Abstract
A neglected Monteggia fracture is defined as the fracture of the proximal ulna associated with radial head dislocation (RHD) without undergoing any treatment for 4 weeks or more after injury. One-stage operation of ulnar corrective osteotomy and open reduction of RHD might result in many complications. Therefore, a two-stage strategy, including ulnar osteotomy (UO) with or without annular ligament reconstruction (ALR), was adopted at our institute since 2010.
We performed a retrospective review of 51 patients with neglected Monteggia fracture between January 2010 and January 2018. Patients with bilateral problems or concomitant injuries in the ipsilateral extremity were excluded. Radiological and clinical data were collected from Hospital Database and clinical visits. All patients were divided into 2 groups based on the status of the ALR: the UO alone (UO) group and the ALR group.
There were 15 patients in the UO group and 36 patients in the ALR group. The age in the UO group (6.1 ± 2.3, year) was significantly younger than the ALR group (9.8 ± 2.8, year) (P < .001). Concerning the duration from initial injury to surgery, there was a significant difference between the UO group (8.6 ± 3.2 months) and the ALR group (23.3 ± 12.6 months, P < .001). Concerning the preoperative elbow function, there was no significant difference between the UO group (67.6 ± 5.0) and the ALR group (66.6 ± 4.4) according to the Mayo elbow performance score (MEPS) (P = .51). Concerning the postoperative parameters, including postoperative ROM of the joint, removal of external fixator (6.7 ± 0.8, 6.9 ± 0.9 weeks) (P = .55), lengthening (8.9 ± 2.5, 10.3 ± 2.5 mm) (P = .10) and MEPS (92.7 ± 2.1, 91.6 ± 2.1) (P = .08), there was no significant difference between the UO group and ALR group.
Two-stage strategy is a reasonable choice for selected patients with long-lasting RHD with ulnar deformity.
Keywords: annular ligament reconstruction, Monteggia fracture, radial head dislocation, ulnar osteotomy
1. Introduction
Monteggia fracture is a relatively rare injury in children.[1] Around 25% to 50% of these injuries may be missed by the health care providers at first encounter, depending on their expertise and experience.[2]
The natural history of chronic Monteggia lesions is not well elucidated, but some patients present with pain, loss of motion (especially flexion and supination), elbow deformity, and even arthritis.[3] Many procedures have been described to treat this condition, including open reduction and annular ligament reconstruction (ALR),[4] radial osteotomy,[5] open reduction and ulnar osteotomy (UO),[6] radial head excision.[7] However, there is no unanimous consensus for neglected Monteggia fracture in children.
A neglected Monteggia fracture is defined as the fracture of the proximal ulna associated with radial head dislocation (RHD) without undergoing any treatment for 4 weeks or more following injury.[2,3,7] Ulnar corrective osteotomy to restore the normal length of the ulna, and the relationship between radius and ulna was reported.[8] But, in certain patients, UO alone is not able to reduce RHD and maintain the reduction afterward.[9] Therefore, a two-stage strategy was adopted at our institute since 2010. The first stage is UO and lengthening; the second stage is the removal of the external fixator (EF) with or without open reduction and ALR. This retrospective study aims to review the clinical outcomes of patients treated with two-stage strategy.
2. Materials and methods
We performed a retrospective review of 51 patients with neglected Monteggia fracture between January 2010 and January 2018 at Union Hospital, Tongji Medical College, Huazhong University of Science and Technology. This study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (IORG No. IORG0003571) on December 20, 2019. Written consent was obtained from the patient's legal guardians.
Among 51 patients (see Table 1), 15 patients were included in the UO alone (UO) group and 36 patients were included in the UO + open reduction and ALR group. All patients were younger than 14 years at the surgery and followed up for more than 24 months. Patients with bilateral problems and/or concomitant injuries in the ipsilateral extremity and incomplete medical records were excluded. Radiological and clinical parameters were collected from the Hospital Database and out-patient visits. The elbow joint function was evaluated using the Mayo elbow performance score (MEPS)[10] during the out-patient visits by the surgeon in charge.
