Abstract
Background:
Mothers of infants with congenital heart disease are at risk for depression.
Objectives:
This study explored the influence on maternal depressive symptoms of several known factors for mothers in the pediatric cardiac intensive care unit, including perceived stressors, attachment, and anxiety.
Methods:
This study was a secondary analysis of 30 mothers of infants awaiting cardiac surgery. Linear regressions were calculated to determine the relationships between perceived stressors, maternal attachment, anxiety, and maternal depressive symptoms.
Results:
Nearly half of mothers reported depressive symptoms above the measure cut-off score, indicating they were at risk for likely clinical depression. Subscales of perceived stress explained 61.7% of the variance in depressive symptoms (F = 11.815, p<0.0001) with parental role alteration subscale as the strongest predictor (standardized beta=0.694, p = 0.03).
Conclusions:
Findings underscore the importance of mental health screening and instituting nursing practices to enhance parental role for mothers of infants awaiting cardiac surgery.
Keywords: Intensive care unit, pediatric; Congenital heart defects, depression, cardiac surgery, preoperative period; Mother; Parent stress
Introduction
Infants born with critical congenital heart disease (CHD) require intensive care and subsequent cardiothoracic surgery in the neonatal period to survive. Consequently, these infants’ mothers experience extreme stress and are at elevated risk of adverse mental health symptoms, including depression.1–3 Depression, also referred to as clinical depression or major depressive disorder/episode, can range in severity based on the number of symptoms and has specific requirements for formal diagnosis based on DSM-V criteria.4 Even without a formal diagnosis, mothers can exhibit depressive symptoms prenatally at the time of fetal CHD diagnosis, with approximately one quarter to one half of mothers experiencing enough symptoms for likely clinical depression.5–7 Postnatally, 1 out of 5 mothers report depressive symptoms in the postoperative period and the transition home, a significantly higher proportion than mothers of infants with other diseases or mothers of healthy infants.7–12 Furthermore, depressive symptoms persist at 6, 18, and 36 months postpartum in mothers of infants with critical CHD, a trajectory significantly different from that of mothers of healthy controls.13
Maternal depressive symptoms during infancy can negatively impact the ability of mothers to form secure attachments.14,15 Maternal mental health and the maternal-infant bond are widely recognized to have a strong influence on the neurodevelopment of healthy children.16–25 There is a growing body of literature calling attention to the potential links between maternal mental health, impaired bonding, and poor neurodevelopmental outcomes in CHD.26–28 A myriad of factors have been found to be associated with neurodevelopmental abnormalities in CHD,29 including, but not limited to, genetic disorders, reduced cerebral perfusion, low birth weight, and longer hospital lengths of stay.30–33 Many of these factors are non-modifiable and together explain less than a third of the variance in poor neurodevelopmental outcomes.31–33 Evidence suggests that interventions targeting maternal stress and mental health can positively impact mental and behavioral development in children with CHD.34,35
Despite the demonstrated risk of depression in mothers of infants with CHD and the critical importance of maternal mental health in infant development, a gap in the literature exists describing early depressive symptoms in mothers during their infants’ critical care hospitalization prior to undergoing cardiac surgery. Few studies have explored predictors of depressive symptoms in mothers in the immediate postpartum period, including perceived stressors. No studies to date have examined early depressive symptoms in mothers of infants with CHD in the preoperative period in the pediatric cardiac intensive care unit (PCICU) or explored factors influencing depressive symptoms that could potentially influence the trajectories of these symptoms over time. Modifiable factors may exist that could be targeted for intervention in a way that mitigates the likelihood of increased depressive symptoms in mothers while their infants are hospitalized in the PCICU.
Lazarus and Folkman36 defined stress as an overarching term, encompassing a stressor that an individual perceives as stressful, which elicits a stress response. Building on this conceptualization of stress, as well as parent stress models posited by Miles and colleagues,37,38 the PCICU parental stress model was created to describe the unique experience for parents of infants with CHD.39,40 According to the PCICU parental stress model, specific stressors that mothers are exposed to in the PCICU can arise from the infant with CHD, the PCICU environment, and from factors arising from within mothers themselves.39,40 These factors combine to elicit both physical and psychological stress responses, which can include both anxiety and depressive symptoms. Factors in the infant category include infant appearance and behavior, severity of illness, and the timing of the infant’s diagnosis (pre- or postnatal) may all influence the perceived stress of mothers. Additionally, factors arising from the PCICU environment category include the sights and sounds of the PCICU, the lack of privacy, and large number of staff, which may be overwhelming and serve as an additional source of stress. Factors in the parent category include parental role alteration in the PCICU, which occurs when parents feel unable or do not know how to care for their hospitalized infant. Additional parent factors include sex/gender, age, race, ethnicity, and underlying tendencies towards anxiety (e.g. trait anxiety) may also influence their experience of stress in the PCICU.
