Abstract
Background:
Ankle fusion is the primary treatment for advanced ankle arthritis. With the advancement of arthroscopy technology, ankle arthroscopy fusion has shown many advantages over traditional surgery. However, there are few related studies globally, and evidence-based medicine is needed to verify the reliability and feasibility of ankle arthroscopy fusion.
Objective:
To compare the clinical efficacy and safety of arthroscopic ankle arthrodesis and open ankle arthrodesis.
Methods:
We searched the databases of PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure [CNKI], Wanfang Database, and VIP Database for published prospective or retrospective controlled studies of arthroscopic-assisted ankle fusion in the treatment of advanced ankle arthritis. The dates were limited from the construction of the library to June 30, 2019. Literature was included based on the principles and methods of evidence-based medicine. Literature retrieval, data extraction, and quality assessment were performed by 2 independent reviewers using the Cochrane 5.1 risk bias assessment tool. The methodological bias of the literature was evaluated, and a meta-analysis was using by RevMan 5.3 software.
Results:
A total of 18 studies and 1102 patients were included in the study, including 551 in the arthroscopic surgery group and 551 in the open surgery group. Arthroscopy-assisted surgery for advanced ankle arthritis was more effective than open surgery in terms of fusion rate (odd ratio[OR] = 3.32, 95% confidence interval[CI]:2.16, 5.10), fusion time (mean difference[MD] = −2.31, 95% CI:−4.63, −2.21), intraoperative blood loss (MD = −43.37, 95%CI: −48.49, −38.25), hospital stay (MD = −1.80, 95%CI: −2.28, −1.33), and visual analog scale score (MD = −1.75, 95%CI: −2.04, −1.46). In addition, rate of complications (OR = 0.33, 95%CI: 0.21, 0.52) was superior to open ankle fusion (P < .00001).
Conclusion:
Arthroscopic ankle arthrodesis has more advantages than open ankle arthrodesis in improving the fusion rate and reducing complications, which is worthy of clinical application.
PROSPERO registration number:
CRD42020195727.
Keywords: advanced ankle arthritis, ankle joint, arthroscopy, fusion, open
1. Introduction
The main manifestations of advanced ankle osteoarthritis are mainly painful walking and severely restricted ankle motion, which seriously affect the patient's quality of life.[1] In contrast to hip arthritis and knee arthritis, ankle osteoarthritis is mainly caused by trauma, accounting for 76% to 78% of all ankle joint diseases. Primary osteoarthritis accounts for only 7% to 9% of cases.[2] Secondary osteoarthritis accounts for 12% to 13% of cases, including rheumatoid arthritis, neuropathic joint disease, pigmentation and postinfection lesions.[3] Advanced ankle osteoarthritis is a common clinical chronic degenerative disease. It is characterized by cartilage degeneration, subchondral osteosclerosis, periarticular osteophyte formation and joint deformity. The main manifestations are chronic pain and joint deformities. The effect of nonsurgical treatment of advanced ankle osteoarthritis is often poor, and surgical treatment methods are diverse. Therefore, individualized treatment is required according to the patient's condition.
Ankle arthrodesis was proposed in 1879, and most scholars still believe that it is the first choice to relieve pain and improve ankle mobility.[4] Ankle fusion is the most reliable way to treat end-stage ankle osteoarthritis. However it may cause complications, such as abnormal movement, gait changes, and adjacent joint arthritis after surgery. In recent years, foreign foot and ankle surgeons have increasingly used ankle fusion surgery to restore the foot and ankle line of force and reconstruct serious deformities, such as the middle rear foot and ankle with poor results of nonsurgical treatment. According to reported, 50% of osteoarthritis patients undergoing ankle fusion will develop arthritis around the hindfoot 7 to 8 years after surgery.[5] After ankle arthrodesis, patients have difficulty walking on uneven roads and long-time activity may cause pain, and increase the contact stress of the talocalcaneal joint and the calcaneocuboid joint. Patients will lose 74% of the sagittal range of motion, 70% of the rotational range of motion, and 77% of the valgus range of motion after ankle fusion. However, the treatment effect is reliable, and more than 90% of the patients are satisfied with the treatment results.[6] Most scholars believe that the best fixed position of the ankle joint a valgus of 5°–8°, external rotation of 5°–10°, neutral back extension and backward offset about 5 mm to increase calcaneal torque.[7]
Currently, ankle fusion is still the gold standard for the treatment of end-stage ankle arthritis, and open ankle fusion are the 2 main and mature surgical methods.[8,9] Before the development of arthroscopic technology, open ankle fusion has been the standard operation for the treatment of advanced ankle arthritis, but the traditional open ankle fusion has potential disadvantages of large trauma, hemorrhage, slow healing and long bone fusion, so the clinical efficacy is affected to a certain extent.[10] With the progress of being minimally invasive techniques, arthroscopic assisted ankle fusion has obvious therapeutic effects, and has the advantages of minimally invasive injury, high fusion efficiency, and quick postoperative recovery.[11,12] Currently, there is a lack of systematic research on the clinical application of these 2 methods for the treatment of advanced ankle arthritis. We aimed to conduct a systematic review using the Cochrane systematic review method. Under the guidance of evidence-based medicine theory, the relevant literature was screened and analyzed to compare the efficacy of arthroscopic and open ankle fusion in the treatment of advanced ankle arthritis, so as to provide clinicians with reference and evidence-based medicine in the treatment of advanced ankle arthritis.
