Abstract
The current Covid-19 pandemic has already had a definite impact on the daily life of many people worldwide. It has been proposed that people with preexisting medical conditions will be harder hit by the pandemic and the subsequent measures to contain the spread of the disease. In this questionnaire-based, observational study, we aimed to assess the impact of the pandemic on patients with a chronic pain disorder, who are treated at a tertiary multidisciplinary pain center.
Participants rated the impact of the pandemic on their chronic pain disorder using a self-designed questionnaire. Also, participants filled out the regular follow-up questionnaire to assess a chronic pain disorder measuring among other parameters pain intensity, symptoms of depression, anxiety, stress, and pain-related quality of life.
Of 136 eligible patients who presented to our pain center between May 5th and July 17th, 112 agreed to participate in the study (82.4%). Eighty two participants (73.2%) reported a deterioration of the pain disorder using the self-designed questionnaire. The more robust parameters of the regular follow-up questionnaire showed no relevant changes compared to data collected before the pandemic. We were not able to detect any demographic and medical parameters that were clinically relevantly associated with a higher impact of the pandemic.
We conclude that a chronic pain disorder is a relatively stable disease that does not change significantly due to external factors, like the Covid-19 pandemic, even if the subjective impact is perceived to be high.
Keywords: chronic pain, COVID-19, pandemics
1. Introduction
At the beginning of the COVID-19 pandemic, most countries focused on treating patients who contracted COVID-19 and, at the same time, tried to prevent the spread of the disease, using different methods of prevention. Most countries imposed measures that affected daily life, such as restricting person-to-person contacts up to issuing home quarantine orders.[1,2] Health providers prepared for a surge of COVID-19 patients by postponing non-emergency treatments [3] and allocating personnel from non-emergency specialties to other areas, for example, intensive care medicine.[4] Also, patients refrained from going to hospitals, even in medical emergencies, because of the fear of getting infected with COVID-19.[5] Due to these reasons, it was recognized early on, that the COVID-19 pandemic indirectly caused a health crisis among other patients as well, for example, oncological patients,[6] and patients with other chronic diseases.[7] The dangers of social distancing and loneliness have been described for patients suffering from preexisting mental illnesses,[8] and for previously healthy individuals as well.[9] The impact of the COVID-19 pandemic on chronic pain has been addressed: Recommendations for the care of patients suffering from chronic non-malignant pain have been proposed.[10,11] Some authors see the potential for an exacerbation of preexisting chronic pain disorders and an increase in the number of people with chronic pain after the pandemic.[12]
In our interdisciplinary pain center, we had to stop our inpatient multimodal pain treatment program at the end of March. We were also unable to see patients in our outpatient clinic in person from the end of March until the beginning of May. At that point, we started a stepwise reopening of the outpatient clinic over 2 months, with a full reopening in July.
This study aimed to examine the short-term impact of the COVID-19 pandemic and the associated measures on patients with chronic non-malignant pain. Also, we tried to identify predisposing factors for a higher impact of the pandemic in these patients.
2. Methods
2.1. Participants
Our outpatient clinic was closed from March 24th until May 4th 2020 (shutdown period). Due to our medical staff being allocated to other clinical areas, we were not able to offer tale health services. During May, we slowly resumed in-person patient contacts, increasing the number of patients seen in June until the full opening of our clinic on July 1st. We asked all patients who had had previous visits to our clinic before March 24th and who presented to our clinic from May 5th until July 17th to participate in our study. Patients younger than 18 years and patients without sufficient knowledge of the German language were excluded from participation. All patients gave written informed consent. The study was approved by the ethics committee of the University of Regensburg (20-1772_1-101).
2.2. Design/data collection
All participants were asked to fill out 2 questionnaires. The first questionnaire was self-designed to assess the subjective impact of the pandemic by posing nine questions (Impact Q). Answers to questions 1 to 7 were formulated in a Likert scale type with a five-point agreement scale, questions 8 and 9 could be answered with yes or no (Table 1). To assess the subjective overall impact of the pandemic, we calculated a sum score from the answers to questions 1 to 7. We scored the individual answer items on the Likert scale from 1 to 5 (e.g., for Q1, 1 = much higher, 2 = rather higher, 3 = equal, 4 = rather lower, 5 = much lower) resulting in a potential sum score range from 7 to 35.
Table 1.