Aims
The aim of this study was to explore depressive symptoms and factors influencing depressive symptoms in postpartum mothers of infants admitted to a PCICU within the first week of life prior to undergoing cardiac surgery. Variables were chosen based on the PCICU Parental Stress Model (Fig. 1). Specifically, the purpose of this study was:
To describe the magnitude of depressive symptoms and the rate of likely clinical depression in the PCICU.
To determine whether differences exist in reported depressive symptoms depending on infant and maternal characteristics.
To measure the perceived stressors for mothers whose infants are awaiting cardiac surgery in the PCICU.
To explore the relationships of maternal perceptions of stressors, trait anxiety, and perceived maternal-infant attachment on maternal depressive symptoms.
Fig. 1.
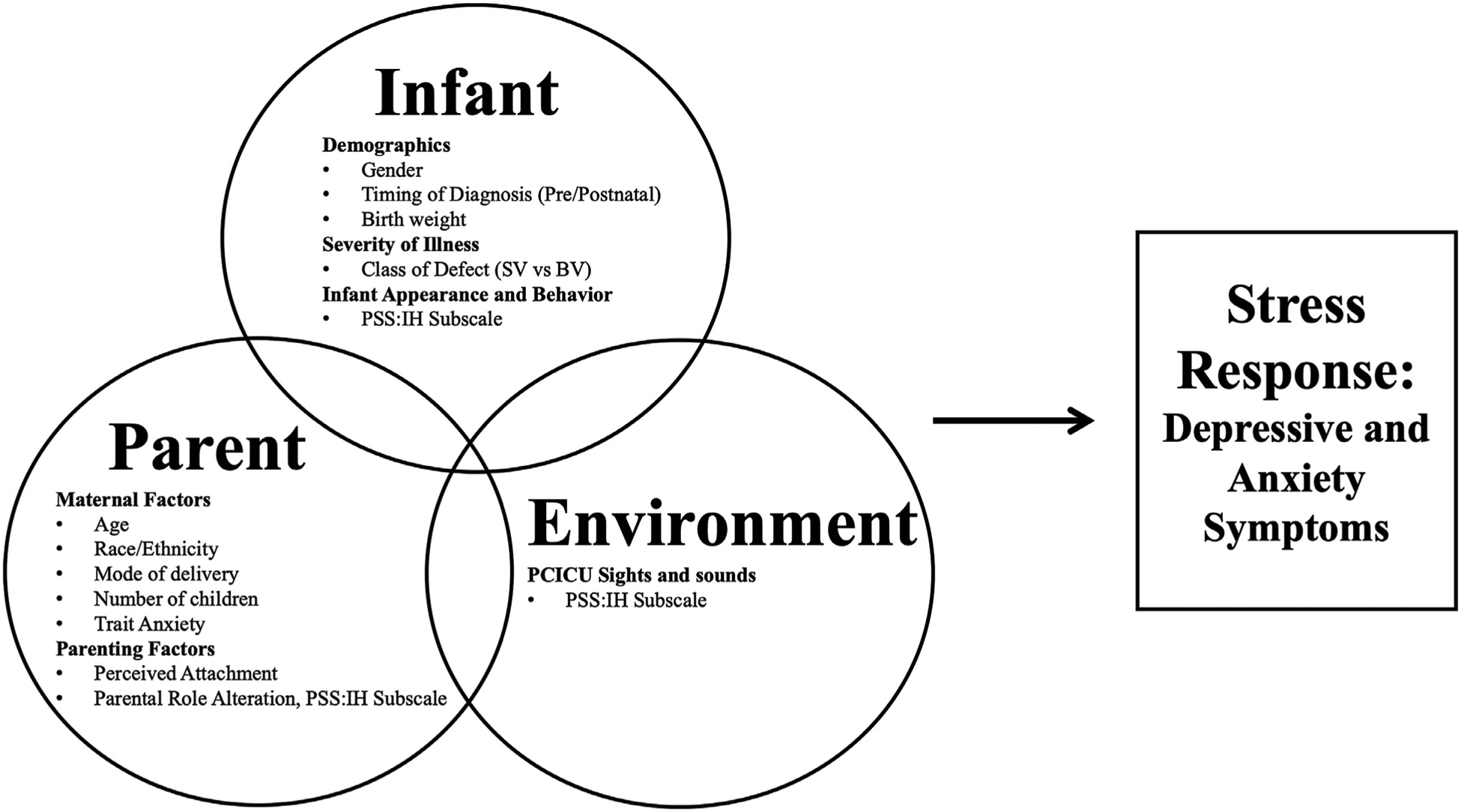
Secondary Analysis Variables Based on the PCICU Parental Stress Model.
