Abstract
Background
COVID-19 pandemic caused huge decrease of pediatric admissions to Emergency Department (ED), arising concerns about possible delays in diagnosis and treatment of severe disorders.
Methods
Impact of COVID-19 on Pediatric Emergency Room (ICOPER) was a retrospective multicentre observational study including 23 Italian EDs.
All the children <18 years admitted, between March 9th and May 3rd 2020 stratified by age, priority code, cause of admission and outcome have been included and compared to those admitted in the same period of 2019.
Our objectives were to assess the characteristics of pediatric admissions to EDs since COVID-19 outbreak until the end of lockdown, and to describe the features of critical children.
Findings
16,426 children were admitted in 2020, compared to 55,643 in 2019 (-70·48%). Higher reduction was reported in hospitals without Pediatric Intensive Care Unit (PICU) (-73·38%) than in those with PICU (-64·08%) (P<0·0001). Admissions with low priority decreased more than critical ones (-82·77% vs. 44·17% respectively; P<0·0001). Reduction of discharged patients was observed both in hospitals with (-66·50%) and without PICU (-74·65%) (P<0·0001). No difference in the duration of symptoms before admission was reported between 2019 and 2020, with the majority of children accessing within 24 h (55·08% vs. 57·28% respectively; P = 0·2344).
Interpretation
Admissions with low priority decreased significantly more than those with high priority; we suppose that the fear of being infected in hospital maybe overcame the concerns of caregivers. Compared to 2019, no significant referral delay by caregivers was reported. Our data suggest the need of adaptation of EDs and primary care services to different needs of children during COVID-9 pandemic.
1. Introduction
The Coronavirus Disease (COVID-19), caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), has provoked a global crisis, leading the World Health Organization to declare the pandemic on March 11th, 2020 [1].
Due to high contagiousness and significant morbidity and mortality rates, many Countries have imposed social distancing, and all public activities have been banned [1]. North-Western Italy was hardly hit by the pandemic. On February 20th, 2020, the first case of COVID-19 has been recorded in a small town of Lombardy, and the lockdown of the whole Country was then imposed between March 9th and May 3rd, 2020.
The burden of the disease involved mainly the older age groups, whereas children were pretty asymptomatic or experienced mild symptoms, resulting in a small number of pediatric COVID-19 visits to the Emergency Department (ED) [2, 3]. On current available Italian surveillance data, 17·3% of reported cases involved children [4]. On the other hand, more concerns arise from the novel Multisystem Inflammatory Syndrome in Children (MIS-C) associated with SARS-CoV-2 infection, which has been increasingly reported, and is characterized by persistent fever, abdominal pain, vomiting, diarrhea, rash, conjunctivitis and other mucocutaneous features [5, 6]. MIS-C is a life-threating condition that may rapidly progress to cardiac failure.
At the same time, decreasing trend of ED admissions was reported since the very first day of lockdown, mainly in pediatric settings [7]. Compared to the same period of past years, many Italian authors have reported a huge reduction of pediatric admissions to ED, ranging from 72% to 92% [1, 3, [8], [9], [10], [11], [12], [13]].
The main aim of our multicentre retrospective study was to assess the number and characteristics of pediatric admissions to ED since the outbreak of COVID-19 until the end of lockdown, compared to the same period of 2019. Second, we described the main features of critical children accessing EDs with high priority.
2. Methods
All the children <18 years admitted to all the 23 Pediatric EDs of Piedmont and Aosta Valley, North-Western Italy, between March 9th and May 3rd, 2020 were included in this multicentre retrospective observational study, and compared to those admitted in the same period of 2019. Among the centres involved, 3 were major Pediatric EDs of hospitals provided with Pediatric Intensive Care Unit (PICU) and 20 were Pediatric EDs of hospitals without PICU.
The medical record databases of each ED were screened for information on the demographic profile of children (age and gender), triage priority code (from lower to higher priority: white, green, yellow and red), and outcome (discharge home, admission to hospital, admission to PICU, transfer to another center). According to age, all the children were stratified in 5 classes: 0–2 years, 3–5 years, 6–10 years, 11–14 years and 15–18 years.
Secondly, we have compared all the children <18 years admitted on March 2019 to those admitted on March 2020, stratified by cause of admission (infectious disease, surgical problem, trauma, psychiatric disorder, and others), and priority code.
Last, we have compared all the children with high priority code (yellow and red) admitted on March 2020 to those evaluated on March 2019. Data about this subgroup of children included age, comorbidities, general practitioner visit before admission, symptoms before admission, cause of admission and outcome.
Every participating centre returned two ad hoc report forms to the Coordinating centre. In the first form, every centre reported the total number of children admitted during the study period, stratified by age, gender, priority code, and outcome. In the second form, every centre reported the total number of children admitted on March 2019 and 2020, stratified by cause of admission and priority code, and those admitted in the same period with high priority code, stratified by the variables described above. The Coordinating centre merged all data in the same database before the analysis.
The study protocol was approved by the Ethical Committee of the Coordinating centre of Turin on June 23rd, 2020 (protocol number: 0060387).
2.1. Statistical analysis
All the statistical analysis were made by comparing the 3 major EDs to the 20 EDs of hospitals without PICU and were performed using SAS V9.4.
ED admissions have been described by absolute frequency and percentage and their reduction between 2019 and 2020 was measured using percentages. Comparison between percentage distribution of characteristics at admission and year of admissions (2019 or 2020) and between characteristics at admission and type of hospital (with or without PICU) have been performed using the Chi-square test or the Fisher's exact test, when the hypothesis for Chi-square test was not met. The significance level was set at alpha=0·05.
To account for multiple comparisons, we estimated the False Discovery Rate (FDR) based on the Benjamini–Hochberg method [14] and we computed the FDR-adjusted p-values at 5% level.
2.2. Role of the funding source
No funding was received for this study.
