Abstract
Rationale:
Cystoisosporiasis is an intestinal infectious disease caused by a coccidian protozoa, Cystoisospora belli (C. belli). It can cause prolonged and refractory diarrhea most commonly in immunocompromised patients, while immunocompetent individuals usually exhibit no symptoms or self-limited diarrhea.
Patient concerns:
We herein report a case of chronic cystoisosporiasis in an immunocompetent patient. A 62-year-old man, who had been first diagnosed with cystoisosporiasis 15 years ago and had been treated with oral administration of trimethoprim-sulfamethoxazole (TMP-SMX), complained of persistent watery diarrhea. He was negative for anti-human immunodeficiency virus antibody and anti-human T-cell leukemia virus type 1 (HTLV-1) antibody.
Diagnosis:
Biopsy specimens from the duodenum revealed oocysts in the atrophic absorptive epithelium and protozoa were detected through stool examination, indicating the recurrence of cystoisosporiasis. Capsule endoscopy showed diffuse atrophic mucosa with white villi in the entire small intestine. We diagnosed him with chronic cystoisosporiasis that occurred in an immunocompetent adult.
Interventions:
Since oral administration of TMP-SMX and ciprofloxacin were ineffective, the intravenous administration of TMP-SMX was initiated.
Outcomes:
Intravenous TMP-SMX exhibited a significant improvement.
Lessons:
This case indicates that even immunocompetent individuals may develop recurrent and refractory cystoisosporiasis. Furthermore, intravenous treatment of antibiotic agents should be considered when the impaired absorptive ability from the small intestine is suspected.
Keywords: capsule endoscopy, case report, cystoisospora belli, cystoisosporiasis, immunocompetent
1. Introduction
Cystoisospora belli (C. belli) is a protozoan parasite that primarily infects the epithelial cells of the small intestine.[1] It is present worldwide but is mostly found in tropics and subtropics.[1] Humans are thought to be only a host of C. belli since there is no report that C. belli infects other animals.[2] People become infected by ingesting oocysts excreted from the stool of infected patients.[3]C. belli infection, called cystoisosporiasis, is characterized by watery and non-bloody diarrhea. Most cases are reported in patients who are immunocompromised hosts with acquired immune deficiency syndrome (AIDS) or adult T-cell leukemia (ATL).[4,5] Diarrhea is usually prolonged and refractory and leads to malabsorption syndrome.[6] In contrast, C. belli infection is often either asymptomatic or associated with self-limited acute diarrhea in immunocompetent hosts.[6]
According to the therapeutic guidelines for patients with AIDS, trimethoprim-sulfamethoxazole (TMP-SMX) is recommended as the first-line antibiotic agent for cystoisosporiasis.[5] When TMP-SMX is ineffective or intolerant, ciprofloxacin should be considered as an alternative treatment.[5,7] However, in cases of severe damage to epithelial cells of the small intestine, these medicines are not absorbed adequately. In this situation, it is recommended to administer medicines intravenously.[5] Here, we report a case of chronic C. belli infection that occurred in an immunocompetent adult. Capsule endoscopy and histopathological findings revealed the severe atrophic mucosa in the small intestine. The patient was successfully treated by intravenous administration of TMP-SMX, but not its oral administration.
2. Case report
A 62-year-old man visited the out-patient department of the Shiga University of Medical Science Hospital with prolonged watery diarrhea and lower-extremity weakness. He was once diagnosed with Cystoisospora infection 15 years ago and treated with oral TMP-SMX. However, diarrhea lasted intermittently after the treatment. Laboratory studies on visit showed eosinophilia (778 /μl), hypoalbuminemia (3.3 g/dl), hypokalemia (3.0 mmol/L), and normal serum C-reactive protein (0.02 mg/dl) (Table 1). He was born and raised on a small island located in south Kyushu, Japan, where human T-cell leukemia virus type 1 (HTLV-1) is endemic, and his father died with ATL. However, he was negative for anti-HTLV-1 antibody (Table 1). Additional laboratory examinations such as human immunodeficiency virus antigen/antibody test, serum soluble interleukin-2 receptor, the CD4 count were normal (Table 1). We performed a stool microscopy examination and found the presence of protozoa that exhibited green autofluorescence under ultraviolet exposure (Fig. 1A). Consistently, esophagogastroduodenoscopy showed diffuse atrophic mucosa in the duodenum (Fig. 1B) and a microscopic examination of the duodenum biopsy specimens revealed invaded oocysts in the atrophic absorptive epithelial cells (Fig. 1C). A contrast-enhanced computed tomography indicated excess fluid in the entire small intestine with no wall thickness (Fig. 2A). Therefore, he underwent capsule endoscopy (PillCam SB 3; Medtronic, Dublin, Ireland) to observe the mucosa of the small intestine and found the atrophic mucosa with diffuse white villi in the entire small intestine and no apparent erosions and ulcers (Fig. 2B). These findings indicated chronic infection with C. belli.