Methods
This is a secondary analysis of a pilot study that enrolled 30 mothers of infants undergoing neonatal cardiac surgery and admitted after birth within the first week of life to a PCICU (citation in press, blinded for peer review). The study was conducted between January 2018 and January 2019 in a large free-standing children’s hospital in a metropolitan area in the northeastern United States. The original study tested a skin-to-skin care intervention in mother-infant dyads in the PCICU. All data for this secondary analysis were baseline data of mothers collected prior to any intervention. Mothers were approached for informed consent if their infants were full term at birth, greater than 2500 gs, not receiving end of life care, and admitted to the PCICU for neonatal cardiac surgery with no other genetic or congenital abnormalities. Mothers were at least 18 years of age and English-speaking. Baseline measures were obtained from mothers on perception of stress, perceived attachment, and symptoms of anxiety and depression. The investigation conforms with the principles outlined in the Declaration of Helsinki41 and received approval by the hospital’s institutional review board.
Variables and measures
The Center for Epidemiological Studies-Depression (CES-D)42 is a well-established instrument measuring depressive symptoms that also provides a cut-off for likely clinical depression versus not depressed. The instrument contains 20 items and asks subjects to rate on a 4-point Likert scale how often they have experienced symptoms associated with depression in the past week.42 Total scores are summed and have a possible range of 0 to 60, with scores greater than or equal to 16 indicating risk for likely clinical depression. The CES-D also has excellent validity and reliability and has been used across a range of populations.43,44
The Parental Stressor Scale: Infant Hospitalization (PSS:IH)45 is a 22-item instrument with established validity and reliability that measures maternal perception of stressors, including the infant’s appearance and behavior, the sights and sounds of the ICU environment, and parental role alteration. Subjects rated each experience on a 5-point Likert scale based on how stressful each experience was perceived from “not at all stressful” to “extremely stressful.” Mean scores could range from 1 to 5 with higher scores indicative of greater perceived stress. The PSS:IH has been successfully used to assess the perception of stressors in mothers of children with CHD.39,46
The State Trait Anxiety Inventory (STAI)47 is another well-established, valid, and reliable instrument that contains two 20-item subscales: State-Anxiety scale and Trait-Anxiety. The State-Anxiety subscale measures the magnitude of anxiety symptoms subjects feel at any current moment. The Trait-Anxiety subscale measures a subject’s tendency towards anxiety and has excellent test-retest reliability. Subjects rank each item on a four-point Likert scale from 1 (not at all) to 4 (very much so). The total scores of the State-Anxiety and Trait-Anxiety subscales are calculated by summing the items of each subscale separately. Scores can range from 20 to 80 with higher scores indicative of greater anxiety. For this study, and as posited by the PCICU Parental Stress Model, state-anxiety scores were used to measure the stress response of anxiety symptoms in mothers. trait-anxiety scores were used to measure a mother’s tendency towards anxiety, which may influence a mother’s stress response.
Mothers’ perceptions of attachment to their infants was measured by the Maternal Attachment Inventory (MAI). The MAI is a self-report instrument with 26-items that measures mothers’ feelings of attachment towards their infants and has been used in studies of mothers of infants with CHD.48–50 Mothers rate each item on a 4-point Likert scale. Scores are generated by summing item responses, with higher scores indicating greater feelings of maternal-infant attachment. The MAI has a total sum range of 26 to 104.
Analysis
Baseline demographic and clinical characteristics of mothers were summarized among the full sample. Frequencies of categorical measures were computed, as well as the means and standard deviations of continuous measures. For each demographic and clinical category, mean and standard deviation CES-D score were computed and t-tests were used to assess whether mean CES-D score was significantly correlated with each characteristic. Mean and standard deviation for PSS:IH survey items were presented as ordered by items’ mean value. Mothers’ mean state and trait anxiety measures were compared using a paired samples t-test. Bivariate associations were assessed between each predictor of interest and the continuous CES-D score outcome using spearman correlations. Predictors which exhibited a significant association with CES-D score at the alpha=0.05 level were included in a multiple linear regression model. To assess whether data satisfied assumptions of multiple linear regression, histograms and normality plots were produced and assessed, and Shapiro Wilk and kolmogorov smirnov tests were conducted. Variance inflation factors were computed and assessed to address model assumptions of collinearity. Adjusted analyses were performed to assess potential confounding regarding the relationships between each predictor of interest and the CES-D outcome. All data were analyzed using SPSS version 25 for Windows.