3. Results
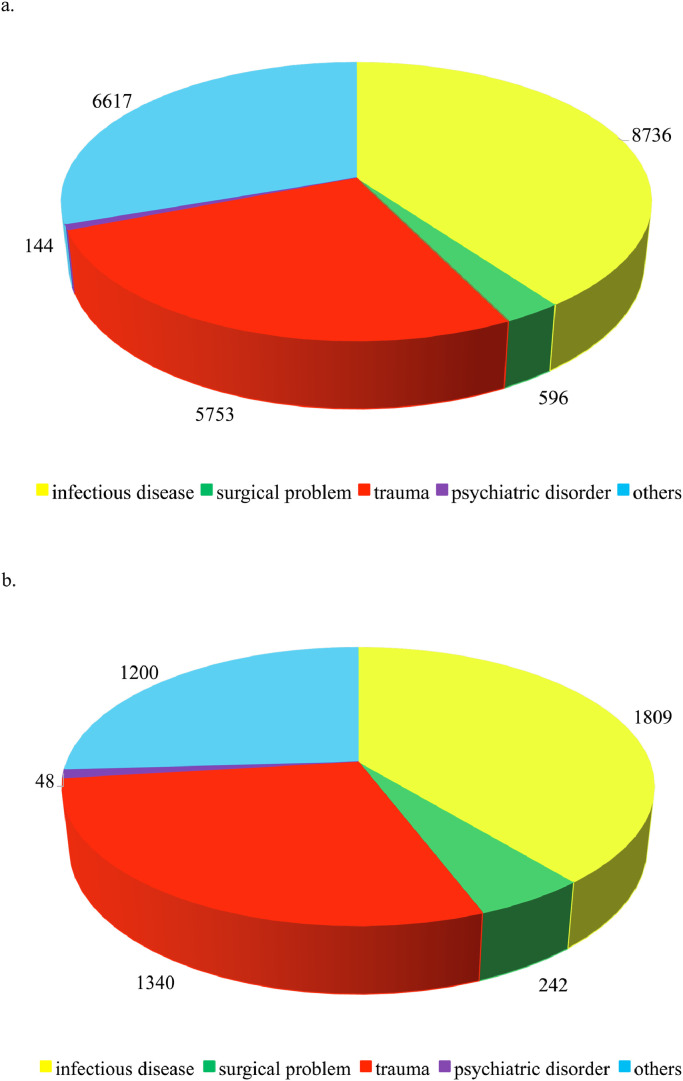
Overall, 16,426 children were admitted to the 23 Pediatric EDs during the study period on 2020, compared to 55,643 admissions recorded on 2019 in the same period (−70·48%). Children aging 0–5 years were 9269 on 2020 (56·43%) and 29,237 on 2019 (52·54%), respectively. Admissions with high priority (yellow and red code) were 1494 (9·09%) on 2020 and 3835 (6·91%) on 2019. Children being discharged home were 14,485 on 2020 (88·18%) and 51,937 on 2019 (93·34%), while those admitted to PICU were 27 (0·16%) and 30 (0·05%), respectively on 2020 and 2019. The distribution of the causes of admission on March of both years is shown in Fig. 1. After stratification by triage priority code, age and outcome, significant reduction of admissions was observed in each class (Table 1).
Fig. 1.
Causes of pediatric admissions (total number) to Emergency Departments on March 2019 (a) and March 2020 (b).
Table 1.
Decrease of admissions to Pediatric Emergency Departments in all the 23 Centres involved (period: March 9th - May 3rd, 2020 vs. March 9th - May 3rd, 2019), stratified by priority code, age and outcome.
| 2019 | 2020 | Decrease of admissions% | p-value | ||
| Total admissions N (%) | 55,643 (100·00) |
16,426 (100·00) |
−70·48 |
||
| Admissions to hospitals with PICUa | 17,343 (31·17) |
6230 (37·93) |
−64·08 |
<0.0001* | |
| Admissions to hospitals without PICUa | 38,300 (68·83) |
10,196 (62·07) |
−73·38 |
||
| Triage priority code | White | 6386 (11·48) |
1100 (6·70) |
−82·77 |
<0.0001* |
| Green | 45,422 (81·63) |
13,832 (84·21) |
−69·55 |
||
| Yellow | 3715 (6·67) |
1427 (8·68) |
−61·59 |
||
| Red | 120 (0·22) |
67 (0·41) |
−44·17 |
||
| Age (years) | 0–2 | 16,842 (30·27) |
5575 (33·94) |
−66·90 |
<0.0001* |
| 3–5 | 12,395 (22·28) |
3694 (22·49) |
−70·20 |
||
| 6–10 | 14,274 (25·65) |
4080 (24·84) |
−71·42 |
||
| 11–14 | 9390 (16·88) |
2298 (13·99) |
−75·53 |
||
| 15–18 | 2742 (4·92) |
779 (4·74) |
−71·59 |
||
| Discharged home | 51,937 (93·34) |
14,485 (88·18) |
−72·11 |
<0.0001* | |
| Admissions to hospital | 3415 (6·14) |
1798 (10·95) |
−47·35 |
||
| Outcome | Transferrals to another hospital | 261 (0·47) |
116 (0·71) |
−55·56 |
|
| Admissions to PICUa | 30 (0·05) |
27 (0·16) |
−10·00 |
0.04 | |
| Admissions to other than PICUa | 3385 (6·08) |
1771 (10·78) |
−47·68 |
False Discovery Rate corrected p-value <0·05.
PICU: Pediatric Intensive Care Unit.
Among admissions due to infectious disease, two children had encephalitis and one had sepsis, all on 2019. Overall, four children were admitted for status epilepticus (two on 2020) and nine for the onset of diabetes type I (three on 2020). Among overall children with psychiatric disorders, 12 were suicidal attempts (five on 2020). Admissions for abuse and neglect were 34 (six on 2020). On 2020, two children with MIS-C have been recorded, showing persistent fever, diarrhea, and mucocutaneous involvement (conjunctivitis, fissured lips, skin rash, erythema, and edema of hands and feet). They both had high level of SARS-CoV2 antibody and inflammation markers, lymphopenia, thrombocytopenia, and complement consumption, but negative nasal swabs.