Questionnaire to assess the impact of the pandemic (ImpactQ).
| Item | Question text | Possible answers |
| Q1 | During the pandemic, I felt the intensity of my pain to be ... | much higher - rather higher - equal - rather lower - much lower |
| Q2 | During the pandemic, my mood was ... | much worse - rather worse - equal - rather better - much better |
| Q3 | During the pandemic, my pain treatment was generally ... | much worse - rather worse - equal - rather better - much better |
| Q4 | During the pandemic, my relationships with other people were ... | much worse - rather worse - equal - rather better - much better |
| Q5 | The experience of the pandemic makes accepting my pain disorder ... | much harder - rather harder - equal - rather easier - much easier |
| Q6 | Because of the experience of the pandemic, the importance of my pain disorder for my life has ... | much increased – rather increased – not changed – rather decreased – much decreased |
| Q7 | Due to the effects of the pandemic, I suspect that the future my pain disorder will be ... | much worse - rather worse - equal - rather better - much better |
| Q8 | Have you tested positive for the novel coronavirus yourself? | yes - no |
| Q9 | Has anyone in your close acquaintance and / or family tested positive for the novel coronavirus? | yes - no |
The second questionnaire was the follow-up questionnaire recommended by the German Pain Society (Deutsche Schmerzgesellschaft e.V.) to use in follow-up visits of patients with chronic pain. It consists of 6 sub-tests that measure different aspects of a chronic pain disorder (Table 2). We regularly ask our patients to fill out this questionnaire on each of their follow-up visits.
Table 2.
Content of the follow-up questionnaire.
| Name of sub-test (Abbreviation) | Measured aspect/Scoring | Reference |
| Von-Korff graduation of pain intensity (PI) | Measures pain intensity. Mean of current, average and highest pain intensity, each rated on an 11-point scale (0–10) multiplied by 10, resulting in a number from 0–100 (0 = no pain, 100 = highest pain intensity). | [31] |
| Von-Korff graduation of pain-related disability (PD) | Measures pain-related disability. Mean of impairment in daily life, leisure activities, and work ability, each rated on an 11-point scale (0 – 10), multiplied with 10, resulting in a number from 0–100 (0 = no disability, 100 = highest disability). | [31] |
| Pain Descriptor List (SBL) | Measures the affective component of pain. Patients rate how four adjectives describing the affective component fit their pain sensation on a 4-point scale (0–3), resulting in a sum of 0–12 (0 = no affective component, 12 = high affective component). | [32] |
| Marburg Questionnaire (FW7) | Measures subjective well-being. Patients rate their affirmation of seven statements concerning well-being on a 6-point scale (0–5), resulting in a sum of 0–35 (0 = no subjective well-being, 35 = highest subjective well-being). | [33] |
| Veterans RAND 12 Item Health Survey (VR-12) | Measures health-related quality of life. Patients rate 12 items. Scores for physical and psychological well-being are calculated (Physical Composite Summary PCS, Mental Composite Summary MCS). Higher scores indicate higher well-being. | [34] |
| Depression Anxiety Stress Scale (DASS) | Measures symptoms of depression (DASS-D), anxiety (DASS-A), and stress (DASS-S). Patients rate their affirmation of twenty one statements with seven statements concerning each subscale on a 4-point scale (0–3), resulting in a sum score of 0–21 for each subscale (0 = no symptoms, 21 = high symptom-load) | [35] |
The results of the 2 questionnaires were entered into an Excel spreadsheet (Excel 2016, Microsoft, Redmond, WA) and then linked to the results of the follow-up questionnaire that were available from the last visit of the patient before the shutdown period of our clinic. Participants’ demographic and medical data were collected from their medical records.
2.3. Data analysis
We used IBM SPSS Statistics 26 (IBM, Armonk, NY) for data analysis. We compared the demographic and medical information of participants and non-participants with a t-test, a Mann–Whitney test, and a Chi-Squared test where appropriate. The results of the follow-up questionnaires before the shutdown period (preQ) to the results of the follow-up questionnaires after the shutdown (postQ) were compared using a paired t-test. To examine the association of the participants’ demographic and medical parameters and the sum score (ImpactQ) and the differences of certain sub-tests of the preQ/postQ, we performed a t-test for nominal, a one-way ANOVA for ordinal data, and calculated Pearson correlation coefficients for interval data. For all tests, a P value <.05 was defined as statistically significant.
