Abstract
Background
Inguinal hernia repair is the most common general surgery operation in the United States. Nearly 80% of inguinal hernia operations are performed under general anesthesia versus 15%–20% using local anesthesia, despite the absence of evidence for superiority of the former. Although patients aged 65 years and older are expected to benefit from avoiding general anesthesia, this presumed benefit has not been adequately studied. We hypothesized that the benefits of local over general anesthesia for inguinal hernia repair would increase with age.
Materials and Methods
We analyzed 87,794 patients in the American College of Surgeons National Surgical Quality Improvement Project who had elective inguinal hernia repair under local or general anesthesia from 2014–2018, and we used propensity scores to adjust for known confounding. We compared postoperative complications, 30-day readmissions, and operative time for patients aged <55 years, 55–64 years, 65–74 years, and ≥75 years.
Results
Using local rather than general anesthesia was associated with a 0.6% reduction in postoperative complications in patients aged 75+ years (95% CI −0.11 to −1.13) but not in younger patients. Local anesthesia was associated with faster operative time (2.5 minutes – 4.7 minutes) in patients <75 years but not in patients aged 75+ years. Readmissions did not differ by anesthesia modality in any age group. Projected national cost savings for greater use of local anesthesia ranged from $9 million to $45 million annually.
Conclusions
Surgeons should strongly consider using local anesthesia for inguinal hernia repair in older patients and in younger patients because it is associated with significantly reduced complications and substantial cost savings.
Keywords: Older adult, General anesthesia, Local anesthesia, Hernia repair
INTRODUCTION
Inguinal hernia repair is the most common general surgery operation in the United States and provides a unique opportunity for surgeons and anesthesiologists to improve outcomes for older adults.1 Inguinal hernias lead to 4 million clinic visits and 800,000 operations annually, and individuals ≥65 years old are 40%-90% more likely to develop hernias than younger adults.1–4
Nearly 80% of inguinal hernia operations are performed under general anesthesia versus 15%-20% under local anesthesia, despite the absence of evidence for improved perioperative outcomes with the former.5,6 Several small randomized trials and observational studies suggested that local anesthesia for hernia repair reduces morbidity by up to 30%, unplanned admissions by 20%, and operative time and costs by 15%, while other studies showed no significant differences.5,7–9 These studies focused on younger patients (<65 years old) with limited comorbidities, largely ignoring elderly patients. However, patients aged 65 years and older are more likely to benefit from avoiding exposure to general anesthesia, which may increase risk of cognitive dysfunction and metabolic derangements.10 Consequently, the American College of Surgeons and the American Geriatrics Society recommendations for the care of older adults urged surgeons to conduct research to determine which operations are associated with improved outcomes when general anesthesia is avoided in older adults.11 However, despite the frequency of inguinal hernia repair, no nationally representative studies have evaluated postoperative outcomes following exposure to general or local anesthesia for older adults having inguinal hernia surgery. Additionally, no studies have assessed whether the potential benefits of local anesthesia vary as a function of age.
The purpose of this study was to compare the effects of local and general anesthesia on postoperative recovery for adults aged 65 years and older. We also sought to determine whether potential benefits of local anesthesia differed according to patient age. We hypothesized that using local anesthesia for inguinal hernia repair would significantly reduce complications and that the benefit would be more pronounced in adults aged 65 years and above.
MATERIAL AND METHODS
Setting and patient selection
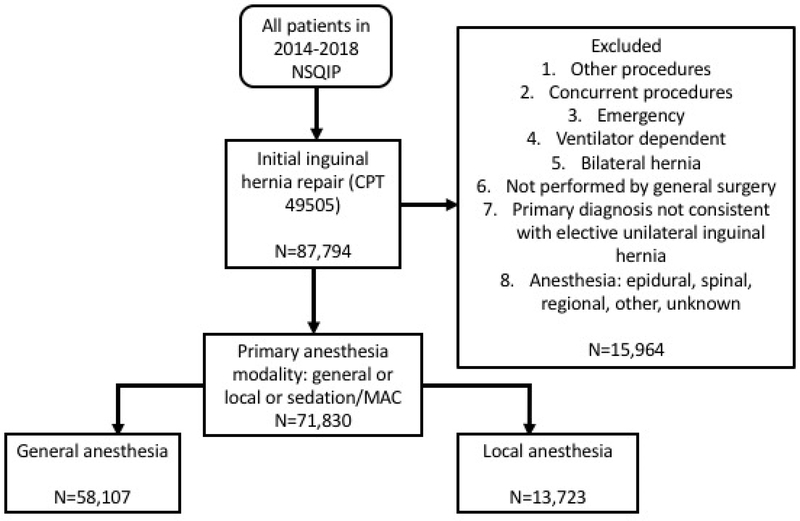
We identified 87,794 patients in the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database from 2014–2018 who had elective, unilateral, open inguinal hernia repair based on Common Procedure Terminology code 49505 (Figure 1). We excluded patients who had concurrent procedures or other procedures not consistent with hernia repair, bilateral hernias, primary diagnosis other than unilateral inguinal hernia, preoperative ventilator dependence, or if the primary surgeon specialty was not general surgery in order to minimize confounding between the groups. We also excluded patients if anesthesia was coded as epidural, spinal, regional, other, or unknown. In order to determine the difference between anesthesia modality based on patient age, we categorized patients into those less than 55 years, 55–64 years, 65–74 years, and those aged 75 years and older.