3.1. Comparison between hospitals with and without PICU stratified by priority code, age and outcome
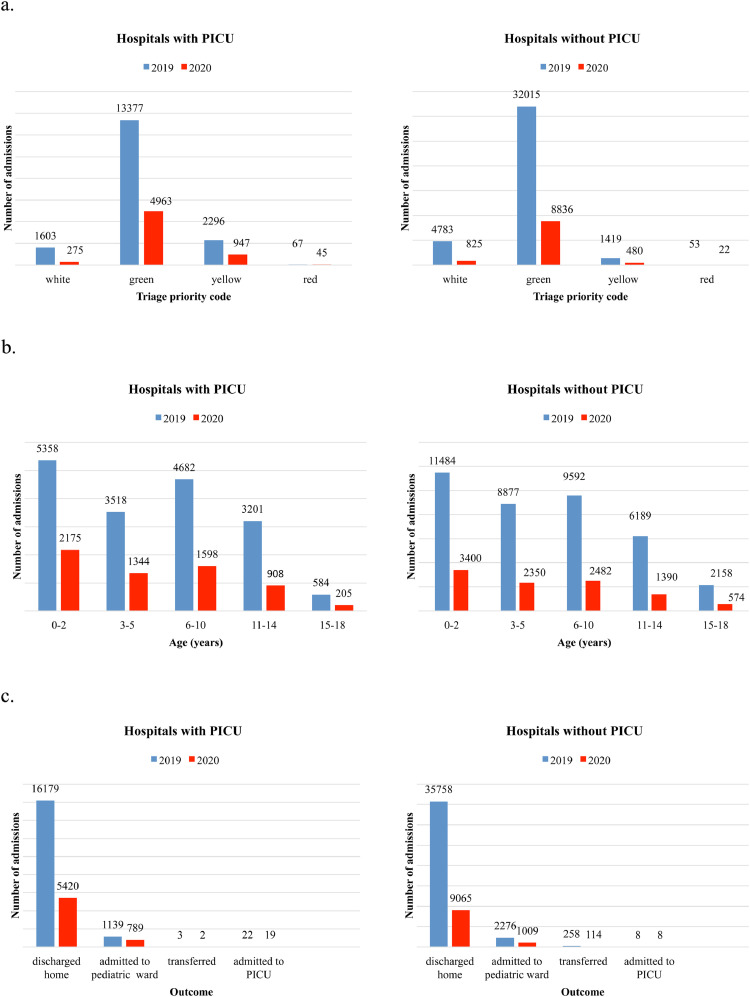
The reduction of admissions was reported in Pediatric EDs of hospitals without PICU (−73·38%) and in those with PICU (−64·08%) with a significant decrease in both of them (p <0·0001). Detailed descriptive analysis by priority code, age, and outcome is shown in Fig. 2 and Table 2.
Fig. 2.
Admissions to the Pediatric Emergency Department of hospitals with Pediatric Intensive Care Unit (PICU) compared to hospitals without PICU between March 9th and May 3rd, 2019 vs. March 9th and May 3rd, 2020, stratified by: a. priority code b. age c. outcome.
Table 2.
Admissions to the Pediatric Emergency Department of hospitals with Pediatric Intensive Care Unit (PICU) compared to hospitals without PICU between March 9th and May 3rd, 2019 vs. March 9th and May 3rd, 2020, stratified by priority code, age and outcome.
| Hospitals with PICUa |
Hospitals without PICUa |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | Decrease of admissions% | p-value | 2019 | 2020 | Decrease of admissions% | p-value | p-value comparison hospitals with PICUa vs. hospitals without PICUa | ||
| Total admissions N (%) | 17,343(100·00) | 6230(100·00) | −64·08 | 38,300(100·00) | 10,196(100·00) | −73·38 | <0·0001* | |||
| Triage priority code | White | 1603 (9·24) |
275 (4·19) |
−82·84 |
<0·0001* | 4783 (12·49) |
825 (8·09) |
−82·75 |
<0·0001* | 0·942 |
| Green | 13,377 (77·13) |
4963 (79·79) |
−62·90 |
32,045 (83·67) |
8869 (86·98) |
−72·32 |
<0·0001* | |||
| Yellow | 2296 (13·24) |
947 (15·29) |
−58·75 |
1419 (3·70) |
480 (4·71) |
−66·17 |
0·002* | |||
| Red | 67 (0·39) |
45 (0·73) |
−32·84 |
53 (0·14) |
22 (0·22) |
−58·49 |
0·130 | |||
| Age (years) | 0–2 | 5358 (30·89) |
2175 (34·91) |
−59·41 |
<0·0001* | 11,484 (29·99) |
3400 (33·35) |
−70·39 |
<0·0001* | <0·0001* |
| 3–5 | 3518 (20·28) |
1344 (21·57) |
−61·80 |
8877 (23·18) |
2350 (23·05) |
−73·53 |
<0·0001* | |||
| 6–10 | 4682 (27·00) |
1598 (25·65) |
−65·87 |
9592 (25·04) |
2482 (24·34) |
−74·12 |
<0·0001* | |||
| 11–14 | 3201 (18·46) |
908 (14·58) |
−71·63 |
6189 (16·16) |
1390 (13·63) |
−77·54 |
<0·0001* | |||
| 15–18 | 584 (3·37) |
205 (3·29) |
−64·90 |
2158 (5·63) |
574 (5·63) |
−73·40 |
0·003* | |||
| Outcome | Discharged home | 16,179 (93·29) |
5420 (87·00) |
−66·50 |
<0·0001* | 35,758 (93·37) |
9065 (88·90) |
−74·65 |
<0·0001* | <0·0001* |
| Admissions to hospital | 1139 (6·56) |
789 (12·66) |
−30·73 |
2276 (5·94) |
1009 (9·90) |
−55·67 |
<0·0001* | |||
| Transferrals to another hospital | 3 (0·02) |
2 (0·03) |
−33·33 |
258 (0·67) |
114 (1·12) |
−55·81 |
0·976 | |||
| Admissions to PICUa | 22 (0·13) |
19 (0·31) |
−13·64 |
0·467 | 8 (0·02) |
8 (0·08) |
0·00 |
0·089 | 0·804 | |
| Admissions to other than PICUa | 1117 (6·44) | 770 (12·36) |
−31·06 |
2268 (5·92) | 1001 (9·82) |
−55·86 |
||||
False Discovery Rate corrected p-value <0·05.
PICU: Pediatric Intensive Care Unit.
3.2. Comparison between 2019 and 2020 by cause of admission and priority code
Focusing only on March, we observed 21,846 admissions in 2019, and 4639 in 2020 (−76·76%). After stratification by cause of admission (Figure 1), we observed a significant decrease of the absolute number of admissions for all the subgroups (p <0·0001), especially for infectious disease (−79·29%), and less sharply for surgical and psychiatric disorder (−59·4% and −66·67%, respectively). Admissions for surgical problems with yellow priority code decreased significantly (p = 0·0002), but less than other admissions with the same priority (Table 3).
Table 3.
