Here is an article that offers evidence-based information regarding different protocols used for fluoroscopically guided lumbar punctures. The data were obtained via Web-based anonymous questionnaires sent to neuroradiologists. From 577 responses the following information can be gleaned: most neuroradiologists place the patient prone, use a 22-gauge needle, and access the L2-3 or L3-4 spaces. The techniques for measuring pressure vary widely and only a minority of neuroradiologists rotate their patients for this purpose. The authors recommend developing a uniform protocol for opening pressure measurement.
Abstract
BACKGROUND AND PURPOSE:
Evidenced-based protocols for fluoroscopically guided LP do not exist. This study analyzed the fluoroscopically guided LP techniques currently used by practicing neuroradiologists.
MATERIALS AND METHODS:
An anonymous Web-based survey was e-mailed to members of ASNR. The results were compiled and tabulated on a spreadsheet.
RESULTS:
A total of 577 neuroradiologists completed the survey. Most neuroradiologists perform fluoroscopically guided LPs with the patient in the prone position by using a 22-ga needle at the L2-L3 or L3-L4 intervertebral space. The OP measurement technique is quite variable. Only a minority of patients are rotated to the left LD position for OP measurement. Most neuroradiologists observe patients for 1–2 hours after the procedure and require strict bed rest.
CONCLUSIONS:
Most neuroradiologists have similar protocols for thecal sac puncture. Normative adult OP data exist only for the LD position, and the accuracy of prone OP measurements is not known. We found that the OP measurement technique is not consistent and a standard protocol is warranted.
While LPs are historically performed at the bedside, fluoroscopically guided LPs have become a routine procedure for neuroradiologists. In 2008, the American College of Radiology and the ASNR published “Practice Guidelines for the Performance of Myelography and Cisternography,”1 which included a description of the lumbar approach for accessing the subarachnoid space but did not outline a comprehensive LP protocol with OP measurement. To our knowledge, there are no published guidelines describing fluoroscopically guided LP. The accuracy of OP measurement is crucial to diagnosing those with intracranial hypertension or hypotension. This study aimed to identify practice patterns among neuroradiologists regarding the fluoroscopically guided LP technique and OP measurement.
Materials and Methods
Members of the ASNR were invited to complete an anonymous 16-question multiple-choice Web-based survey. Survey results were tabulated by Survey Monkey (http://try.surveymonkey.com/?gclid=CKyK1PnXuasCFQhN4AodRktRgQ) and analyzed by using Excel (Microsoft, Redmond, Washington). The University of Minnesota institutional review board approved the exemption status for this study.
Results
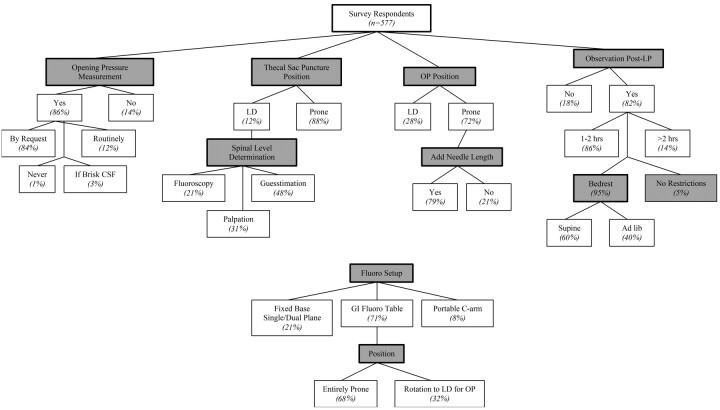
A total of 577 members of the ASNR completed the survey. Not all respondents answered every survey question. Ninety-five percent of survey respondents had >5 years of experience performing fluoroscopically guided LPs, with most (54%) performing fewer than 25 LPs annually (Table). Eighty-four percent of surveyed neuroradiologists measure OP, while 14% do not. Of those who measure OP, most (83%) measure it only when requested by the referring physician, 14% measure OP routinely, and 3% measure OP only when abnormally brisk CSF flow is noted on removal of the stylet from the spinal needle (Fig 1). Three respondents (0.6%) reported never measuring OP (Fig 1).
Experience level of surveyed neuroradiologists
| Survey Respondent Characteristics | No. Respondents |
|---|---|
| LP experience (yr) | |
| 0–5 | 29 (5%) |
| 5–10 | 106 (18%) |
| 10–15 | 85 (15%) |
| 15–20 | 112 (19%) |
| >20 | 244 (42%) |
| LPs per year | |
| 0–25 | 313 (54%) |
| 26–50 | 120 (21%) |
| 51–75 | 52 (9%) |
| 76–100 | 37 (6%) |
| >100 | 54 (9%) |
Fig 1.