2. Materials and methods
This study is a literature study and does not require the consent of the patient or the approval of the ethics committee. This protocol has been registered on the International Prospective Register of Systematic Reviews (registration no.CRD42020195727).
2.1. Literature research
Search Scope: search CNKI Database, Wanfang Database, VIP Database, PubMed, Embase, and Cochrane Library. The temporal interval is limited from the time that the databases created to June 30, 2019, searching for completed documents A randomized controlled trial (RCT) or retrospective case-control study (RCS) of arthroscopic assisted ankle fusion in the treatment of advanced ankle arthritis. The search terms include “ankle joint,” “arthrodesis,” “arthroscopy,” “minimally invasive,” etc., and the combination of keyword and free word retrieval is adopted. Retrieval formula is #1 arthroscopic OR minimally invasive; #2 ankle joint; #3 fusion surgery; #4 #1 AND #2 AND#3.
2.2. Inclusion criteria and exclusion criteria
Inclusion criteria:
-
1.
Study type: RCT or RCS;
-
2.
objects of study: all are clinical studies of advanced ankle arthritis;
-
3.
study method: the experimental group is arthroscopic assisted ankle arthrodesis, and the control group is open ankle arthrodesis.
-
4.
Outcome indicators: operation time, intraoperative blood loss, hospital stay, AOFAS score, fusion rate, fusion time, VAS score, Kofoed score, complications, Harris score.
Exclusion criteria:
-
1.
nonclinical RCT or RCS, basic research, nonChinese and English literature;
-
2.
incomplete or inconsistent data, repeated publication;
-
3.
documents with improper statistical methods or unable to perform statistical analysis;
-
4.
the Data that lack of corresponding outcome indicators, the literature that lack of commercial evaluation.
2.3. Literature screening and quality evaluation
According to the Cochrane Handbook 5.1 operating specifications, 2 literature reviewers selected the retrieved documents in accordance with the inclusion and exclusion criteria, and included qualified documents. The unqualified literatures were gradually eliminated and the qualified ones were included. The results were cross checked. Separate data extraction for the finally included literature. If there is disagreement, the third researcher will participate in the discussion and negotiate a decision. If necessary, you can contact the author of the literature to clarify the relevant information of the study. The data of authors, title, operation time, intraoperative blood loss, hospitalization time, AOFAS score, fusion rate, fusion time, VAS score, complications were mainly extracted. The quality evaluation criteria of Cochrane Handbook 5.1 were used to evaluate the methodological quality of the included literatures and assess the risk of bias in the included literature, including the generation of random sequences, allocation concealment, blinding of participants and related personnel, blinding of evaluators, incomplete results data, selective reporting of results, and other sources of bias.
2.4. Data synthesis and statistical analysis
The Revman 5.3 software provided by Cochrane Collaboration Network was used for analysis. The data were analyzed by heterogeneity test and meta-analysis. In this study, fixed effect model or random effect model was used to analyze the data. Statistical heterogeneity was tested by Q test. P > .05 or I2 < 50% believed that there was no significant statistical heterogeneity among the studies. A fixed-effect model was used to combine data; if P < .05 or I2 > 50% thought that there was significant statistical heterogeneity among them, the random effect model was selected. P < .05 was regarded as a statistically significant criterion. The combined results of counting data were expressed as odds ratio (OR). The continuous variables were combined with mean difference (MD) statistics, and 95% confidence interval (CI) was given.
2.5. Risk of bias
The Cochrane systematic evaluation bias risk assessment tool was used to evaluate the quality of the included literature, including the following 7 aspects:
-
1.
whether the random sequence was generated sufficiently;
-
2.
whether the allocation was hidden;
-
3.
whether the blind intervention was adopted;
-
4.
whether the blind method was used;
-
5.
whether there was selective reporting;
-
6.
whether there was publication bias; and
-
7.
whether there were other biases.
2.6. Outcome measures
We finally selected 6 indicators that appear frequently in the article for meta-analysis. Fusion rate, operation time, hospital stay, AOFAS score, complications were the main outcome measure, and the secondary outcome measures were fusion time, intraoperative blood loss, and VAS score.
2.7. Grading the quality of evidence
We use Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method to assess the quality of the evidence included in the systematic review. According to the difference in the quality of evidence, it can be divided into 4 levels: high/medium/low/very low. All operations are on this page: https://gradepro.org/.