Table 1.
Laboratory findings on admission.
| Parameter | Result | Normal Range | Parameter | Result | Normal Range |
| WBC (/μl) | 6600 | 3000–8000 | CRP (mg/dl) | 0.02 | 000–0.30 |
| Neut (%) | 62.3 | 40.0–74.0 | IgM (mg/dl) | 50 | 35–220 |
| Lymph (%) | 18.8 | 15.0–48.0 | IgG (mg/dl) | 1312 | 870–1700 |
| Eosin (%) | 11.8 | 0.0–7.0 | IgA (mg/dl) | 412 | 110–410 |
| Mono (%) | 6.2 | 2.0–12.0 | IgE (IU/ml) | 3901.1 | 0.0–400.0 |
| CD4 (/μl) | 870 | 500–1200 | sIL-2R (U/ml) | 418 | 121–613 |
| Hb (g/dl) | 13.1 | 12.4–17.0 | Glucose (mg/dl) | 108 | 70–109 |
| Ht (%) | 36.5 | 38.0–54.0 | HbA1c (%) | 5.4 | 4.6–6.2 |
| Plt (x104/μl) | 21.0 | 15.0–40.0 | ESR (mm/hour) | 5.0 | 2.0–10.0 |
| TP (g/dl) | 6.3 | 6.3–8.3 | ANA | (−) | |
| Alb (g/dL) | 3.3 | 4.0–5.0 | HBs-Ag | (−) | |
| Na (mEq/L) | 139 | 138–146 | HCV-Ab | (−) | |
| K (mEq/L) | 3.0 | 3.6–4.9 | HIV-Ag/Ab | (−) | |
| Cl (mEq/L) | 109 | 99–109 | TP-Ag | (−) | |
| T. chol (mg/dl) | 127 | 128–219 | HTLV1-Ab | (−) | |
| TG (mg/dl) | 57 | 30–149 |
Alb = albumin, ANA = anti-nuclear antibody, CRP = C-reactive protein, Eosin = eosinophil, ESR = erythrocyte sedimentation rate, Hb = hemoglobin, HbA1c = glycated hemoglobin, HBs-Ag = hepatitis B surface antigen, HCV-Ab = hepatitis C virus antibody, HIV-Ag/Ab = human immunodeficiency virus antigen/antibody, Ht = hematocrit, HTLV-1-Ab = human T cell leukemia virus type 1 antibody, Lymph = lymphocyte, Mono = monocyte, Neut = neutrophil, Plt = platelet, sIL-2R = soluble interleukin-2 receptor, T. chol = total cholesterol, TG = triglyceride, TP = total protein, TP-Ag = treponema pallidum antigen, WBC = white blood cell.
Figure 1.
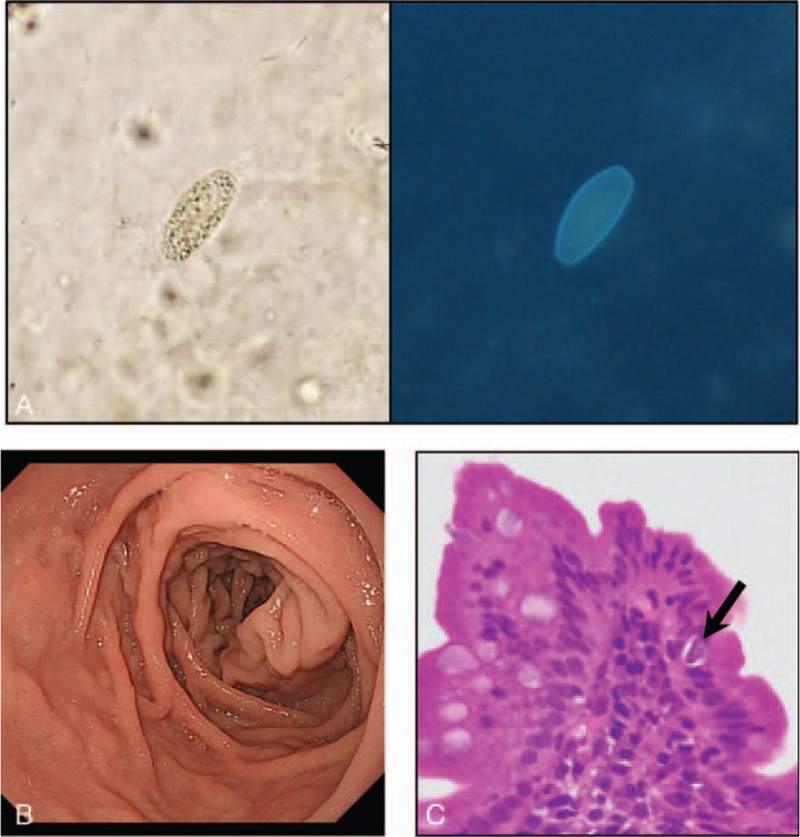
(A) A light microscopic image (left panel) and UV fluorescence microscopy image (right panel) of the stool. (B) EGD showed the marked atrophic mucosa in the duodenum. (C) The H/E-stained section revealed the presence of an oocyst within the absorptive epithelial cells (solid arrow). Original magnification × 100.