Results
Mean infant age at the time of this study was 2.87 days (SD=1.43). All infants were full-term with an average birth weight of 3323 gs (SD=604), and were admitted to a PCICU after birth for neonatal cardiac surgery. Diagnoses of single (47%) and two (53%) ventricle physiology were equally represented in the sample. Eighty percent (n = 24) were diagnosed with CHD prenatally. Detailed infant demographics were reported in the parent study (blinded citations).
Mothers were an average of 29.5 years old (SD=5.29). Half (50%) of mothers delivered via cesarean section (Table 1). The sample was relatively homogeneous with respect to race and ethnicity with a majority White (70%) and non-Hispanic (72%). Approximately three-quarters were married (77%) and just over half had obtained at least a college degree (53.3%). Mothers with only one child represented 40% of the sample, and 60% had more than one child.
Table 1.
Maternal demographics.
| Category | n | % | |
|---|---|---|---|
| Marital Status | Single | 7 | 23 |
| Married | 23 | 77 | |
| Race | Black or African American | 4 | 13 |
| White | 21 | 70 | |
| Asian | 1 | 3 | |
| Unknown/Other | 4 | 13 | |
| Ethnicity† | Hispanic or Latino | 8 | 27 |
| Not Hispanic or Latino | 21 | 72 | |
| Level of Education | Graduated from high school | 5 | 17 |
| Technical/Vocational School | 3 | 10 | |
| Partial college | 6 | 20 | |
| College graduate | 10 | 33 | |
| Master’s degree | 5 | 17 | |
| Doctoral degree | 1 | 3 | |
| Mode of Delivery | Vaginal | 15 | 50 |
| C-section | 15 | 50 |
Does not equal 100% due to missing data.
Aim 1
Mean scores on the CES-D were 15.70 (SD=8.53), with response scores ranging from 5 to 33. Forty-seven percent of mothers reported symptoms of depression that were at or above the cut off for likely clinical depression.
Aim 2
Depressive symptoms as measured by the CES-D were significantly higher among mothers identifying as White and/or non-Hispanic. Mothers of infants admitted with a postnatal diagnosis also reported significantly higher CES-D scores than mothers of infants who were prenatally diagnosed (Table 2). No association was found between depressive symptoms and other characteristics including mode of delivery, infant birth weight or gender, and class of defect (Tables 2 and 3).
Table 2.
Comparisons of maternal and infant factors with depressive symptoms.
| N (%) | CES-D Score M (SD) | p-value | ||
|---|---|---|---|---|
| Maternal Demographic Factors | ||||
| Race | White | 21 (70.0%) | 18.48 (8.39) | .001 |
| Non-White | 9 (30.0%) | 9.22 (4.55) | ||
| Ethnicity | Hispanic | 8 (26.7%) | 11.75 (5.37) | .048 |
| Non-Hispanic | 21 (70.0%) | 17.52 (9.14) | ||
| Mode of Delivery | Vaginal | 15 (50.0%) | 15.87 (7.87) | .917 |
| Cesarean Section | 15 (50.0%) | 15.53 (9.43) | ||
| Number of Children | 1 child | 12 (40.0%) | 19.33 (9.90) | .055 |
| >1 child | 18 (60.0%) | 13.28 (6.73) | ||
| Infant Demographics and Clinical Factors | ||||
| Gender | Male | 20 (66.7%) | 16.60 (8.49) | .433 |
| Female | 10 (33.3%) | 13.90 (8.77) | ||
| Class of Defect | Single Ventricle | 14 (46.7%) | 15.57 (8.06) | .940 |
| Two Ventricle | 16 (53.3%) | 15.81 (9.19) | ||
| Timing of Diagnosis | Prenatal | 24 (80.0%) | 12.92 (6.66) | <0.001 |
| Postnatal | 6 (20.0%) | 26.83 (5.71) | ||
Table 3.
