Abstract
Laryngeal injury from intubation can substantially impact airway, voice, and swallowing, thus necessitating multidisciplinary interventions. The goals of this systematic review were: (1) to review the types of laryngeal injuries and their patient-reported symptoms and clinical signs resulting from endotracheal intubation in patients intubated for surgeries and (2) to better understand the overall the frequency at which these injuries occur. We conducted a search of 4 online bibliographic databases (i.e., PubMed, Embase, Cumulative Index of Nursing and Allied Health Literature (CINAHL), and The Cochrane Library) and ProQuest and Open Access Thesis Dissertations (OPTD) from database inception to September 2019 without restrictions for language. Studies that completed post-extubation laryngeal examinations with visualization in adult patients who were endotracheally intubated for surgeries were included. We excluded: 1) retrospective studies, 2) case studies, 3) pre-existing laryngeal injury/disease, 4) patients with histories of or surgical interventions that risk injury to the recurrent laryngeal nerve, 5) conference abstracts, and 6) patient populations with non-focal, neurological impairments that may impact voice and swallowing function, thus making it difficult to identify isolated post-extubation laryngeal injury. Independent, double-data extraction, and risk of bias assessment followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and the Cochrane Collaboration’s criteria. Twenty-one articles (1 cross-sectional, 3 cohort, 5 case series, 12 randomized controlled trials) representing 21 surgical studies containing 6140 patients met eligibility criteria. The mean patient age across studies reporting age was 49 (95%CI: 45, 53) years with a mean intubation duration of 132 (95%CI: 106, 159) minutes. Studies reported no injuries in 80% (95%CI: 69%, 88%) of patients. All 21 studies presented on type of injury. Edema was the most frequently reported mild injury, with a prevalence of 9-84%. Vocal fold hematomas were the most frequently reported moderate injury, with a prevalence of 4% (95%CI: 2%, 10%). Severe injuries that include subluxation of the arytenoids and vocal fold paralysis are rare (<1%) outcomes. The most prevalent patient complaints post-extubation were dysphagia (43%), pain (38%), coughing (32%), a sore throat (27%), and hoarseness (27%). Overall, laryngeal injury from short-duration surgical intubation is common and is most often mild. No uniform guidelines for laryngeal assessment post-extubation from surgery are available and hoarseness is neither a good indicator of laryngeal injury or dysphagia. Protocolized screening for dysphonia and dysphagia post-extubation may lead to improved identification of injury and, therefore, improved patient outcomes and reduced healthcare utilization.
Keywords: endotracheal intubation, surgery, larynx, voice, deglutition, dysphagia, injury
INTRODUCTION
Globally, more than 320 million patients undergo surgical procedures each year.1,2 In the United States, approximately 30% of surgeries require orotracheal intubation.3 The placement of an endotracheal tube (ETT) for surgery is most often a planned and controlled procedure. Despite considerable skill, adequate preparation, good execution, and optimized environments, placement of an ETT may result in both short- and long-term consequences. In turn, these consequences may require additional and unplanned medical care after extubation.
Post-extubation patient complaints frequently include voice dysfunction (dysphonia), voice loss (aphonia), sore throat, and swallowing dysfunction (dysphagia).4-7 These complaints are often dismissed or overlooked, owing to the frequent observation that they are temporary.8 Laryngeal injuries are also believed to be minor, often going unevaluated despite the fact that more severe injuries and complications can occur.4,6-10 As data emerge that support an association between duration of intubation and subsequent laryngeal injury,4,11-13 it is clear that awareness of potential injury needs to extend to short-term intubation as well.
Many referrals for evaluation of laryngeal injury/voice dysfunction will occur after being present for 1 week,14-16 even as long as 2-3 months in the setting of ongoing symptoms.17-19 Despite more than 100 years of intubation during surgery,4 no standard practice for post-extubation assessment of laryngeal injury/dysphonia/dysphagia exists. Patients with laryngeal injuries are at risk for long-term functional impairment in critical laryngeal functions of voice, swallow, and airway. For example, both delayed-onset laryngeal stenosis20,21 and chronic dysphonia22 are reported after intubation injury.
The goals of this systematic review were: (1) to review the types of laryngeal injuries and their patient-reported symptoms and clinical signs resulting from endotracheal intubation in patients intubated for surgeries and (2) to better understand the prevalence at which these injuries and their symptoms occur. This prevalence systematic review specifically encompasses prospective studies with post-extubation laryngeal visualization.
MATERIALS AND METHODS
This systematic review on laryngeal injury post-extubation in patients after surgery followed methodology used for a separate systematic review of laryngeal injury following prolonged intubation in the intensive care unit (ICU).11
Literature Search
In consultation with a content expert (M.B.B.), a clinical informationist (C.P.) created the search strategy. This strategy was executed using 4 electronic bibliographic databases from their inception to April 2016: PubMed, Embase, Cumulative Index of Nursing and Allied Health Literature (CINAHL), and Cochrane Library. Three updates (i.e., March 2017, September 2017, September 2019) were completed (Supplemental Table 1) and ProQuest, and Open Access Thesis Dissertations as part of the gray literature. Controlled vocabulary supplied by each electronic database (e.g., Medical Subject Headings, Emtree terms, and CINAHL headings) was supplemented with keywords for the broad concepts of intubation, methods of visualization, and injury. This systematic review focused on all prospective study designs that included adult humans. Pediatrics-focused research terms were excluded from titles only. Animal only research was filtered out. A research filter was applied based on the Cochrane Highly Sensitive Search Strategy for identifying randomized trials in MEDLINE, sensitivity and precision-maximizing version23 with additions for other types of clinical studies.
Selection Criteria
Inclusion criteria included: 1) prospective studies other than case studies, 2) adult (≥18 years old) patients who underwent scheduled surgical procedures requiring oral endotracheal intubation, 3) completed laryngoscopic evaluations using direct (e.g., line of sight) or indirect (e.g., flexible endoscopy) visualization of the larynx post-extubation, and 4) studies that reported sufficient data on laryngeal injury (e.g., frequency, nature). Exclusion criteria included: 1) retrospective studies, 2) case studies, 3) pre-existing laryngeal injury/disease, 4) patients with histories of or surgical interventions presented in the research study that risk injury to the recurrent laryngeal nerve (e.g., neck surgeries, open thoracic surgeries), 5) conference abstracts, and 6) patient populations with non-focal, neurological impairments that may impact voice and swallowing function, making it difficult to identify isolated post-extubation laryngeal injury (e.g., stroke, Parkinson’s disease).