Decrease of admissions to Pediatric Emergency Departments of all the 23 Centres on March 2020 vs. March 2019, stratified by priority code and cause of admission.
| 2019 | 2020 | Decrease of admissions% | p-value | |
|---|---|---|---|---|
| Total admissions N (%) | 21,846 (100·00) |
4639 (100·00) |
−76·76 |
|
| All priority codes | ||||
| Infectious disease | 8736 (39·99) |
1809 (39·00) |
−79·29 |
<0·0001* |
| Surgical problem | 596 (2·73) |
242 (5·22) |
−59·40 |
|
| Trauma | 5753 (26·33) |
1340 (28·89) |
−76·71 |
|
| Psychiatric disorder | 144 (0·66) |
48 (1·02) |
−66·67 |
|
| Other disease | 6617 (30·29) |
1200 (25·87) |
−81·86 |
|
| White code | ||||
| Infectious disease | 969 (4·44) |
124 (2·67) |
−87·20 |
0·457 |
| Surgical problem | 40 (0·18) |
7 (0·15) |
−82·50 |
|
| Trauma | 283 (1·30) |
35 (0·75) |
−87·63 |
|
| Psychiatric disorder | 2 (0·01) |
1 (0·02) |
−50·00 |
|
| Other disease | 862 (3·95) |
124 (2·67) |
−85·61 |
|
| Green code | ||||
| Infectious disease | 7154 (32·75) |
1507 (32·49) |
−78·93 |
<0·0001* |
| Surgical problem | 487 (2·22) |
185 (3·99) |
−62·01 |
|
| Trauma | 5183 (23·72) |
1220 (26·30) |
−76·46 |
|
| Psychiatric disorder | 90 (0·41) |
27 (0·58) |
−70·00 |
|
| Other disease | 5289 (24·21) |
901 (19·42) |
−82·96 |
|
| Yellow code | ||||
| Infectious disease | 583 (2·66) |
165 (3·57) |
−71·70 |
0·0002* |
| Surgical problem | 69 (0·32) |
48 (1·03) |
−30·43 |
|
| Trauma | 281 (1·28) |
83 (1·79) |
−70·46 |
|
| Psychiatric disorder | 52 (0·24) |
19 (0·41) |
−63·46 |
|
| Other disease | 447 (2·05) |
165 (3·56) |
−63·09 |
|
| Red code | ||||
| Infectious disease | 30 (0·14) |
13 (0·28) |
−56·57 |
0·187 |
| Surgical problem | 0 (0·00) |
2 (0·04) |
Not applicable |
|
| Trauma | 6 (0·03) |
2 (0·04) |
−66·67 |
|
| Psychiatric disorder | 0 (0·00) |
1 (0·02) |
Not applicable |
|
| Other disease | 19 (0·09) |
10 (0·22) |
−47·37 |
|
False Discovery Rate corrected p-value <0·05.
In the same period, comparing children admitted to hospitals with and without PICU stratified by cause of admission and priority code, we observed significantly higher decrease of all the causes of admissions with any priority code to hospitals without PICU than with PICU (p<0·0001), except for psychiatric disorders (p = 0·238).
Detailed analysis is reported in Table 4.
Table 4.
Admissions to the Pediatric Emergency Department of hospitals with Pediatric Intensive Care Unit (PICU) compared to hospitals without PICU on March 2019 vs. March 2020, stratified by priority code and cause of admission.
| Hospitals with PICUa |
Hospitals without PICUa |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | Decrease of admissions% | p-value | 2019 | 2020 | Decrease of admissions% | p-value | p-value comparison hospitals with PICUa vs. hospitals without PICUa | |
| Total admissions N (%) | 7021 (100·00) |
1920 (100·00) |
−72·65 |
14,825 (100·00) |
2719 (100·00) |
−81·66 |
|||
| All priority codes | |||||||||
| Infectious disease | 2603 (37·07) |
662 (34·48) |
−74·57 |
<0·0001* | 6133 (41·37) |
1147 (42·18) |
−81·30 |
<0·0001* | <0·0001* |
| Surgical problem | 212 (3·02) |
142 (7·40) |
−33·02 |
384 (2·59) |
100 (3·68) |
−73·96 |
<0·0001* | ||
| Trauma | 2050 (29·20) |
622 (32·40) |
−69·66 |
3703 (24·98) |
718 (26·41) |
−80·61 |
<0·0001* | ||
| Psychiatric disorder | 58 (0·83) |
24 (1·25) |
−58·62 |
86 (0·58) |
24 (0·88) |
−72·09 |
0·238 | ||
| Other disease | 2098 (29·88) |
470 (24·48) |
−77·60 |
4519 (30·48) |
730 (26·85) |
−83·85 |
<0·0001* | ||
| White code | |||||||||
| Infectious disease | 254 (3·50) |
21 (1·09) |
−91·73 |
Not applicable | 715 (4·82) |
103 (3·79) |
−85·59 |
0·595 | 0·025 |
| Surgical problem | 22 (0·31) |
3 (0·15) |
−86·36 |
18 (0·12) |
4 (0·15) |
−77·78 |
0·553 | ||
| Trauma | 47 (0·61) |
0 (0·00) |
−100 |
236 (1·59) |
35 (1·28) |
−85·17 |
0·009* | ||
| Psychiatric disorder | 0 (0·00) |
0 (0·00) |
Not applicable |
2 (0·01) |
1 (0·04) |
−50·00 |
Not applicable | ||
| Other disease | 307 (4·30) |
40 (2·08) |
−86·97 |
555 (3·75) |
84 (3·09) |
−84·86 |
0·464 | ||
| Green code | |||||||||
| Infectious disease | 1922 (27·32) |
518 (26·98) |
−73·05 |
<0·0001* | 5232 (35·29) |
989 (36·38) |
−81·86 |
<0·0001* | <0·0001* |
| Surgical problem | 146 (2·05) |
100 (5·22) |
−31·51 |
341 (2·30) |
85 (3·13) |
−75·07 |
<0·0001* | ||
| Trauma | 1833 (26·10) |
574 (29·89) |
−68·69 |
3350 (22·61) |
646 (23·75) |
−80·72 |
<0·0001* | ||
| Psychiatric disorder | 25 (0·33) |
12 (0·63) |
−52·00 |
65 (0·44) |
15 (0·55) |
−76·92 |
0·102 | ||
| Other disease | 1541 (21·94) |
337 (17·55) |
−78·33 |
3748 (25·28) |
564 (20·74) |
−84·95 |
<0·0001* | ||
| Yellow code | |||||||||
| Infectious disease | 421 (6·00) |
111 (5·78) |
−73·63 |
<0·0001* | 162 (1·09) |
54 (1·99) |
−66·67 |
0·560 | 0·216 |
| Surgical problem | 44 (0·60) |
38 (1·98) |
−13·64 |
25 (0·17) |
10 (0·36) |
−60·00 |
0·074 | ||
| Trauma | 146 (2·05) |
47 (2·45) |
−67·81 |
135 (0·91) |
36 (1·32) |
−73·33 |
0·454 | ||
| Psychiatric disorder | 33 (0·46) |
12 (0·63) |
−63·64 |
19 (0·13) |
7 (0·26) |
−63·16 |
0·981 | ||
| Other disease | 250 (3·52) |
88 (4·58) |
−64·80 |
197 (1·33) |
77 (2·83) |
−60·91 |
0·567 | ||
| Red code | |||||||||
| Infectious disease | 16 (0·22) |
12 (0·63) |
−25·00 |
Not applicable | 14 (0·09) |
1 (0·04) |
−92·86 |
0·028 | 0·014* |
| Surgical problem | 0 (0·00) |
1 (0·05) |
Not applicable |
0 (0·00) |
1 (0·04) |
Not applicable |
Not applicable | ||
| Trauma | 4 (0·55) |
1 (0·05) |
−75·00 |
2 (0·01) |
1 (0·04) |
−50·00 |
0·673 | ||
| Psychiatric disorder | 0 (0·00) |
0 (0·00) |
Not applicable |
0 (0·00) |
1 (0·04) |
Not applicable |
Not applicable | ||
| Other disease | 10 (0·14) |
5 (0·26) |
−50·00 |
9 (0·06) |
5 (0·18) |
−44·44 |
0·893 | ||
False Discovery Rate corrected p-value <0·05.