Correlations of maternal and infant factors with depressive symptoms.
| Summary Statistics | CES-D Correlations | ||
|---|---|---|---|
| Mean ± SD | Spearman r | p-value | |
| Maternal Demographic and Mental Health Factors | |||
| Maternal Age | 29.50 ± 5.290 | −0.036 | .851 |
| State Anxiety | 49.90 ± 12.617 | .808 | <0.0001 |
| Trait Anxiety | 36.40 ± 8.779 | .187 | .323 |
| Maternal Attachment | 101.73 ± 2.288 | .153 | .419 |
| Infant Demographics | |||
| Infant birth weight | 3323.13 ± 604.088 | .093 | .623 |
Mothers’ mean state-anxiety was 49.40 (SD=12.62) and mean trait-anxiety score was 36.4 (SD=8.78). State anxiety scores were significantly higher than trait-anxiety scores (p<0.001). Maternal attachment as measured by the MAI revealed scores ranging from 97 to 104, the maximum possible score for the instrument, and averaged 101.73 (SD=2.288). While trait-anxiety and maternal attachment were not significantly associated with report of depressive symptoms, state-anxiety was significantly associated with CES-D scores (Table 3).
Aim 3
Total scores for the PSS:IH averaged 3.30 (SD=0.95). When comparing PSS:IH composites, mothers identified their infant’s appearance and behavior as the greatest source of stress (M = 3.71; SD=1.08), followed by parental role alteration (M = 3.29; SD=0.93), and the sights and sounds of the ICU (M = 2.50, SD=0.95). The top five mean-ranked PSS:IH items were (Table 4): “Seeing your child in pain”, “Seeing your baby have problems breathing”, “Not being able to protect your baby from pain and painful experiences,” “Not being able to comfort or help your baby,” and “Not being able to hold your baby.”
Table 4.
PSS:IH rank order descriptive statistics.
| Mean | Standard Deviation | |
|---|---|---|
| Seeing your child in pain | 4.08 | 1.152 |
| Seeing your baby have problems breathing | 4.04 | 1.107 |
| Not being able to protect your baby from pain and painful experiences | 4.00 | 1.145 |
| Not being able to comfort or help your baby | 4.00 | 1.134 |
| Not being able to hold your baby | 3.37 | 1.171 |
| When your child looks afraid, upset or cries a lot | 3.70 | 1.235 |
| Seeing your baby look sad | 3.62 | 1.329 |
| Not being able to regularly care for your baby | 3.57 | 1.194 |
| Being separated from your baby | 3.50 | 1.137 |
| Seeing your baby surrounded by machinery and having medical treatments | 3.47 | 1.279 |
| When your baby can’t respond to you | 3.42 | 1.465 |
| Seeing your baby with tubes or IV lines on him/her | 3.37 | 1.189 |
| Seeing a needle or tube put in your baby | 3.35 | 1.198 |
| The sudden sound of monitor alarms | 3.17 | 1.392 |
| Not having a chance to be alone with your baby | 3.17 | 1.147 |
| Not being able to share your baby with family and friends | 2.87 | 1.306 |
| The other sick children in the room | 2.79 | 1.473 |
| When other children in the hospital have a crisis | 2.63 | 1.334 |
| Monitors and equipment in the room | 2.57 | 1.104 |
| The large number of nurses, doctors, and other staff who work with your child | 2.00 | 1.069 |
| The needs of other parents in the hospital | 1.60 | .957 |
| The nurses and other staff seeming closer to the baby than you feel | 1.59 | .931 |
Aim 4
CES-D depression scores were significantly associated with measures of hospital related stress on the PSS:IH including: Parental Role Alteration (p<0.001, spearman r = 0.749), Infant Appearance and Behavior (p<0.001, spearman r = 0.722), and Sights and Sounds of the ICU (p<0.001, spearman r = 0.645), such that mothers who endorsed higher levels of stress on these composites also reported higher depressive scores.
In recognizing that our sample size does not provide us enough power to adjust for all predictors of interest and potential confounding factors in a single multivariable model, adjusted analyses were conducted separately for each predictor of interest. Race, ethnicity, and pre/postnatal diagnosis were identified as potential confounding factors, as they exhibited significant associations with mothers’ CES-D scores (Table 2). As trait-anxiety and maternal attachment were not significantly correlated with depressive symptom scores, only the PSS:IH subscales were included in the final multiple linear regression model to examine the relationship between hospital related parent stress and depression scores. Each predictor of interest (each PSS: IH subscale) remained a significant predictor of CES-D when adjusting for each variable identified to be a potential confounding factor. In the final model, the PSS:IH subscales explained 62% of the variance in maternal report of depressive symptoms as measured by the CES-D, while parental role alteration alone was a significant predictor (p<0.0001) (Table 5).
Table 5.