3. Results
Participation is shown in Figure 1. Two hundred nine patients presented to our outpatient pain clinic between May 5th and July 17th. One hundred thirty six patients were eligible for participation. Of these, 112 consented to participate in the study (82.4%). These patients answered the ImpactQ and the postQ. Participants and non-participants did not differ statistically significant in most of their demographic and medical parameters (Table 3). For 98 of the participants, preQ questionnaires were available from previous visits (87.5%). Scoring the answer items on the Likert scale from 1–5 (e.g., for Q1, 1 = much higher, 2 = rather higher, 3 = equal, 4 = rather lower, 5 = much lower) we found that the mean of all answers for Q1-Q7 was below 3 (Table 4). When calculating the sum scores of Q1-Q7, 82 participants (73.2%) scored less than 21 points (result if all items had been rated as unchanged), 25 (22.3%) scored 21 points, and 5 (4.5%) more than 21 points (Fig. 2). The mean sum score was 17.3 (SD 3.9). One patient reported that he had been tested positive for the novel coronavirus (Q8), and 10 had close relatives or acquaintances who had tested positive (Q9). Comparing the preQ and postQ results, we observed only small changes in all sub-tests, none of which reached a level of statistical significance (Table 5). We examined the association of the participants’ demographic and medical parameters with the sum score of the Impact Q and the differences of the sub-tests Von-Korff graduation of pain intensity (PI), Physical Composite Summary (PCS), and Mental Composite Summary (MCS) from the preQ and postQ. We found 3 statistically significant associations (Table 6). Participants taking opioid medications had a mean reduction of PI of 4.3 points from preQ to postQ, while participants without opioid medication had an increase of PI of 4.5 points. Education at the university level was associated with an increase of MCS of 5.7 points, education on high school level with a reduction of 0.5 points. Participants living in a household with underaged children showed an increase in PCS of 4.0 points, those living without underaged children had a reduction of 1.4 points.
Figure 1.
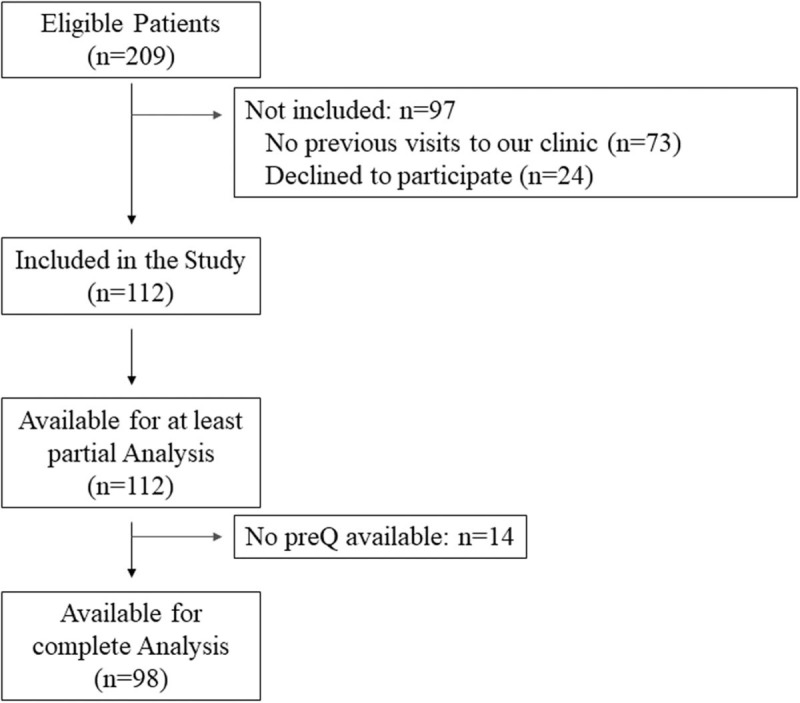
Flow diagram of participation.
Table 3.
Demographic and medical parameters of all eligible patients.