PICU: Pediatric Intensive Care Unit.
3.3. Comparison between 2019 and 2020 by features of critical admissions
Focusing only on critical patients (Table 5), yellow and red codes were 508 on March 2020, compared to 1487 on March 2019 (−65·84%). We observed no difference in the duration of symptoms before admission between 2019 and 2020 (p = 0·2344), with majority of children accessing EDs within 24 h since the onset of symptoms. The features of critical admissions to hospitals with and without PICU are described in Tables 6 and 7, respectively.
Table 5.
Decrease of admissions with high priority codes (yellow and red) to Pediatric Emergency Departments (EDs) in all the 23 Centres on March 2020 vs. March 2019, stratified by age, comorbidities, cause of ED admission, general practitioner visit before admission, duration of symptoms before admission, and outcome.
| 2019 | 2020 | p-value | ||
|---|---|---|---|---|
| Total admissions N (%) | 1487(100·00) | 508(100·00) | ||
| Age | <12 months | 290 (19·51) |
114 (22·44) |
0·4879 |
| 12–23 months | 180 (12·10) |
73 (14·37) |
||
| 2–5 years | 410 (27·57) |
139 (27·36) |
||
| 6–9 years | 220 (14·79) |
57 (11·22) |
||
| 10–14 years | 286 (19·24) |
90 (17·72) |
||
| 15–18 years | 101 (6·79) |
35 (6·89) |
||
| Comorbidities | Yes | 293 (19·70) |
118 (23·22) |
0·0083* |
| No | 1194 (80·30) |
390 (76·78) |
||
| General practitioner visit before admission | Yes | 237 (15·94) |
72 (14·17) |
0·6091 |
| No | 1037 (69·74) |
369 (72·64) |
||
| Unknown | 213 (14·32) |
67 (13·19) |
||
|
Duration of symptoms before admission |
<24 h | 819 (55·08) |
291 (57·28) |
0·2344 |
| 1–3 days | 448 (30·12) |
127 (25·00) |
||
| 4–7 days | 108 (7·27) |
46 (9·05) |
||
| >7 days | 65 (4·37) |
25 (4·92) |
||
| Unknown | 47 (3·16) |
19 (3·75) |
||
| Cause of ED admission | Infectious disease | 608 (40·89) |
190 (37·40) |
0·0155* |
| Surgical problem | 61 (4·10) |
47 (9·25) |
||
| Trauma | 305 (20·51) |
105 (20·67) |
||
| Psychiatric disorder | 48 (3·23) |
17 (3·35) |
||
| Neurological disease | 167 (11·23) |
53 (10·43) |
||
| Other disease | 298 (20·04) |
96 (18·90) |
||
| Outcome | Discharge home | 828 (55·68) |
215 (42·32) |
<0·001* |
| Admission to hospital | 372 (25·02) |
168 (33·08) |
||
| Admission to Short Observation Unit | 198 (13·32) |
73 (14·37) |
||
| Admission to PICUa | 17 (1·14) |
11 (2·16) |
||
| Need for urgent surgery | 27 (1·81) |
18 (3·54) |
||
| Death | 0 (0·00) |
0 (0·00) |
||
| Transfer to another hospital | 33 (2·22) |
17 (3·35) |
||
| Spontaneously left the EDb | 3 (0·20) |
1 (0·20) |
||
| Admission refusal | 9 (0·61) |
5 (0·98) |
False Discovery Rate corrected p-value <0·05.
PICU: Pediatric Intensive Care Unit.
ED: Emergency Department.
Table 6.
Reduction of admissions with high priority code (yellow and red) to Pediatric Emergency Departments of hospitals with Pediatric Intensive Care Unit (PICU) on March 2020 vs. March 2019, stratified by age, comorbidities, general practitioner visit before admission, duration of symptoms before admission, cause of admission and outcome·.
| 2019 | 2020 | p-value | ||
|---|---|---|---|---|
| Total admissions N (%) | 924(100·00) | 315(100·00) | ||
| Age | <12 months | 232 (25·11) |
74 (23·49) |
0·3060 |
| 12–23 months | 112 (12·12) |
38 (12·06) |
||
| 2–5 years | 203 (21·97) |
86 (27·30) |
||
| 6–9 years | 147 (15·91) |
43 (13·66) |
||
| 10–14 years | 180 (19·48) |
52 (16·51) |
||
| 15–18 years | 50 (5·41) |
22 (6·98) |
||
| Comorbidities | Yes | 203 (21·97) |
92 (29·21) |
0·0020* |
| No | 721 (78·03) |
223 (70·79) |
||
| General practitioner visit before admission | Yes | 185 (20·02) |
52 (16·51) |
0·1208 |
| No | 526 (56·93) |
200 (63·49) |
||
| Unknown | 213 (23·05) |
63 (20·00) |
||
| Duration of symptoms before admission | <24 h | 483 (52·28) |
169 (53·65) |
0·5873 |
| 1–3 days | 257 (27·81) |
74 (23·49) |
||
| 4–7 days | 78 (8·44) |
30 (9·53) |
||
| >7 days | 61 (6·60) |
23 (7·30) |
||
| Unknown | 45 (4·87) |
19 (6·03) |
||
| Cause of admission | Infectious disease | 427 (46·21) |
124 (39·37) |
0·0043* |
| Surgical problems | 48 (5·19) |
36 (11·42) |
||
| Trauma | 151 (16·34) |
52 (16·51) |
||
| Psychiatric disorders | 32 (3·47) |
12 (3·81) |
||
| Neurological diseases | 81 (8·77) |
33 (10·48) |
||
| Other diseases | 185 (20·02) |
58 (18·41) |
||
| Outcome | Discharged home | 500 (54·11) |
131 (41·59) |
0·0009* |
| Admitted to pediatric ward | 231 (25·00) |
106 (33·65) |
||
| Admitted to Short Observation Unit | 152 (16·45) |
51 (16·19) |
||
| Admitted to PICUa | 11 (1·19) |
9 (2·86) |
||
| Need for urgent surgery | 24 (2·60) |
15 (4·76) |
||
| Death | 0 (0·00) |
0 (0·00) |
||
| Transferred to another hospital | 0 (0·00) |
1 (0·32) |
||
| Spontaneously left the EDb | 1 (0·11) |
0 (0·00) |
||
| Refuse admission | 5 (0·54) |
2 (0·63) |
False Discovery Rate corrected p-value <0·05.