Table 1.
baseline information of the patients.
| Parameters | UO (n = 15) | ALR (n = 36) | P value |
| Age (years) | 6.1 ± 2.3 | 9.8 ± 2.8 | <.001 |
| Sex | |||
| male | 7 | 21 | .46 |
| Female | 8 | 15 | |
| Side | |||
| Left | 6 | 14 | .95 |
| Right | 9 | 22 | |
| Bado classification | |||
| Type I | 14 | 36 | .12 |
| Type III | 1 | 0 | |
| From initial injury to surgery (m) | 8.6 ± 3.2 | 23.3 ± 12.6 | <.001 |
| Follow-up time (years) | 3.5 ± 1.1 | 3.4 ± 1.0 | .75 |
| Pre-op ROM of elbow | |||
| Extension | −1.8 ± 1.8 | −2.2 ± 1.9 | .53 |
| Flexion | 108.1 ± 5.8 | 112.0 ± 6.1 | .047 |
| Pronation | 69.3 ± 9.0 | 63.0 ± 8.7 | .034 |
| Supination | 73.3 ± 4.3 | 71.9 ± 5.3 | .34 |
| Pre-op MEPI score | 67.6 ± 5.0 | 66.6 ± 4.4 | .51 |
ALR = annular ligament reconstruction, UO = ulnar osteotomy alone.
All descriptive data were presented as the mean±SD. Statistical analysis was performed using SPSS (SPSS Inc, Chicago, IL). A P value of <.05 is regarded as statistical significance.
2.1. Surgical Technique
Stage 1: The proximal part of the ulna is exposed through the dorsal approach. A sagittal Z-shaped osteotomy of the ulna was performed, and then 2 Schanz screws were placed in the distal and proximal part of the ulna at an angle as per the preoperative plan. After the insertion of the Schanz screws, the pins were adjusted to be parallel and installed into the unilateral external fixator. Excessive bony spikes on the dorsal side might be shaved off to prevent prominence on the dorsal aspect. The arm was immobilized in a long-arm slab for 4 to 6 weeks according to the lengthening process. Lengthening was initiated at the rate of 1 mm/day and started once the pain was subsided, usually at 5 to 7 days. The patient was followed up at the out-patient clinic weekly. If severe pain or nerve palsy occurred, the lengthening would be suspended for 3 to 5 days and then continued. If the length of the ulna was restored, the lengthening process would be stopped regardless of the status of the radial head. The external fixator was not removed until the consolidation of the osteotomy site was evident.
Stage 2: After the evidence of bony union of the osteotomy site, if the radial head was reduced and stable, the external fixator was removed during the out-patient visits (Fig. 1). If the radial head was not reduced, then open reduction of radial head and ALR was performed. Boyd approach or Henry approach was used to expose the radio-capitellar joint (RCJ). Any residual scar hindering the reduction was thoroughly debrided. The fascia of the triceps was used as the reconstructive material, and in some cases, a suture anchor was used for the fixation. After ALR, the stability of reduction was evaluated with passive pronation and supination intraoperatively. The joint capsule was then closed with absorbable sutures. After the open reduction, the elbow was immobilized at 90° flexion and full supination for 4 to 6 weeks (Fig. 2).
Figure 1.
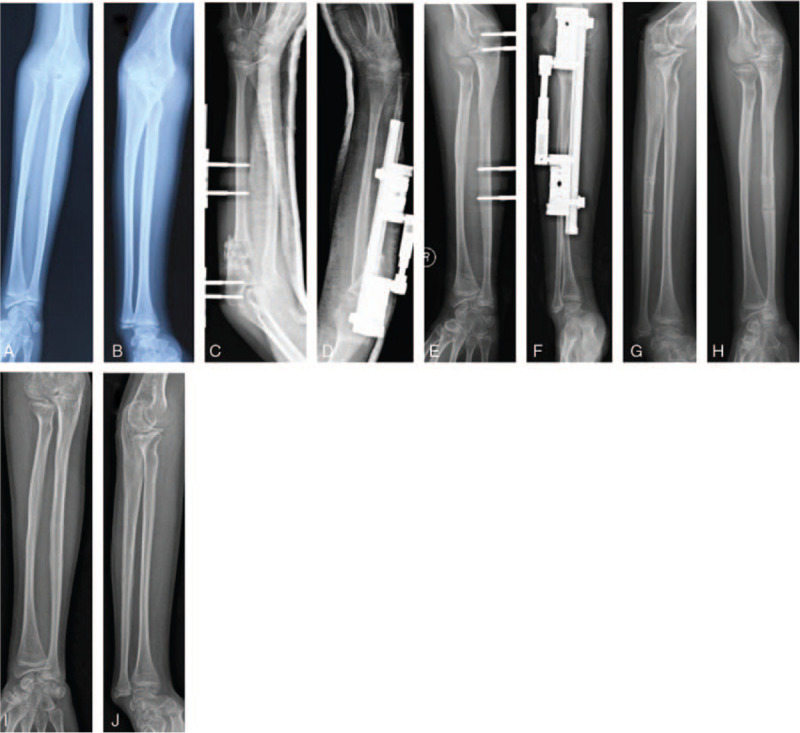
A 13-year-old boy of right Monteggia fracture treated with UO. A. AP view of the forearm, B. Lateral view of the forearm, C. AP view of the forearm after surgery, D. Lateral view of the forearm after surgery. E. AP view of the forearm at 3-month follow-up. F. Lateral view of the forearm at 3-month follow-up. G. AP view of the forearm after external fixator removal. H. Lateral view of the forearm after external fixator removal. I. AP view of forearm 3-month after fixator removal. J. Lateral view of forearm 3-month after fixator removal.