| Participants (N = 112) | Nonparticipants (N = 24) | Group comparison (P value)∗ | |
| Age in years, mean (SD) | 55.0 (13.1) | 56.3 (17.1) | .735 |
| Gender | |||
| Female, N (%) | 77 (69%) | 17 (71%) | .841 |
| Male, N (%) | 35 (31%) | 7 (29%) | |
| Years since onset of the pain disorder, mean (SD) | 15.0 (12.4) | 11.7 (11.7) | .224 |
| Years being treated at our tertiary pain center, mean (SD) | 4.0 (3.8) | 3.9 (3.0) | .735 |
| Additional psychiatric diagnosis, N (%)† | |||
| -Affective disorder | 63 (56%) | 8 (33%) | .041 |
| -Anxiety disorder | 18 (16%) | 3 (13%) | .660 |
| -Other | 27 (24%) | 5 (21%) | .732 |
| Opioid medication, N (%) | 38 (34%) | 8 (33%) | .955 |
| Previous intensive multidisciplinary pain treatment | 62 (55%) | 10 (42%) | .223 |
| Currently employed, N (%) | 44 (39%) | 9 (38%) | .871 |
| Highest education, N (%) | |||
| -No education | 0 | 0 | .226 |
| -High school | 99 (88%) | 19 (79%) | |
| -University | 13 (12%) | 5 (21%) | |
| Lives with a partner, N (%) | 75 (67%) | 14 (58%) | .420 |
| Lives with under aged children, N (%) | 22 (20%) | 4 (17%) | .737 |
| Place of residence‡, N (%) | |||
| -City | 30 (27%) | 6 (25%) | .494 |
| -Town | 23 (21%) | 3 (13%) | |
| -Rural | 59 (53%) | 15 (63%) | |
Significant differences in BOLD.
More than one diagnosis possible.
City >100,000 inhabitants, Town 10,000–99,999 inhabitants, Rural <10,000 inhabitants, classification adapted from[36].
Table 4.
Results of the ImpactQ.
| Rating, N (%)∗ | ||||||
| Question (n) | much higher (1) | rather higher (2) | equal (3) | rather lower (4) | much lower (5) | Mean† (SD) |
| During the pandemic, I felt the intensity of my pain to be ... (112) | 11 (9.8%) | 38 (33.9%) | 59 (52.7%) | 3 (2.7%) | 1 (0.9%) | 2.51 (0.747) |
| much worse (1) | rather worse (2) | equal (3) | rather better (4) | much better (5) | ||
| During the pandemic, my mood was ... (112) | 16 (14.3%) | 50 (44.6%) | 42 (37.5%) | 2 (1.8%) | 2 (1.8%) | 2.32 (0.808) |
| During the pandemic, my pain treatment was generally ... (109) | 19 (17.4%) | 35 (32.1%) | 52 (47.7%) | 3 (2.8&) | 0 (0%) | 2.36 (0.800) |
| During the pandemic, my relationships with other people were ... (112) | 21 (18.8%) | 44 (39.3%) | 41 (36.6%) | 6 (5.4%) | 0 (0%) | 2.29 (0.832) |
| much harder (1) | rather harder (2) | equal (3) | rather easier (4) | much easier (5) | ||
| The experience of the pandemic makes accepting my pain disorder ... (112) | 5 (4.5%) | 26 (23.2%) | 76 (67.9%) | 5 (4.5%) | 0 (0%) | 2.72 (0.618) |
| much increased (1) | rather increased (2) | equal (3) | rather decreased (4) | much decreased (5) | ||
| Because of the experience of the pandemic, the importance of my pain disorder for my life has ... (112) | 10 (8.9%) | 29 (25.9%) | 69 (61.6%) | 3 (2.7%) | 1 (0.9%) | 2.61 (0.727) |
| much worse (1) | rather worse (2) | equal (3) | rather better (4) | much better (5) | ||
| Due to the effects of the pandemic, I suspect that the future my pain disorder will be ... (111) | 11 (9.9%) | 28 (20.6%) | 70 (51.5%) | 2 (1.5%) | 0 (0%) | 2.57 (0.696) |
The most frequently selected answer is shown in bold.
Each rating on the Likert-Scale was awarded a score from 1 to 5. Mean was calculated from these scores.
Figure 2.
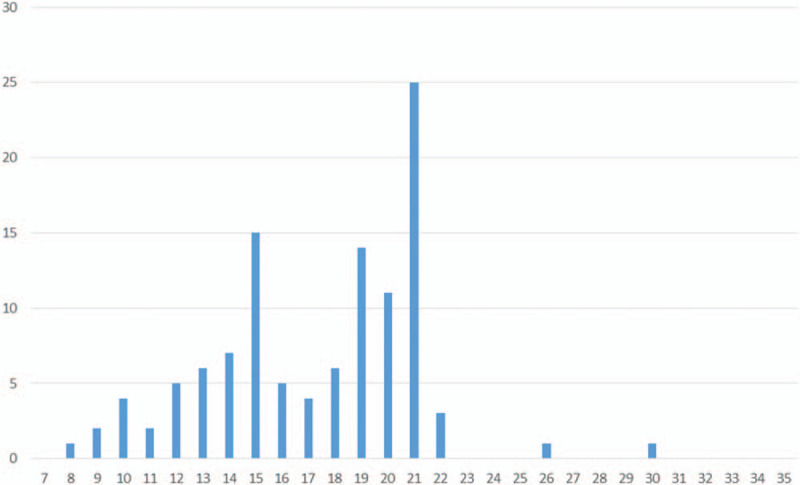
Display of the distribution of sum scores of the ImpactQ.
