Abstract
Background:
Blood pressure lowering treatments can help prevent cardiovascular disease. However, little is known about the possibility of home visiting programs for hypertension. This study aims to evaluate the effectiveness of home visiting programs on hypertensive patients.
Methods:
We systematically reviewed the medical literature and performed a meta-analysis. Five electronic databases were systematically searched from their inception to September 2019. Two reviewers independently assessed the risk of bias of the studies included in the review using tools developed by the Cochrane Collaboration. The meta-analysis was performed using Review Manager software (version 5.3).
Results:
Thirteen RCTs with 2674 participants were identified. The home visiting program demonstrated a greater reduction in systolic blood pressure (MD = −5.63, 95% confidence interval (CI): −8.32 to −2.94), diastolic blood pressure (MD = −4.14, 95% CI: −6.72 to −1.56) and waist circumference (MD = −2.61, 95% CI: −3.5, −1.72) during a 6 month intervention. However, there were no significant differences between the groups in terms of body mass index, weight, or blood lipids.
Conclusion:
Home visiting programs were associated with improved BP control and reduced blood pressure, which indicate that it might be an effective method for management of hypertension.
Keywords: home visit, hypertension, meta-analysis
1. Introduction
Hypertension is a public health challenge worldwide that contributes to societal burdens and whose global prevalence is ∼31.9%.[1] High blood pressure (BP) is the most common attributable risk factor to cardiovascular disease, cerebrovascular disease, death and disability, with ∼9.4 million deaths each year and >1 billion affected individuals.[2,3] According to the guidelines of the American College of Cardiology (ACC)/American Heart Association (AHA), hypertension is now defined as systolic blood pressure (SBP) ≥ 130 mm Hg or a diastolic blood pressure (DBP) ≥ 80 mm Hg.[4] The adoption of the 2017 ACC/AHA guidelines will therefore result in a substantial increase in both prevalence and the number of hypertension patients.
However, the control of hypertension is far from satisfactory.[5] It was reported that although 53.7% of hypertension patients were recommended to take antihypertensive medications, the current treatment rate is only 16.8%.[6] Untreated hypertension results in a progressive increase in blood pressure. Because of the high prevalence and low control rate,[7] the management and control of hypertension is becoming a public health problem worldwide. However, the most effective approach to reducing blood pressure remains controversial.[8,9]
The ACC/AHA has indicated that follow-up is an important component of BP management in hypertensive patients.[4] As the European Society of Cardiology/European Society of Hypertension (ESC/ESH) has stated, it is necessary to revisit the patient after the initiation of antihypertensive drug therapy.[10] Furthermore, home visiting is a concrete strategy of follow-up that has been utilized in many clinical paradigms, such as for preterm infants, young children, postnatal and perinatal advice, smoking, and diabetes.[11–14] It is considered an economical and effective method for preventing and controlling chronic diseases, providing benefits for patients, their families and society in general, in addition to improving the quality of life among older patients with chronic diseases.[15,16] Because home visiting is a comprehensive term, in this review, we have defined it as: the utilization of individuals or teams of health professionals, which may include nurses, primary care providers, pharmacists, and behavioral health specialists with the aim of improving health and social outcomes, conducting the visit at the patients’ home.[17] So far, many studies have shown that home visiting can improve the clinical outcomes of hypertensive and manage the hypertensive effectively, but robust evidence from home visiting for hypertension is sparse and contested.[13,18–21] As far as we have known, this is the first meta-analysis which is to synthesis the effectiveness of home visiting on hypertensive. Therefore, the study uses the methods of systematic review and meta-analysis to evaluate the effectiveness of home visiting for hypertension management, and to provide theoretical basis for the continuation of nursing methods for patients with hypertension.
2. Methods and analysis
2.1. Search strategy
Six electronic databases (PubMed, EMBASE, Cochrane Library, Web of Science, CINAHL, and the Chinese BioMedical Literature Database) were searched for articles that evaluated blood pressure and home visits, that had been published from database inception to September 2019. We also checked the reference lists of relevant articles for additional studies, utilizing backward, and forward searching for relevant articles. Only randomized controlled trials were included in this review. The search strategy used for PubMed is provided in Appendix 1, which used a combination of MeSH and free text terms. The search ensured that MeSH terms were exploded. Free text terms were searched in the title, abstract, summary, heading, or keywords. The search strategy was adjusted as appropriate for each database searched.
2.2. Eligible criteria
Studies meeting the following criteria were included:
-
1.
evaluation of adult patients (≥ 8 years old) with hypertension (regardless of treatment status) without complications;
-
2.
the intervention evaluated was a home visit program, conducted at the patients’ home with no limitations as to who conducted the visit (nurse, primary care provider, pharmacist or behavioral health specialist);
-
3.
usual care employed health education leaflets or pamphlets regarding hypertension;
-
4.
the primary outcome measures were change in SBP and DBP.
-
5.
Secondary outcome measures were changes in body mass index (BMI), waist circumference, weight, and blood lipids;
-
6.
study design was an RCT (regardless of blinding status); and
-
7.
publication full text was published in English or Chinese.
2.3. Study selection
Two reviewers independently scanned eligibility by reading the abstract of each study identified by the search. These reviewers independently eliminated studies that clearly did not satisfy eligibility criteria and obtained full copies of all remaining studies. The same two reviewers read the studies independently to identify those that were eligible. In the event of disagreement, a third reviewer adjudicated. We did not anonymize studies before assessment and followed a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement to report our manuscript.[22]
2.4. Data extraction and quality appraisal
Two reviewers independently extracted data of interest using a standard electronic form which were checked for agreement prior to data analysis. Disagreements regarding data extraction were resolved through discussion. The extracted data included patient and study characteristics, including sample size, treatment comparisons, baseline blood pressure, final blood pressure, and mean blood pressure reduction. If not reported, we contacted the corresponding author to obtain data about baseline blood pressure through use of individually tailored data request forms.