Figure 1.
Patients having open inguinal hernia repair under local and general anesthesia were selected from the 2014–2018 American College of Surgeons National Surgical Quality Improvement Program database.
Primary outcome
The primary outcome was occurrence of any postoperative NSQIP complication within 30 days of surgery. Complications which factored into this outcome variable included wound infection, dehiscence, pneumonia, re-intubation, pulmonary embolus, failure to wean from the ventilator, renal insufficiency/failure, urinary tract infection, stroke, cardiac arrest, myocardial infarction, postoperative bleeding that requires transfusion, deep vein thrombosis, sepsis/septic shock, reoperation, and readmission.
Secondary outcomes
Secondary outcomes included: (1) total operative time (patient entry to exit from the operating room), (2) 30-day readmissions, and (3) potential cost savings.
Independent variable
The primary variable/exposure of interest was use of local or general anesthesia.
Propensity scores
To adjust for known confounding, we generated a propensity score using factors shown in Table 1. The propensity score was developed using an iterative process where different functional forms of the variables in Table 1 were entered into a binary logistic regression with the dependent variable of local or general anesthesia. Predicted probability from the model was then log transformed, and we verified that a sufficient number of cases and controls were contained within the common support region of the estimated propensity score prior to conducting any analysis.12
Table 1.
Patient characteristics (unadjusted and using the propensity score for inverse probability weighting and matching).
| Variable | General Anesthesia | Local Anesthesia | P value | Standardized Difference (Unadjusted) | Standardized Difference After Inverse Probability Weighting | Standardized Difference after Propensity Matching |
|---|---|---|---|---|---|---|
| Total = 58,107 N (%) | Total = 13,723 N (%) | |||||
| Age, Median (IQR) | 60 (23) | 66 (21) | <0.001 | 37.4 | 1.3 | 2.2 |
| *Age (years) | <0.001 | |||||
| <55 | 22,432 (38.6) | 3,469 (25.3) | ||||
| 55–64 | 13,715 (23.6) | 3,013 (22.0) | 3.9 | 0.2 | 0.4 | |
| 65–74 | 12,816 (22.1) | 3,617 (26.4) | 10.1 | 0.22 | 0.06 | |
| 75+ | 9,144 (15.7) | 3,624 (26.4) | 26.4 | 0.08 | 0.02 | |
| *Male gender | 53,012 (91.2) | 12,304 (89.7) | <0.001 | 5.4 | 0.1 | 7.2 |
| *Race/Ethnicity | <0.001 | |||||
| Non-Hispanic Caucasian | 37,776 (65.0) | 10,341 (75.4) | ||||
| Hispanic | 3,801 (6.5) | 543 (4.0) | 8.7 | 0.02 | 5.3 | |
| African American | 5,753 (9.9) | 762 (5.6) | 16.2 | 0.4 | 1.3 | |
| Other | 1,763 (3.0) | 448 (3.3) | 1.3 | 0.2 | 4.1 | |
| Unknown | 9,014 (15.5) | 1,629 (11.9) | 10.6 | 0.3 | 1.3 | |
| *Year of Surgery | <0.001 | |||||
| 2014 | 9,844 (16.9) | 2,680 (19.5) | ||||
| 2015 | 11,129 (19.2) | 2,868 (20.9) | 4.2 | 0.04 | 1.4 | |
| 2016 | 12,429 (21.4) | 3,050 (22.2) | 3.9 | 0.3 | 0.8 | |
| 2017 | 12,148 (20.9) | 2,718 (19.8) | 2.7 | 0.4 | 1.2 | |
| 2018 | 12,557 (21.6) | 2,407 (17.5) | 14.7 | 0.7 | 1.1 | |
| Preoperative Functional Status | <0.001 | |||||
| Independent | 57,359 (98.7) | 13,358 (97.3) | ||||
| Partially or Totally Dependent | 317 (0.6) | 115 (26.6) | 1.8 | 0.3 | 0.8 | |
| American Society of Anesthesiology Score | <0.001 | |||||
| 1 | 9,943 (17.1) | 2,027 (14.8) | ||||
| 2 | 31,477 (54.2) | 6,977 (50.8) | 7.7 | 0.2 | 0.8 | |
| 3–5 | 16,645 (28.7) | 4,612 (33.6) | 5.4 | 0.2 | 0.4 | |
| Predicted Morbidity Quintiles | <0.001 | |||||
| 1 | 11,928 (20.5) | 2,436 (17.8) | ||||
| 2 | 11,692 (20.1) | 2,672 (19.5) | 0.4 | 0.2 | 1.7 | |
| 3 | 11,778 (20.3) | 2,585 (18.8) | 10.8 | 02 | 1.2 | |
| 4 | 11,562 (19.9) | 2,802 (20.4) | 10.2 | 0.01 | 2.9 | |
| 5 | 11,135 (19.2) | 3,228 (23.5) | 3.5 | 0.09 | 0.4 | |
| Number of comorbidities | 0.1 | |||||
| 0 | 25,932 (44.6) | 6,095 (44.4) | ||||
| 1 | 21,906 (37.7) | 5,105 (37.2) | 10.5 | 0.1 | 1.5 | |
| 2+ | 10,269 (17.7) | 2,523 (18.4) | 8.3 | 0.2 | 3.0 |
Indicates that the variable was included in the propensity analysis.