Data Extraction/Risk of Bias Assessment
For the original search and for each update, either one of the authors (M.B.B.) or the clinical informationist (C.P.) imported the search strategy results to an online platform (Covidence: www.covidence.org, Melbourne, Victoria, Australia) for independent review. Each entry was independently screened by title, abstract, and full text by 2 authors (B.B., E.J.). Disagreements were independently resolved by a third author (M.B.B.), masked to the decision by each of the screeners. Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, double-data extraction and risk of bias assessment were independently completed by 6 authors (L.M.A., M.B.B., G.C., E.J., M.J.L., V.P.). The Cochrane Collaboration’s criteria24 was used to determine risk of bias. Each of the 7 risk parameters (plus 2 additional criteria for randomized controlled trials) was judged as low-, unknown-, or high risk. Accuracy of all data was confirmed by at least 2 authors and disagreements were resolved by consensus. Attempts to contact corresponding authors to provide missing data and clarifications were made as needed. Across the accepted articles there was large variability of study methods, including ETT modifications, use of pharmacologic agents, and changes in overall patient management. Based on this variability, we made the a priori decision to look only at the control groups/standard of care groups in an attempt to minimize the potential occurrence of confounding variables that may be related to laryngeal injury (Supplemental Table 2). Despite these efforts, a substantial heterogeneity among the accepted studies remained.
Borrowing from the literature, we adapted a 4-step grading rubric to classify laryngeal injuries (Table 1).25-27 This rubric was updated via consensus validation by 5 authors: 3 laryngologists (L.M.A., S.R.B., A.T.H.), an emergency medicine physician (M.J.L.), and a speech-language pathologist (M.B.B.). We calculated prevalence as the total number of patients with each laryngeal injury or symptom divided by the total number of subjects analyzed for each of these particular outcomes across studies. Post-extubation outcomes not reported were excluded from prevalence calculations. Because all studies did not evaluate the same outcomes relative to either laryngeal injury or patient symptoms, denominators for prevalence calculations differ across categories. Any outcome assessed prior to extubation was not included. Many studies reported voice quality using terminology that was inconsistent across studies. As a result, we report dysphonia, aphonia, and hoarseness separately for purposes of prevalence. Collectively, however, we grouped these symptoms of laryngeal injury as “voice dysfunction” for purposes of discussion. Two additional terms, pain and sore throat, have similar meanings and were likewise grouped.
Table 1.
Prevalencea of laryngeal injury by grade after extubation.
| GRADE/Injury | Patients | Study N | Studies Reporting: Count (%) |
Prevalence: % (95%CI) |
|---|---|---|---|---|
| GRADE 0 | ||||
| No injury | 2052 | 2328 | 16 (76) | 80 (69, 88) |
| GRADE I | ||||
| Arytenoid edema | 42 | 50 | 1 (5) | 84 |
| Vocal process(es) erythema | 15 | 23 | 1 (5) | 65 |
| Tracheal irritation | 52 | 100 | 1 (5) | 52 |
| Interarytenoid edema | 34 | 73 | 2 (10) | 47 |
| Vocal process(es) edema | 4 | 23 | 1 (5) | 17 |
| Reinke space edema | 7 | 53 | 1 (5) | 13 |
| Edema | 91 | 574 | 8 (38) | 11 (3, 35) |
| Interarytenoid erythema | 2 | 23 | 2(10) | 9 |
| Post-cricoid edema | 2 | 23 | 1 (5) | 9 |
| Erythema | 59 | 581 | 5 (24) | 8 (2, 30) |
| Subglottic mucosa erythema | 2 | 123 | 2 (10) | 2 |
| GRADE II | ||||
| Thickening of vocal folds | 16 | 116 | 3 (14) | 10 (0.3, 83) |
| Ulceration | 10 | 100 | 1 (5) | 10 |
| Inter-arytenoid fibrin | 11 | 123 | 2 (10) | 9 |
| Vocal process(es) fibrin | 2 | 23 | 1 (5) | 9 |
| Hematoma, petichiae | 122 | 2368 | 13 (62) | 4 (2, 10) |
| Granuloma/granulation | 3 | 186 | 2 (10) | 2 |
| Laceration | 12 | 1475 | 2 (10) | 1 |
| Vocal process(es) ulceration | 0 | 23 | 1 (5) | 0 |
| GRADE III | ||||
| Paralysis | 9 | 3878 | 4 (19) | 0.4 (0.1, 3) |
| Subluxation | 4 | 4093 | 2 (10) | 0.1 |
Abbreviation: CI, confidence interval
Estimated average prevalence (95% confidence intervals) were computed by applying the inverse-logit transformation. Confidence intervals were calculated only for injuries reported by ≥3 studies. Raw data are available in Electronic Supplementary Material 3.
Statistical Methods
Pooled estimates of the average patient age and duration of intubation were estimated using linear random effects models including a random intercept for each study, an overall intercept (the pooled estimate) and study-specific, known variance estimates. For studies with average age reported as median and interquartile range or range, the mean and standard deviation were estimated using existing methods.28 For injury types reported in at least three studies, similar linear random intercept regression models were used for the log odds of each injury (logit transformation of injury prevalence). The estimated pooled prevalence and 95% confidence intervals were computed by applying the inverse-logit transformation. Similar models were used to compute the prevalence of each symptom reported in at least three studies. For injuries/symptoms reported in only two studies, the prevalence was calculated by dividing the total number of patients with the injury/symptom by the total sample size, with the total taken across the two studies. SAS® version 9.4 (2016, Cary, NC) was used to conduct all analyses.
RESULTS
Search Results
After an original search and three updates, 6754 publications were identified from the 4 databases and other sources. Screening by title and abstract resulted in 160 full-text reviews. After the September 2019 search update, ICU studies were excluded from the search; thus, there is no update to the final count of ICU studies. Of these 160 full-text reviews, 21 surgical studies were accepted (Figure 1) and included 6140 patients from 1 cross-sectional study,29 3 cohort studies,4,6,30 5 case series,31-35 and 12 randomized controlled trials (RCT).7,9,36-45 Of the 12 RCTs, 4 (33%) studies were registered clinical trials with ClinicalTrials.gov (Table 2).41-44
Figure 1. Study selection flowchart.