Table 5.
Comparison of preQ and postQ results for participants who had filled out both questionnaires∗.
| Sub-test † (N) | Result preQ | Result postQ | Difference preQ - postQ | Comparison (P value) |
| PI (92) | 63.4 (16.8) | 64.9 (17.3) | -1.5 | .345 |
| PD (89) | 57.5 (20.4) | 58.9 (23.1) | -1.4 | .478 |
| SBL (98) | 4.3 (3.6) | 4.2 (3.7) | 0.1 | .795 |
| FW7 (98) | 13.6 (8.1) | 13.8 (8.5) | -0.2 | .806 |
| VR-12, PCS (98) | 30.6 (8.8) | 30.3 (9.4) | 0.3 | .722 |
| VR-12, MCS (98) | 33.5 (8.7) | 33.7 (7.8) | -0.2 | .862 |
| DASS-D (98) | 8.7 (5.6) | 8.7 (6.3) | 0 | .967 |
| DASS-A (98) | 6.4 (4.8) | 6.3 (4.9) | 0.1 | .769 |
| DASS-S (98) | 10.4 (5.3) | 10.1 (5.7) | 0.3 | .586 |
Data given in mean (SD).
PI = Von-Korff graduation of pain intensity, PD = Von-Korff graduation of pain related disability, SBL = Pain Descriptor List, FW7 = Marburg Questionnaire, VR-12 = Veterans RAND 12 Item Health Survey, PCS = Physical Composite Summary, MCS = Mental Composite Summary, DASS = Depression Anxiety Stress Scale.
Table 6.
Levels of statistical significance for the comparison/correlation of demographic and medical parameters with test results∗.
| Parameters | Sumscore (P value) | PI preQ-postQ (P value) | PCS preQ-postQ (P value) | MCS preQ-postQ (P value) |
| Nominal data (T-test) | ||||
| Gender | .276 | .793 | .904 | .908 |
| Affective disorder | .529 | .931 | .680 | .373 |
| Anxiety disorder | .098 | .052 | .535 | .893 |
| Other psychiatric disorder | .968 | .203 | .560 | .972 |
| Opioid medication | .473 | .009 | .885 | .705 |
| Previous intensive multidisciplinary pain treatment | .973 | .163 | .564 | .154 |
| Currently employed | .161 | .817 | .161 | .510 |
| Highest education | .983 | .207 | .284 | .038 |
| Lives with a partner | .590 | .971 | .511 | .817 |
| Lives with under aged children | .479 | .207 | .011 | .514 |
| Ordinal data (one-way ANOVA) | ||||
| Place of residence | .050 | .128 | .782 | .550 |
| Metric data (Pearson correlation coefficient) | ||||
| Age | .887 | .848 | .808 | .785 |
| Years since onset of the pain disorder | .706 | .646 | .660 | .534 |
| Years being treated at our tertiary pain center | .454 | .695 | .947 | .144 |
Statistically significant results in BOLD.
4. Discussion
In this study, we aimed to determine the short-term impact of the COVID-19 pandemic on patients with a chronic pain disorder. There is no validated tool for measuring the impact of a health crisis on any group of patients, therefore we self-designed the ImpactQ. We understand this questionnaire as a general measuring instrument of the subjective impression of the pandemic on each individual. We also evaluated whether the experience of the pandemic led to any change in our follow-up questionnaire. While this questionnaire does not cover all outcome domains that are currently discussed as relevant for the assessment of chronic pain,[13] it has been used in our pain center for many years and is recommended for use by the German Pain Society until further notice.