Pediatric Intensive Care Unit.
Emergency Department.
Table 7.
Reduction of admissions with high priority code (yellow and red) to Pediatric Emergency Departments (EDs) of hospitals without Pediatric Intensive Care Unit (PICU) on March 2020 vs. March 2019, stratified by age, comorbidities, general practitioner visit before admission, duration of symptoms before admission, cause of admission and outcome·.
| 2019 | 2020 | p-value | ||
|---|---|---|---|---|
| Total admissions N (%) | 563(100·00) | 193(100·00) | ||
| Age | <12 months | 58 (10·30) |
40 (20·73) |
0·0351 |
| 12–23 months | 68 (12·08) |
35 (18·13) |
||
| 2–5 years | 207 (36·77) |
53 (27·46) |
||
| 6–9 years | 73 (12·96) |
14 (7·25) |
||
| 10–14 years | 106 (18·83) |
38 (19·69) |
||
| 15–18 years | 51 (9·06) |
13 (6·74) |
||
| Comorbidities | Yes | 90 (15·99) |
26 (13·47) |
0·0793 |
| No | 473 (84·01) |
167 (86·53) |
||
| General practitioner visit before admission | Yes | 52 (9·24) |
20 (10·37) |
0·0015* |
| No | 511 (90·76) |
169 (87·56) |
||
| Unknown | 0 (0·00) |
4 (2·07) |
||
| Duration of symptoms before admission | <24 h | 336 (59·68) |
122 (63·21) |
0·3321 |
| 1–3 days | 191 (33·93) |
53 (27·46) |
||
| 4–7 days | 30 (5·33) |
16 (8·29) |
||
| >7 days | 4 (0·71) |
2 (1·04) |
||
| Unknown | 2 (0·35) |
0 (0·00) |
||
| Cause of admission | Infectious disease | 181 (32·15) |
66 (34·20) |
0·8228 |
| Surgical problems | 13 (2·31) |
11 (5·70) |
||
| Trauma | 154 (27·35) |
53 (27·46) |
||
| Psychiatric disorders | 16 (2·84) |
5 (2·59) |
||
| Neurological diseases | 86 (15·28) |
20 (10·36) |
||
| Other diseases | 113 (20·07) |
38 (19·69) |
||
| Outcome | Discharged home | 328 (58·27) |
84 (43·53) |
0·0319 |
| Admitted to pediatric ward | 141 (25·04) |
62 (32·12) |
||
| Admitted to Short Observation Unit | 46 (8·17) |
22 (11·40) |
||
| Admitted to PICU | 6 (1·06) |
2 (1·04) |
||
| Need for urgent surgery | 3 (0·53) |
3 (1·55) |
||
| Death | 0 (0·00) |
0 (0·00) |
||
| Transferred to another hospital | 33 (5·87) |
16 (8·29) |
||
| Spontaneously left the ED | 2 (0·35) |
1 (0·52) |
||
| Refuse admission | 4 (0·71) |
3 (1·55) |
False Discovery Rate corrected p-value <0·05.
aPediatric Intensive Care Unit
bEmergency Department.
4. Discussion
This is the first large multicentre study describing how COVID-19 pandemic has changed the referral of children to EDs in hardly hit North-Western Italy. We observed massive reduction of pediatric admissions, as reported in already published subgroups of our population [8], [9], [10] and by other Italian centres [1, [11], [12], [13]]. Non-urgent visits have dropped significantly more than urgent ones, reflecting how maybe the fear of being infected by SARS-CoV-2 in hospitals overcame the anxiety and the need of reassurance of caregivers, as already reported in previous epidemics [15, 16]. We could suppose that COVID-19 has unveiled previous widespread misuse of emergency care facilities, which are often accessed for the management of non-urgent conditions. Children with green and yellow codes decreased significantly more in hospitals without PICU, and mild proportional increase of both high priority codes and admissions to PICU has been observed, as reported by Iozzi et al. [11] Anyway, the absolute number of high priority codes and admissions to PICU decreased, as recently noted by the Italian Network of Pediatric Intensive Care Unit Research Group [17]. Interestingly, we did not detect any significant delay in ED referral by caregivers, as previously speculated by other authors [11, 13].
Overall, on 2020 we observed a decrease of pediatric admissions to EDs for all the age groups, but in particular in major hospitals with PICU such reduction was less marked for younger children and patients with comorbidities and high priority code, who are usually more fragile. As already reported, the most evident drop regarded infectious diseases, which usually represent the main reason of Pediatric ED visits [11]. Children did not attend schools or other communities during the lockdown, thus decreasing the spread of both SARS-CoV-2 and other pathogens. Nonetheless, although restrictive measures and mandatory use of facial mask were imposed to all the population, we confirm that most of critical patients were affected by infectious diseases and admissions with high priority due to infections dropped significantly only in hospitals without PICU [11, 12]. This might be the expression of families’ preference to bring their children to major centres rather than to small ones during the lockdown, even if farer from home.
During the study period, only two cases of MIS-C were reported in our centres, and 14 more were recorded between the end of the study period and December 2020. The first reports of COVID-19-associated hyperinflammatory syndromes (including Kawasaki-like presentation and symptoms mimicking acute appendicitis and peritonitis) have been published on May 2020 [18, 19]. Unanimous consensus has not yet been reached either on diagnostic criteria or on therapy, and many different protocols have been proposed by different Institutions [6]. Based on available evidence and clinical awareness, we designed a dedicated clinical pathway: all the patients identified on clinical criteria underwent laboratory tests including investigations on inflammation, cardiac involvement, coagulation profile, and SARS-CoV2 serology; echocardiogram was always done as soon as possible. Therapy included corticosteroids and intravenous immunoglobulin, along with fluid restriction and strict cardiac and respiratory monitoring.