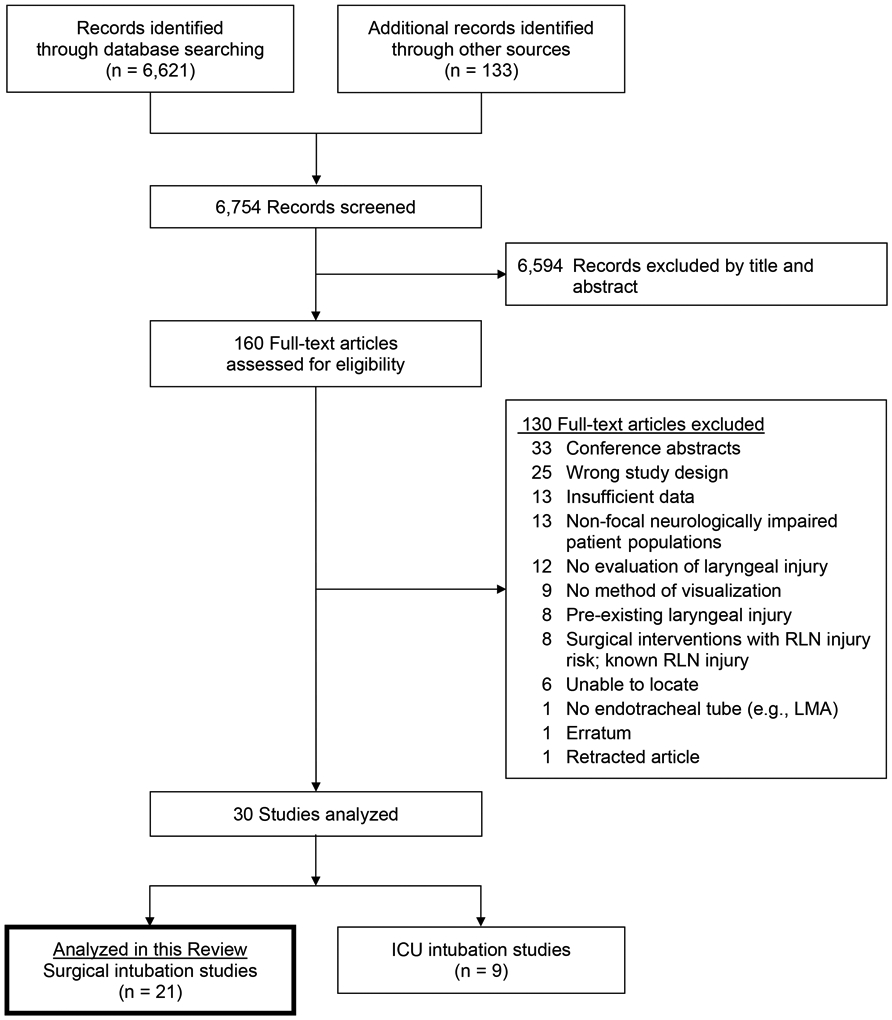
Abbreviations: LMA, laryngeal mask airway; RLN, recurrent laryngeal nerve
Table 2.
Summary of included studies.
| Author/Year | Country | Study Design | Number of patients analyzeda |
Mean Patient Age (years) |
ETT size | Method of Visualization |
Intubation Duration (minutes) |
|---|---|---|---|---|---|---|---|
| Alexopoulos 19839 | Sweden | RCT | 100 | NR | NR | Direct | 180 |
| Baillard 200530 | France | Cohort | 612 | 49 | 7.0-7.5 | Indirect | 120 |
| Beckford 19904 | United States | Cohort | 9 | 33 | NR | Indirect | 66 |
| Böttcher 201436 | Germany | RCT | 53 | 48 | 7.0-8.5 | Stroboscopy | 98 |
| Friedrich 200031 | Germany | Case Series | 210 | 57 | 7.5-8.5 | Indirect | 145 |
| Geraci 20136 | Italy | Cohort | 50 | 57 | NR | Indirect | 160 |
| Heidegger 200737 | Switzerland | RCT | 129 | 54 | 7.0-8.0 | Indirect | NR |
| Kambič 197832 | Yugoslavia | Case Series | 1000 | NR | NR | Stroboscopy | NR |
| Lesser 198733 | Wales | Case Series | 5 | 48 | 8.0-9.0 | Indirect | 80 |
| Mencke 200338 | Germany | RCT | 36 | 48 | 7.5-8.5 | Stroboscopy | 65 |
| Mencke 2006 (Rocuronium)39 | Germany | RCT | 150 | 50 | 7.0-8.0 | Stroboscopy | 93 |
| Mencke 2006 (Timing)40 | Germany | RCT | 25 | 39 | 7.0-8.0 | Stroboscopy | 146 |
| Mencke 201341 | Germany | RCT | 29 | 49 | 7.0-8.0 | Stroboscopy | 94 |
| Nordang 20167 | Sweden | RCT | 22 | 58 | 7.0-8.0 | Indirect | 1320 |
| Ovari 201742 | Germany | RCT | 87 | 51 | 7.0-8.0 | Indirect | 98 |
| Peppard 198334 | United States | Case Series | 475 | 47 | 8.0-9.0 | Indirect | 120 |
| Seo 201643 | Korea | RCT | 70 | 57 | NR | Indirect | 194 |
| Sørensen 201344 | Denmark | RCT | 55 | 49 | 7.0-8.0 | Indirect | 120 |
| Walts 198029 | United States | Cross Sectional | 100 | NR | 6.0-9.5 | Direct | 156 |
| Yamanaka 200935 | Japan | Case Series | 3093 | 53 | 7.5-8.0 | Stroboscopy | 283 |
| Zimmert 199945 | Germany | RCT | 22 | 29 | NR | Indirect | 87 |
Abbreviations: ETT, endotracheal tube; NR, not reported; RCT, randomized controlled trial
Reflects the number of patients meeting inclusion/exclusion criteria for this systematic review, and therefore analyzed and reported in this systematic review.