The two reviewers independently evaluated the risk of bias using the Cochrane Collaboration tool,[23] which evaluated random sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other sources of bias.[24,25] Each study was assessed as either “low risk of bias,” “high risk of bias,” or “unclear risk of bias” for each item based on study reporting and/or additional information provided by the study authors (Fig. 2).
Figure 2.
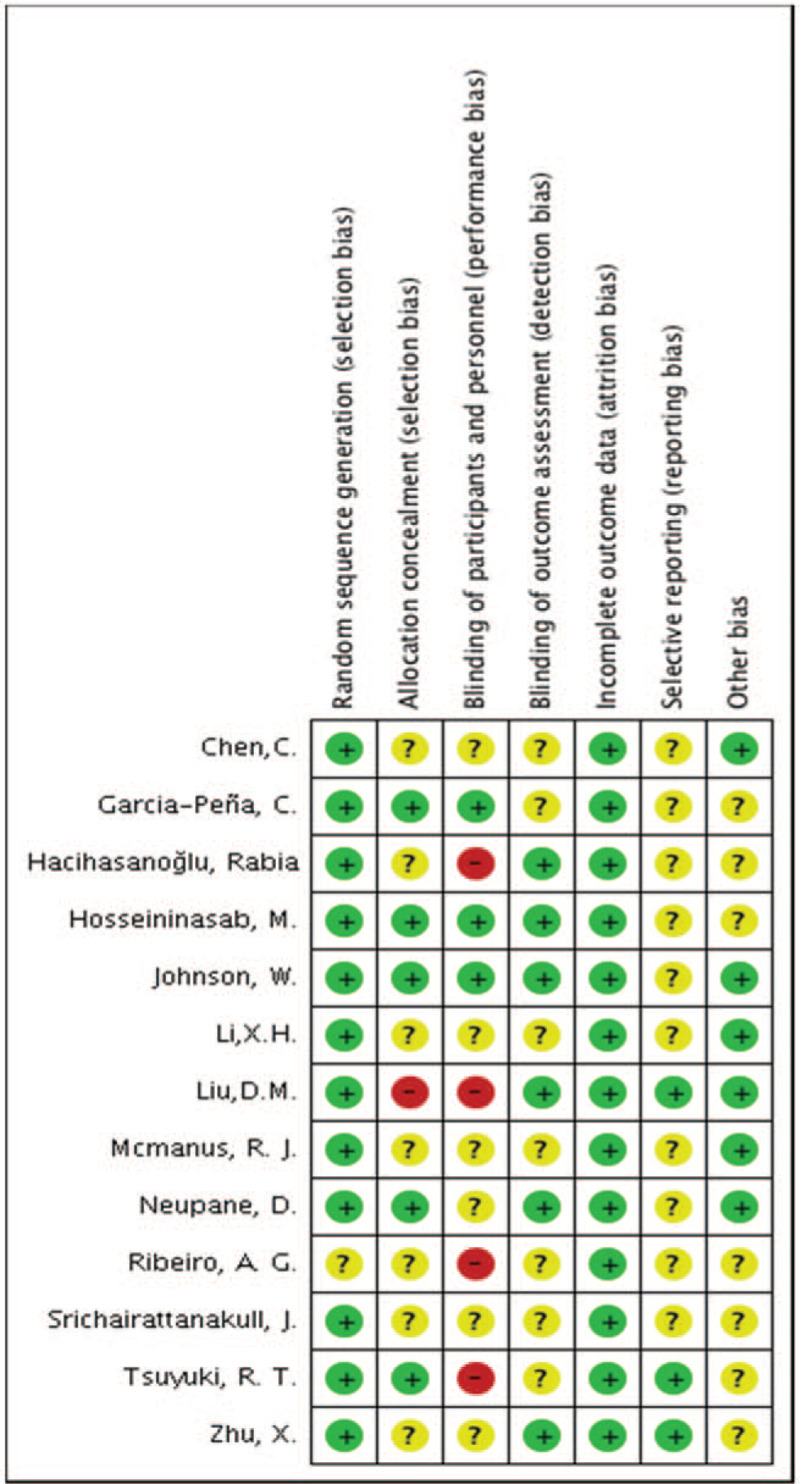
Risk of bias assessment results.
2.5. Data analysis
Heterogeneity was independently assessed through visual inspection of forest plots and on the basis of quantitative results of both a χ2 test of heterogeneity and the I2 statistic. Changes in blood pressure were calculated based on the differences between pre- and post-intervention blood pressure using the Cochrane Collaboration tool. When quantitative synthesis (i.e., meta-analysis) was feasible, a random-effects model was utilized to analyze dichotomous outcomes with odds ratios, continuous outcomes with mean differences (MD). Where sufficient data were available, a subgroup analysis was undertaken to examine potential sources of heterogeneity based on the duration of intervention. Review Manager software (version 5.3) was used for pooling related data. A narrative synthesis of studies was presented for parameters for which the required data were unavailable for meta-analysis. All P values were calculated from two tailed tests of statistical significance with a type I error rate of .05.
2.6. Ethical approval
This systematic review does not require ethical assessment because only indirect literature will be included and evaluated.
3. Results
3.1. Literature selection
The literature search identified 1506 studies, of which 280 were duplicates. A further 997 studies were excluded after the initial screening of titles and abstracts. The full-text of the remaining 155 studies were further reviewed, of which 13 were considered eligible for this review (Fig. 1).
Figure 1.