Figure 2.
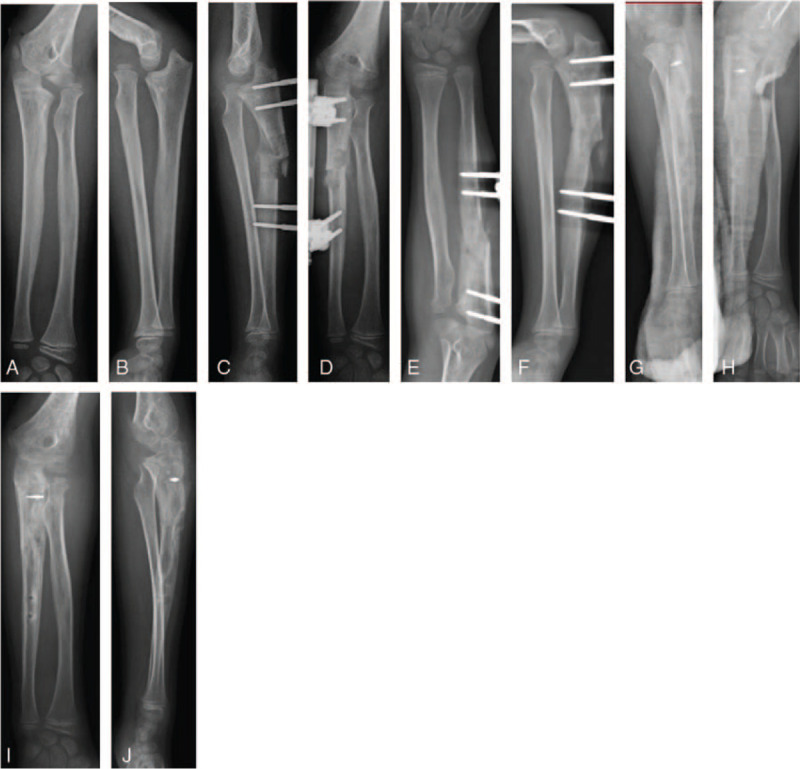
A 10-year-old boy of Monteggia fracture treated with UO + ALR. A, AP view of the forearm, B. Lateral view of the forearm, C. AP view of the forearm after surgery, D. Lateral view of the forearm after surgery, E. AP view of the forearm at 2-month follow-up, F. Lateral view of the forearm at 2-month follow-up, G. AP view of the forearm after external fixator removal and ALR, H. Lateral view of the forearm after external fixator removal and ALR, I. AP view of forearm 2-month after fixator removal and ALR, J. Lateral view of forearm 2-month after fixator removal and ALR.
2.2. Postoperative rehabilitation
After the removal of the slab, active rehabilitation was encouraged with or without the help of the physical therapists. All patients were followed up at out-patient visits at the interval of 2 to 3 months (Fig. 3).
Figure 3.

The appearance of an 11-year-old boy treated with UO+ALR. A. The appearance of the elbow at extension, B. The appearance of the elbow at flexion, C. The appearance of the elbow at pronation, D. The appearance of the elbow at supination.