Patient Demographics and Presentation
There was 1 (5%) study that did not report the type of surgery performed.35 The remaining 20 (95%) studies completed surgeries and imposed inclusion/exclusion criteria that did not involve areas associated with the pharynx, larynx, or procedures that may have affected function of either of these two anatomical areas. Studies that included head and neck surgeries largely focused on eye, ear, or nasal procedures. Other studies included surgeries unrelated to the head and neck (e.g., extremities, gynecological, orthopedic, abdominal, vascular).
Six (29%) studies targeted reduction of symptom severity through evaluation of different medications during intubation.37-42 Four (19%) studies tested changing the shape of the ETT7,9,44 or its pliability.43 In all 10 (48%) of these aforementioned studies, prevention of injury and/or symptoms was the goal. The remaining 11 (52%) studies determined prevalence of injury without intervention, assessed various pharmacologic approaches to improve laryngeal exposure, characterized patient symptoms and voice quality, and assessed laryngeal injury as part of this effort.4,6,29-36,45 The mean patient age was 49 (95% confidence interval [95%CI]: 45, 53) years was similar across the 18 (86%) studies reporting age.4,6,7,30,31,33-45 The mean intubation duration for 19 (90%) studies4,6,7,9,29-31,33-36,38-45 that reported this variable was 132 (95%CI: 106, 159) minutes, excluding one study that included the post-operative intubation period with a mean intubation duration of 22 (range: 12 - 52; SD = 8) hours.7
Endotracheal Tube Characteristics
There were 16 (76%) studies that reported ETT size,7,29-31,33-42,44,45 12 (75%) that distinguished ETT size between the sexes with females receiving an inner diameter 0.5 mm30,33,35 − 1.0 mm7,33,37-42,44,45 smaller than males. Most often, males received an 8.0 ETT and females received a 7.0 ETT.7,37,39-42,44 Four different ETT manufacturers were reported in 11 (52%) studies.7,32,33,36,37,39,40,42-45 Only 8 (38%) studies reported both ETT size and manufacturer.7,33,36,37,39,40,42,44
Post-extubation Laryngeal Evaluation
All studies reported the type of visualization of the larynx and surrounding tissues that was performed. Direct visualization occurred in 2 (10%) studies9,29 and indirect visualization occurred in 19 (90%) studies (Table 2).4,6,7,30-45 Of the 19 studies using indirect visualization, 9 (47%) used stroboscopy, allowing for observations specific to vocal fold vibration. Post-extubation assessment was completed immediately in 6 (30%) studies,9,29,32,34,43,45 ≤24 hours in 12 (60%) studies,4,6,7,30,33,36-38,40-42,44 and ≤3 days in 1 (5%) study.39 Two (10%) studies extended initial follow-up beyond 3 days.31,35 Interpretation of findings was performed in 13 (57%) studies by an otolaryngologist,7,30,31,35,37-44 in 1 (5%) study by an anesthesiologist,9 and in 1 (5%) study by both an otolaryngologist and a thoracic surgeon.6 The remaining 7 (35%) studies did not report the evaluator’s training.4,29,32-34,45
Post-extubation Laryngeal Injuries – Short Duration Follow-up
Five studies (25%) did not report on the number of patients without laryngeal injury, either due to a requisite period for screening patients with symptoms,30,35,39 observation of select injury types,29 or unclear reporting,6 and reported only individual outcomes. Therefore, prevalence of injury is derived from the 16 (76%) studies that reported patients with and without injury.4,7,9,31-34,36-38,40-45 Of these, 2052/2328 (80%, 95%CI: 69%, 88%) patients did not present with laryngeal injury post-extubation. Follow-up durations for 2 studies exceeded 4 days and were not considered in this calculation due to the potential for recovery of some injuries within the 4-23 day window.31,35
Studies often did not distinguish whether there was co-occurrence of multiple injuries or each injury was isolated. The prevalence reported in this systematic review makes no assumption that each patient experienced a single injury. A high prevalence of minor injury and reduced prevalence of more severe injury was observed (Table 1; Supplemental Table 3). The majority of laryngeal injuries were self-limiting, Grade I injuries. Edema (in various forms) was the most frequently reported injury, with a prevalence ranging 9% - 84% across 9 (45%)4,6,7,9,36,39,42-44 studies. The most frequently reported moderate (i.e., Grade II) injury was hematoma, with a 4% (95%CI: 2%, 10%) prevalence across 13 (62%) studies.4,29,31,32,34,37-40,42-45 Severe injuries (i.e., Grade III) were reported in 5 (24%) studies reporting these outcomes.29,31,32,34,35 These 13 patients included 4 patients with subluxation (prevalence: 0.1%) of an arytenoid cartilage35,37 and 9 patients with vocal fold paralysis (prevalence: 0.4%, 95%CI: 0.1%, 3%).31,34,35
Post-extubation Laryngeal Injuries – Long Duration Follow-up
Initial follow-up in 2 studies was extended beyond 3 days post-extubation, questioning the potential for not being able to identify injuries that resolved during this period.31,35 The 210-patient case series by Friedrich completed initial evaluations in 4-9 days post-extubation on all patients with the goal of determining laryngeal injuries post-extubation,31 but no detail was provided for the distribution of this time. The 3093-patient case series by Yamanaka had the goals of determining the duration of hoarseness and the final outcome of patients with hoarseness lasting >7 days.35 Laryngoscopic evaluations were only completed on 25 (0.8%) patients with hoarseness lasting >7 days. Of these, 7 (28%) patients were unable to be followed and an additional 2 (8%) patients were not done. Among the 16 (64%) remaining patients who were evaluated post-extubation, the median follow-up time was 13.5 (interquartile range: 8, 15) days.
Post-extubation Patient Symptoms
There were 16 (76%) studies that reported post-extubation symptoms of laryngeal injury.6,7,9,30,34-45 However, the specific types of symptoms were inconsistently reported across studies (Table 3; Supplemental Table 4). The most frequently reported symptom was hoarseness, with a 27% (95%CI: 12%, 50%) prevalence.6,7,34-45 Pain and sore throat were studied in 11 (52%) studies, reporting a 38% (95%CI: 0.5%, 99%) prevalence and 27% (95%CI: 16%, 42%) prevalence, respectively.6,7,9,30,34,39-43,45 Although dysphagia was not studied widely, only 3 (14%) studies, it had a large average prevalence of 43% (95%CI: 21%, 68%) prevalence.6,7,45 No additional information was provided about the impact of dysphagia on patient safety, (i.e., aspiration, aspiration pneumonia) or other patient outcomes (e.g., altered diets). Other areas of inquiry, such as cough, aphonia, and dyspnea were infrequently reported.