We were able to include 112 of 136 eligible patients in this study. Considering the high participation rate, although there was 1 statistically significant difference between participants and non-participants, we assume that the participants are a representative sample of our patients in general. The participants’ characteristics show similarities concerning age, gender prevalence, and duration of the chronic pain disorder to the patients of other tertiary multidisciplinary pain centers.[14–16]
Looking at the results of the ImpactQ, the answers to items Q1-Q7 all shift on average towards deterioration. The item Q4 (social relationships) was rated the lowest. The risk of losing social contacts during the pandemic with a subsequent negative impact on well-being has already been mentioned.[17] Also, the availability of pain therapy was rated as rather worse. Although not systematically analyzed, many patients mentioned the lack of exercise therapy/physiotherapy as an important reason for an increase in pain intensity. When dealing with the pandemic and subsequent measures in the future, we feel that it would be important to enable patients to continue exercise therapy/physiotherapy, maybe even in a group under the strict following of hygienic rules to sustain social contacts, especially since physical activity has been shown to have a positive impact on psychological health during the pandemic.[18] While the construction of a sum score out of Likert scale items can be viewed critically, some authors think this is possible if the single items are rated equally and the distance between the single scores is visualized with equal lengths (as we did in the ImpactQ).[19]
Almost 3/4 of participants had a sum score <21, indicating an over-all shift in the direction of deterioration. Interestingly, this deterioration was not evident in the differences between preQ and postQ. The sub-tests of the follow-up questionnaire seem to be more robust towards changes or adverse events than the ImpactQ. Our study encompassed patients with a high degree of chronification, typical for a tertiary pain center. We assume that in these patients, the chronic pain disorder represents a rather stable disease not easily influenced in its trajectory while at the same time, the subjective impact of external factors is felt to be high. A stable disease trajectory in terms of persistent pain intensity levels over time has been shown in chronic pain patients in previous studies,[20,21] complying with our results. In another study, patients with fibromyalgia-like pain reported no relevant changes after the 9/11 attacks in New York in 2002,[22] suggesting that the effect of major events on individual health might not be as high as expected.
We saw only a few patients with improved test results (either ImpactQ or postQ/preQ difference). It seems that the pandemic has not caused a positive change after adversity, as described by some studies under different adverse events.[23] One could have expected that the experience of the pandemic would shift attention from personal problems (i.e., pain disorder) towards greater social challenges (i.e., Covid-19 pandemic) and coping thereof. We found no evidence for this mechanism in our study, with only 5 participants feeling an increased acceptance of their pain disorder (Q5) and 4 participants seeing less importance of their pain disorder for their life (Q6).
The analysis of parameters associated with changes in selected test results showed an inconclusive pattern. While some parameters were associated with differences, the clinical relevance is rather low. For example, the intake of opioid medication led to a reduction of PI of 4.3 points on a 101-point scale. While there is no established minimally clinically important difference for PI, it can be deducted from other studies that it should be at least 10 points.[24] Also, the changes in MCS and PCS for participants with a university education (5.7 points increase) and living with under aged children (4.0 points increase) respectively barely reached the minimally clinically important difference published for these components of the VR-12.[25]
We believe that based on these results, it is not justified to identify any parameters as having a relevant association with the impact of the pandemic in patients with a chronic pain disorder. Consequently, they cannot be used to define populations at risk of a higher negative impact of the pandemic. This differs from the results of another study that had identified women, young people and people living with preschool-aged children to be at risk of developing future mental illnesses. [26]
There are some limitations in this study. The study has been conducted at a single-center with a selected group of patients, reducing the generalizability of the results. Also, the direct impact of the pandemic on health systems worldwide has been very different, with different closure times at different medical institutions. We still feel that our results can be transferred to other treatment facilities since the measures undertaken to reduce the spread of Covid-19 were quite strict in our area and resemble those of other regions. Since there is no validated tool to measure the impact of a pandemic, we had to rely on a self-designed non-validated questionnaire as other researchers have done as well.[27,28] We felt that validated questionnaires to assess the impact of a traumatic experience, as the Impact of Event Scale,[29] were not useful for our purpose since they usually focus on the symptoms of a posttraumatic stress disorder. We were not able to form a control group since the ImpactQ and the preQ/postQ are focused on patients with chronic pain and therefore not applicable to a normal cohort. Finally, we only examined the short-term impact of the Covid-19 pandemic. While most patients experience symptoms close to traumatic events, some patients have a delayed onset of symptoms.[30] To identify these patients, repeated surveys at greater intervals would be necessary.