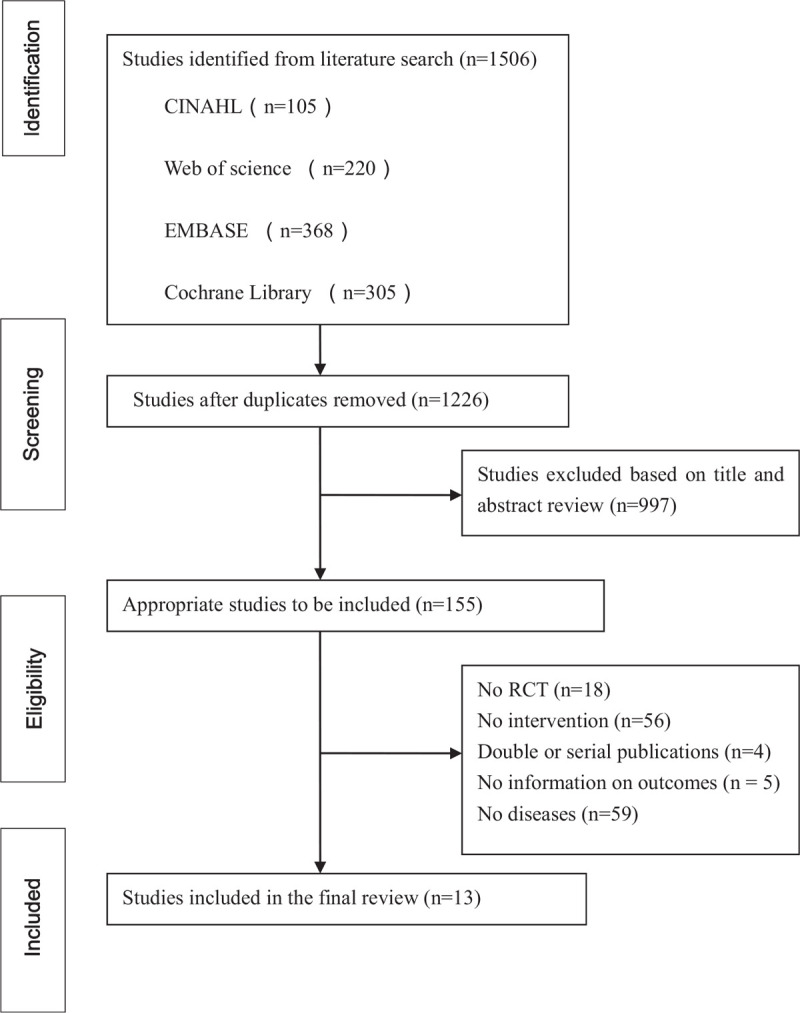
Process of study identification and selection.
3.2. 3.2 Study characteristics and risks of bias
Table 1 summarizes the main characteristics of the selected RCTs, which included the authors, publication date, study location, sample size, mean age, sex distribution, implementor, and study duration. Thirteen studies with 2674 patients (of which 1432 received home visits and 1242 received usual care) were included. These studies were performed in China (4 studies), Turkey (1 study), Mexico (1 study), Thailand (1 study), Nepal (1 study), Iran (1 study), Canada (1 study), Brazil (1 study), India (1 study), and the United States (1 study). The duration of intervention ranged from 8 weeks to 12 months.
Table 1.
Characteristics of the included randomized controlled trials.
| Sex (F/M) | Sample size (n) | Age range (years) Mean (SD) | |||||||||
| References | Study location | Home visit | Usual care | Home visit | Usual care | Home visit | Usual care | Study duration | Implementer | Intervention group | Control group |
| Neupane (2018) | Nepal | 134/121 | 115/65 | 255 | 180 | 50.12 ± 8.99 | 50.28 ± 8.14 | 1 year | Female community health volunteers | FCHVS-led home-based health education and screening of BP in adults | Usual care pertaining to current practices for hypertension management at the community level |
| Garcia-Peña (2001) | Mexico | 229/116 | 230/108 | 345 | 338 | 70.8 ± 7.11 | 70.34 ± 6.92 | 6 months | Nurse-led intervention | Nurse and patient reviewed information from the baseline health check, and discussed possible lifestyle changes at home | Receive usual care from family physicians in the Institute's clinics and a mailed pamphlet about hypertension. |
| Tsuyuki (2015) | Canada | 92/89 | 35/32 | 181 | 67 | 63 ± 13 | 65 ± 11 | 24 weeks | Pharmacist | Guided by the CHEP guidelines and consisted of pharmacist assessment of and counseling about cardiovascular risk and BP control, review of antihypertensive medications, and prescribing of drug therapy, in addition to a wallet card for recording BP measurements, lifestyle advice | Usual care group received a wallet card for recording BP, lifestyle advice as required |
| Johnson (2015) | American | 15/12 | 16/11 | 27 | 27 | 58.5 ± 7.4 | 59 ± 8.15 | 6 months | Community health worker | Community health worker educational session | Usual care group assessment of BP, pulse and adverse events, but did not receive the educational intervention |
| Zhu (2014) | China | 21/15 | 12/25 | 36 | 37 | 70.42 ± 10.63 | 67.81 ± 8.82 | 8 weeks | Nurse-led intervention,and pharmacological | Nurse-led hypertension management designed on the basis of the 4-C (comprehensiveness, collaboration, coordination, and continuity) framework | The control group in the study received hypertensive care guided by the traditional doctor-led model,included unstructured and irregular follow-ups with pharmacological treatment by general practitioners. |
| Ribeiro (2011) | Brazil | 14/0 | 14/0 | 14 | 14 | 55.6 ± 2.8 | 50.7 ± 6.5 | 5 months | – | Participated in the educative workshops and received personalized orientation through periodic home visits. | Received orientation regarding the dietary treatment of hypertension through monthly dialogic education workshops |
| Hacihasanoğlu (2011) | Turkey | 20/20 | 22/18 | 40 | 40 | 56.92 ± 8.04 | 56.62 ± 8.46 | 6 months | – | Education in medication compliance in addition to education in healthy lifestyle behaviours | Six interviews to usual care but only blood pressure and weight measurements were checked at each interview |