Table 3.
Prevalencea of signs/symptoms reported after extubation.
| Sign/Symptom | Patients | Study N | Studies Reporting: Count (%) |
Prevalence % (95% CI) |
|---|---|---|---|---|
| dysphagia | 41 | 95 | 3 (14) | 43 (21, 68) |
| pain | 91 | 670 | 4 (19) | 38 (0.5, 99) |
| cough | 39 | 123 | 2 (10) | 32 |
| sore throat | 363 | 1427 | 10 (48) | 27 (16, 42) |
| hoarseness | 1173 | 4297 | 14 (67) | 27 (12, 50) |
| dysphonia | 31 | 491 | 3 (14) | 17 (0.0, 99) |
| laryngeal dyspnea | 15 | 123 | 2 (10) | 12 |
| aphonia | 2 | 55 | 1 (5) | 4 |
Abbreviation: CI, confidence interval
Estimated average prevalence (95% confidence intervals) were computed by applying the inverse-logit transformation. Confidence intervals were calculated only for injuries reported by ≥3 studies. Raw data are available in Electronic Supplementary Material 4.
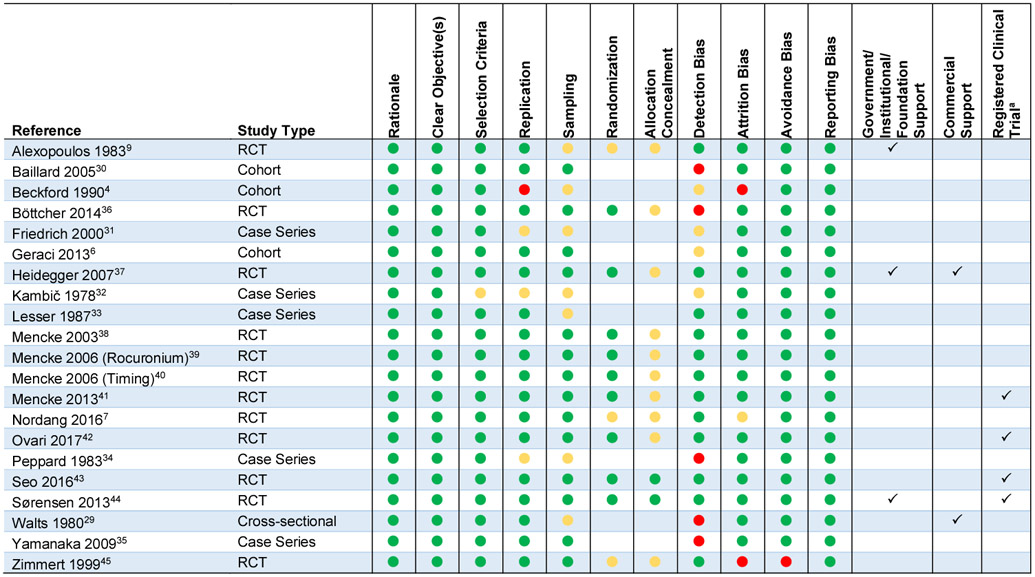
Methodological Quality/Risk of Bias
Methodological quality is summarized as risk of bias assessment (Table 4). Definitions for each of the assessment categories are provided in Supplemental Table 5. All studies provided adequate rationale and clear objectives. There were 2 (10%) studies, both RCTs, that presented with low risk of bias for all 9 of the RCT measures.43,44 An additional 7 (33%) studies had only 1 unknown risk of bias reported.6,37-42 Reporting bias was judged as low risk for all studies. There was 1 study that had a high risk for avoidance bias.45 There were several weaknesses. Perhaps the most concerning weakness was detection bias, with unknown risk of bias in 4 (19%) studies4,6,31,32 and high risk of bias in 5 studies.29,30,34-36 There was an unknown risk of sampling bias in 7 (33%) studies.4,9,29,31-34 Of the 12 RCTs, 3 (25%) had unknown risk of bias with randomization methods7,9,45 and 10 (83%) had unknown allocation concealment methods.7,9,36-42,45 Government/institution/foundation support was reported by 2 (10%) studies9,44 and commercial support was reported by 1 (5%) study.29 One (5%) study reported both institution and commercial support.37 The 2 (10%) studies reporting commercial support both received equipment to assist with obtaining outcomes29,37 and one that additionally received financial support for liability insurance.37
Table 4.
Risk of bias assessment.
 |
Key:  = low risk of bias;
= low risk of bias;  = unknown risk of bias;
= unknown risk of bias;  = high risk of bias.
= high risk of bias.
All registered trials were registered with ClinicalTrials.gov.
Abbreviation: RCT, randomized controlled trial
DISCUSSION
This systematic review focused on the prevalence of the types of laryngeal injury and their severity subsequent to endotracheal intubation during surgery. The 21 studies reporting on 6140 patients accepted for review demonstrated considerable heterogeneity of patient populations, study methods, and reported outcomes. The most remarkable finding was that although laryngeal injury and its symptoms are common consequences of intubation after surgery, an overwhelming majority of patients will emerge post-extubation from short-term (i.e., average of 2 hours) surgeries without laryngeal injury. Most patients who experience injury will be confined to self-limiting, soft tissue injuries (Grade I). Although more severe injuries (Grades II and III) are reportedly rare events, they should not be overlooked, either because of the functional consequences (i.e., dysphonia, dysphagia) or the potential for medical legal action.46
Several studies omitted reporting ETT size4,6,9,32,43,45 and nearly half did not report the ETT manufacturer.4,6,9,29-31,34,35,38,41 Seven (33%) studies4,9,29,32-34,45 were written before 2000 that, although not detailed, may have used different ETT materials or high pressure cuffs compared with other accepted studies, potentially affecting outcomes.47 These omissions limit this study’s ability to offer conclusions about the impact of ETT size on laryngeal injury and its severity. Until recently, there was virtually no link between ETT size and laryngeal injury. A study in the ICU literature suggests that a 7.0 ETT may be protective for laryngeal injury compared to ETT sizes 7.5 and 8.0.12 With 88% prevalence of no injury and all studies that reported size use ≥7.5 ETTs, clinicians may continue using larger ETT sizes. However, the 4-5% of surgeries resulting in moderate-to-severe laryngeal injuries as unintended consequences should give clinicians pause. Future studies should report ETT size, model, and manufacturer in their analyses, with the broader intentions of transparency in reporting and understanding the effects of these characteristics on laryngeal injury.