3. Result
As shown in Table 1, the average age of the UO group (6.1 ± 2.3, year) was significantly younger than the ALR group (9.8 ± 2.8, year) (P < .001). No statistically significant differences were observed between the 2 groups concerning baseline information, including sex, operative side, Bado classification, follow-up time. Statistically significant difference was observed concerning the duration from initial injury to surgery between the UO group (8.6 ± 3.2 months) and ALR group (23.3 ± 12.6 months) (P < .001). There was no statistically significant difference between the UO group (67.6 ± 5.0) and ALR group (66.6 ± 4.4) (P = .51) group was observed according to the MEPS. Concerning the preoperative flexion, there was a significant difference between the UO group (108.1 ± 5.8) and ALR group (112.0 ± 6.1) (P = .047); with regard to the preoperative pronation, there was a significant difference between the UO group (69.3 ± 9.0) and ALR group (63.0 ± 8.7) (P = .034); there was no significant difference between the UO group and ALR group concerning extension (−1.8 ± 1.8; −2.2 ± 1.9) (P = .53) and supination (73.3 ± 4.3;71.9 ± 5.3) (P = .34).
Radiographs of the full-length forearm were used to validate the reduction of the radial head and the alignment of the upper extremity.
As shown in Table 2, concerning the the postoperative parameters including postoperative ROM of the joint, removal time of EF (6.7 ± 0.8, 6.9 ± 0.9 weeks (P = .55), lengthening (8.9 ± 2.5, 10.3 ± 2.5 mm) (P = .10) and MEPS (92.7 ± 2.1, 91.6 ± 2.1) (P = .08), there was no significant difference between the UO and ALR group.
Table 2.
Clinical parameters.
| Clinical outcomes | UO (n = 15) | ALR (n = 36) | P value |
| Post-op ROM of elbow | |||
| Extension | −1.8 ± 1.8 | −2.2 ± 1.9 | .53 |
| Flexion | 123.2 ± 5.0 | 126.0 ± 3.2 | .07 |
| Pronation | 88.6 ± 1.6 | 87.8 ± 1.7 | .12 |
| Supination | 87.1 ± 2.0 | 87.4 ± 1.8 | .68 |
| Removal (weeks) | 6.7 ± 0.8 | 6.9 ± 0.9 | .55 |
| Lengthening (mm) | 8.9 ± 2.5 | 10.3 ± 2.5 | .10 |
| Post-op MEPI Score | 92.7 ± 2.1 | 91.6 ± 2.1 | .08 |
As shown in Table 3, there were significant differences between preoperative and postoperative ROM of elbow joint and MEPS in both groups.
Table 3.
Clinical outcomes comparison.
| 3.1 Ulnar osteotomy alone | |||
| Clinical parameters | Pre-op | Post-op | P value |
| ROM of Elbow | |||
| Extension | −1.8 ± 1.8 | −1.8 ± 1.8 | >.999 |
| Flexion | 108.1 ± 5.8 | 123.2 ± 5.0 | <.001 |
| Pronation | 69.3 ± 9.0 | 88.6 ± 1.6 | <.001 |
| Supination | 73.3 ± 4.3 | 87.1 ± 2.0 | <.001 |
| MEPI Score | 67.6 ± 5.0 | 92.7 ± 2.1 | <.001 |
| 3.2 Ulnar osteotomy + OR + ALR | |||
| Clinical parameters | Pre-op | Post-op | P value |
| ROM of Elbow | |||
| Extension | −2.2 ± 1.9 | −2.2 ± 1.9 | >.999 |
| Flexion | 112.0 ± 6.1 | 126.0 ± 3.2 | <.001 |
| Pronation | 63.0 ± 8.7 | 87.8 ± 1.7 | <.001 |
| Supination | 71.9 ± 5.3 | 87.4 ± 1.8 | <.001 |
| MEPI Score | 66.6 ± 4.4 | 91.6 ± 2.1 | <.001 |
4. Discussion
The two-stage strategy achieved the spontaneous reduction of RHD without ALR in selected patients. In patients without spontaneous reduction of the radial head, open reduction and ALR can be easily obtained in stage 2 with the normalized length of the ulna.