3. Results
3.1. Basic characteristics of included literature
According to the method of literature retrieval, 4760 articles were obtained through the database, including CNKI (929 articles), Wanfang database (545 articles), VIP database (262 articles), PubMed (1326 articles), Embase (1623 articles), Cochrane (75 articles). After inputting them into EndNote X8 software, 1975 repetitive literatures were excluded through the software's system check function and 2785 articles were left. By reading the titles and abstracts of the literatures, the articles not related to arthroscopic or open ankle arthrodesis were excluded, including 345 reviews, 532 systematic reviews, 442 meta-analyses, 735 case reports and 662 unrelated studies. A total of 2761 articles were excluded and the remaining 69 were left. By reading the full text in the remaining documents, 46 uncontrolled studies were excluded, and the remaining 23 articles. After intensive reading of the documents, 5 documents different from other documents were excluded, and 18 documents were included.[13–30] Finally, 18 articles and 1102 patients were included, including 551 in the arthroscopic surgery group and 551 in the open surgery group (Table 1). The results of the included literature quality evaluation and risk evaluation are shown in Figure 1.
Table 1.
Specific situation of included literatures.
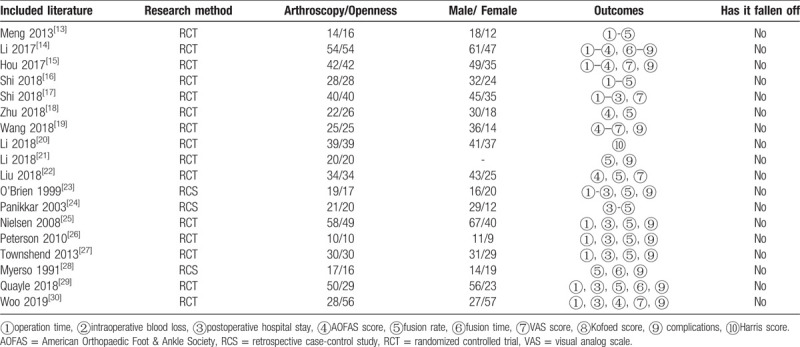
Figure 1.
Results of bias risk assessment included in randomized controlled trials.
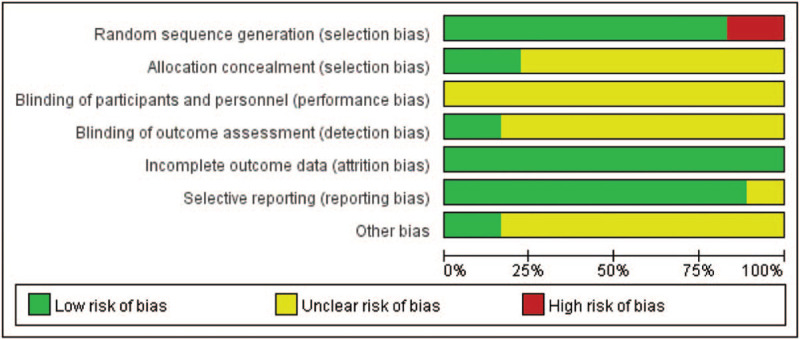
3.2. Risk of bias
The quality evaluation and risk evaluation results of the included literature are shown in Figure 2.15 included literatures belonged to RCTs.[13,14–22,25–27,29,30] Ten of them used random number table method to generate random numbers,[13,14–22] and 5 of them used computers to generate control and experimental groups.[13,14–22] Three included literatures belonged to RCS.[23,24,28] Four studies used the method of allocation concealment,[26,27,29,30] and other studies did not specify it. All studies did not specify the use of blinding. Selective reporting was difficult to assess, and trial protocols were unavailable.
3.3. Meta-analysis results
3.3.1. Fusion rate
Fusion rate: Thirteen studies[13,16,18,19,21–29] included in the literature compared the clinical efficacy of arthroscopic surgery with that of open surgery in terms of postoperative fusion rate for patients with advanced ankle arthritis. A total of 666 cases were included, including 351 in the arthroscopic surgery group and 315 in the open surgery group. Heterogeneity analysis showed that 13 studies had mild heterogeneity (P = .11, I2 = 35%); hence, a fixed effects model was used for statistical analysis. Meta-analysis results showed that the difference in fusion rate was statistically significant (odds ratio [OR] = 3.32, 95% confidence interval [CI]: 2.16–5.10, P < .00001, Z = 5.49); 4 articles were included in the fusion time studies[14,15,19,29] encompassing 321 cases (150 cases in the arthroscopic surgery group and 171 cases in the open surgery group). There was significant heterogeneity among the 4 included studies (P = .006, I2 = 80%), therefore, the random effect model was used for meta-analysis. The results showed: MD = −2.31, 95%CI: −4.63 to −2.21, P < .00001, Z = 6.22; there were significant differences in the fusion rate and fusion time between the arthroscopic surgery and open surgery groups in the treatment of advanced ankle arthritis (Fig. 2).
Figure 2.
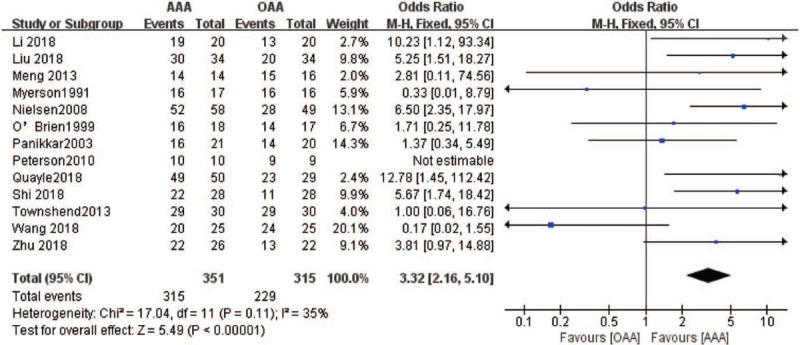
Forest diagram of fusion rate.