There do not appear to be guidelines for ETT size during surgery. Smaller size ETTs should be used for routine anesthesia,48 yet all reviewed studies used similar size ETTs to those in our previous systematic review of 9 ICU studies.11 Recently published guidelines for intubation during critical care explicitly state that a full discussion of ETT size is “beyond the remit of this guideline” (p. 337).49 With short durations and minimal expectation of intubation post-surgery, it follows that large ETTs are not necessary. The primary purpose of anesthesia delivery during surgery would suggest small ETTs are most appropriate. Moreover, the choice of smaller ETTs reduces concerns for its placement, especially in cases with difficult airways.48,49
Considering the frequency of Grade I injuries and voice dysfunction, it is tempting to think the two are associated; however, this is not an accurate conclusion. Our raw data suggest that voice dysfunction is independent of laryngeal impairment and dysphagia. Additionally, there is no apparent association between anatomical findings and subjective complaints of hoarseness36,42 or dysphagia.6,7 Updated guidelines for dysphonia after surgery state that new onset dysphonia after surgery “should have an expedited laryngeal evaluation according to the AAO-HNSF [American Academy of Otolaryngology-Head and Neck Surgery Foundation] guidelines, which recommend that this occur between 2 weeks and 2 months following the surgery” (S13).18 Two statements later, the guidelines read: “Early evaluation is also recommended for patients with dysphonia after extubation, regardless of duration of intubation, since they are at increased risk of having laryngeal injury, vocal fold paralysis, and aspiration. These patients are all more easily treated if identified early (S13).” Our data support early laryngeal assessment for interventions that are in patients’ best interests.
We found that 6/7 (86%) studies4,9,29,32,34,45 published before 2000 had multiple areas of unknown/high risk of bias, specifically insufficient information for study replication, sampling bias, and detection bias. Additionally, both RCTs during this period provided inadequate information for randomization and allocation concealment.9,45 After 2000, detection bias and allocation concealment for RCTs continue to be problematic; the remaining 7 parameters were virtually all low risk of bias. Contributors to reducing risk of bias and improved study quality around this time frame are the International Committee of Medical Journal Editors guidelines50,51 and the U.S. law52 for publications being followed by the National Institutes of Health.53 Future studies should consider these frequently updated guidelines and improvements in the clarity and transparency of research publications.
Limitations
We acknowledge several possible limitations. We limited our search to peer-reviewed publications with planned prospective data only. The gray literature that was excluded is characterized by conference abstracts unable to provide sufficient detail for review. Excluded studies, specifically retrospective studies, may have influenced estimates of prevalence. Even with these restrictions in the context of various methods across this relatively small number of accepted studies and the multiple focuses of the accepted studies, the subjects analyzed in this review were well-controlled a priori. We only permitted the analysis of control groups/standard of care groups, thus the strength of our findings for each injury grade is not likely to be substantially altered and largely agrees with the extant literature. Another potential limitation is that each of these studies were planned surgeries. Although we did not exclude studies based on duration of the surgery, we did not find surgeries that had longer durations while meeting other inclusion/exclusion criteria. These findings are not likely generalizable to longer duration surgeries. Despite these limitations, we believe this systematic review makes a unique contribution to the literature surrounding airway management of surgical patients by addressing post-extubation laryngeal injury, its prevalence and severity, and its clinical signs and symptoms, offering several areas for additional research and clinical action.
CONCLUSIONS
Short durations of intubation are associated with laryngeal injuries, but are generally mild. Moderate and severe injuries are rarer. Still, astute clinical observation will identify injuries leading to early treatment with the best potential outcomes. Best-practice guidelines for laryngeal assessment post-extubation from surgery are needed. Based on these data, a postoperative screening/assessment should occur for surgeries longer than 2 hours. Such an assessment will help facilitate the timely recognition and early interventions for serious laryngeal injury and its associated sequalae.
Supplementary Material
ACKNOWLEDGEMENTS
We offer sincere thanks to Lisa Aronson Friedman, Sc.M. and Elizabeth Colantuoni, Ph.D. for their statistical guidance and expertise in completing the meta-analysis. This research was supported by the National Institutes of Health/National Institute on Deafness and Other Communication Disorders (5K23DC013569, Brodsky) and National Institute of Nursing Research (5R01NR017433, Brodsky/Needham/Pandian).
FUNDING: This research was supported by the National Institutes of Health/National Institute on Deafness and Other Communication Disorders (5K23DC013569, PI: Brodsky) and National Institute of Nursing Research 5R01NR017433, Multiple PIs: Brodsky/Needham/Pandian)
GLOSSARY OF TERMS
- 95%CI
95% confidence interval
- AAO-HSNF
American Academy of Otolaryngology-Head and Neck Surgery Foundation
- CINAHL
Cumulative Index of Nursing and Allied Health Literature
- ETT
endotracheal tube
- ICU
intensive care unit
- LMA
laryngeal mask airway
- mm
millimeter(s)
- NR
not reported
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
randomized controlled trial
- RLN
recurrent laryngeal nerve
- SD
standard deviation
Footnotes
PRIOR PRESENTATION: American Thoracic Society (ATS) – May 21, 2017.
FINANCIAL RELATIONSHIPS:
- Royalties: MedBridge, Inc.
- Expert Testimony: Carroll, Kelly, Trotter & Franzen, PC
- Advisory Board, Olympus America Inc.
Erin Jedlanek, MS: None
- Grants
- City of Aberdeen and Harford County Drug Policy Office
- Johns Hopkins Hospital
- Johns Hopkins University
- NIH
- Sigma/American Nurses Credentialing Center
- University of Delaware
Brendan Blackford, MHS: None
Carrie Price, MLS: None.