In conclusion, we could show that the short term impact of the Covid-19 pandemic was rated as high by patients with a chronic pain disorder on a subjective scale. At the same time, more robust measuring tools for chronic pain showed a stable disease trajectory. We were not able to identify demographic or medical parameters that had a relevant association with the impact of the pandemic. We think that to reduce the (subjective) impact of the Covid-19 pandemic, treatment facilities should offer as much therapeutic content and keep contact to the patients as possible while maintaining safety measures to reduce the risk of infection.
Acknowledgments
The authors would like to thank Anja Kretschmann, Susanne Weber, Melanie Schreiner-Pinkert, and Kai Meyer for data imputation.
Author contributions
Conceptualization: Christoph Lassen, Laila Siam, Tobias W. Klier, Anika Bundscherer, Nicole Lindenberg.
Data curation: Laila Siam, Astrid Degenhart, Nicole Lindenberg.
Formal analysis: Christoph Lassen, Laila Siam, Astrid Degenhart, Tobias W. Klier, Anika Bundscherer, Nicole Lindenberg.
Methodology: Christoph Lassen, Tobias W. Klier, Anika Bundscherer, Nicole Lindenberg.
Supervision: Nicole Lindenberg.
Writing – original draft: Christoph Lassen.
Writing – review & editing: Laila Siam, Astrid Degenhart, Tobias W. Klier, Anika Bundscherer, Nicole Lindenberg.
Footnotes
Abbreviations: MCS = Mental Composite Summary, PCS = Physical Composite Summary, PI = Von-Korff graduation of pain intensity.
How to cite this article: Lassen CL, Siam L, Degenhart A, Klier TW, Bundscherer A, Lindenberg N. Short-term impact of the COVID-19 pandemic on patients with a chronic pain disorder. Medicine. 2021;100:10(e25153).
This work was solely funded by institutional sources.
The authors have no conflict of interest to declare.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Pan A, Liu L, Wang C, et al. Association of Public Health Interventions with the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 2020;323:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Parmet WE, Sinha MS. Covid-19 - the law and limits of quarantine. N Engl J Med 2020;382:e28.doi:10 1056/. [DOI] [PubMed] [Google Scholar]
- [3].American College of Surgeons. COVID-19: recommendations for management of elective surgical procedures. https://www.facs.org/covid-19/clinical-guidance/elective-surgery. Updated 2020 Mar 13. Accessed 2020 Jun 28. [Google Scholar]
- [4].Dunn M, Sheehan M, Hordern J, et al. ’Your country needs you’: the ethics of allocating staff to high-risk clinical roles in the management of patients with COVID-19. J Med Ethics 2020;46:436–40. doi:10.1136/medethics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Mantica G, Riccardi N, Terrone C, et al. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health 2020;183:40–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].van de Haar J, Hoes LR, Coles CE, et al. Caring for patients with cancer in the COVID-19 era. Nat Med 2020;26:665–71. [DOI] [PubMed] [Google Scholar]
- [7].Boettler T, Newsome PN, Mondelli MU, et al. Care of patients with liver disease during the COVID-19 pandemic: EASL-ESCMID position paper. JHEP Rep 2020;2:100113.doi:10.1016/j.jhepr.2020.100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chatterjee SS, Barikar CM, Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian J Psychiatr 2020;51:102071.doi:10.1016/j.ajp.2020.102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hiremath P, Suhas Kowshik CS, Manjunath M, et al. COVID 19: Impact of lock-down on mental health and tips to overcome. Asian J Psychiatr 2020;51:102088.doi:10.1016/j.ajp.2020.102088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cohen SP, Baber ZB, Buvanendran A, et al. Pain management best practices from multispecialty organizations during the COVID-19 pandemic and public health crises. Pain Med 2020;21:1331–46. doi:10.1093/pm/pnaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Coluzzi F, Marinangeli F, Pergolizzi J. Managing chronic pain patients at the time of COVID-19 pandemic. Minerva Anestesiol 2020;86:797–9. [DOI] [PubMed] [Google Scholar]
- [12].Clauw DJ, Häuser W, Cohen SP, et al. Considering the potential for an increase in chronic pain after the COVID-19 pandemic. Pain 2020;161:1694–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kaiser U, Kopkow C, Deckert S, et al. Developing a core outcome domain set to assessing effectiveness of interdisciplinary multimodal pain therapy: the VAPAIN consensus statement on core outcome domains. Pain 2018;159:673–83. [DOI] [PubMed] [Google Scholar]