| Hosseininasab (2014) | Iran | 58/39 | 61/36 | 97 | 97 | 59.6 ± 10.3 | 57.8 ± 11.1 | 6 months | Study investigator | Received a wrist blood pressure measurement device, they were instructed how to use the device and document their measurements in a logbook and measure their blood pressure once daily at a specific time every day | Received usual care as suggested by the physician. |
| Mcmanus (2010) | UK | 110/124 | 115/131 | 234 | 246 | 66.6 ± 8.8 | 66.2 ± 8.8 | 12 months | Family doctor and study investigator | Participants were trained to monitor their own blood pressure for the fi rst week of each month with a validated automated sphygmomanometer | Usual care and performance-related pay an annual review to monitor blood pressure, provide support, and discuss lifestyle, symptoms, and medication |
| Srichairattanakull (2012) | Thailand | 15/7 | 9/11 | 22 | 20 | 51.3 ± 6 | 51.8 ± 6.3 | 12 weeks | – | Group meetings and home visit monitoring | The basic services were health checkups and group health education. |
| Chen (2015) | China | 43/20 | 37/25 | 63 | 62 | – | – | 6 months | Nurse-led intervention | Home visiting for hypertension based on Omaha system | Usual care according to community hypertension routine care |
| Liu (2015) | China | 38/20 | 40/14 | 58 | 54 | 69.5 ± 6.9 | 70.1 ± 6.2 | 6 months | Nurse-led intervention | Home visiting | Usual care according to community hypertension routine care |
| Li (2013) | China | 33/27 | 31/29 | 60 | 60 | 65 ± 8 | 66 ± 7 | 6 months | Nurse-led intervention and study investigator | Home visit for hypertension based on standard nursing language | Community health service stations carry out regular health education. |
F/M = female/male, FCHVS = female community health volunteers, BP = blood pressure, SD = standard deviation.
Figure 2 displays the risks of bias for the studies included in the review. Random sequence generation was adequate in 12/13 studies and allocation concealment in 5/13 studies. However, the blinding of participants was not possible in the majority of studies due to the nature of the intervention, in addition to blinding of the outcomes. Overall, incomplete outcome data were reported in every study, but selective reporting was so poor that only 3 studies reported this item.
3.3. Meta-analysis
3.3.1. Blood pressure
Systolic and DBP were reported in 13 trials (2674 participants randomised). The pooling of data across studies of varying duration was limited by the noticeable statistical heterogeneity between studies. Consequently the results are presented through subgroup analyses of duration of studies. In a pre-specified subgroup analysis, the pooled intervention effect estimate tended to be more pronounced among the 6 months groups (MD = −5.63, 95% CI: −8.32 to −2.94, 9 trials, 1997 participants, I2 = 88%) rather than those of 12 months (MD = −4.75, 95% CI: −6.96 to −2.54, 2 trials, 912 participants, I2 = 0) in favor of home visits (Fig. 3). However, 3 month intervention was not statistically significantly different between home visit and usual care. Similarly, the pooled effect showed a statistically significant reduction in DBP in 6 month intervention (MD = −4.14 mm Hg, 95% CI: −6.72 to −0.56, 1997 participants, I2 = 88%) and 12 months (MD = −2.33, 95% CI: −3.8 to −0.85, I2 = 0) in favor of home visit interventions (Fig. 4). We found a subgroup effect of SBP among 3, 6, and 12-months follow up (P = .01), but no significant difference between 6 and 12-months follow up. We failed to explore the subgroup effect for DBP among different durations of follow up (P = .10).
Figure 3.
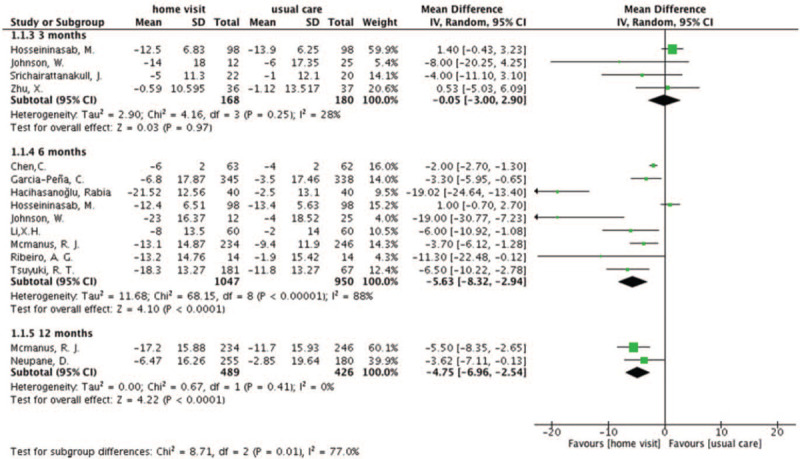
Change in systolic blood pressure with home visit compare with usual care.
Figure 4.
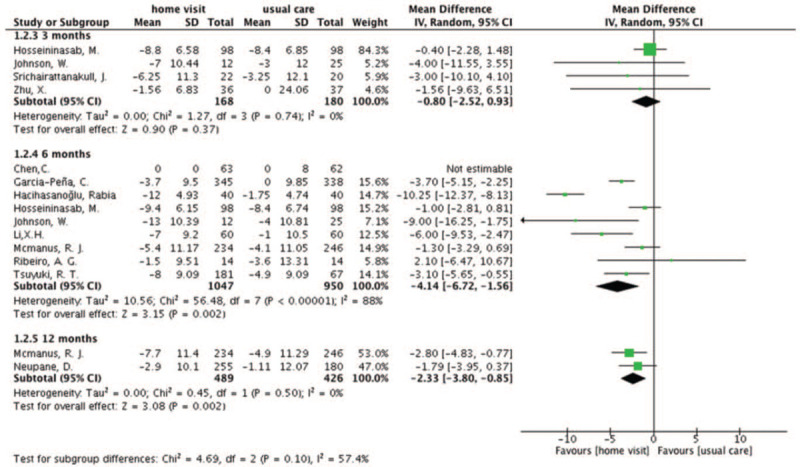
Change in diastolic blood pressure with home visit compare with usual care.