Gai Cole, DrPH, MBA, MHA: None.
Pedro A. Mendez-Tellez, MD: None.
- Consultant, Ambu
- Expert Testimony:
- Jackson & Campbell, LLC
- Bailes, Craig, Yon & Sellards, PLLC
- Steptoe & Johnson, PLLC
- Grants: NIH/NIDCD, Triological Society, American College of Surgeons, NSF
Simon R. Best, MD: None.
Matthew J. Levy, DO, MSc: None.
REFERENCES
- 1.Rose J, Weiser TG, Hider P, Wilson L, Gruen RL, Bickler SW. Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health. 2015;3 Suppl 2:S13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weiser TG, Haynes AB, Molina G, et al. Size and distribution of the global volume of surgery in 2012. Bull World Health Organ. 2016;94(3):201–209f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Durbin CG Jr., Bell CT, Shilling AM. Elective intubation. Respir Care. 2014;59(6):825–846; discussion 847-829. [DOI] [PubMed] [Google Scholar]
- 4.Beckford NS, Mayo R, Wilkinson A 3rd, Tierney M. Effects of short-term endotracheal intubation on vocal function. Laryngoscope. 1990;100(4):331–336. [DOI] [PubMed] [Google Scholar]
- 5.Hamdan AL, Sibai A, Rameh C, Kanazeh G. Short-term effects of endotracheal intubation on voice. J Voice. 2007;21(6):762–768. [DOI] [PubMed] [Google Scholar]
- 6.Geraci G, Cupido F, Lo Nigro C, Sciuto A, Sciume C, Modica G. Postoperative laryngeal symptoms in a general surgery setting. Clinical study. Ann Ital Chir. 2013;84(4):377–383. [PubMed] [Google Scholar]
- 7.Nordang L, Lindholm CE, Larsson J, Linder A. Early laryngeal outcome of prolonged intubation using an anatomical tube: A double blind, randomised study. Eur Arch Otorhinolaryngol. 2016;273(3):703–708. [DOI] [PubMed] [Google Scholar]
- 8.Hamdan AL, Sabra O, Rameh C, El-Khatib M. Persistant dysphonia following endotracheal intubation. Middle East J Anaesthesiol. 2007;19(1):5–13. [PubMed] [Google Scholar]
- 9.Alexopoulos C, Lindholm CE. Airway complaints and laryngeal pathology after intubation with an anatomically shaped endotracheal tube. Acta Anaesthesiol Scand. 1983;27(4):339–344. [DOI] [PubMed] [Google Scholar]
- 10.Winslow CP, Winslow TJ, Wax MK. Dysphonia and dysphagia following the anterior approach to the cervical spine. Arch Otolaryngol Head Neck Surg. 2001;127(1):51–55. [DOI] [PubMed] [Google Scholar]
- 11.Brodsky MB, Levy MJ, Jedlanek E, et al. Laryngeal injury and upper airway symptoms after oral endotracheal intubation with mechanical ventilation during critical care: A systematic review. Crit Care Med. 2018;46(12):2010–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shinn JR, Kimura KS, Campbell BR, et al. Incidence and outcomes of acute laryngeal injury after prolonged mechanical ventilation. Crit Care Med. 2019;47(12):1699–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krisciunas GP, Langmore SE, Gomez-Taborda S, et al. The association between endotracheal tube size and aspiration (during flexible endoscopic evaluation of swallowing) in acute respiratory failure survivors. Crit Care Med. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benjamin B. Prolonged intubation injuries of the larynx: Endoscopic diagnosis, classification, and treatment. Ann Otol Rhinol Laryngol Suppl. 1993;160:1–15. [DOI] [PubMed] [Google Scholar]
- 15.Benjamin B, Holinger LD. Laryngeal complications of endotracheal intubation. Ann Oto Rhinol Laryn. 2008;117(9):2–20. [Google Scholar]
- 16.Sadoughi B, Fried MP, Sulica L, Blitzer A. Hoarseness evaluation: a transatlantic survey of laryngeal experts. Laryngoscope. 2014;124(1):221–226. [DOI] [PubMed] [Google Scholar]
- 17.Colice GL. Resolution of laryngeal injury following translaryngeal intubation. Am Rev Respir Dis. 1992;145(2 Pt 1):361–364. [DOI] [PubMed] [Google Scholar]
- 18.Stachler RJ, Francis DO, Schwartz SR, et al. Clinical practice guideline: Hoarseness (Dysphonia) (Update). Otolaryngol Head Neck Surg. 2018;158(1_suppl):S1–S42. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz SR, Cohen SM, Dailey SH, et al. Clinical practice guideline: Hoarseness (dysphonia). Otolaryngol Head Neck Surg. 2009;141(3 Suppl 2):S1–s31. [DOI] [PubMed] [Google Scholar]
- 20.Whited RE. A prospective study of laryngotracheal sequelae in long-term intubation. Laryngoscope. 1984;94(3):367–377. [DOI] [PubMed] [Google Scholar]
- 21.Wain JC. Postintubation tracheal stenosis. Chest Surg Clin N Am. 2003;13(2):231–246. [DOI] [PubMed] [Google Scholar]
- 22.Havas TE, Priestley J, Lowinger DS. A management strategy for vocal process granulomas. Laryngoscope. 1999;109(2 Pt 1):301–306. [DOI] [PubMed] [Google Scholar]
- 23.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions: Version 5.1.0 (updated March 2011). Cochrane Collaboration; 2011. [Google Scholar]
- 24.Higgins JPT, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. British Medical Journal. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lindholm C-E. Prolonged endotracheal intubation: A clinical investigation with special reference to its consequences for the larynx and trachea and to its place an alternative to intubation through a tracheostomy. Acta Anaesthesiol Scand. 1969;13(s33):1–80.5363891 [Google Scholar]
- 26.Eckerbom B, Lindholm CE, Alexopoulos C. Airway lesions caused by prolonged intubation with standard and with anatomically shaped tracheal tubes. A post-mortem study. Acta Anaesthesiol Scand. 1986;30(5):366–373. [DOI] [PubMed] [Google Scholar]
