Abstract
Hysterectomy for large uterine anterior cervical myoma is a challenging surgical procedure. We summarize our experience in the management of large uterine anterior cervical myoma. Three patients underwent hysterectomy for uterine anterior cervical myoma with similar sizes and different positions treated by laparoscopic surgery. Total laparoscopic hysterectomy (TLH) for cervical myoma is possible by performing ureterolysis and adopting retrograde hysterectomy. Because the position of myoma is important to determine the difficulty of TLH, we propose to measure the axis between the most caudal point of the myoma and external cervical os and pubococcygeal line as a possible useful method in objectively predicting the difficulty of TLH for large anterior cervical myoma.
Keywords: Laparoscopic hysterectomy, magnetic resonance imaging, uterine cervical leiomyoma
INTRODUCTION
Myoma of the uterine cervix is rare, accounting for approximately 5% of all myomas.[1] Hysterectomy for large uterine anterior cervical myoma is a challenging surgical procedure whether performed with laparotomy or laparoscopy and surgeons should be prepared to modify the surgical technique based on the position of the myoma. Performing laparoscopic surgery for the treatment of cervical myoma is difficult because of poor access to the operative field, increased blood loss, and distortion of the anatomy in the vital neighboring structures in the pelvic cavity.[2] Total laparoscopic hysterectomy (TLH) seems to be more difficult to perform for myoma of the anterior than the posterior cervix. This may be caused by the following reasons: (1) securing a visual field for surgery and separating the bladder from the uterus are difficult when the cervical myoma bulges out to the anterior and caudal side and (2) the complete incision of the parametrium is difficult because it tends to widen and deviate to the posterior part.
In this manuscript, we present our experience with three cases of uterine anterior cervical myoma treated by laparoscopic surgery. We summarize the surgical strategy and propose a presurgical assessment of the surgery's difficulty. This study was approved by the Yokohama Municipal Citizen's Hospital Institutional Review Board (reference no. 19-01-06). Written informed consent was obtained from all the participants included in the study.
CASE REPORT
Case 1
A 48-year-old Japanese woman, gravida 6, para 3 (3 vaginal deliveries and 3 miscarriages) presented with heavy menstrual bleeding. Cytology of the uterine cervix and endometrium were negative for intraepithelial lesion of malignancy (NILM) and negative, respectively. Magnetic resonance imaging (MRI) revealed a 14-cm leiomyoma in the anterior wall of the uterine cervix and no other prominent tumor was found. Gonadotropin-releasing hormone analog (GnRHa) was omitted because we expected TLH was possible without administering it. The surgical procedure was performed as follows: (1) a total of four ports were inserted in a diamond pattern. The round ligaments, mesosalpinx, and utero-ovarian ligaments were sectioned. Both ovaries were preserved, (2) after identifying the uterine artery and ureter, the former was ligated twice. Then, the ureters were isolated from the posterior leaf of the broad ligament to the ureteral tunnel, (3) the vesicouterine peritoneum was opened, and the bladder was pushed down from the uterine anterior wall as much as possible, 4) the parametrium was coagulated and incised including the ascending branch of the uterine artery. The flattened parametrium caused by the cervical myoma resulted in a widened and deviated to the posterior part of the myoma, thus making the procedure more challenging, (5) a malleable retractor was inserted into the anterior fornix of the vagina, and the anterior part was incised followed by the circumferential dissection of the vagina, (6) completion of colpotomy was performed in a retrograde fashion by incising the uterosacral ligaments and posterior leaf of the broad ligaments, (7) The uterus was transvaginally removed in small pieces, and (8) the vaginal vault was sutured laparoscopically.
The procedure lasted for 121 min, with intraoperative blood loss of 200 ml. The weight of the removed uterus was 888 g, and the pathological examination was consistent with a benign leiomyoma. The postoperative course was uneventful, and the patient was discharged on a postoperative day 3 without complications.
Case 2
A 55-year-old Japanese woman, gravida 2, para 2 (1 vaginal delivery and 1 cesarean section) presented with heavy menstrual bleeding and pollakisuria. Cytology of the uterine cervix was NILM and of the endometrium was negative. MRI revealed a 15.9-cm leiomyoma in the anterior wall of the uterine cervix with no other prominent tumors found. GnRHa was administrated five times preoperatively. The size of the myoma became slightly smaller, that is, 13.4 cm before the surgery. The surgical procedure was essentially the same as in case 1. However, due to the further caudally positioned cervical myoma than that in case 1, the incision of the parametrium was difficult at one side and resulted in a relatively large amount of bleeding.