Practice patterns for fluoroscopically guided LP and OP measurement.
The overwhelming majority of fluoroscopically guided LPs are performed by using a 22- (68%) or 20- (24%) ga needle. The preferred spinal entry level varies, but the L2-L3 (42%) and L3-L4 (30%) levels are the most common. Eighty-eight percent of respondents perform the thecal sac puncture prone, while 12% puncture the sac with the patient in the LD position (Fig 1).
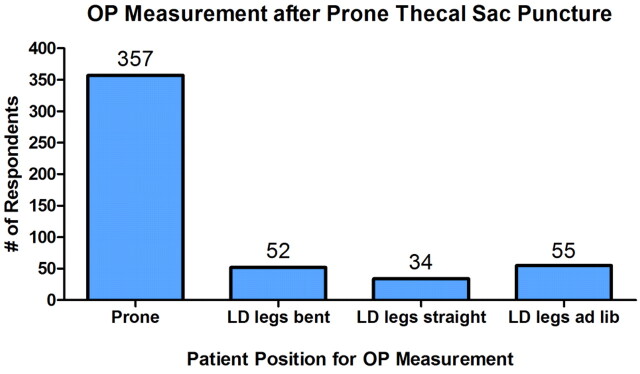
Of the 497 neuroradiologists who typically perform thecal sac puncture with the patient in the prone position, 356 (72%) measure OP in the prone position, while 141 (28%) rotate the patient to measure OP in the LD position (Fig 1). When measuring OP in the LD position, 73 (21%) use fluoroscopy to determine the level of the spinal canal (and thus the 0-cm mark on the manometer), 105 (31%) palpate the spinous processes, and 164 (48%) use “guesstimation” (Fig 1). When OP is measured with the patient in the LD position following prone thecal sac puncture, leg position varies among bent (37%), straight (24%), and ad lib (39%) (Fig 2). Of the survey respondents who typically measure OP with the patient in the prone position, 280 (79%) add the needle length to the OP measurement (the tip of the needle in the thecal sac therefore serves as the 0-cm mark), while 72 (21%) do not. When assessing the equilibration point between the CSF pressure and the manometer in any position, 365 (64%) measure when the meniscus stops rising and 205 (36%) measure the OP when systolic-diastolic fluctuation/respiratory fluctuation begins.
Fig 2.
Patient position following prone LP.
Most survey respondents (71%) perform fluoroscopically guided LP on a GI fluoroscopy table. Alternatively, 21% use fixed-base single/dual plane fluoroscopy, and 8% use a portable C-arm. Of the 400 neuroradiologists who routinely use the GI fluoroscopy table, 68% perform the entire procedure with the patient prone, while 32% perform prone thecal sac puncture followed by a transfer to the LD position for OP measurement (Fig 1). Radiation protection of the radiologist during the procedure was not investigated.
Following fluoroscopically guided LP, most neuroradiologists (82%) regularly observe their patients for some time; 86% of whom observe their patients for 1–2 hours postprocedure (Fig 1). When patients are observed postprocedure, 95% of survey respondents restrict activity to bed rest, 57% further restrict body position to supine, and 38% allow ad lib positioning during bed rest (Fig 1). Five percent observe without any position or activity restrictions (Fig 1). In the event that an epidural blood patch is needed to treat post-LP headache, most surveyed neuroradiologists (61%) do not perform their own blood patches, while 39% do perform this procedure themselves.
Discussion
Despite the absence of practice guidelines for fluoroscopically guided LP, neuroradiologists generally appear to perform these in a similar fashion. Most perform thecal sac puncture and OP measurement on a GI fluoroscopy table with the patient prone throughout the entire procedure. A 22-ga needle is typically used to puncture at L2-L3 or L3-L4. Almost two- thirds (64%) record the OP when the CSF meniscus stops rising as opposed to the traditional, and likely more accurate, teaching of OP measurement when systolic-diastolic or respiratory fluctuation begins.2 This may result in falsely high or low opening pressure measurements.
Most (80%) neuroradiologists who typically perform OP measurement with the patient prone add the needle length to the manometer reading to determine the final CSF OP. The OP is based on the CSF height within the manometer, where zero is the level of the left atrium of the heart. In the LD position, zero level corresponds to the position of the spinal canal and is determined clinically with various techniques. In the prone position, however, needle length must be added to the meniscus height or the recorded pressure will be falsely low. According to the survey data, 1 in 5 neuroradiologists does not add the needle length when measuring OP in the prone position. Underestimation of CSF pressure by omitting needle length from the final OP measurement may have clinical implications. For example, IIH is a diagnosis of exclusion that depends on an accurate OP measurement to prevent potentially irreversible vision loss. Conceivably, the respondents who do not add needle length to the manometer reading after prone OP measurement could be using flexible extension tubing, which theoretically allows prone OP measurement with zero at the level of the left atrium. This survey did not specifically address the use of flexible tubing, so prevalence of this technique remains unclear.
