j.juro.2017.06.082. [DOI] [PubMed] [Google Scholar]
- 72.Camara JG, Rodriguez RE. Real-time telementoring in ophthalmology. Telemed J. 1998;4:375–7. doi: 10.1089/tmj.1.1998.4.375. [DOI] [PubMed] [Google Scholar]
- 73.Camara JG, Zabala RR, Henson RD, Senft SH. Teleophthalmology: the use of real-time telementoring to remove an orbital tumor. Ophthalmology. 2000;107:1468–71. doi: 10.1016/s0161-6420(00)00211-6. [DOI] [PubMed] [Google Scholar]
- 74.Talbot M, Harvey EJ, Berry GK, Reindl R, Tien H, Stinner DJ, et al. A pilot study of surgical telementoring for leg fasciotomy. J R Army Med Corps. 2018;164:83–6. doi: 10.1136/jramc-2017-000817. [DOI] [PubMed] [Google Scholar]
- 75.Nguyen NT, Okrainec A, Anvari M, Smith B, Meireles O, Gee D, et al. Sleeve gastrectomy telementoring: a SAGES multi-institutional quality improvement initiative. Surg Endosc. 2018;32:682–7. doi: 10.1007/s00464-017-5721-8. [DOI] [PubMed] [Google Scholar]
- 76.Lacy AM, Bravo R, Otero-Pineiro AM, Pena R, De Lacy FB, Menchaca R, et al. 5G-assisted telementored surgery. Br J Surg. 2019;106:1576–9. doi: 10.1002/bjs.11364. [DOI] [PubMed] [Google Scholar]
- 77.Jell A, Vogel T, Ostler D, Marahrens N, Wilhelm D, Samm N, et al. 5th-generation mobile communication: data highway for surgery 4.0. Surg Technol Int. 2019;35:36–42. [PubMed] [Google Scholar]
- 78.Choi PJ, Oskouian RJ, Tubbs RS. Telesurgery: past, present, and future. Cureus. 2018;10:e2716–e. doi: 10.7759/cureus.2716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wirz R, Torres LG, Swaney PJ, Gilbert H, Alterovitz R, Webster RJ, 3rd, et al. An experimental feasibility study on robotic endonasal telesurgery. Neurosurgery. 2015;76:479–84. doi: 10.1227/NEU.0000000000000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xu S, Perez M, Yang K, Perrenot C, Felblinger J, Hubert J. Determination of the latency effects on surgical performance and the acceptable latency levels in telesurgery using the dV-Trainer((R)) simulator. Surg Endosc. 2014;28:2569–76. doi: 10.1007/s00464-014-3504-z. [DOI] [PubMed] [Google Scholar]
- 81.Nuzzi R, Brusasco L. State of the art of robotic surgery related to vision: brain and eye applications of newly available devices. Eye Brain. 2018;10:13–24. doi: 10.2147/EB.S148644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chammas J, Sauer A, Pizzuto J, Pouthier F, Gaucher D, Marescaux J, et al. Da Vinci Xi robot-assisted penetrating keratoplasty. Transl Vis Sci Technol. 2017;6:21. doi: 10.1167/tvst.6.3.21. [DOI] [PMC free article] [PubMed] [Google Scholar]