3.3.2. BMI
Five trials reported BMI (395 patients).[26–30] There was no statistically significant difference between intervention and control group in mean change from baseline BMI (MD = −0.49 95% CI: −1.10 to 0.13, 395 participants), although there was a trend suggesting that home visit programs could decrease the BMI of the participants. The I2 statistic (0%) showed no heterogeneity among the five trials (Fig. 5).
Figure 5.
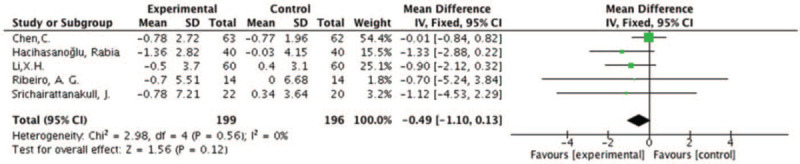
Change in BMI with home visit compare with usual care.
3.3.3. Other outcomes
Three trials reported waist circumference as an individual outcome.[26,28,29] There was a statistically significant difference between intervention and control in mean change from baseline waist circumference (MD = −2.61 cm, 95% CI: −3.5 to −1.72, 195 participants). Two trials reported weight[29,31] although there was no statistically significant difference between the intervention and control groups in mean change from baseline weight (MD = −1.02 kg, 95% CI: −2.89 to 0.85). One trial reported on blood lipids,[32] but no statistically significant difference was observed between intervention and control in mean change from baseline high density lipoprotein (HDL) (MD = −5.7, 95% CI: −13.3 to 1.9), low density lipoprotein (LDL) (MD = −6.4, 95% CI: −36.2 to 23.4) and total cholesterol (MD = −1.7, 95% CI: −39.6 to 36.2) (Table 2).
Table 2.
Summary of meta-analyses of studies using home visit to manage diabetes.
| Heterogeneity | |||||||
| Outcome measure | Trails | Sample size (Intervention/Control) | Measure of effects | Intervention effect size (95%CI) | P-value of effect | I2 (%) | P |
| Waist circumference, cm | 3 | 195 (99/96) | MD | −2.61 [−3.5, −1.72]∗ | 0.001 | 0 | .94 |
| Weight,Kg | 2 | 711 (359/352) | MD | −1.02 [−2.89, 0.85] | 0.28 | 0 | .89 |
| High density Lipoprotein, mg/dL | 1 | 28 (14/14) | MD | −5.7 [−13.3, 1.9] | 0.14 | N/A | N/A |
| Low density Lipoprotein, mg/dL | 1 | 28 (14/14) | MD | −6.4 [−36.2, 23.4] | 0.67 | N/A | N/A |
| Total cholesterol, mg/dL | 1 | 28 (14/14) | MD | −1.7 [−39.6, 36.2] | 0.93 | N/A | N/A |
CI = confidence intervals; I2 = I-squared, MD = mean difference, NA = not applicable.
P < .05.
3.4. Meta-regression
Meta regression analysis showed that age and gender had no significant change on blood pressure (Table 3).
Table 3.
The result of meta-regression.
| Coef | P | 95% CI | |
| Age | 0.01199 | .572 | (−0.03376, 0.05773) |
| Sex | −0.47229 | .679 | (−2.93989, 1.99530) |
CI = confidence Interval, Coef = coefficient.
4. Discussion
4.1. Principal findings of this review
This review identified thirteen trials of home visit programs for the management of hypertension patients. Given the significant burden of hypertension, and the increasing prevalence of related risk factors, it is important to focus on the prevention and control of the condition.[5,33] The findings of the present meta-analysis suggest that home visit programs are more effective at reducing SBP, DBP, and waist circumference. However, there was no evidence that they affect BMI, weight, or blood lipids (LDL, HDL, or total cholesterol). The main theoretical mechanism why home visiting can manage the hypertensive patients are as follows: first, in the process of home visiting, the medical staff or health care manager could discuss the common problems, difficulties and obstacles with the patient of hypertension, and help different patients to seek personalized solutions; Secondly, studies have shown that home visiting can improve the family functions of patients with hypertension and give full play to the role of the family support system, while family blood pressure monitoring and family support can improve patients’ drug compliance behavior.[34] However, changes in BMI, body weight, and blood index require a long-term process, which may be the main theoretical basis for this study to obtain the results.