Predictors of maternal depressive symptoms.
| Unstandardized Coefficient | Standard Error | Effect Size (standardized Coefficient Beta | p-value | |
|---|---|---|---|---|
| Parental Role Alteration | 6.736 | 2.976 | .694 | .034 |
| Infant Appearance and Behavior | −0.022 | 2.671 | −0.003 | .994 |
| Sights and Sounds | 1.077 | 2.042 | .118 | .603 |
R Square = 0.617, F = 11.815, p<0.0001.
Discussion
The current study adds to a growing body of literature identifying high levels of stress, anxiety, and depressive symptoms in mothers of infants with CHD. To our knowledge, this is the first study to examine the relationship of stressors influencing depressive symptoms in mothers of infants with CHD admitted to the PCICU awaiting surgical intervention. Similar to what has been reported for participants in studies that measured maternal depression upon diagnosis of the infants’ CHD,6,7 close to a procedure,51 or during hospitalization,9 our sample of mothers reported high rates of likely clinical depression at almost 50 percent. Most importantly, the current study revealed that nearly two-thirds of the variance in depressive symptom scores was explained by perceived stress in the form of parental role alteration.
In previous research, parental role alteration has been described as a central experience of mothers of infants in the PCICU as well as the neonatal ICU.26,52–55 Parental role alteration has also been shown to predict State-Anxiety scores in mothers of infants in the PCICU after surgical intervention39 and has been associated with depressive symptoms in mothers of premature infants.56,57 These findings are critically important as current PCICU care practices can be targeted to promote the maternal role and reduce experiences of parental role alteration with the goal of reducing maternal anxiety and depressive symptoms. Parenting in the critical care environment is inherently stressful with restrictions on how and when mothers can touch, feed, care for, and comfort their infants. Pediatric cardiovascular nurses in the PCICU can reduce parental role alteration by facilitating partnership with mothers in both basic (e.g., skin-to-skin care, holding, feeding, diaper changes, bathing) and medical (e.g., oral care, obtaining vitals, facilitated tucking during stressful care) care. Nurses are uniquely positioned to champion family-centered developmental care practices that promote the parental role and can empower mothers to protect, comfort, and care for their infant in the PCICU.
While there have been very few interventional studies targeting mental health in mothers of infants with CHD,58 one study providing a phased, individualized intervention to parents of infants in the neonatal intensive care unit, including infants with CHD, was able to reduce symptoms of anxiety and depression in mothers at hospital discharge.59 Utilization of similar strategies in the PCICU, such as family-centered developmental care practices,28,60,61 that encourage mother-infant interaction and facilitate maternal partnership in care may reduce symptoms of depression and anxiety, facilitate the maternal-infant bond, and lessen the overall stress mothers report experiencing.
Consistent with previous research,62 depressive symptoms were correlated with current symptoms of anxiety (state-anxiety), but not with a mother’s tendency towards being anxious (trait-anxiety). Mothers in the current sample reported mean state-anxiety scores that fall in the 87th percentile of normative values for females of child bearing age.47 These findings suggest that any mother, regardless of baseline tendency towards anxiety, may be at risk for experiencing symptoms of anxiety during their infant’s admission. Additionally, mothers identified numerous stressors associated with their infant’s hospitalization on the PSS:IH with mean total scores indicating moderate levels of stress. As found in other samples of mothers of infants with CHD,39,46 Infant Appearance and Behavior was ranked as most stressful, followed by Parental Role Alteration, and the Sights and Sounds of the ICU. Rank order of PSS:IH items from most to least stressful was consistent with past research by Lisanti and colleagues39 in which the top stressors focused on infant pain and the inability of mothers to provide comfort or care for their infant. These findings provide additional support for the PCICU Parental Stress Model that identifies infant pain as a perceived stressor for mothers as well as the parental role alteration that arises when mothers are not able to help, comfort and hold their infant.
While child-specific factors such as disease severity have been associated with maternal depressive symptoms in older children with CHD,12,13,51,63 our findings are consistent with previous research that suggests severity of illness may be less meaningful when mothers’ infants are critically ill and awaiting open heart surgery.64,64 Our results also pointed to a significant difference in depressive symptoms based on race/ethnicity, such that mothers who identified as White and/or non-Hispanic reported significantly higher depression scores than did those who self-identified as a racial/ethnic minority. This is inconsistent with literature demonstrating racial/ethnic disparities in rates of perinatal depression regardless of fetal health status65,66 and may be a reflection of our relatively homogenous sample and the small sample size of mothers from minority groups. Additional research exploring how maternal, infant, and diagnosis-related factors influence maternal depressive symptoms is warranted.