3.3.2. Operation time
Nine studies[13–17,26,27,29,30] compared the operation times of the 2 methods. A total of 650 patients were included (316 in the arthroscopic surgery group and 334 in the open surgery group). There was significant heterogeneity among the 9 studies (P < .00001, I2 = 99%), and the random-effects model was used for meta-analysis. The results showed that there was no statistically significant difference in the operation time between the arthroscopic and open surgery groups (MD = −8.54, 95%CI: −23.08 to 6.01, P = 025, Z = 1.15) (Fig. 3).
Figure 3.
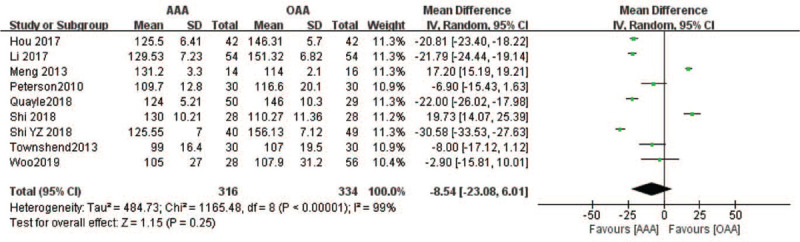
Forest diagram of operation time.
3.3.3. Intraoperative blood loss and hospital stay
Five articles[13–17] evaluated the amount of intraoperative blood loss in the 2 groups. A total of 358 cases were included (178 and 180 cases in the arthroscopic and open surgery groups, respectively). There was significant heterogeneity in the heterogeneity analysis of the 5 studies (P < .00001, I2 = 96%), and the random-effects model was used for statistical analysis. The results showed: MD = −43.37, 95%CI: −48.49 to −38.25, P < .00001, and Z = 16.59. Nine articles[13–17,26,27,29,30] evaluated the 2 methods by comparing the length of hospital stay. A total of 601 cases were included, including 296 and 305 cases in the arthroscopic and open surgery groups, respectively. There was significant heterogeneity in the heterogeneity analysis of these 9 studies (P = .008, I2 = 61%), and the fixed-effects model was used for statistical analysis. The results showed: MD = −1.80, 95%CI: −2.28 to −1.33, P < .00001, and Z = 7.42. In terms of hospitalization time, for patients with advanced ankle arthritis, there was a statistically significant difference between open surgery and arthroscope-assisted fusion, and the hospitalization time of patients undergoing arthroscope-assisted fusion was significantly shorter than that of patients undergoing open surgery (Figs. 4 and 5).
Figure 4.
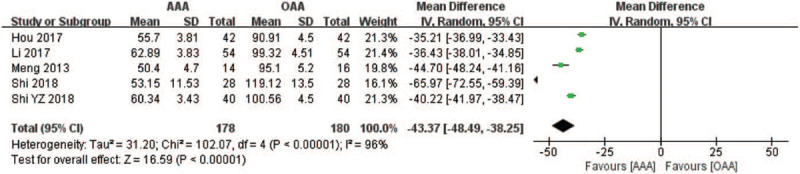
Forest diagram of intraoperative blood loss.
Figure 5.
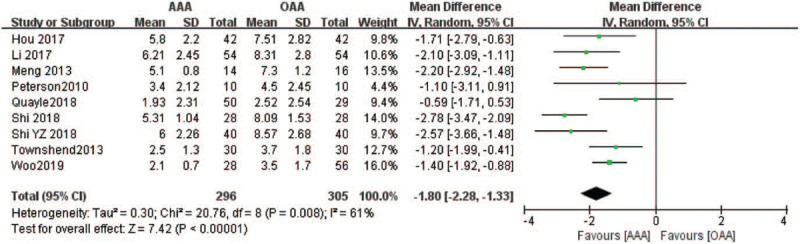
Forest diagram of hospital stay.
3.3.4. VAS and AOFAS score
Six studies were included in the literature;[14,15,17,19,22,30] pain levels after the 2 surgical treatments were evaluated using the VAS, including 474 cases (223 cases in the arthroscopic surgery group, and 251 cases in the open surgery group). The results of heterogeneity analysis showed that there was no substantial heterogeneity among the 6 studies (P = .06, I2 = 54%); the random-effects model was used for analysis. Meta-analysis results showed: MD = −1.75, 95%CI: −2.04 to −1.46, P < .00001, and Z = 11.83. Eight studies[13–17,26,27,30] evaluated the postoperative functional recovery of ankle arthritis after the 2 surgical treatments using the AOFAS, including 562 cases (266 in the arthroscopic operation group and 296 in the open operation group), and the results of heterogeneity analysis showed that there was substantial heterogeneity among the 8 studies (P < .00001, I2 = 99%). Therefore, the random-effects model was used for analysis. Meta-analysis showed that the difference was not statistically significant (MD = −5.23, 95%CI: − −21.21 to 10.75, P = .52, Z = 0.64), indicating that arthroscopic ankle fusion can effectively improve the ankle joint function and relieve pain (Figs. 6 and 7).