In pediatric patients with persistent dislocated radial head, surgical interventions are usually recommended since RHD may lead to loss of flexion and forearm rotation and malformation of the radial head.[11] Certain authors recommend the open reduction of RHD with or without ALR.[11–13] This approach is effective if the time from injury is less than 4 to 6 months, and the shape of the ulna is not compromised.[14,15] Besides, reduction without exposing the RCJ has also been reported using ulnar lengthening angulation osteotomy.[16,17] Moreover, certain authors recommend UO combined with open reduction of RHD.[18–20] Although all the authors reported improved outcomes after surgeries, complications are common, including radial head subluxation and instability.
In our medical center, one-stage operation, including UO with angulation and lengthening, with or without ALR, with or without radius shortening, was performed before 2010. But the outcomes were not always satisfactory, consistent with reports by certain authors.[7,21–22] UO is based on the concept that the abnormal shape of the ulna prevents the reduction of the radial head, and tightening the interosseous membrane through ulnar angulation and lengthening can return the radial head to an acceptable position or even complete reduction. However, the intraoperative distraction of the ulna is limited, and in certain cases, acute osteotomy with angulation and lengthening is unable to reduce the radial head. Over-distraction during the surgery increased the risk of delayed union or nonunion of osteotomy site, nerve palsy and postoperative compartment syndrome.[7,16–18,23] Besides, the gap of the osteotomy site should be filled with bone graft.[7,23]
UO with angulation and gradual distraction using a unilateral external fixator is a less invasive approach without extensive exposure.[24,25] The angulation was calculated before the surgery; however, the angulation might not be maintained as planned since the external fixator cannot provide rigid stability. Gradual lengthening overcame the soft tissue contracture, reduced the risk of delayed union or nonunion, and lowered the incidence of nerve palsy and compartment syndrome.[25] There was no patient with delayed union or nonunion in our study, and the incidence of nerve palsy was nil. The potential disadvantages of external fixator included pin tract infection (PTI) and the inconvenience of wearing clothes. In this study, all patients of PTI were easily ameliorated by oral antibiotics.
Many authors recommend open reduction and repair or reconstruction of the annular ligament.[7,12,23] However, in surgical exploration, the remnants of the annular ligament are usually difficult to recognize. In order to facilitate the reduction of the radial head, the fibrous scarring tissue needs to be removed, and ALR might be performed simultaneously. The reconstruction materials included the forearm fascia,[26] palmaris longus,[27] and triceps tendon.[28] At our institute, the fascia of the triceps tendon was used as reconstruction material. In our study, no severe complications such as a noticeable restriction of forearm rotation and radial head necrosis were observed during the follow-up.
Certain authors advocated open reduction without ALR,[29,30] and they emphasized the importance of restoring the normal alignment of the ulna. As for our study, in stage 2, after removing the fibrous scarring tissue, all the radial head could be easily reduced. However, it was not very stable. Therefore, ALR was performed to reduce the incidence of delayed subluxation or instability. Besides, trans-capitellar Kirschner wire was not used at our institute because of its futility of maintaining stability and its possibility of breakage.[3] The incidence of subluxation and redislocation in our study was quite low.
It is reported that the radial head shifts more as the angulation of ulna increased,[7,19,23] consistent with our findings. There was no clarified indication that the osteotomy should be performed at the maximum of deformity[24] or as proximal as possible.[7] A higher rate of delayed union and nonunion, reduced rotation of forearms, and a reduced shift of the radial head were observed in the UO at the distal level.[15] Therefore, in our study, the osteotomy site was determined by the insertion of proximal pins, and it should be as proximal as possible. As shown in the result, the decreased rotation of the forearms was not noticeable.
In our study, 30% of patients manifested spontaneous reduction of radial head after ulnar lengthening. After removing the external fixator, the reduction of the radial head was stable during the rotation of the forearm. Compared with the patient receiving open reduction and ALR, patients with a spontaneous reduction of RHD displayed similar postoperative elbow function.
Although the angulation of UO was calculated preoperatively, but it is often necessary to over-correct the ulna dorsal angulation.[7] The normal ulnar dorsal angulation angle in children during the growth has not been thoroughly investigated. The over-correction of dorsal angulation and distraction cannot be meticulously planned and executed. It might be the cause of different outcomes of the UO. Besides, abundant scarring tissue or heterotopic bone formation might also prevent the spontaneous reduction of the radial head. As for patients without spontaneous reduction after lengthening, we performed open reduction + ALR when removing the external fixator.