Unlike other studies that have found prenatal diagnosis as a risk factor for depression9 or no difference based on timing of diagosis,10 we found that mothers of infants who received postnatal diagnoses of CHD reported significantly more depressive symptoms than mothers who received prenatal diagnoses. This may be due to timing of assessment (first week versus 2–4 weeks into hospital admission), but may also reflect the differing experiences of pre- and postnatally diagnosed mothers in our sample. Prenatally diagnosed mothers may also have had more time to prepare themselves and their families for their infant’s birth, both mentally and emotionally, but also logistically for the hospitalization. Prenatally diagnosed infants were delivered in our institution, which may contribute to less mother-infant separation in the first few days of life. They also receive comprehensive psychosocial services prenatally as a standard of care. These experiences may have influenced maternal depressive symptoms experienced in that group.
In terms of perceived maternal attachment, mothers in our sample reported attachment scores that were very similar to maternal attachment in mothers of healthy infants.48 We found no correlation between depressive scores and attachment in our sample of mothers. This is inconsistent with previous research showing that perceived maternal attachment can be negatively impacted by infant congenital anomaly and maternal depressive symptoms.48 More research is needed in this area to better understand the relationships of perceived attachment and depression.
Findings from this study highlight the need for universal parental mental health screening upon infant admission to the PCICU, as has been advocated by others.1–3,15 Psychosocial providers can focus on helping mothers navigate the stressors of the PCICU and adjust to their infant’s hospitalization by promoting effective coping skills and encouraging mothers to prioritize self-care as needed. These and other practice changes that enhance the parental role early and frequently throughout an infant’s hospitalization may be helpful in mitigating maternal symptoms of depression and anxiety.
As the present study is a secondary data analysis of a pilot study with small sample size, it must be recognized we were limited in our power to detect significant associations, as well as our ability to adjust for all potential confounding factors in a single multivariable analysis. Thus, we emphasize the need for these preliminary findings to be validated among a larger sample. Moderate effect sizes were found in the regression modeling, which will inform power analyses in future studies with greater sample sizes. The generalizability of this study is also limited by the lack of a comparison group. Additionally, this study focused solely on mothers of infants in the preoperative period. Literature surrounding stress and mental health of parents of infants with CHD show fathers have differing experiences.53,67 Future research exploring anxiety and depressive symptoms and perceived stress should include fathers and other caregivers.
Conclusions
This study adds to the current knowledge regarding the mental health mothers of infants with CHD in the immediate postpartum period. Mothers are at risk for increased depressive symptoms, which are influenced by their perceptions of altered parental role in the PCICU. Pediatric cardiovascular nurses can support these vulnerable mothers through targeted care practices that enhance parental role, screen to identify at-risk mothers, and promote coping and overall wellbeing.
Acknowledgments/Financial Support
Dr. Lisanti was funded by Association of PeriOperative Registered Nurses and Stryker through a grant from the American Nurses Foundation. Dr. Lisanti was also supported by NINR T32NR007100. The authors would like to thank Dr. Shira Birnbaum for her careful review and feedback on this manuscript.
Abbreviations:
- CES-D
Center for Epidemiological Studies-Depression
- CHD
Congenital Heart Disease
- ICU
Intensive Care Unit
- MAI
Maternal Attachment Inventory
- PCICU
Pediatric Cardiac Intensive Care Unit
- PSS:IH
Parental Stressor Scale: Infant Hospitalization
- STAI
State-Trait Anxiety Inventory
Footnotes
Declaration of Competing Interest
The authors have no conflicts of interest to disclose.