We used three methods (propensity matching, inverse probability weighting, and regression adjustment) to incorporate the propensity score into our analysis.13 Similar results from all three methods yield increased confidence that systematic differences between treated and control groups have been effectively balanced.13
First, we used nearest neighbor matching with replacement within calipers of 0.25 × the estimated propensity score. We also tested caliper distances of 0.2, 0.15, and 0.10, which yielded essentially identical results to the 0.25 caliper, so only data from the 0.25 caliper scheme are presented. Second, we used inverse probability weighting where patients receiving general anesthesia were weighted according to the formula 1/(1-[log transformed propensity score]) and patients who received local anesthesia were weighted according to the formula 1/(log transformed propensity score). Finally, we employed regression adjustment where the outcome of interest was regressed on a binary indicator for local versus general anesthesia and the estimated propensity score. For each of these methods, we used the propensity score to calculate the average treatment effect, which represents the mean difference in the outcome between patients who had hernia surgery under local versus general anesthesia. To assess adequate balance of confounders on the propensity matching and weighting, we calculated the standardized difference and variance for populations before and after propensity scores until the standardized difference was <10% and the variance was close to 1.14 Differences were expressed in terms of average treatment effect.
Estimating costs
To estimate potential cost savings with increased use of local anesthesia among NSQIP-participating hospitals, we calculated the product of: (1) percent change in operations performed under local anesthesia, (2) number of patients in each age group, (3) average change in operative time, and (4) average cost of 1 minute of operating room time.15 To estimate national savings, we assumed that the 800,000 operations performed annually in the US contained a similar proportion of patients in each age group as our study. We then calculated a product using the same equation as described above. We also calculated the potential reduction in postoperative complications with increased use of local anesthesia.
Statistical analysis
All analyses were performed with Stata version 15.1. We used the Stata commands teffects psmatch, teffects ipw, and teffects ra for propensity matching, inverse probability weighting, and regression adjustment, respectively. Differences were considered significant at α<0.05. As findings from each of the three propensity score methods were used to confirm results from the other methods, we did not employ a correction for multiple comparisons.
RESULTS
Patient characteristics
From 2014–2018, open inguinal hernia repair was performed in 13,723 patients using local anesthesia and in 58,107 patients using general anesthesia (Table 1). As shown in Table 1, patients who had inguinal hernia surgery under local anesthesia were significantly older than those who received general anesthesia (median age 66 years versus 60 years). Patients who were partially or totally dependent in activities of daily living, those with a higher American Society of Anesthesiology score, and those with higher predicted morbidity were also more likely to have hernia repair using local anesthesia. Hispanics and African Americans were 10% less likely to undergo surgery with local compared to non-Hispanic whites. Additionally, the overall use of local anesthesia for inguinal hernia repair declined over time, from 21% in 2014 to 18% in 2018.
Local anesthesia was associated with fewer postoperative complications in patients aged 75 years and older
The unadjusted complication rate for all patients having inguinal hernia repair under general anesthesia was 1.2% compared to 1.1% for local anesthesia (p=0.2).
Table 2 shows that the complication rate increased with age and that using local anesthesia was associated with a 0.1%-0.3% decrease in complications for the three youngest age groups, though this difference was not significant. For the oldest patients (75+ years), there was a reduction in complications from 2.1% with general anesthesia to 1.6% with local anesthesia (p=0.04). For information on specific complications see Supplemental Table 1.
Table 2.
In the unadjusted cohort, local anesthesia was associated with fewer postoperative complications in patients ≥75 years and shorter operative time in younger patients. Readmissions rates were not affected by using local anesthesia.