The procedure lasted for 209 min, with intraoperative blood loss of 400 ml. She received 400 ml of autologous blood. The weight of the removed uterus was 1130 g, and the pathological examination was consistent with a benign leiomyoma. The patient was discharged on a postoperative day 3 without complications.
Case 3
A 50-year-old Japanese woman, gravida 2, para 2 (2 vaginal deliveries) presented with abdominal distension and abnormal genital bleeding. Cytology of the uterine cervix was NILM and of the endometrium was not fulfilled. MRI revealed a 13.7-cm leiomyoma in the anterior wall of the uterine cervix and another 3-cm leiomyoma in the anterior uterine corpus. GnRHa was administrated four times and found to be noneffective. The surgical procedure has essentially started as in case 2. However, the view of the surgical field could not be achieved safely, and the complete incision of both parametrium was not possible considering the bulging cervical myoma expanded more to the anterior and caudal sides than that in case 2. Therefore, open surgery and subsequent uterus removal were done.
The operation lasted for 197 min and the intraoperative blood loss was 1280 ml. She received 400 ml of autologous blood. The weight of the removed uterus was 1182 g, and the pathological result was degenerative leiomyoma. The postoperative course was uneventful, and the patient was discharged on a postoperative day 5 without complications.
DISCUSSION
Recent advances in equipment, surgical techniques, and training have made TLH a well-tolerated and efficient technique. Furthermore, as more surgeons become trained in advanced laparoscopic surgery, the role of TLH has significantly taken the place of total abdominal hysterectomy.[3] In fact, recent studies have reported that TLH can be performed safely regardless of the uterine size.[4] Therefore, we opted for TLH as the first choice for hysterectomy even for large anterior cervical myoma. However, studies reporting TLH for cervical myoma are limited due to its difficulty.
Based on our experiences, the key points to a successful laparoscopic surgery in the case of large uterine anterior cervical myoma are performing ureterolysis and adopting retrograde hysterectomy.
Ureterolysis was adopted to avoid ureteral injury. We usually mobilize the ureters from the posterior leaf of the broad ligament up to the entrance of the ureteral tunnel and then coagulate and transect the parametrium, including the ascending branch of the uterine artery.
Retrograde hysterectomy is useful for TLH in patients with frozen pelvis and an unclear cervical region.[5,6] We did it to identify the uterosacral ligaments and posterior leaf of the broad ligaments that were dorsally deviated and excised them after the dissection of the vaginal wall. In case of cervical myoma, the portio vaginalis is often flattened by the myoma, making it difficult to recognize. The vaginal wall around the fornix also tends to extend along the myoma; therefore, the cutting line of the vaginal wall should be identified correctly. For this reason, a malleable retractor was inserted to the anterior fornix of the vagina, which helps finding a cutting line of the anterior part of the vagina more feasible.
We encountered three cases of uterine anterior cervical myoma with similar tumor sizes and weights of the removed uteri (14 cm, 888 g; 13.4 cm, 1,130 g; and 13.7 cm, 1,182 g, respectively). The challenge of performing TLH depends on the patient's characteristics, such as body mass index, previous surgeries, and complications, as well as the size, position, and characteristics of the myoma. Experiences in these cases suggest that the position of the myoma is a crucial determinant factor in assessing the difficulty of anterior cervical myoma surgery; the degree increases as the tumor is further caudally positioned and may lead to incomplete incision of the parametrium. Therefore, we speculate that MRI may be useful to predict the difficulty of surgery. For this purpose, we tried to use the pubococcygeal line (PC line), the line between the bottom edge of the pubic bone and the second coccygeal bone obtained in the sagittal images of T2-weighted imaging sequence.[7] To use the PC line as a reference axis, the axis was made based on the line between the most caudal point of the myoma and external cervical os and PC line [Figure 1]. In these three cases, the patient 1 showed that the two lines were almost parallel, whereas the axis made by the two lines was approximately 10° in case 2 and 20° in case 3. This result indicates that the larger the angle between the two lines, the more caudal is the myoma, which increases the difficulty of surgery. Therefore, measuring the axis between these two lines may be useful to objectively predict the difficulty of TLH for anterior cervical myoma.
Figure 1.