The considerable reduction of patients discharged home on 2020, especially in hospitals without PICU, was consistent to what reported by other Italian centres [8, 12]. We presume it could be due to the huge reduction of children with low priority conditions, who are usually more easily discharged. We suppose that massive reduction of non-critical ED admissions was also responsible for increased prevalence of critical ED admissions during the study period, which reduced significantly less, as already shown by other Italian centres [9, 13].
Another consequence of community isolation and social restrictions was the reduction of admissions related to trauma and outdoor injuries. Interestingly, the decrease of pediatric trauma was stronger than reported in March and April in Finland (−24%) and the United States, where fracture reduction was 58% [20, 21]. At the same time, we globally reported significantly lighter decrease of admissions due to surgical problems, compared to all the other subgroups, and proportional increase of need for urgent surgery only in hospitals without PICU. Anyway, no significant delay in presentation was reported for surgical problems or for any cause of admission with high priority code, as the analysis of the duration of critical patients’ symptoms before they accessed EDs showed no difference between 2019 and 2020.
Delayed access to EDs, due to the fear of contracting COVID-19, has been suggested to cause more severe clinical presentation of some children and adults [11, 13, 22, 23]. Anyway, such perception of pediatric healthcare professionals is not sustained by evidence provided by our study on a large population. In fact, the major part of our critical children arrived within 24 h since the onset of symptoms, suggesting that lockdown and fear of COVID-19 were not responsible for delayed provision of care. On the other hand, the results of an early single center report from Ireland [24] and other recent papers on the need for urgent surgery in large cohorts of children are consistent with our findings [20, 21]. Often, critical patients were not brought to their general practitioners before attending EDs: we might suppose that families preferred to refer directly to hospitals (in particular the major ones) in order not to delay diagnosis and care. Also increased prevalence of patients with comorbidities in major hospitals suggests such hypothesis. During the lockdown, the families of children with special needs felt particularly isolated and stressed [25]: though telemedicine has been implemented also by community medical services, we suppose that caregivers felt more reassured accessing directly the ED of reference centres.
The COVID-19 pandemic shows heavy impact on mental health of both adults and children, in particular those who already suffered from psychiatric disorders [26], [27], [28]. The global reduction of admissions for psychiatric disorders, along with the increased prevalence of children with mental health disorders among those admitted to Pediatric EDs during the study period are matter of concern, consistently with the results shown by McDonnell et al. [26] Our finding confirms the need to take particular care of children and adolescents’ mental health, as isolation and social restrictions may have serious psychiatric consequences, in particular on the most fragile patients [28].
Our study has some strengths. First, to our knowledge it is the first large multicentre study on the impact of COVID-19 on pediatric admissions to EDs in Europe. This allowed us to discuss previous hypothesis and perceptions based on case series and small studies in the early phase of the pandemic. In particular, we could demonstrate that there was no significant increase in time-to-presentation for care to our centres. Second, we could evaluate the differences between large hospitals and smaller ones: we believe this could be useful to help drawing future strategies. Last, it provides insight on the main causes of admittance to pediatric EDs, again helping eventual remodeling strategies for hospital emergency settings for next challenging times.
Our study has also some limits. Of course, first this is a retrospective study reflecting the experience of 23 EDs of North-Western Italy, which limits the generalizability of our results. However, all the Pediatric EDs of our region have been included and are representative of both urban and rural areas. Second, we did not compare admissions during lockdown to those immediately after its end, therefore we could not compare patients before and after re-opening activities, as reported by other studies [12]. Moreover, our analysis was performed only on aggregate data, so we could not use a time series model, or difference-in-difference approach to better describe the differences between admissions in 2019 and 2020. We are aware that the comparison of two time points using aggregate data might lead to some biases.
In conclusion, in our multicentre retrospective study, we observed massive reduction of pediatric admissions to EDs, but the decrease was higher in hospitals without PICU than in major ones with PICU. Admissions with low priority code decreased significantly more than those with high priority, in particular in hospitals without PICU; we suppose that the fear of being infected by SARS-CoV-2 maybe overcame the concerns of caregivers. Compared to 2019, no significant delay in ED referral by caregivers was reported on 2020. Dedicated strategies for the care of children with comorbidities or mental health disorders should be implemented, involving both hospitals and community medical services.
Author Contributions
IR, EC, IF, CB, FR, AFU have given substantial contribution to conception and design of the work; FR has given contributions to analysis and interpretation of data for the work; LB, ABdP, PC, GC, EF, PF, MRG, FG, PG, AG, OH, PM, AM, IvR, LR, SS, AS, ET, GMT, FST, FT, AV revised it critically for important intellectual content; SA, MA, AA, LB, MB, SB, GC, MC, RC, NC, EC, MC, EC, SDF, BDV, AGD, VDG, MED, RG, LG, DG, EG, MG, EG, GG, BL, CM, GM, MAM, IM, MP, FR, LR, RR, RoRo, RoRu, FT, IT, AT, CTop, CTor, AnT, CV, MPV, AnV, AlV have given contributions to the acquisition of data for the work; furthermore, they have draft, critically revised and finally approved the version to be published.
Declaration of Interests
Nothing to disclose.
Data sharing statement
Individual participant data that underlie the results reported in this article will be available after de-identification (text, tables, figures, and appendices). Other available documents will include the study protocol, the statistical analysis plan, and the analytic code. Data will be available at a third party website for 5 years, beginning 3 months after publication, to those investigators whose aims and types of analysis will be approved by an independent review committee identified for this purpose. The proposals should be directed to ecastagno@cittadellasalute.to.it to gain access, and data requestors will sign a data access agreement.