- [14].Brain K, Burrows T, Rollo ME, et al. Population characteristics in a tertiary pain service cohort experiencing chronic non-cancer pain: weight status, comorbidities, and patient goals. Healthcare (Basel) 2017;5: doi:10.3390/healthcare5020028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Stedenfeldt M, Kvarstein G, Nilsen TIL, et al. Pre-consultation biopsychosocial data from patients admitted for management at pain centers in Norway. Scand J Pain 2020;20:363–73. [DOI] [PubMed] [Google Scholar]
- [16].Hooten WM, Townsend CO, Bruce BK, et al. Sex differences in characteristics of smokers with chronic pain undergoing multidisciplinary pain rehabilitation. Pain Med 2009;10:1416–25. [DOI] [PubMed] [Google Scholar]
- [17].Tull MT, Edmonds KA, Scamaldo KM, et al. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res 2020;289:113098.doi:10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Maugeri G, Castrogiovanni P, Battaglia G, et al. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020;6:e04315.doi:10.1016/j.heliyon.2020.e04315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Völkl K, Korb C. Deskriptive Statistik: Eine Einführung für Politikwissenschaftlerinnen und Politikwissenschaftler. 1. Auflage 2018. Wiesbaden: Springer Fachmedien Wiesbaden; 2018. Elemente der Politik. [Google Scholar]
- [20].Tamcan O, Mannion AF, Eisenring C, et al. The course of chronic and recurrent low back pain in the general population. Pain 2010;150:451–7. [DOI] [PubMed] [Google Scholar]
- [21].Glette M, Stiles TC, Borchgrevink PC, et al. The natural course of chronic pain in a general population: stability and change in an eight-wave longitudinal study over four years (the HUNT Pain Study). J Pain 2020;21:689–99. [DOI] [PubMed] [Google Scholar]
- [22].Raphael KG, Natelson BH, Janal MN, et al. A community-based survey of fibromyalgia-like pain complaints following the World Trade Center terrorist attacks. Pain 2002;100:131–9. [DOI] [PubMed] [Google Scholar]
- [23].Linley PA, Joseph S. Positive change following trauma and adversity: a review. J Trauma Stress 2004;17:11–21. [DOI] [PubMed] [Google Scholar]
- [24].Salaffi F, Stancati A, Silvestri CA, et al. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain 2004;8:283–91. [DOI] [PubMed] [Google Scholar]
- [25].Kronzer VL, Jerry MR, Ben Abdallah A, et al. Changes in quality of life after elective surgery: an observational study comparing two measures. Qual Life Res 2017;26:2093–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020;7:883–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Antony A, Connelly K, Silva T de, et al. Perspectives of patients with rheumatic diseases in the early phase of COVID-19. Arthritis Care Res (Hoboken) 2020;72:1189–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Grunert PC, Reuken PA, Stallhofer J, et al. Inflammatory Bowel Disease in the COVID-19 Pandemic - the Patients’ Perspective. J Crohns Colitis 2020;doi:10.1093/ecco-jcc/jjaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther 2003;41:1489–96. [DOI] [PubMed] [Google Scholar]
- [30].Smid GE, Mooren TT, van dMR, et al. Delayed posttraumatic stress disorder: systematic review, meta-analysis, and meta-regression analysis of prospective studies. J Clin Psychiatry 2009;70: doi:10.4088/JCP.08r04484. [DOI] [PubMed] [Google Scholar]
- [31].von Korff M, Ormel J, Keefe FJ, et al. Grading the severity of chronic pain. Pain 1992;50:133–49. [DOI] [PubMed] [Google Scholar]
- [32].Korb J, Pfingsten M. Der Deutsche Schmerzfragebogen - Implementierte Psychometrie. Schmerz 2003;17:S47. [Google Scholar]
- [33].Basler HD. Marburger Fragebogen zum habituellen Wohlbefinden. Untersuchung an Patienten mit chronischem Schmerz. Schmerz 1993;13:385–91. [DOI] [PubMed] [Google Scholar]
- [34].Kazis LE, Selim A, Rogers W, et al. Dissemination of methods and results from the veterans health study: final comments and implications for future monitoring strategies within and outside the veterans healthcare system. J Ambul Care Manage 2006;29:310–9. [DOI] [PubMed] [Google Scholar]
- [35].Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 1995;33:335–43. [DOI] [PubMed] [Google Scholar]
- [36].Lederbogen F, Kirsch P, Haddad L, et al. City living and urban upbringing affect neural social stress processing in humans. Nature 2011;474:498–501. [DOI] [PubMed] [Google Scholar]