Most interesting, normative OP data exist only for the LD position, not for prone measurements. Clinical decisions based on these pressures deserve careful consideration, especially when the OP is borderline. We are currently studying the relationship of prone-versus-LD OP.
The lower extremity position likely affects the OP measurement. While some studies have demonstrated that the lower extremity position does not affect CSF pressure, others have shown a significant difference between OP in the flexed- and extended-leg positions.3–6 In this survey, extended lower extremity position was not consistently maintained during OP measurement in the LD position. The clinical significance of this difference is debated, but lower extremity position could affect clinical decision-making in borderline cases. While this is more applicable to LPs performed at the bedside and only applies to the small percentage (28%) of OPs measured in the LD position during fluoroscopically guided LP, it illustrates a deficiency in practice guidelines that may affect opening pressures.
As obesity increases in the US population, it is likely that the incidence of IIH will also rise. The diagnosis of IIH depends on an accurate OP of ≥25-cm water measured in the LD position. In the absence of practice guidelines for OP measurement, patients may receive a false-positive IIH diagnosis or go undiagnosed if the neuroradiologist fails to add the needle length to prone OP measurements.
Conclusions
We recognize that the limitations of this study include accurate self-report by the survey respondents as well as a common understanding of the questions asked. Despite these limitations, it appears that neuroradiologists generally perform fluoroscopically guided LPs in a similar fashion. Practice guidelines for standardizing the fluoroscopically guided LP technique would improve the accuracy of OP measurement. Therefore, we propose the following suggestions regarding OP measurements for fluoroscopically guided LP:
1) Ideally, OP is measured in the left LD position because normative data exist for this position only. At the time of OP measurement, the neck and lower extremities should be completely extended.
2) If OP is measured in the prone position, the needle length must be added to the meniscus height. If flexible extension tubing is used, it should be positioned with zero at the level of the spinal canal. Procedure notes should reflect the manner of OP measurement.
3) Meniscus height should be assessed when systolic-diastolic fluctuation/respiratory fluctuation begins.
4) Patients should be coached to relax because use of the Valsalva maneuver to maintain body position can falsely elevate OP.7 This is especially important in patients with excessive abdominal or thoracic girth who may struggle to maintain position.
5) Normative data for prone OP measurements are needed because most fluoroscopically guided LPs are performed with patients entirely in the prone position.
ABBREVIATIONS:
- ASNR
American Society of Neuroradiology
- GI
gastrointestinal
- IIH
idiopathic intracranial hypertension
- LD
lateral decubitus
- LP
lumbar puncture
- OP
opening pressure
Footnotes
Disclosures: Andrew Harrison—UNRELATED: Consultancy: Merz Pharmaceuticals.
This work was supported by an unrestricted grant from Research to Prevent Blindness (New York, New York) and the Lions Club of Minnesota (M.S.L., A.R.H.).
References
- 1. ACR-ASNR Practice Guidelines for the Performance of Myelography and Cisternography. 2008. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/guidelines/dx/head-neck/Myelography.pdf. Accessed May 1, 2011. [Google Scholar]
- 2. Euerle BD. Spinal puncture and cerebrospinal fluid examination. In: Roberts JR, Hedges JR. eds. Clinical Procedures in Emergency Medicine. 5th ed. Philadelphia: Saunders/Elsevier; 2010:1107–27 [Google Scholar]
- 3. Abbrescia KL, Brabson TA, Dalsey WC, et al. , for the Lumbar Puncture Study Group The effect of lower-extremity position on cerebrospinal fluid pressures. Acad Emerg Med 2001;8:8–12 [DOI] [PubMed] [Google Scholar]
- 4. Avery RA, Mistry RD, Shah SS, et al. Patient position during lumbar puncture has no meaningful effect on cerebrospinal opening pressure in children. Child Neurol 2010;25:616–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ellis R. Lumbar cerebrospinal fluid opening pressure measured in a flexed lateral decubitus position in children. Pediatrics 1994;93:622–23 [PubMed] [Google Scholar]
- 6. Sithinamsuwan P, Sithinamsuwan N, Tejavanija S, et al. The effect of whole body position on lumbar cerebrospinal fluid opening pressure. Cerebrospinal Fluid Res 2008;5:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Neville L, Egan RA. Frequency and amplitude of elevation of cerebrospinal fluid resting pressure by the Valsalva maneuver. Can J Ophthalmol 2005;40:775–77 [DOI] [PubMed] [Google Scholar]