Figure 6.
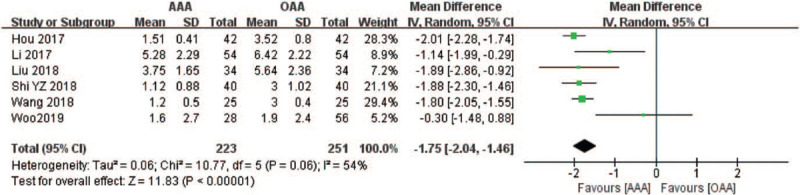
Forest diagram of VAS score.
Figure 7.
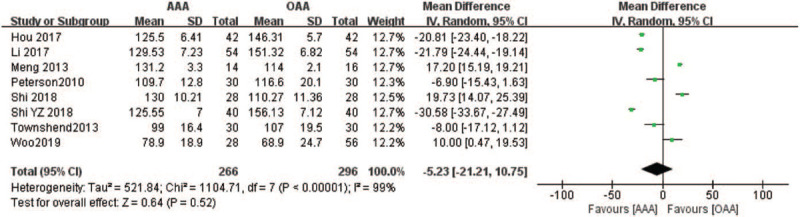
Forest diagram of AOFAS score.
3.3.5. Complications
Eleven studies[14,15,19,21,23–26,28–30] were included to compare the effects of arthroscopic surgery and open surgery in patients with advanced ankle arthritis in terms of postoperative complications (wound infection, malunion, nerve injury, and screw breakage). A total of 701 cases were included, including 332 in the arthroscopic surgery group and 369 in the open surgery group. The results of heterogeneity analysis showed that there was no substantial heterogeneity in the 11 studies (P = .36 < .05, I2 = 9% < 50%), so the fixed-effects model was used for statistical analysis. Meta-analysis results showed that the difference was statistically significant (OR = 0.33, 95%CI:0.21–0.52, P < .00001, Z = 4.85), indicating that arthroscopic surgery for advanced ankle osteoarthritis can effectively reduce the incidence of postoperative complications(Fig. 8).
Figure 8.
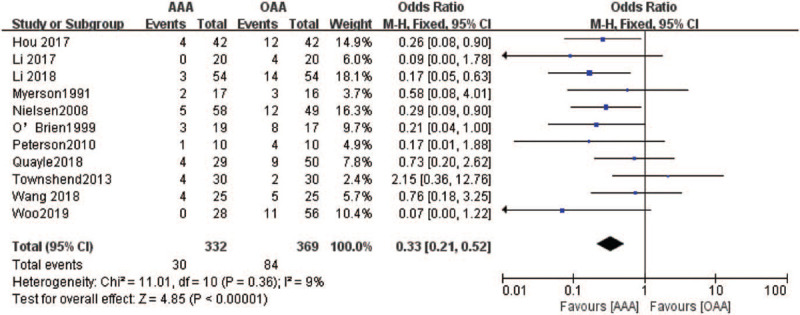
Forest diagram of postoperative complications.
3.3.6. Publication bias
We performed a publication bias analysis by drawing a funnel chart. The left and right distribution of the funnel chart represented by the fusion rate and complications was not completely symmetrical, indicating that there was a publication bias (Fig. 9).
Figure 9.
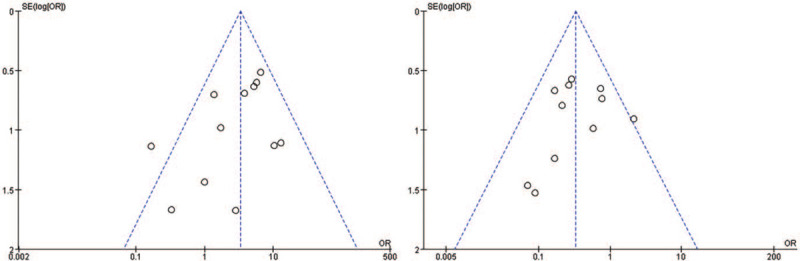
Funnel plot of the trials that compared treatment group with control group (fusion rate, complications).
3.3.7. GRADE level of evidence
By grading the core indicators included in the study, we found that the evidence level of fusion rate, hospital stay, AOFAS, and complications was medium, whereas the level of evidence for fusion time, operation time, intraoperative blood loss, and VAS score was low. The main reason for the degradation is the unclear random method and calculation of the optimal sample size.
4. Discussion
Ankle arthritis is a degenerative disease, and advanced ankle arthritis is the final stage of delayed treatment or poor conservative treatment. This is mainly due to cartilage destruction and synovial hyperplasia, resulting in restricted mobility, and severe pain, and seriously affecting the patient's quality of life. Current treatments for advanced ankle arthritis include ankle arthrodesis, ankle traction arthroplasty, and total ankle arthroplasty. The purpose of ankle arthrodesis is to eliminate pain and improve the quality of life. Ankle arthrodesis was first reported by Albert in 1879. Currently, the common methods of ankle arthrodesis include open incision fusion and minimally invasive arthroscopic fusion. Open ankle arthrodesis can relieve pain and improve function, but it is prone to complications such as incision infection and nonfusion rate of 5% to 37%.[31] In 1983, ankle arthroscopy-assisted ankle arthrodesis was first reported. Since then, this method has been gradually popularized and evolved.[32] Owing to its advantages of small minimally invasive incision, less bleeding, high fusion rate, and fewer complications, it has gradually replaced open ankle arthrodesis as a treatment method for advanced ankle arthritis.