4.1.1. Blood pressure
This body of evidence supports the role of home visit programs as a central feature of individual and population health promotion strategies for patients with hypertension. This was consistent with those described in other studies that evaluated similar strategies to improve blood pressure control. For example, a smartphone app[35] decrease mean blood pressure by 2.5 mm Hg, and nurse-managed protocols[36] could make systolic and DBP decrease by 3.68 and 1.56 mm Hg. The differences found in this trial were smaller than those of the team-based care interventions for hypertension,[37] but greater than trials using nurse-managed protocols and telecare.[36,38] Although the absolute differences in blood pressure appear small, they are significant. For example, the benefits of reduction in cardiovascular endpoints in the Systolic Hypertension in Europe (SYST-EUR) study and coronary events in the Systolic Hypertension in the Elderly Program (SHEP) study were both achieved following a reduction in SBP of <10 mm Hg.[39,40] Furthermore, a recent meta-analysis revealed that blood pressure reduction treatment significantly reduced the risk of cardiovascular disease and death, a 10 mm Hg reduction in SBP reducing the risks of major cardiovascular disease events (–20%), coronary heart disease (–17%), stroke (–27%), heart failure (–28%), and all causes of mortality (–13%).[41] This highlights the clinical significance of even small changes in resting blood pressure. However, this study indicates that home visit programs for 6 months are more favorable than 12 months for lowering blood pressure. This may in part be due to a sample size effect, as only two trials reported the reduction of systolic and DBP over 12 months, resulting in the studies being too underpowered to demonstrate differences in outcomes. This small trial lacked statistical power and so it was not possible to draw a reliable conclusion.[42]
4.1.2. BMI, body weight, and waist circumference
Although this meta-analysis indicated that home visit programs have a significant effect on blood pressure reduction, the analysis found the evidence less clear toward BMI and body weight compared to usual care, a result which is similar to previous meta-analyses,[36,43] but dissimilar to other research.[19] Obesity is a major influence on the development of hypertension.[44,45] BMI is a strong predictor of overall mortality both above and below the apparent optimum of about 22.5 to 25 kg/m2.[46,47] The results suggest that home visit programs have no significant effect on BMI or body weight, possibly because the duration of the intervention was too brief to achieve a substantial impact. In addition, weight and BMI were reported in only 2 to 3 studies,[44,47,48] which might not be great enough to observe any actual benefit. Waist circumference, which may be the best single indicator of other individual and multiple cardiovascular risk factors,[49] demonstrated a significant treatment effect. A previous studies demonstrated that a 1 cm increase in waist circumference was associated with a 2% increase in the relative risk of a cardiovascular disease event.[50] That means even a small decrease in waist circumference brought about by home visiting may have substantial public health benefits.
4.1.3. Blood lipids
The meta-analysis demonstrated that home visit programs have no significant effect on blood lipids. The results are not in agreement with those of most other studies evaluating the efficacy of nurse-led interventions on lipid profile.[43,48,51] Only 1 of the 13 studies reported LDL, HDL, and total cholesterol.[40] The strength of evidence was judged, therefore, to be insufficient to determine the effect of home visit programs on blood lipids related to hypertension. A small sample size may result in larger bias due to variations among the participants or in some conditions, contribute to a positive result when the observed effect is much larger than the true difference. Therefore, future studies should be planned with a longer duration to improve the likelihood of detecting change and assessing long-term sustainability of blood pressure reductions.
4.2. Strengths, limitations, and future research
This study has many strengths, including a comprehensive search, careful quality assessment and methods that provide rigorous quantitative synthesis. However, this study, as does the literature, has limitations.[52] First, it is not possible to perform deep analysis on some important outcomes because the original research was not reported. There are large differences in the duration and frequency of interventions. For example, studies had limited descriptions of intervention intensity, intervention frequency, intervention supervision or their level of education, training, or other performance measures, and rarely reported were treatment adherence, lifestyle index and so on. Secondly, we restricted our research to articles in English and Chinese, which may have excluded some potential data published in other languages.[53] Finally, there is a paucity of randomised controlled trials studying the effects of home visit programs for hypertension management over the long-term.
Recent studies of home visit programs and hypertension focused on blood pressure control, BMI, weight, and blood lipids. Other important outcome indicators were ignored, such as cost effectiveness, self-care adherence, patient satisfaction, intensity of blood pressure lowering medication, physical activity or lifestyle changes. Therefore, the results of the present meta-analysis highlighted three important topics for future research. First, it will be important to evaluate the cost effectiveness of home visit programs, with a more complete cost analysis possibly required. Secondly, high-quality multicenter RCTs are needed to examine the specific outcomes of home visit programs.[54] Thirdly, further research is also required to identify which form, intensity, duration and frequency of home visit programs are most effective in caring for hypertension patients, which modes of home visit and which settings are key for an effective home visit program. Therefore, we need more than evidence of effectiveness as a basis for formulating recommendations for how governments should provide services.[55,56]
5. Conclusions
The findings of the present meta-analysis suggested that home visiting might be more effective at improving the patient with hypertension. The present systematic review provided some important findings. First, lowering blood pressure levels should therefore be routinely considered for the prevention of cardiovascular disease. Home visiting is an effective method to manager hypertension, especially SBP and DBP. Second, there is a scarcity of high-quality evidence regarding the effects of home visiting on hypertensive management. Therefore, additional studies are required to provide a greater body of evidence regarding the extent to which the duration and frequency of intervention plays a major role in home visiting. This systematic review can serve as a guide to researchers and practitioners interested in understanding and/or developing home visit programs in the hypertension domain.
Author contributions
Conceptualization: Yuxia Ma, Lin Han, Hongmei Lu.
Data analysis: Hongmei Lu.
Data curation: Yuanyuan Zhang, Sijun Li.
Formal analysis: Yuanyuan Zhang.
Methodology: Yutan Wang, Sijun Li, Fanghong Yan.
Software: Yutan Wang, Fanghong Yan.
Writing – original draft: Yuxia Ma, Hongmei Lu.
Writing – review & editing: Lin Han.
Supplementary Material
Footnotes
Abbreviations: ACC = American College of Cardiology, AHA = American Heart Association, BMI = body mass index, BP = blood pressure, CHEP = Canadian Hypertension Education Program, CI = confidence interval, coef = coefficient, DBP = diastolic blood pressure, ESC/ESH = European Society of Cardiology/European Society of Hypertension, FCHVs = Female community health volunteers, HDL = high density lipoprotein, LDL = low density lipoprotein, MD = mean differences, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, RCTs = randomized controlled trials, SBP = systolic blood pressure, SD = standard deviation, SHEP = Hypertension in the Elderly Program, SYST-EUR = Systolic Hypertension in Europe.
How to cite this article: Ma Y, Lu H, Zhang Y, Wang Y, Li S, Yan F, Han L. Effectiveness of home visiting on patients with hypertension: A systematic review and meta-analysis. Medicine. 2021;100:10(e24072).