Our result showed a significant difference between the UO group and ALR group concerning the age of surgery and the duration from initial injury to surgery. Therefore, in younger children with a shorter history of injury, there might be no need for open reduction and ALR.
The limitations of our study include the small sample size and the retrospective nature without long-term follow-up. It is a rare condition, and larger series from multiple centers might deliver a more convincing conclusion.
5. Conclusion
The two-stage strategy is a reasonable choice for selected patients with long-lasting RHD with ulnar deformity.
Author contributions
Conceptualization: Pan Hong.
Data curation: Xiaolong Zhao, Qi Zhang.
Formal analysis: Yuhong Ding, Ruikang Liu.
Investigation: Xiaolong Zhao.
Methodology: Yuhong Ding, Xin Tang.
Resources: Renhao Ze.
Software: Yuhong Ding, Ruikang Liu.
Writing – original draft: Pan Hong.
Writing – review & editing: Jin Li, Xiaolong Zhao, Saroj Rai, Pan Hong.
Footnotes
Abbreviations: ALR = annular ligament reconstruction, RCJ = radio-capitellar joint, RHD = radial head dislocation, UO = ulnar osteotomy.
How to cite this article: Li J, Zhao X, Rai S, Ding Y, Zhang Q, Ze R, Tang X, Liu R, Hong P. Two-stage strategy for neglected Monteggia fracture in children: a retrospective study of 51 patients. Medicine. 2021;100:10(e25129).
JL and XZ have contributed equally to this work.
The authors have no funding and conflicts of interests to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Goyal T, Arora SS, Banerjee S, et al. Neglected Monteggia fracture dislocations in children: a systematic review. J Pediatr Orthop B 2015;24:191–9. [DOI] [PubMed] [Google Scholar]
- [2].Hubbard J, Chauhan A, Fitzgerald R, et al. Missed pediatric Monteggia fractures. JBJS Rev 2018;6:e2. [DOI] [PubMed] [Google Scholar]
- [3].Chin K, Kozin SH, Herman M, et al. Pediatric Monteggia fracture-dislocations: avoiding problems and managing complications. Instr Course Lect 2016;65:399–407. [PubMed] [Google Scholar]
- [4].Gyr BM, Stevens PM, Smith JT. Chronic Monteggia fractures in children: outcome after treatment with the Bell-Tawse procedure. J Pediatr Orthop B 2004;13:402–6. [DOI] [PubMed] [Google Scholar]
- [5].Horii E, Nakamura R, Koh S, et al. Surgical treatment for chronic radial head dislocation. J Bone Joint Surg Am 2002;84A:1183–8. [DOI] [PubMed] [Google Scholar]
- [6].Rahbek O, Deutch SR, Kold S, et al. Long-term outcome after ulnar osteotomy for missed Monteggia fracture dislocation in children. J Child Orthop 2011;5:449–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Nakamura K, Hirachi K, Uchiyama S, et al. Long-term clinical and radiographic outcomes after open reduction for missed Monteggia fracture-dislocations in children. J Bone Joint Surg Am 2009;91:1394–404. [DOI] [PubMed] [Google Scholar]
- [8].Stragier B, De Smet L, Degreef I. Long-term follow-up of corrective ulnar osteotomy for missed Monteggia fractures in children. J Shoulder Elbow Surg 2018;27:e337–43. [DOI] [PubMed] [Google Scholar]
- [9].Di Gennaro GL, Martinelli A, Bettuzzi C, et al. Outcomes after surgical treatment of missed Monteggia fractures in children. Musculoskelet Surg 2015;99:S75–82. [DOI] [PubMed] [Google Scholar]
- [10].Schneeberger AG, Kösters MC, Steens W. Comparison of the subjective elbow value and the Mayo elbow performance score. J Shoulder Elbow Surg 2014;23:308–12. [DOI] [PubMed] [Google Scholar]
- [11].Çevi KHB, Yuvaci F, Ecevi ZE, et al. Four different management strategies in missed Monteggia lesions in children. J Orthop 2020;21:207–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Mohan Kumar EG, Yathisha Kumar GM, Noorudheen M. Functional outcome of Bell Tawse procedure for the management of chronic unreduced Monteggia fracture-dislocation in children. Indian J Orthop 2019;53:745–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Chen HY, Wu KW, Dong ZR, et al. The treatment of chronic radial head dislocation in Monteggia fracture without annular ligament reconstruction. Int Orthop 2018;42:2165–72. [DOI] [PubMed] [Google Scholar]