The purpose of this meta-analysis was to compare the clinical effects of arthroscopic-assisted surgery and open ankle arthrodesis in the treatment of advanced ankle arthritis. We selected the operation time, intraoperative blood loss, postoperative hospital stay, postoperative VAS and AOFAS scores, fusion rate and fusion time, complications, and other outcome indicators were selected to comprehensively compare the differences in intraoperative and postoperative indicators between the 2 surgical methods, so as to determine the optimal treatment for ankle arthritis. The results of the meta-analysis showed that arthroscopic-assisted surgery for advanced ankle arthritis was superior to open arthrodesis in terms of the joint fusion rate and fusion time (P < .001). Arthroscopic-assisted ankle fusion surgery involves fast fusion and high fusion rate, which may be related to the relatively small error associated with the arthroscopic direct vision operation. During the operation, the articular cartilage can be repaired, and the alignment and alignment of the ankle joint can be restored.[33] Arthroscopic-assisted surgery for the treatment of advanced ankle arthritis was significantly better than open ankle fusion (P < .001) in terms of postoperative pain score (P < .001), which may be related to the small minimally invasive incision in arthroscopic surgery and less soft tissue damage during the operation. Arthroscopic ankle arthrodesis permits hand exploration while addressing the injured part, comprehensive treatment, and overall repair, enabling the restoration of ankle joint function to the maximum. Although the difference in the effect of bone healing between the 2 is small, arthroscopic surgery has obvious advantages in the short-term curative effects. The time required for bone fusion was shorter, and the effect of joint function improvement was more obvious. Arthroscopic surgery can relieve the patient's pain after a short period of time and improve the quality of life. The 2 surgical methods have significant differences in intraoperative blood loss, hospital stay, and postoperative complications, with arthroscopic ankle fusion being significantly better than open ankle fusion in all 3 areas. Arthroscopic ankle arthrodesis can be operated under direct vision, thus fully damage to the peripheral blood vessels, reducing bleeding, and reducing soft tissue damage. Furthermore, this approach shorten the operation time, improve the treatment effect, reduce complications, promote recovery of the ankle joint function, relieve pain as soon as possible, improve the satisfaction rate of treatment, and have little impact on daily life after surgery.[34,35]
The included literature showed that arthroscopic ankle arthrodesis was more effective than open ankle arthrodesis for the treatment of advanced ankle arthritis in terms of fusion rate, intraoperative blood loss, length of hospital stay, VAS score, fusion time, and postoperative complications. The meta-analysis showed that P < .05, I2 were both greater than 50%, and the combined effect size value was P < .00001, indicating that arthroscopic-assisted arthrodesis has significant clinical efficacy and better postoperative recovery than open surgery for advanced ankle arthritis. Open operative surgery is more practical for patients with severe ankle malformation and articular cavity hyperplasia. There are more than 40 surgical approaches and fixation methods.[36–40] This operation involves a large wound area, long operation time, and a high degree of soft tissue damage. Because of the specialized anatomical structure around the ankle joint and less muscle tissue coverage, the area is prone to incision infection and skin necrosis after surgery, leading to increased postoperative complications.
Arthroscopic ankle fusion has the advantages of small minimally invasive incision, high fusion efficiency, fewer complications, obvious symptom relief, and quicker postoperative recovery; however, the disadvantages include higher equipment cost, more clinical experience required, and more technical requirements compared with open surgery. The operating range of ankle arthroscopy is limited because of the small ankle joint space. Moreover, arthroscopic ankle fusion is not suitable for patients with ankle malformation or poor alignment, ankle varus and valgus alignment exceeding 15°, and obvious ankle varus and valgus malformations.
This study included a large number of documents which increased the sample size and improved the credibility of the conclusion; however, the quality of the articles was relatively insufficient, the random allocation method was not detailed, and the allocation hidden scheme was not perfect. Therefore, more prospective, multicenter, large-sample RCTs should be carried out in the future, and special attention should be paid to the research design to provide evidence-based medicine for the treatment of advanced ankle arthritis.
5. Conclusions
Arthroscopic ankle fusion has the advantages of lower intraoperative blood loss, shorter hospital stay, higher fusion rate, and fewer postoperative complications. The overall clinical effect is better than that of open ankle fusion, and it is worthy of popularization and application. For patients with severe ankle joint deformities, surgical indications should be strictly controlled, and the best surgical method should be selected according to the specific conditions of the patient to reduce the occurrence of postoperative complications.
Author contributions
Conceptualization: Weikai Qin, Weidong Sun.
Data curation: Yanjun Yang, Xuhan Cao.
Formal analysis: Si Chen.
Investigation: Yanjun Yang, Yongli Dong.