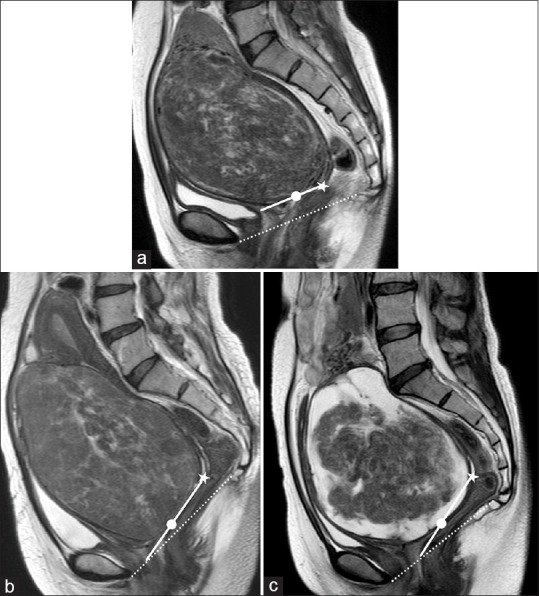
Sagittal T2-weighted images of the three cases taken using plain pelvic magnetic resonance imaging. •: Most caudad point of the myoma, ★: External cervical OS. Dotted line: Pubococcygeal line. (a) Magnetic resonance imaging of case 1 shows that the two lines are almost parallel. (b) Magnetic resonance imaging of case 2 shows that the axis made by the two lines shows approximately 10°. (c) Magnetic resonance imaging of case 3 shows that the axis made by the two lines shows approximately 20°
The limitations of this case series are that this is a retrospective study and the proposed possibility is brought on through the experience of only three cases. Therefore, its applicability is not all-inclusive. Further evidence is required before a definitive conclusion can be derived about the relationship between the difficulty of TLH for large anterior cervical myoma and measuring the axis between the lines described on MRI. For experienced surgeons, the combination between sonography and manual pelvic examination may be enough to predict the difficulty of surgery. However, MRI is the most accurate imaging technique for detection, localization, and characterization of myomas, and preoperative MRI may be a powerful tool to predict the difficulty of TLH.[8,9] In addition, MRI seems to be a good tool to share the information objectively with other doctors and inherits the strategy for TLH to young doctors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Matsuoka S, Kikuchi I, Kitade M, Kumakiri J, Kuroda K, Tokita S, et al. Strategy for laparoscopic cervical myomectomy. J Minim Invasive Gynecol. 2010;17:301–5. doi: 10.1016/j.jmig.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 2.Patel P, Banker M, Munshi S, Bhalla A. Handling cervical myomas. J Gynecol Endosc Surg. 2011;2:30–2. doi: 10.4103/0974-1216.85277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elkington NM, Chou D. A review of total laparoscopic hysterectomy: Role, techniques and complications. Curr Opin Obstet Gynecol. 2006;18:380–4. doi: 10.1097/01.gco.0000233930.21307.5a. [DOI] [PubMed] [Google Scholar]
- 4.Uccella S, Cromi A, Bogani G, Casarin J, Formenti G, Ghezzi F. Systemic implementation of laparoscopic hysterectomy independent of uterine size: Clinical effect. J Minim Invasive Gynecol. 2013;20:505–6. doi: 10.1016/j.jmig.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Paul PG, Shabnam K, Bhosale SA, Kaur H, Talwar P, Thomas T. Laparoscopic hysterectomy in frozen pelvis-an alternative technique of retrograde adhesiolysis. Gynecol Surg. 2013;10:285–90. [Google Scholar]
- 6.Nakayama K, Tsukao M, Ishikawa M, Ishibashi T, Nakamura K, Sanuki K, et al. Total laparoscopic hysterectomy for large uterine cervical myoma. Mol Clin Oncol. 2017;6:655–60. doi: 10.3892/mco.2017.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fielding JR. Practical MR imaging of female pelvic floor weakness. Radiographics. 2002;22:295–304. doi: 10.1148/radiographics.22.2.g02mr25295. [DOI] [PubMed] [Google Scholar]
- 8.Bazot M, Salem C, Frey I, Daraï E. Imaging of myomas: Is preoperative MRI usefull.? Gynecol Obstet Fertil. 2002;30:711–6. doi: 10.1016/s1297-9589(02)00428-9. [DOI] [PubMed] [Google Scholar]
- 9.Saito A, Hirata T, Koga K, Takamura M, Fukuda S, Neriishi K, et al. Preoperative assessment of factors associated with difficulty in performing total laparoscopic hysterectomy. J Obstet Gynaecol Res. 2017;43:320–9. doi: 10.1111/jog.13198. [DOI] [PubMed] [Google Scholar]