| Age <55 | Age 55–64 | Age 65–74 | Age 75+ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General N (%) | Local N (%) | P | General N (%) | Local N (%) | p | General N (%) | Local N (%) | P | General N (%) | Local N (%) | p | |
| Any complication | 194 (0.9) | 24 (0.7) | 0.3 | 127 (0.9) | 24 (0.8) | 0.5 | 187 (15) | 42 (12) | 0.2 | 193 (2.1) | 57 (16) | 0.04 |
| Readmission | 169 (0.8) | 21 (0.6) | 0.3 | 132 (1.0) | 31 (1.0) | 0.7 | 199 (1.6) | 54 (1.5) | 0.8 | 290 (3.2) | 114 (3.2) | 0.9 |
| Operative time in minutes | 60 (35) | 50 (28) | 0.001 | 53 (34) | 50 (27) | 0.001 | 51 (33) | 51 (29) | 0.02 | 50 (30) | 50 (28) | 0.08 |
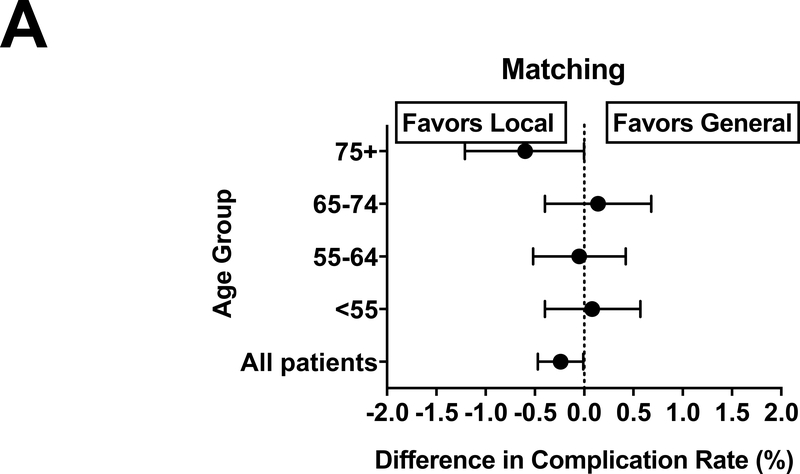
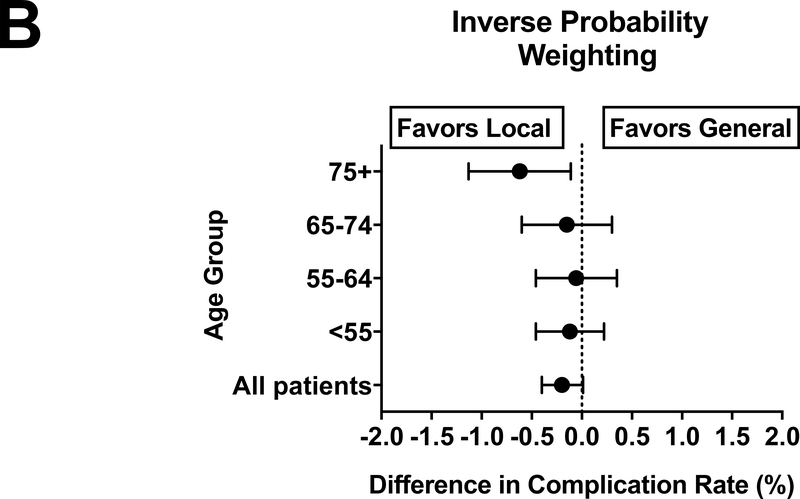
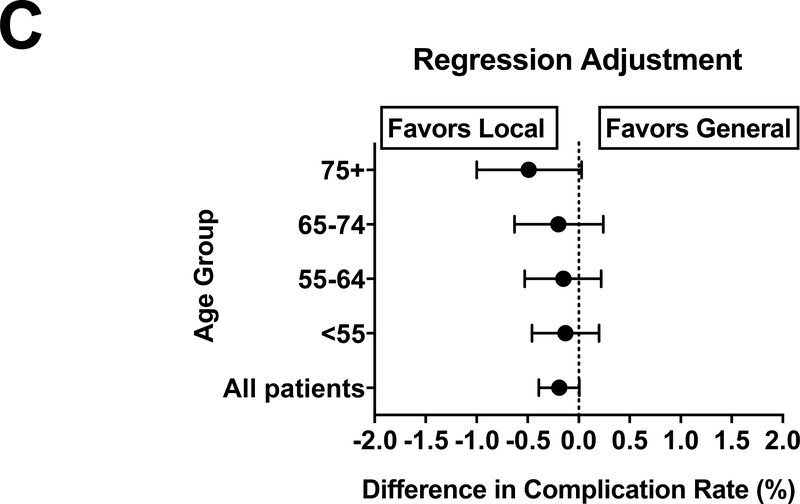
After propensity score adjustment, using local rather than general anesthesia was associated with fewer postoperative complications. After propensity matching, there was a 0.24% lower complication rate (95% CI -0.008% to -0.05%, p<0.05) for all patients having hernia surgery under local (Figure 2A). Inverse probability weighting (Figure 2B) showed a 0.20% reduction (0.012% to -0.40%, p=0.06)and regression adjustment (Figure 2C) demonstrated a 0.30% decrease (-0.04% to 0.005%, p=0.06) in postoperative complications, however these were not significant.
Figure 2.
Patients aged 75 years and older experience fewer postoperative complications when their hernias are repaired using local anesthesia. The decrease in complications is similar when estimated using propensity matching (A), inverse probability weighting (B) and regression adjustment, although this was not significant (C).