Methodology: Xuhan Cao.
Resources: ZiXing Bai.
Software: Yanjun Yang, Si Chen.
Validation: Si Chen, Yongli Dong.
Visualization: Weikai Qin, Weidong Sun.
Writing – original draft: ZiXing Bai, Si Chen.
Writing – review & editing: ZiXing Bai, Yanjun Yang.
Footnotes
Abbreviations: AOFAS = American Orthopaedic Foot & Ankle Society, CI = confidence interval, CNKI = China National Knowledge Infrastructure, GRADE = the grading of recommendations assessment development and evaluation, MD = mean difference, OR = odd ratio, PROSPERO = international database of prospectively registered systematic reviews, RCS = retrospective case-control study, RCT = randomized controlled trial, VAS = visual analog scale.
How to cite this article: Bai Z, Yang Y, Chen S, Dong Y, Cao X, Qin W, Sun W. Clinical effectiveness of arthroscopic vs open ankle arthrodesis for advanced ankle arthritis: a systematic review and meta-analysis. Medicine. 2021;100:10(e24998).
ZB and YY contributed equally.
The authors would like to acknowledge the National Natural Science Foundation of China (81373802, awarded to Weidong Sun) and Beijing Municipal Natural Science Foundation (7172244, awarded to Weidong Sun) for financial support.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Khlopas H, Khlopas A, Samuel LT, et al. Current concepts in osteoarthritis of the ankle: review. Surg Technol Int 2019;35:280–94. [PubMed] [Google Scholar]
- [2].Saltzman CL, Salamon M L, Blanchard GM, et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J 2005;25:44–6. [PMC free article] [PubMed] [Google Scholar]
- [3].Nwankwo EC, Jr, Labaran LA, Athas V, et al. Pathogenesis of posttraumatic osteoarthritis of the ankle. Orthop Clin North Am 2019;50:529–37. [DOI] [PubMed] [Google Scholar]
- [4].Shibuya N, McAlister JE, Prissel MA, et al. Consensus statement of the American College of Foot and Ankle surgeons: diagnosis and treatment of ankle arthritis. J Foot Ankle Surg 2020;59:1019–31. [DOI] [PubMed] [Google Scholar]
- [5].Garras DN, Raikin SM. Supramalleolar osteotomies as joint sparing management of ankle arthritis. Semin Arthroplasty 2010;21:230–9. [Google Scholar]
- [6].Myerson MS, Quill G. Ankle arthrodesis. A comparison of an arthros- copic and an open method of treatmen. Clin Orthop Relat Res 1991;84–95. [PubMed] [Google Scholar]
- [7].Buck P, Morrey BF, Chao EY. The optimum position of arthrodesis of the ankle. A gait study of the knee and ankle. J Bone Joint Surg Am 1987;69:1052–62. [PubMed] [Google Scholar]
- [8].Zhenhui S, Nan L, Tao Z, et al. Progress of total ankle arthroplasty for end-stage ankle osteoarthritis. Chin J Reparat Reconstruct Surg 2018;32:1313–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Maffulli N, Longo UG, Locher J, et al. Outcome of ankle arthrodesis and ankle prosthesis: a review of the current status. Br Med Bull 2017;124:91–112. [DOI] [PubMed] [Google Scholar]
- [10].Viláy RJ, Jiménez DV, Bravo GB, et al. Results of arthroscopic subtalar arthrodesis for adult-acquired flatfoot deformity vs posttraumatic arthritis. Foot Ankle Int 2016;37:198–204. [DOI] [PubMed] [Google Scholar]
- [11].Min Z, Fanzhe F. Recent progress in foot and ankle surgery. Chin J Reparat Reconstruct Surg 2018;32:860–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chenglong L, Qi L, Li Z, et al. Clinical application of arthroscopic ankle arthrodesis. Chin J Reparat Reconstruct Surg 2010;24:1530–1. [Google Scholar]
- [13].Qingyang M, Tengbo Y, Liankui Y, et al. Effectiveness comparison between arthroscopic and open ankle arthrodeses. Chin J Reparat Reconstruct Surg 2013;27:288–91. [PubMed] [Google Scholar]
- [14].Gang L, Peng Z, Xiaolong W. Efficacy comparison of arthroscopic arthrodesis and open ankle arthrodeses on treatment of advanced traumatic arthritis. J Guangxi Med Univ 2017;34:1590–3. [Google Scholar]
- [15].Yu H, Linjie W, Zhixing L, et al. Effect of arthroscopic internal fixation and fusion for the treatment of patients with advanced ankle arthritis and the influence of AOFAS and VAS score. China J Endosc 2017;12:60–5. [Google Scholar]
- [16].Jie S, Bo Q. The effect of arthroscopy-assisted ankle joint fusion for advanced traumatic ankle arthritis. Clin J Med Officers 2018;46:1320–1. [Google Scholar]