- 27.Thomas R, Kumar EV, Kameswaran M, et al. Post intubation laryngeal sequelae in an intensive care unit. J Laryngol Otol. 1995;109(4):313–316. [DOI] [PubMed] [Google Scholar]
- 28.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walts LF, Calcaterra T, Cohen A. Vocal cord function following short term endotracheal intubation. Clin Otolaryngol Allied Sci. 1980;5(2):103–105. [DOI] [PubMed] [Google Scholar]
- 30.Baillard C, Adnet F, Borron SW, et al. Tracheal intubation in routine practice with and without muscular relaxation: An observational study. Eur J Anaesthesiol. 2005;22(9):672–677. [DOI] [PubMed] [Google Scholar]
- 31.Friedrich T, Hansch U, Eichfeld U, Steinert M, Staemmler A, Schonfelder M. [Recurrent laryngeal nerve paralysis as intubation injury?]. Chirurg. 2000;71(5):539–544. [DOI] [PubMed] [Google Scholar]
- 32.Kambič V, Radšel Z. Intubation lesions of the larynx. Br J Anaesth. 1978;50(6):587–590. [DOI] [PubMed] [Google Scholar]
- 33.Lesser TH, Lesser PJ. Laryngeal trauma vs length of intubation. J Laryngol Otol. 1987;101(11):1165–1167. [DOI] [PubMed] [Google Scholar]
- 34.Peppard SB, Dickens JH. Laryngeal injury following short-term intubation. Ann Otol Rhinol Laryngol. 1983;92(4 Pt 1):327–330. [DOI] [PubMed] [Google Scholar]
- 35.Yamanaka H, Hayashi Y, Watanabe Y, Uematu H, Mashimo T. Prolonged hoarseness and arytenoid cartilage dislocation after tracheal intubation. Br J Anaesth. 2009;103(3):452–455. [DOI] [PubMed] [Google Scholar]
- 36.Böttcher A, Mencke T, Zitzmann A, et al. Laryngeal injuries following endotracheal intubation in ent surgery: Predictive value of anatomical scores. Eur Arch Otorhinolaryngol. 2014;271(2):345–352. [DOI] [PubMed] [Google Scholar]
- 37.Heidegger T, Starzyk L, Villiger CR, et al. Fiberoptic intubation and laryngeal morbidity: A randomized controlled trial. Anesthesiology. 2007;107(4):585–590. [DOI] [PubMed] [Google Scholar]
- 38.Mencke T, Echternach M, Kleinschmidt S, et al. Laryngeal morbidity and quality of tracheal intubation: A randomized controlled trial. Anesthesiology. 2003;98(5):1049–1056. [DOI] [PubMed] [Google Scholar]
- 39.Mencke T, Knoll H, Schreiber JU, et al. Rocuronium is not associated with more vocal cord injuries than succinylcholine after rapid-sequence induction: A randomized, prospective, controlled trial. Anesth Analg. 2006;102(3):943–949. [DOI] [PubMed] [Google Scholar]
- 40.Mencke T, Echternach M, Plinkert PK, et al. Does the timing of tracheal intubation based on neuromuscular monitoring decrease laryngeal injury? A randomized, prospective, controlled trial. Anesth Analg. 2006;102(1):306–312. [DOI] [PubMed] [Google Scholar]
- 41.Mencke T, Zitzmann A, Machmueller S, et al. Anesthesia with propofol versus sevoflurane: Does the longer neuromuscular block under sevoflurane anesthesia reduce laryngeal injuries? Anesthesiol Res Pract. 2013;2013:723168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ovari A, Bicker I, Machmueller S, et al. Sevoflurane at 1.0 MAC together with remifentanil and propofol produces clinically acceptable intubation conditions at the vocal cords: A prospective randomized study. J Int Med Res. 2017;45(3):1098–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Seo JH, Cho CW, Hong DM, Jeon Y, Bahk JH. The effects of thermal softening of double-lumen endobronchial tubes on postoperative sore throat, hoarseness and vocal cord injuries: A prospective double-blind randomized trial. Br J Anaesth. 2016;116(2):282–288. [DOI] [PubMed] [Google Scholar]
- 44.Sørensen MK, Rasmussen N, Kristensen MS, et al. Laryngeal morbidity after tracheal intubation: the Endoflex((R) tube compared to conventional endotracheal intubation with stylet. Acta Anaesthesiol Scand. 2013;57(6):737–744. [DOI] [PubMed] [Google Scholar]
- 45.Zimmert M, Zwirner P, Kruse E, Braun U. Effects on vocal function and incidence of laryngeal disorder when using a laryngeal mask airway in comparison with an endotracheal tube. Eur J Anaesthesiol. 1999;16(8):511–515. [DOI] [PubMed] [Google Scholar]
- 46.Domino KB, Posner KL, Caplan RA, Cheney FW. Airway injury during anesthesia: A closed claims analysis. Anesthesiology. 1999;91(6):1703–1711. [DOI] [PubMed] [Google Scholar]
- 47.Sultan P, Carvalho B, Rose BO, Cregg R. Endotracheal tube cuff pressure monitoring: A review of the evidence. J Perioper Pract. 2011;21(11):379–386. [DOI] [PubMed] [Google Scholar]
- 48.Farrow S, Farrow C, Soni N. Size matters: Choosing the right tracheal tube. Anaesthesia. 2012;67(8):815–819. [DOI] [PubMed] [Google Scholar]
- 49.Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120(2):323–352. [DOI] [PubMed] [Google Scholar]
- 50.Huth EJ, Case K. The URM: Twenty-five years old. Science Editor. 2004;27(1):17–21. [Google Scholar]
- 51.International Committee of Medical Journal Editors. Uniform requirements for manuscripts submitted to biomedical journals. N Engl J Med. 1997;336(4):309–315. [DOI] [PubMed] [Google Scholar]
- 52.Food and Drug Administration. Food and Drug Administraton Amendments Act of 2007. Pub. L. No. 110-85, 121 Stat. 823 (September. 27, 2007).
- 53.National Institutes of Health. Clinical trials registration in ClinicalTrials.gov (Public Law 110-85): Competing applications and non-competing progress reports (NOT-OD-08-023). Bethesda, MD: 2007. NOT-OD-08-023. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