When patients were analyzed by age, the only age group that showed a significant difference in complication rates were patients ≥75 years older. Propensity matching (Figure 2A) demonstrated that local anesthesia was associated with 0.6% fewer (95% CI -0.0003% to -1.20%, p<0.005) postoperative complications, inverse probability weighting (Figure 2B) showed a 0.6% reduction (95% CI -0.1% to -1.14%, p<0.05), and regression adjustment (Figure 2C) showed no difference in complications (-0.5% 95% CI -1.0% to 0.03%, p=0.06) in patients ≥75 years old. For other age groups, there were no significant differences in postoperative complications. However, Figure 2 demonstrates that the overall complication rate remained lower for local compared to general anesthesia for all age groups.
Local anesthesia was associated with shorter operative time for patients <75 years old
Prior to propensity adjustment, inguinal hernia repair under local anesthesia was associated with a 2-minute decrease in total operative time (p<0.001). Table 2 shows that the benefits of decreased operative time were largely confined to younger age groups and that there were no significant differences in operative time for patients aged 75 and older. These results were confirmed by our propensity score analysis.
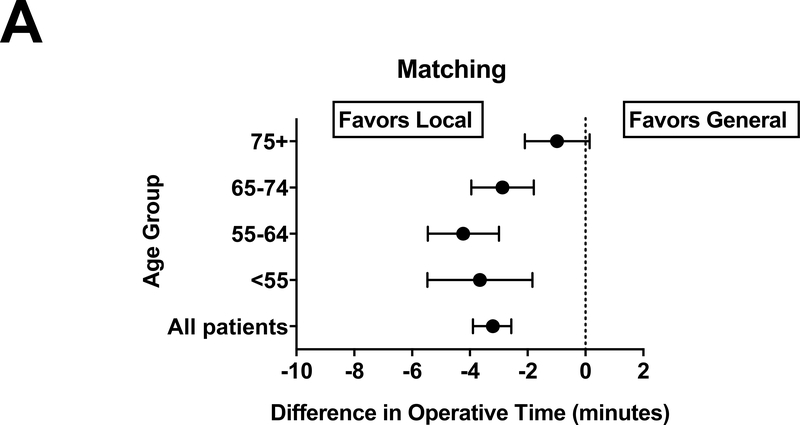
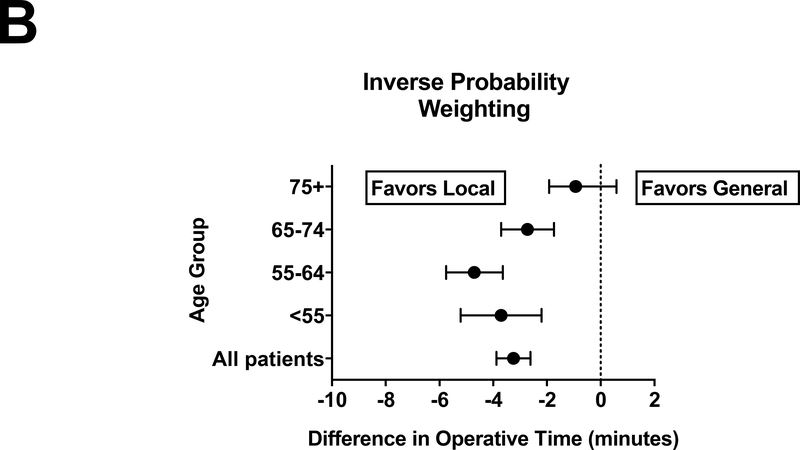
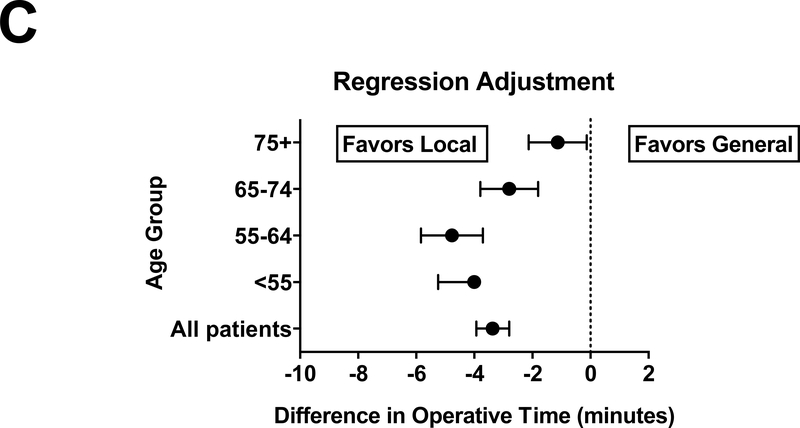
Propensity matching (Figure 3A) showed that the average decrease in operative time for all patients was 3.2 minutes (95% CI −3.9 to −2.6 minutes, p<0.001), inverse probability weighting (Figure 3B) also showed a decrease of 3.2 minutes (95% CI −3.9 to −2.6 minutes, p<0.001), and regression adjustment (Figure 3C) showed a 3.4-minute decrease (95% CI −3.9 to −2.8, p<0.001). As shown in Figure 3, patients ≤64 years derived the most benefit from having their operations performed under local anesthesia (~4 minutes faster). Patients in the 65–74 age group also benefited from faster operative times with local anesthesia (2.5- to 2.9-minute decrease). There were no significant differences in operative time for the oldest age group (75+ years).