Footnotes
Impact of COVID-19 on Pediatric Emergency Room (ICOPER) Study Group:
Sonia Aguzzia, MD; Marco Aicardik, MD; Antonella Aimare, MD; Luca Baroerog, MD; Michelangelo Barbaglian, MD; Stefania Bezzioq, MD; Giulia Calossoh, MD; Mario M. Calvox, MD; Roberto Cerchioa, MD; Nicoletta Ceschinau, MD; Elisa Chiomab, MD; Margherita Conrieria, PhD; Elena Coppoa, MD; Simona De Francoo, MD; Barbara De Vitoa, MD; Angelo G. Delmonacoa, MD; Valeria Di Giannif MD; Maria E. Donadiob, MD; Rachele Gallos, MD; Laura Garassinom, MD; Davide Garellia, MD; Emanuela Garronea, MD; Marianna Genisiob, MD; Elena Giachettib, MD; Giulia Grassoa, MD; Barbara Lauriaa, MD; Cinzia Marcianoi, MD; Giuseppina Migliorea, MD; Maria Angela Militellop, MD; Ilaria Mussinattob, MD; Manuela Paganoa, PhD; Francesca Romanob, MD; Lorenza Rossib, MD; Roberta Rossia, MD; Romina Ruffattoz, MD; Francesco Tagliaferrir, MD; Irene Tardivoa, MD; Alberto Testaa, MD; Claudia Toppinoa, MD; Claudia Tortoneb, MD; Antonella Tuscanob, MD; Cristina Vassiaa, MD; Maria Paola Vardeua, MD; Antonia Versacea, MD; Alice Vianol, MD.
I, the corresponding author, had final responsibility for the decision to submit for publication.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanepe.2021.100081.
Appendix. Supplementary materials
References
- 1.Bellan A., Gavelli F., Hayden E. Pattern of emergency department referral during the Covid-19 outbreak in Italy. Panminerva Med. 2020 doi: 10.23736/S0031-0808.20.04000-8. [DOI] [PubMed] [Google Scholar]
- 2.Dong Y., Mo X., Hu Y. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020;145 [Google Scholar]
- 3.Parri N., Lenge M., Buonsenso D. Children with Covid-19 in pediatric emergency departments in Italy. N Engl J Med. 2020;383:187–190. doi: 10.1056/NEJMc2007617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Italian National Health Institute (Istituto Superiore di Sanità). COVID-19 epidemic. 20 October 2020 national update. October 23, 2020. (in Italian) https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_20-ottobre-2020.pdf. Accessed October 30,2020.
- 5.Blumfield E., Levin T.L., Kurian J., Lee E.Y., Liszewski M.C. Imaging findings in multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease (COVID-19) Am J Roentgenol. 2021;216:507–517. doi: 10.2214/AJR.20.24032. [DOI] [PubMed] [Google Scholar]
- 6.Dove M.L., Jaggi P., Kelleman M., Abuali M., Ang J.Y., Ballan W. Multisystem inflammatory syndrome in children: survey of protocols for early hospital evaluation and management. J Pediatr. 2021;229:33–40. doi: 10.1016/j.jpeds.2020.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Isba R., Edge R., Jenner R., Broughton E., Francis N., Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child. 2020;105:704. doi: 10.1136/archdischild-2020-319385. [DOI] [PubMed] [Google Scholar]
- 8.Scaramuzza A., Tagliaferri F., Bonetti L. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch Dis Child. 2020;105:704–706. doi: 10.1136/archdischild-2020-319397. [DOI] [PubMed] [Google Scholar]
- 9.Ciacchini B., Tonioli F., Marciano C. Reluctance to seek pediatric care during the COVID-19 pandemic and the risks of delayed diagnosis. Ital J Pediatr. 2020;46:87. doi: 10.1186/s13052-020-00849-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manzoni P., Militello M.A., Fiorica L., Cappiello A.R., Manzionna M. Impact of COVID-19 epidemics in paediatric morbidity and utilisation of hospital paediatric services in Italy. Acta Paediatr. 2020 doi: 10.1111/apa.15435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iozzi L., Brambilla I., Foiadelli T., Marseglia G.L., Ciprandi G. Paediatric emergency department visits fell by more than 70% during the COVID-19 lockdown in Northern Italy. Acta Paediatr. 2020 doi: 10.1111/apa.15458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cozzi G., Zanchi C., Giangreco M. The impact of the COVID-19 lockdown in Italy on a pediatric emergency setting. Acta Paediatr. 2020 doi: 10.1111/apa.15454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4:e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benjamini Y., Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289–300. [Google Scholar]
- 15.Farion K.J., Wright M., Zemek R. Understanding low-acuity visits to the pediatric emergency department. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0128927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang H.J., Huang N., Lee C.H., Hsu Y.J., Hsieh C.J., Chou Y.J. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. 2004;94:562–564. doi: 10.2105/ajph.94.4.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sperotto F., Wolfer A., Biban P. Unplanned and medical admissions to pediatric intensive care units significantly decreased during COVID-19 outbreak in Northern Italy. Eur J Pediatr. 2020 doi: 10.1007/s00431-020-03832-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riphagen S., Gomez X., Gonzales-Martinez C., Wilkinson N., Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607–1608. doi: 10.1016/S0140-6736(20)31094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verdoni L., Mazza A., Gervasoni A. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395:1771–1778. doi: 10.1016/S0140-6736(20)31103-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raitio A., Ahonen M., Jääskelä M. Reduced number of pediatric orthopedic trauma requiring operative treatment during COVID-19 restrictions: a nationwide cohort study. Scand J Surg. 2020 doi: 10.1177/1457496920968014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bram J.T., Johnson M.A., Magee L.C. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop. 2020;40:373–379. doi: 10.1097/BPO.0000000000001600. [DOI] [PubMed] [Google Scholar]
- 22.Snapiri O., Danizger C.R., Krause I. Delayed diagnosis of pediatric appendicitis during the COVID-19 pandemic. Acta Paediatr. 2020;109:1672–1676. doi: 10.1111/apa.15376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tam C.F., Cheung K.S., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dann L., Fitzsimons J., Gorman K.M., Hourihane J., Okafor I. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch Dis Child. 2020;105:810–811. doi: 10.1136/archdischild-2020-319654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Tilburg M.A.L., Edlynn E., Maddaloni M., van Kempen K., Dias-Gonzales de Ferris M., Thomas J. High levels of stress due to the SARS-CoV-2 pandemic among parents of children with and without chronic conditions across the USA. Children. 2020;7:193. doi: 10.3390/children7100193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McDonnell T., Nicholson E., Conlon C. Assessing the impact of COVID-19 public health stages on paediatric emergency attendance. Int J Environ Res Public Health. 2020;17:6719. doi: 10.3390/ijerph17186719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Golberstein E., Wen H., Miller B.F. Coronavirus Disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174:819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 28.Arora T., Grey I., Östlundh L., Hubert Lam K.B., Omar O.M., Arnone D. The prevalence of psychological consequences of COVID-19: a systematic review and meta-analysis of observational studies. J Health Psychol. 2020 doi: 10.1177/1359105320966639. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.