National Nature Science Foundation of China (71663002, 71704071), the fund of China Medical Board(#20-374), the Research Funds for the School of Nursing of Lanzhou University (LZUSON202002), Natural Science Foundation of Gansu Province (20JR10RA603), the Fundamental Research Funds for the Central Universities (lzujbky-2020-10).
The authors have no conflicts of interests to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Supplemental digital content is available for this article.
References
- [1].Naghavi M, Abajobir AA, Abbafati C, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1151–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].WHO. A global brief on hypertension. Geneva: World Health Organization. 2013. Available at: https://www.who.int. Accessed December 2019. [Google Scholar]
- [3].Carey RM, Muntner P, Bosworth HB, et al. Prevention and control of hypertension: JACC health promotion series. J Am Coll Cardiol 2018;72:1278–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018;71:e127–248. [DOI] [PubMed] [Google Scholar]
- [5].Huang D, Song X, Cui Q, et al. Is there an association between aircraft noise exposure and the incidence of hypertension? A meta-analysis of 16784 participants. Noise Health 2015;17:93–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Yang C, Wang J, Gao B, et al. Prevalence and treatment of hypertension in China: impacts of 2017 American College of Cardiology/American Heart Association High Blood Pressure Guideline. Sci Bull 2018;63:488–93. [DOI] [PubMed] [Google Scholar]
- [7].Zhu X, Wong FK, Wu LH. Development and evaluation of a nurse-led hypertension management model in a community: a pilot randomized controlled trial. Int J Clin Exp Med 2014;7:4369–77. [PMC free article] [PubMed] [Google Scholar]
- [8].James PA, Oparil S, Carter BL, et al. 2014 guideline for management of high blood pressure. JAMA 2014;311:507–20. [DOI] [PubMed] [Google Scholar]
- [9].Emdin CA, Rahimi K, Neal B, et al. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA 2015;313:603–15. [DOI] [PubMed] [Google Scholar]
- [10].Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018;36:1953–2041. [DOI] [PubMed] [Google Scholar]
- [11].Lee E, Kirkland K, Miranda-Julian C, et al. Reducing maltreatment recurrence through home visitation: a promising intervention for child welfare involved families. Child Abuse Neglect 2018;86:55–66. [DOI] [PubMed] [Google Scholar]
- [12].Griffis H, Matone M, Kellom K, et al. Home visiting and perinatal smoking: a mixed-methods exploration of cessation and harm reduction strategies. BMC Public Health 2016;16:764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Han L, Ma Y, Wei S, et al. Are home visits an effective method for diabetes management? A quantitative systematic review and meta-analysis. J Diabetes Invest 2017;8:701–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Goyal NK, Angelique T, Ammerman RT. Home visiting and outcomes of preterm infants: a systematic review. Pediatrics 2013;132:502–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Caldera D, Burrell L, Rodriguez K, et al. Impact of a statewide home visiting program on parenting and on child health and development. Child Abuse Neglect 2007;31:829–52. [DOI] [PubMed] [Google Scholar]
- [16].Edraki M, Moravej H, Rambod M. Effect of home visit training program on growth and development of preterm infants: a double blind randomized controlled trial. Int J Community Based Nurs Midwifery 2015;3:12–22. [PMC free article] [PubMed] [Google Scholar]
- [17].Turnbull C, Osborn DA. Home visits during pregnancy and after birth for women with an alcohol or drug problem. Cochrane Database Syst Rev 2012;1:CD004456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Glynn LG, Murphy AW, Smith SM, et al. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2010;CD005182. [DOI] [PubMed] [Google Scholar]
- [19].Cicolini G, Simonetti V, Comparcini D, et al. Efficacy of a nurse-led email reminder program for cardiovascular prevention risk reduction in hypertensive patients: a randomized controlled trial. Int J Nurs Stud 2014;51:833–43. [DOI] [PubMed] [Google Scholar]
- [20].Persell SD, Eder M, Friesema E, et al. EHR-based medication support and nurse-led medication therapy management: rationale and design for a three-arm clinic randomized trial. J Am Heart Assoc 2013;2:e000311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Spies LA, Bader SG, Opollo JG, et al. Nurse-led interventions for hypertension: a scoping review with implications for evidence-based practice. Worldviews Evid Based Nurs 2018;15:247–56. [DOI] [PubMed] [Google Scholar]
- [22].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [Updated March 2011]. Cochrane Collab 2011;Available at: www.cochrane-handbook.org. Accessed December 2019. [Google Scholar]
- [24].Xiu-xia L, Ya Z, Yao-long C, et al. The reporting characteristics and methodological quality of Cochrane reviews about health policy research. Health Policy 2015;119:503–10. [DOI] [PubMed] [Google Scholar]
- [25].Ge L, Tian JH, Li YN, et al. Association between prospective registration and overall reporting and methodological quality of systematic reviews: a meta-epidemiological study. J Clin Epidemiol 2018;93:45–55. [DOI] [PubMed] [Google Scholar]
- [26].Srichairattanakull J, Kaewpan W, Powattana A, et al. Self-management improvement program combined with community involvement in Thai hypertensive population: an action research. J Med Assoc Thai 2014;97:456–66. [PubMed] [Google Scholar]
- [27].Li XH, Du WJ, Mao XR, et al. Effect of home visit applying standardized nursing language to the elderly with hypertension in community. Chin Gen Pract 2013;16:3231–3. [Google Scholar]
- [28].Chen C, Zheng CH, Zhao M, et al. Implementing home visit to improve treatment compliance of community hypertension patients. Chin Nurs Manage 2013;15:186–90. [Google Scholar]