Figure 3.
Total operative time was decreased for all patients except those 75 years and older when inguinal hernias are repaired under local anesthesia. The reduction in operative time was similar when estimated using propensity matching (A), inverse probability weighting (B) and regression adjustment (C).
We also analyzed specific complications between local and general anesthesia, as shown in Table 2. We found that there were very few differences between the anesthesia types, however there was a 0.5% reduction in the occurrence of postoperative urinary tract infection among patients ≥75 years (p=0.001).
Local anesthesia did not affect readmission rates in any age group
The unadjusted rate of readmissions was low for both anesthesia groups, and actually suggested that local anesthesia may be associated with increased readmission rates (1.6% vs 1.4%, p=0.03). Readmission rates were lowest in the youngest patients (<1% for those <55 years old) but increased steadily with age. Patients aged 75 years and older experienced the highest readmission rates but there was no difference between the anesthesia groups (3.2 vs 3.2, p=0.9). Although the unadjusted rate of readmission was significantly higher in the local anesthesia group, after adjustment with propensity scores, there were no significant differences in readmission rates between local and general anesthesia. There were no differences in readmission rates between local and general anesthesia at different age groups.
Increasing use of local could significantly reduce costs and complications
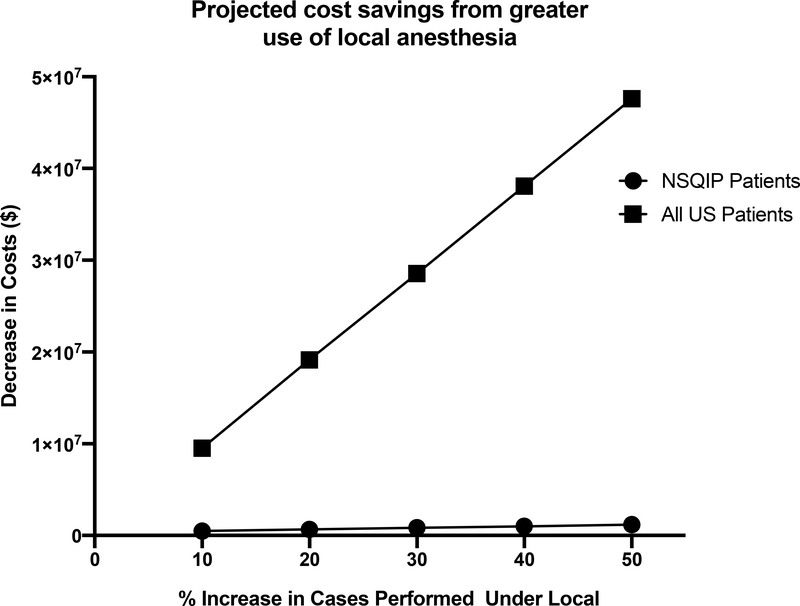
Based on our estimates of faster operative time in nearly all patients, we estimated the impact that greater use of local anesthesia could have on US healthcare spending. Using a published cost of $36 per minute of operating room time, Figure 4 shows that a 10% increase in the use of local anesthesia for hernia repair would save NSQIP hospitals $495,754 annually and a 50% increase would save nearly $1.2 million annually.15 Similarly, the entire US healthcare system could save over $9 million annually if 10% more hernia operations were performed under local anesthesia, and over $47 million if there were a 50% increase. With respect to postoperative complications, a 10% increase in the use of local anesthesia among patients 75 years and older nationally would lead to 124 fewer patients experiencing complications and a 50% increase would lead to 624 fewer complications each year.
Figure 4.
Increasing the utilization of local anesthesia for inguinal hernia repair will lead to significant cost savings for hospitals participating in the National Surgical Quality Improvement Program (NSQIP) and for all hospitals performing inguinal hernia surgery (All US Patients).
DISCUSSION
Our study demonstrated that local anesthesia offered significant benefits in patients having inguinal hernia surgery. Patients aged 75 years and older were significantly less likely to have postoperative complications when the surgery was performed under local anesthesia. In particular, there was a reduction in urinary tract infections, which may be a reflection of a lower rate of postoperative urinary retention when local as opposed to general anesthesia is utilized. The reduced complication rate in the oldest patients (≥75 years) did not come at the expense of increased procedure time, as there was no significant difference in total operative time for surgeries performed under local compared to general anesthesia in these patients. In contrast, local anesthesia was not associated with a reduction in complications for patients under 75 years old, however, there was a significant reduction in operative time. The magnitude of the observed effects may appear to be small (less than a 1% reduction in complications and a difference of about 3 minutes in operative time) but the effects on our healthcare system overall are substantial because inguinal hernia repair is an extremely common operation. Using only the difference in operative time, we found that greater use of local anesthesia for hernia repair could save upwards of $47 million each year in the United States. Our estimate of cost savings is likely to be conservative, as we only included the decrease in operative time. Our results were overall robust to the choice of analytic approach however, we did note that for patients ≥75 years, there was no difference in complication rate was regression adjustment was employed. We also did not see any significant differences from the main findings when comparing patients with and without various comorbidities including heart failure, chronic obstructive pulmonary disease, diabetes, and dependence in activities of daily living (not shown).