Figure 2.
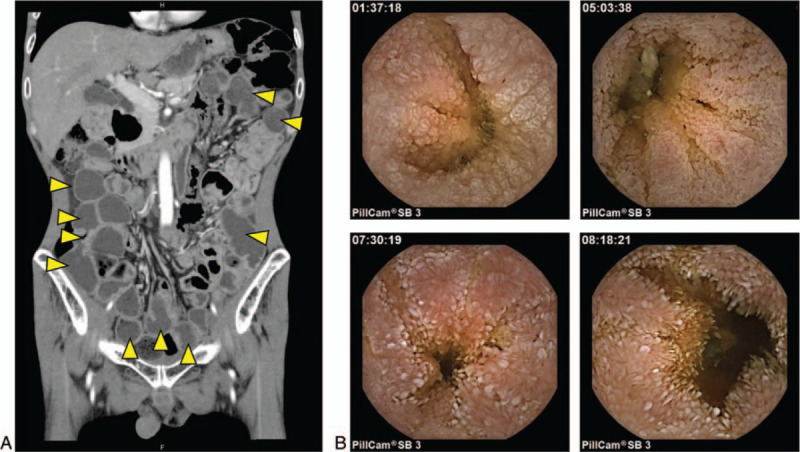
(A) Contrast-enhanced CT on admission. The small intestine contained excessive fluid (Yellow Arrowheads) but showed no obvious wall thickness. (B-E) Capsule endoscopy showed unique images with white villi in the entire small intestine. Small bowel transit time was 8 hour 21 minutes.
We started oral administration of 2 tablets of trimethoprim-sulfamethoxazole (TMP-SMX; 160 mg of TMP, 800 mg of SMX per day), followed by ciprofloxacin (400 mg per day). However, both failed to improve the patient's symptoms. Afterward, he received central parenteral nutrition and was treated with intravenous administration of TMP-SMX (15 mg per kg per day based on TMP component) for 10 days, since an impairment of drug absorption was suspected. After this, his symptoms were remarkably improved, and the protozoa became undetectable in the stool. So far, 9 months have passed since the intravenous intervention, and there is no evidence of recurrence.
3. Discussion
We experienced a case of chronic C. belli infection in an immunocompetent adult. C. belli is a protozoan pathogen that causes an opportunistic infection primarily in immunocompromised patients with AIDS and/or ATL.[8] Cystoisosporiasis is also reported in patients with non-Hodgkin lymphoma, alcoholism, and ulcerative colitis taking azathioprine and anti-TNF-α antibody treatment.[9–11] However, only a few reports described C. belli infection in immunocompetent individuals.[12,13] In our case, there was no evidence of immunocompromised status by extensive examinations. Given that ATL was endemic in his birthplace, it is speculated that he might be infected with C. belli in infancy and become chronic. Furthermore, C. belli infection was chronic because the patient exhibited intermittent diarrhea for more than 15 years. Severe atrophic mucosa observed in capsule endoscopy also supported chronic infection. These endoscopic images are invaluable in understanding how cystoisosporiasis affects the small intestinal mucosa.
The diagnosis of C. belli infection is usually based on the detection of oocysts in the stool. It can be also found in an intestinal biopsy specimen.[5] However, it can be difficult to detect by routine examinations. Therefore, the detection of autofluorescence is helpful to identify C. belli in the stool when C. belli infection is suspected.[14] Interestingly, our case showed prominent eosinophilia that is one of the unique features of cystoisosporiasis.[15] Other protozoan infections generally do not cause eosinophilia; this finding is useful for diagnosing cystoisosporiasis. Of note, our case also showed markedly elevated serum IgE levels, suggesting an excess allergic response in the small intestine.
Treatment of cystoisosporiasis was usually performed with oral administration of antibiotic agents. However, the oral administration of drugs was ineffective in our patients. This is presumably due to the impaired absorption ability associating with severe mucosal atrophy. It should be noted that intravenous administration of antibiotic agents is recommended for the treatment of C. belli infection when impaired mucosal absorption is suspected.[5] Indeed, intravenously administered TMP-SMX quickly improved his symptoms.