- [29].Ribeiro AG, Ribeiro SM, Dias CM, et al. Non-pharmacological treatment of hypertension in primary health care: a comparative clinical trial of two education strategies in health and nutrition. BMC Public Health 2011;11:637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hacihasanoğlu R, Gözüm S. The effect of patient education and home monitoring on medication compliance, hypertension management, healthy lifestyle behaviours and BMI in a primary health care setting. J Clin Nurs 2011;20:692–705. [DOI] [PubMed] [Google Scholar]
- [31].Garcia-Pena C, Thorogood M, Armstrong B, et al. Pragmatic randomized trial of home visits by a nurse to elderly people with hypertension in Mexico. Int J Epidemiol 2001;30:1485–91. [DOI] [PubMed] [Google Scholar]
- [32].Neupane D, McLachlan CS, Mishra SR, et al. Effectiveness of a lifestyle intervention led by female community health volunteers versus usual care in blood pressure reduction (COBIN): an open-label, cluster-randomised trial. Lancet Glob Health 2018;6:e66–73. [DOI] [PubMed] [Google Scholar]
- [33].Wang X, Bots ML, Yang F, et al. Prevalence of hypertension in China: a systematic review and meta-regression analysis of trends and regional differences. J Hypertens 2014;32:1919–27. [DOI] [PubMed] [Google Scholar]
- [34].Yan J. Analysis of nursing effect of individualized home visit on elderly patients with hypertension in community. Electron J Clin Med Lit 2019;6:70–2. [Google Scholar]
- [35].Márquez Contreras E, Márquez Rivero S, Rodríguez García E, et al. Specific hypertension smartphone application to improve medication adherence in hypertension: a cluster-randomized trial. Curr Med Res Opin 2019;35:167–73. [DOI] [PubMed] [Google Scholar]
- [36].Shaw RJ, McDuffie JR, Hendrix CC, et al. Effects of nurse-managed protocols in the outpatient management of adults with chronic conditions: a systematic review and meta-analysis. Ann Intern Med 2014;161:113–21. [DOI] [PubMed] [Google Scholar]
- [37].Carter BL, Rogers M, Daly J, et al. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med 2009;169:1748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Verberk WJ, Kessels AG, Thien T. Telecare is a valuable tool for hypertension management, a systematic review and meta-analysis. Blood Press Monit 2011;16:149–55. [DOI] [PubMed] [Google Scholar]
- [39].Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet 1997;350:757–64. [DOI] [PubMed] [Google Scholar]
- [40].Probstfield JL. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA 1991;265:3255–64. [PubMed] [Google Scholar]
- [41].Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957–67. [DOI] [PubMed] [Google Scholar]
- [42].Lee LL, Watson MC, Mulvaney CA, et al. The effect of walking intervention on blood pressure control: a systematic review. Int J Nurs Stud 2010;47:1545–61. [DOI] [PubMed] [Google Scholar]
- [43].Murtagh EM, Nichols L, Mohammed MA, et al. The effect of walking on risk factors for cardiovascular disease: an updated systematic review and meta-analysis of randomised control trials. Prev Med 2015;72:34–43. [DOI] [PubMed] [Google Scholar]
- [44].Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res 2017;122:1–7. [DOI] [PubMed] [Google Scholar]
- [45].Baran M, Celikkalkan K, Appak YC, et al. Body fat mass is better indicator than indirect measurement methods in obese children for fatty liver and metabolic syndrome. Sci Med J 2019;1:168–75. [Google Scholar]
- [46].Lee SH, Kim DH, Park JH, et al. Association between body mass index and mortality in the Korean elderly: a nationwide cohort study. PLoS One 2018;13:e0207508.DOI: 10.1371/journal.pone.0207508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Gajalakshmi V, Lacey B, Kanimozhi V, et al. Body-mass index, blood pressure, and cause-specific mortality in India: a prospective cohort study of 500 810 adults. Lancet Glob Health 2018;6:e787–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Pan B, Ge L, Xun YQ, et al. Exercise training modalities in patients with type 2 diabetes mellitus: a systematic review and network meta-analysis. Int J Behav Nutr Phys Act 2018;15:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Choi B, Steiss D, Garcia-Rivas J, et al. Comparison of body mass index with waist circumference and skinfold-based percent body fat in firefighters: adiposity classification and associations with cardiovascular disease risk factors. Int Arch Occ Env Hea 2016;89:435–48. [DOI] [PubMed] [Google Scholar]
- [50].de Koning L, Merchant AT, Pogue J, et al. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur Heart J 2007;28:850–6. [DOI] [PubMed] [Google Scholar]
- [51].Chang AK, Fritschi C, Mi JK. Nurse-led empowerment strategies for hypertensive patients with metabolic syndrome. Contemp Nurse 2012;42:118–28. [DOI] [PubMed] [Google Scholar]
- [52].Yao L, Sun R, Chen YL, et al. The quality of evidence in Chinese meta-analyses needs to be improved. J Clin Epidemiol 2016;74:73–9. [DOI] [PubMed] [Google Scholar]
- [53].Li L, Tian J, Tian H, et al. Network meta-analyses could be improved by searching more sources and by involving a librarian. J Clin Epidemiol 2014;67:1001–7. [DOI] [PubMed] [Google Scholar]
- [54].Tian J, Zhang J, Ge L, et al. The methodological and reporting quality of systematic reviews from China and the USA are similar. J Clin Epidemiol 2017;85:50–8. [DOI] [PubMed] [Google Scholar]
- [55].Li X, Wei L, Shang W, et al. Trace and evaluation systems for health services quality in rural and remote areas: a systematic review. J Public Health 2017;26:1–9.29416959 [Google Scholar]
- [56].Mavrogiorgou A, Kiourtis A, Touloupou M, et al. Internet of medical things (IoMT): acquiring and transforming data into HL7 FHIR through 5G network slicing. ESJ 2019;3:64–77. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