Our projection for the potential benefits from greater use of local anesthesia likely represents a significant underestimate, especially for older adults. Exposure to general anesthesia may cause significant short- and medium-term cognitive dysfunction, in older adults.16,17 There is also some evidence, though far from conclusive, that general anesthesia increases risk of developing Alzheimer’s dementia.18,19 NSQIP does not capture changes in cognitive function or capacity for self-care, and these effects of general anesthesia are likely to increase the overall costs of hernia surgery. Further, we noted a disparity in use of local anesthesia among Non-Hispanic Whites (Table 1), which would be predicted to result in higher complications rates in African-American and Hispanic hernia surgery patients. Although racial and ethnic disparities were not the focus of our study, future work should examine the disparate economic impact of local vs general anesthesia use among these minority groups.
Our results are consistent with most studies that compare local versus general anesthesia for inguinal hernia surgery, though this is the first study to explicitly examine whether the effects of local anesthesia vary by age. Nordin etal. conducted a randomized study comparing local, regional, and general anesthesia for inguinal hernia repair. Mean age of participants in their study was 57 years for the local group and 56 years for the general group. Similar to the current study, the authors found that local anesthesia was associated with a 5-minute decrease in operative time compared to general anesthesia. They also noted a 19% reduction in unplanned admissions, which was not present in our NSQIP analysis.8 The authors found that using local anesthesia saved £316 ($413) in healthcare costs compared to general anesthesia, which was primarily attributable to a reduction in operative and recovery time.7 In contrast, O’Dwyer et al. randomly assigned 276 patients to local or general anesthesia for inguinal hernia surgery, with a mean age of 55 years for each group.9 The authors did not find a significant difference in operative time or complication rates, but did note cost savings of £30.5 ($40) per case. Neither of these randomized trials specifically examined outcomes among older adults compared to younger ones, and neither study was adequately powered to detect small differences in complication rates.
Bhattacharya et al. conducted a study of 25,213 patients using NSQIP data from 2005–2009 comparing general to local/regional (combined local, spinal, or other regional) anesthesia for inguinal hernia repair.5 The local/regional group demonstrated a 10-minute decrease in total operative time, and a 0.4% reduction in morbidity, which is similar to the current study, although they noted a much more substantial reduction in operative time. Another study used the International Hernia Mesh Registry to track quality of life for 1 year after inguinal hernia repair under local and general anesthesia in 1,128 patients, and found improved quality of life at up to 1 year after surgery when the operation was performed under local anesthesia.20 These studies focused on the overall population, without analyzing differences in older patients. Finally, Bay-Nielsen et al. used the Danish Hernia Database to identify 29,033 elective inguinal hernia operations and found a lower complication rate among patients 65 years and older having surgery under local anesthesia (2.1%, 95% CI 1.5%–2.9%) compared to general (2.8%, 95% CI 2.5%–3.1%).21 The complication rate of our study was much lower across all age groups, although the change in complication rate was similar. Unfortunately, their analysis did not risk-adjust for comorbidities or other confounders.
Our study is distinguished from prior work by exploring outcome differences based on age. We also divided the older population into distinct groups (65–74 and 75+ years) for analysis, which allowed us to examine finer trends as patient age increases. Additionally, we employed a more robust methodology than prior studies by using several propensity score-based methods. This approach increases confidence in the results because even though each method estimates the average treatment effect differently, they all yielded similar findings. Finally, the large sample size enabled us to detect smaller differences in outcomes than the relatively underpowered randomized trials.
Our findings provide novel information for surgeons to consider when deciding on their approach to open inguinal hernia repair, but there are several limitations to acknowledge. First, use of propensity scores can only adjust for known confounders within the data set. It is possible that unknown confounders could account for observed differences. NSQIP does not capture postoperative urinary retention or need for catheterization, which are common complications of general but not local anesthesia, so our projections likely underestimate the true benefit of local anesthesia in the oldest patients. Finally, NSQIP does not contain information on outcomes beyond the 30-day postoperative period, so we cannot comment on the effects of local versus general anesthesia on longer-term outcomes.