- [14].He JP, Hao Y, Shao JF. Comparison of treatment methods for pediatric Monteggia fracture: met vs missed radial head dislocation. Medicine (Baltimore) 2019;98:e13942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Zheng ET, Waters PM, Vuillermin CB, et al. Surgical reconstruction of missed Monteggia lesions in children. J Pediatr Orthop 2020;40:e916–21. [DOI] [PubMed] [Google Scholar]
- [16].Kawoosa AA, Dhar SA, Butt MF, et al. Stable relocation of the radial head without annular ligament reconstruction using the Ilizarov technique to treat neglected Monteggia fracture: two case reports. J Med Case Rep 2010;4:344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gallone G, Trisolino G, Stilli S, et al. Complications during the treatment of missed Monteggia fractures with unilateral external fixation: a report on 20 patients in a 10-year period in a tertiary referral center. J Pediatr Orthop B 2019;28:256–66. [DOI] [PubMed] [Google Scholar]
- [18].Hayami N, Omokawa S, Iida A, et al. Effect of soft tissue injury and ulnar angulation on radial head instability in a Bado type I Monteggia fracture model. Medicine (Baltimore) 2019;98:e17728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Eamsobhana P, Chalayon O, Kaewpornsawan K, et al. Missed Monteggia fracture dislocations treated by open reduction of the radial head. Bone Joint J 2018;100-B:1117–24. [DOI] [PubMed] [Google Scholar]
- [20].Take M, Tomori Y, Sawaizumi T, et al. Ulnar osteotomy and the Ilizarov mini-fixator for pediatric chronic monteggia fracture-dislocations. Medicine (Baltimore) 2019;98:e13978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lu X, Yan G, Wang Y, et al. Repositioning of the annular ligament in the management of missed Monteggia fracture. J Pediatr Orthop 2017;37:20–2. [DOI] [PubMed] [Google Scholar]
- [22].Xu Z, Li Y, Wang Z, Cai H. Open reduction combined with CORA-based osteotomy of the ulna in the treatment of missed Bado type I Monteggia injury: a retrospective study of 5 cases. Medicine (Baltimore) 2017;96:e8609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Datta T, Chatterjee N, Pal AK, et al. Evaluation of outcome of corrective ulnar osteotomy with bone grafting and annular ligament reconstruction in neglected monteggia fracture dislocation in children. J Clin Diagn Res 2014;8:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Bae DS. Successful strategies for managing Monteggia injuries. J Pediatr Orthop 2016;36:67–70. [DOI] [PubMed] [Google Scholar]
- [25].Bor N, Rubin G, Rozen N, et al. Chronic anterior Monteggia lesions in children: report of 4 cases treated with closed reduction by ulnar osteotomy and external fixation. J Pediatr Orthop 2015;35:7–10. [DOI] [PubMed] [Google Scholar]
- [26].Wang MN, Chang WN. Chronic posttraumatic anterior dislocation of the radial head in children: reconstruction through a Boyd incision. J Orthop Trauma 2006;20:1–5. [DOI] [PubMed] [Google Scholar]
- [27].Kim HT, Park BG, Suh JT, et al. Chronic radial head dislocation in children, part 2: results of open treatment and factors affecting final outcome. J Pediatr Orthop 2002;22:591–7. [PubMed] [Google Scholar]
- [28].Hirayama T, Takemitsu Y, Yagihara K, et al. Operation for chronic dislocation of the radial head in children. Reduction by osteotomy of the ulna. J Bone Joint Surg Br 1987;69:639–42. [DOI] [PubMed] [Google Scholar]
- [29].Bhaskar A. Missed Monteggia fracture in children: is annular ligament reconstruction always required? Indian J Orthop 2009;43:389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Rajasekaran S, Venkatadass K. Sliding angulation osteotomy: preliminary report of a novel technique of treatment for chronic radial head dislocation following missed Monteggia injuries. Int Orthop 2014;38:2519–24. [DOI] [PubMed] [Google Scholar]