In conclusion, this case emphasizes that immunocompetent individuals can develop chronic and recurrent cystoisosporiasis. Cystoisosporiasis should be taken into account in patients with chronic diarrhea who have mucosal atrophy in the small intestine. In addition, capsule endoscopy is thought to be a useful tool for the early detection of mucosal atrophy.
Author contributions
Conceptualization: Masashi Ohno, Osamu Inatomi.
Funding acquisition: Masashi Ohno.
Investigation: Masashi Ohno, Takayuki Imai, Kenichiro Takahashi, Keiji Konishi, Ryoji Kushima.
Supervision: Osamu Inatomi, Akira Andoh.
Validation: Shigeki Bamba, Masaya Sasaki.
Writing – original draft: Masashi Ohno.
Footnotes
Abbreviations: AIDS = acquired immune deficiency syndrome, ATL = adult T-cell leukemia, C. belli = Cystoisospora belli, TMP-SMX = trimethoprim-sulfamethoxazole.
How to cite this article: Ohno M, Inatomi O, Imai T, Takahashi K, Bamba S, Konishi K, Sasaki M, Kushima R, Andoh A. Chronic cystoisosporiasis in an immunocompetent adult: a case report. Medicine. 2021;100:10(e24890).
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this article. This work was supported by JSPS KAKENHI Grant Number JP19K23844.
The patient has provided informed consent for the publication of this case report and accompanying images.
The authors state that they have no conflict of interest.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Dubey JP, Almeria S. Cystoisospora belli infections in humans: the past 100 years. Parasitology 2019;146:1490–527. [DOI] [PubMed] [Google Scholar]
- [2].Franzen C, Muller A, Bialek R, et al. Taxonomic position of the human intestinal protozoan parasite Isospora belli as based on ribosomal RNA sequences. Parasitol Res 2000;86:669–76. [DOI] [PubMed] [Google Scholar]
- [3].Bonadonna L, Briancesco R, Ottaviani M, et al. Occurrence of Cryptosporidium oocysts in sewage effluents and correlation with microbial, chemical and physical water variables. Environ Monit Assess 2002;75:241–52. [DOI] [PubMed] [Google Scholar]
- [4].DeHovitz JA, Pape JW, Boncy M, et al. Clinical manifestations and therapy of Isospora belli infection in patients with the acquired immunodeficiency syndrome. N Engl J Med 1986;315:87–90. [DOI] [PubMed] [Google Scholar]
- [5].Kaplan JE, Benson C, Holmes KK, et al. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep 2009;58(RR-4):1–207. quiz CE201-204. [PubMed] [Google Scholar]
- [6].Ramakrishna BS, Venkataraman S, Mukhopadhya A. Tropical malabsorption. Postgrad Med J 2006;82:779–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Verdier RI, Fitzgerald DW, Johnson WD, Jr, et al. Trimethoprim-sulfamethoxazole compared with ciprofloxacin for treatment and prophylaxis of Isospora belli and Cyclospora cayetanensis infection in HIV-infected patients. A randomized, controlled trial. Ann Intern Med 2000;132:885–8. [DOI] [PubMed] [Google Scholar]
- [8].Goodgame RW. Understanding intestinal spore-forming protozoa: cryptosporidia, microsporidia, isospora, and cyclospora. Ann Intern Med 1996;124:429–41. [DOI] [PubMed] [Google Scholar]
- [9].Resiere D, Vantelon JM, Bouree P, et al. Isospora belli infection in a patient with non-Hodgkin's lymphoma. Clin Microbiol Infect 2003;9:1065–7. [DOI] [PubMed] [Google Scholar]
- [10].Kim MJ, Kim WH, Jung HC, et al. Isospora belli Infection with Chronic Diarrhea in an Alcoholic Patient. Korean J Parasitol 2013;51:207–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Stein J, Tannich E, Hartmann F. An unusual complication in ulcerative colitis during treatment with azathioprine and infliximab: Isospora belli as ’Casus belli’. BMJ Case Rep 2013;bcr2013009837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Tas Cengiz Z, Yilmaz H, Cicek M, et al. Cystoisospora sp. Infection determined in immunosuppressed and immunocompetent children: three cases report. Turkiye Parazitol Derg 2016;40:107–9. [DOI] [PubMed] [Google Scholar]
- [13].Woon SA, Yang R, Ryan U, et al. Chronic cystoisospora belli infection in an immunocompetent Myanmar refugee - microscopy is not sensitive enough. BMC Infect Dis 2016;16:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bialek R, Binder N, Dietz K, et al. Comparison of autofluorescence and iodine staining for detection of Isospora belli in feces. Am J Trop Med Hyg 2002;67:304–5. [DOI] [PubMed] [Google Scholar]
- [15].Apt WB. Eosinophilia in Isospora infections. Parasitol Today 1986;2:22. [DOI] [PubMed] [Google Scholar]