- [17].Yongzheng S. Comparative observation and safety analysis of arthroscopic-assisted internal fixation ankle fusion and open ankle fusion in the treatment of advanced traumatic ankle arthritis. Healthmust-Readmagazine 2018;134. [Google Scholar]
- [18].Xuhong Z, Jianlong L, Yaxian L. Effect analysis of arthroscopic ankle fusion for traumatic anklebone arthritis. Electron J Foot Ankle Surg 2018;5:36–8. 43. [Google Scholar]
- [19].Jianhua W. Short-term effect and surgical points of arthroscopic ankle arthrodesis in the treatment of severe ankle joint osteoarthritis. Clin Res Pract 2018;3:74–5. [Google Scholar]
- [20].Guocheng L, Min W. Ankle arthroscopic bone graft fusion in patients with advanced arthritis and its effect on limb function. Diabetes World 2018;15:173–4. [Google Scholar]
- [21].Jiuyuan L, Youfei F. Clinical effect of arthroscopic bone graft fusion in the treatment of advanced ankle arthritis. Home Med 2018;10:100. [Google Scholar]
- [22].Xiaodong L. Clinical study of minimally invasive ankle arthrodesis in the treatment of traumatic arthritis. China Reflexol 2018;27:147–8. [Google Scholar]
- [23].O’Brien TS, Hart TS, Shereff MJ, et al. Open versus arthroscopic ankle arthrodesis: a comparative study. Foot Ankle Int 1999;20:368–74. [DOI] [PubMed] [Google Scholar]
- [24].Panikkar KV, Taylor A, Kamath S, et al. A comparison of open and arthroscopic ankle fusion. Foot Ankle Surg 2003;9:169–72. [Google Scholar]
- [25].Nielsen KK, Linde F, Jensen NC. The outcome of arthro-scopic and open surgery ankle arthrodesis: a comparative retrospective study on 107 patients. Foot Ankle Surg 2008;14:153–7. [DOI] [PubMed] [Google Scholar]
- [26].Peterson KS, Lee MS, Buddecke DE. Arthroscopic versus open ankle arthrodesis: a retrospective cost analysis. J Foot Ankle Surg 2010;49:242–7. [DOI] [PubMed] [Google Scholar]
- [27].Townshend D, Di Silvestro M, Krause F, et al. Arthroscopic versus open ankle arthrodesis: a multicenter comparative case series. J Bone Joint Surg Am 2013;95:98–102. [DOI] [PubMed] [Google Scholar]
- [28].Myerson MS, Quill G. Ankle arthrodesis. A comparison of an arthroscopic and an open method of treatment. Clin Orthop Relat Res 1991;84–95. [PubMed] [Google Scholar]
- [29].Quayle J, Shafafy R, Khan MA, et al. Arthroscopic versus open ankle arthrodesis. Foot Ankle Surg 2018;24:137–42. [DOI] [PubMed] [Google Scholar]
- [30].Woo BJ, Lai MC, Ng S, et al. Clinical outcomes comparing arthroscopic vs open ankle arthrodesis. Foot Ankle Surg 2019;S1268-7731:30100–6. [DOI] [PubMed] [Google Scholar]
- [31].Qiang X. Ankle fusion by plating through an anterior approach followed by posterolateral approach: a three-dimensional finite element analysis. Chin J Tissue Eng Res 2017;21:5697–702. [Google Scholar]
- [32].Xiaojun D, Liu Y, Xu P, et al. Arthroscopic ankle arthrodesis for end-stage post-traumatic ankle arthritis. Chin J Orthopaed 2013;33:403–8. [Google Scholar]
- [33].Le M. Application of minimally invasive ankle arthrodesis in the treatment of traumatic arthritis of the foot and ankle. China Pract Med 2019;14:52–4. [Google Scholar]
- [34].Yinghui Z, Zhijian W, Tao Z, et al. Analysis of the effect of ankle arthrodesis in the treatment of traumatic arthritis of the foot and ankle. Chin J Modern Drug Appl 2016;10:63–4. [Google Scholar]
- [35].Guanggang Y, Yongxiong P, Wanzhong L, et al. Analysis of ankle arthrodesis in the treatment of traumatic arthritis of foot and ankle. Chin J Mod Drug Appl 2016;10:60–1. [Google Scholar]
- [36].Nickisch F, Avilucea FR, Beals T, et al. Open posterior approach for tibiotalar arthrodesis. Foot Ankle Clin 2011;16:103–14. [DOI] [PubMed] [Google Scholar]
- [37].Torudom Y. The results of ankle arthrodesis with screws for end stage ankle arthrosis. J Med Assoc Thai 2010;93: Suppl 2: S50–4. [PubMed] [Google Scholar]
- [38].Clare MP, Sanders RW. The anatomic compression arthrodesis technique with anterior plate augmentation for ankle arthrodesis. Foot Ankle Clin 2011;16:91–101. [DOI] [PubMed] [Google Scholar]
- [39].Yasui Y, Takao M, Miyamoto W, et al. Technique tip: open ankle athrodesis using locking compression plate combined with anterior sliding bone graft. Foot Ankle Int 2010;31:1125–8. [DOI] [PubMed] [Google Scholar]
- [40].Gessmann J, Ozokyay L, Fehmer T, et al. Arthrodesis of the infected ankle joint: results with the Ilizarov External Fixator. Z Orthop Unfall 2011;149:212–8. [DOI] [PubMed] [Google Scholar]