CONCLUSIONS
Our findings suggest that surgeons who perform open inguinal hernia repair should strongly consider using local rather than general anesthesia regardless of patient age. Greater use of local can enhance postoperative recovery by reducing complications in patients aged 75 years and older, which would improve patient outcomes and may produce substantial savings for health systems. While there did not appear to be a reduction in morbidity for patients younger than 75 years, the reduced operative time in this group contributes to significant cost savings and improved operating room efficiency. Given the observational nature of this study, our findings should ultimately be confirmed by a randomized trial focusing on older adults.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to thank Dave Primm for help in editing this manuscript.
This work was supported by a GEMSSTAR grant from the National Institute of Aging (1R03AG056330; for C.J.B.). Dr. Brown was supported, in part, by a VA Rehabilitation R&D Merit Award (1 I01 RX001995). Dr. Berger acknowledges support from K76 AG057022.
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Digestive diseases statistics for the United States. https://www.aafp.org/afp/2013/0615/p844.html-afp20130615p844-b2. Published 2010. Accessed 12/20/2017.
- 2.Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surgical Clinics of North America. 2003;83(5):1045–1051. [DOI] [PubMed] [Google Scholar]
- 3.de Goede B, Timmermans L, van Kempen BJH, et al. Risk factors for inguinal hernia in middle-aged and elderly men: Results from the Rotterdam Study. Surgery. 2015;157(3):540–546. [DOI] [PubMed] [Google Scholar]
- 4.Ruhl CE, Everhart JE. Risk Factors for Inguinal Hernia among Adults in the US Population. American Journal of Epidemiology. 2007;165(10):1154–1161. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharya SD, Vaslef SN, Pappas TN, Scarborough JE. Locoregional versus general anesthesia for open inguinal herniorrhaphy: a National Surgical Quality Improvement Program analysis. Am Surg. 2012;78(7):798–802. [PubMed] [Google Scholar]
- 6.Neumayer L, Giobbie-Hurder A, Jonasson O, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med. 2004;350(18):1819–1827. [DOI] [PubMed] [Google Scholar]
- 7.Nordin P, Zetterström H, Carlsson P, Nilsson E. Cost–effectiveness analysis of local, regional and general anaesthesia for inguinal hernia repair using data from a randomized clinical trial. British Journal of Surgery. 2007;94(4):500–505. [DOI] [PubMed] [Google Scholar]
- 8.Nordin P, Zetterström H, Gunnarsson U, Nilsson E. Local, regional, or general anaesthesia in groin hernia repair: multicentre randomised trial. The Lancet. 2003;362(9387):853–858. [DOI] [PubMed] [Google Scholar]
- 9.O’Dwyer PJ, Serpell MG, Millar K, et al. Local or General Anesthesia for Open Hernia Repair: A Randomized Trial. Annals of Surgery. 2003;237(4):574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hussain M, Berger M, Eckenhoff RG, Seitz DP. General anesthetic and the risk of dementia in elderly patients: current insights. Clin Interv Aging. 2014;9:1619–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Optimal Perioperative Management of the Geriatric Patient: Best Practices Guidelines from ACS NSQIP/American Geriatrics Society. . Available at: https://www.facs.org/~/media/files/quality_programs/geriatrics/acs. Accessed 12/18/2017.
- 12.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. American Statistician. 1985;39:33–38. [Google Scholar]
- 13.Austin PC. The relative ability of different propensity score methods to balance measured covariates between treated and untreated subjects in observational studies. Med Decis Making. 2009;29(6):661–677. [DOI] [PubMed] [Google Scholar]
- 14.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Communications in Statistics Simulation and Computation. 2009;38:1228–1234. [Google Scholar]
- 15.Childers CP, Maggard-Gibbons M. Understanding Costs of Care in the Operating Room. JAMA surgery. 2018;153(4):e176233–e176233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term postoperative cognitive dysfunction in the elderly: ISPOCD1 study. The Lancet. 1998;351(9106):857–861. [DOI] [PubMed] [Google Scholar]
- 17.Optimal Perioperative Management of the Geriatric Patient: Best Practices Guidelines from ACS NSQIP/American Geriatrics Society. https://www.facs.org/~/media/files/qualityprograms/geriatric/acs. Accessed 12/18/2017.
- 18.Chen C-W, Lin C-C, Chen K-B, Kuo Y-C, Li C-Y, Chung C-J. Increased risk of dementia in people with previous exposure to general anesthesia: A nationwide population-based case–control study. Alzheimer’s & Dementia. 2014;10(2):196–204. [DOI] [PubMed] [Google Scholar]
- 19.Chen P-L, Yang C-W, Tseng Y-K, et al. Risk of dementia after anaesthesia and surgery. The British Journal of Psychiatry. 2014;204(3):188–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huntington CR, Wormer BA, Cox TC, et al. Local Anesthesia in Open Inguinal Hernia Repair Improves Postoperative Quality of Life Compared to General Anesthesia: A Prospective, International Study. The American Surgeon. 2015;81(7):704–709. [PubMed] [Google Scholar]
- 21.Bay-Nielsen M, Kehlet H. Anaesthesia and post-operative morbidity after elective groin hernia repair: a nation-wide study. Acta Anaesthesiologica Scandinavica. 2008;52(2):169–174. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.