References
- 1.Woolf-King SE, Anger A, Arnold EA, Weiss SJ, Teitel D. Mental health among parents of children with critical congenital heart defects: a systematic review. J Am Heart Assoc. 2017;6:(2) e004862. 10.1161/JAHA.116.004862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kolaitis GA, Meentken MG, Utens E. Mental health problems in parents of children with congenital heart disease. Front Pediatr. 2017;5:102. 10.3389/fped.2017.00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jackson AC, Frydenberg E, Liang RP, Higgins RO, Murphy BM. Familial impact and coping with child heart disease: a systematic review. Pediatr Cardiol. 2015;36 (4):695–712. 10.1007/s00246-015-1121-9. [DOI] [PubMed] [Google Scholar]
- 4.Tolentino JC, Schmidt SL. DSM-5 criteria and depression severity: implications for clinical practice. Front Psychiatry. 2018;9:450. 10.3389/fpsyt.2018.00450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu M, Liang H, Feng J, Wang Z, Wang W, Zhou Y. Effectiveness of medical self-experience counseling in pregnant women after echocardiographic detection of a suspected fetal heart anomaly: a longitudinal study. J Obstet Gynaecol Res. 2016;42 (10):1236–1244. 10.1111/jog.13050. [DOI] [PubMed] [Google Scholar]
- 6.Rychik J, Donaghue DD, Levy S, et al. Maternal psychological stress after prenatal diagnosis of congenital heart disease. J Pediatr. 2013;162(2).. 302–307 e301; 10.1016/j.jpeds.2012.07.023. [DOI] [PubMed] [Google Scholar]
- 7.Hancock HS, Pituch K, Uzark K, et al. A randomised trial of early palliative care for maternal stress in infants prenatally diagnosed with single-ventricle heart disease. Cardiol Young. 2018;28(4):561–570. 10.1017/S1047951117002761. [DOI] [PubMed] [Google Scholar]
- 8.Re JM, Dean S, Mullaert J, Guedeney A, Menahem S. Maternal distress and infant social withdrawal (ADBB) following infant cardiac surgery for congenital heart disease. World J Pediatr Congenit Heart Surg. 2018;9(6):624–637. 10.1177/2150135118788788. [DOI] [PubMed] [Google Scholar]
- 9.Bevilacqua F, Palatta S, Mirante N, et al. Birth of a child with congenital heart disease: emotional reactions of mothers and fathers according to time of diagnosis. J Matern Fetal Neonatal Med. 2013;26(12):1249–1253. 10.3109/14767058.2013.776536. [DOI] [PubMed] [Google Scholar]
- 10.Hearps SJ, McCarthy MC, Muscara F, et al. Psychosocial risk in families of infants undergoing surgery for a serious congenital heart disease. Cardiol Young. 2014;24 (4):632–639. 10.1017/S1047951113000760. [DOI] [PubMed] [Google Scholar]
- 11.Lawoko S, Soares JJF. Distress and hopelessness among parents of children with congenital heart disease, parents of children with other diseases, and parents of healthy children. J Psychosom Res. 2002;52(4):193–208. 10.1016/s0022-3999(02)00301-x. [DOI] [PubMed] [Google Scholar]
- 12.Lawoko S, Soares JJ. Psychosocial morbidity among parents of children with congenital heart disease: a prospective longitudinal study. Heart Lung. 2006;35 (5):301–314. 10.1016/j.hrtlng.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Solberg O, Gronning Dale MT, Holmstrom H, Eskedal LT, Landolt MA, Vollrath ME. Trajectories of maternal mental health: a prospective study of mothers of infants with congenital heart defects from pregnancy to 36 months postpartum. J Pediatr Psychol. 2012;37(6):687–696. 10.1093/jpepsy/jss044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obeidat HM, Bond EA, Callister LC. The parental experience of having an infant in the newborn intensive care unit. J Perinat Educ. 2009;18(3):23–29. 10.1624/105812409X461199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jordan B, Franich-Ray C, Albert N, et al. Early mother-infant relationships after cardiac surgery in infancy. Arch Dis Child. 2014;99(7):641–645. 10.1136/archdischild-2012-303488. [DOI] [PubMed] [Google Scholar]
- 16.Park M, Brain U, Grunau RE, Diamond A, Oberlander TF. Maternal depression trajectories from pregnancy to 3 years postpartum are associated with children’s behavior and executive functions at 3 and 6 years. Arch Womens Ment Health. 2018;21(3):353–363. 10.1007/s00737-017-0803-0. [DOI] [PubMed] [Google Scholar]
- 17.Hayes LJ, Goodman SH, Carlson E. Maternal antenatal depression and infant disorganized attachment at 12 months. Attach Hum Dev. 2013;15(2):133–153. 10.1080/14616734.2013.743256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morgan JK, Ambrosia M, Forbes EE, et al. Maternal response to child affect: role of maternal depression and relationship quality. J Affect Disord. 2015;187:106–113. 10.1016/j.jad.2015.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1–27. 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- 20.Gerstein ED, Njoroge WFM, Paul RA, Smyser CD, Rogers CE. Maternal depression and stress in the neonatal intensive care unit: associations with mother-child interactions at age 5 years. J Am Acad Child Adolesc Psychiatry. 2019;58(3).. 350–358 e352; 10.1016/j.jaac.2018.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bowlby J Attachment: Attachment and Loss. 1. New York: Basic Books; 1969. [Google Scholar]
- 22.Schore AN. Attachment and the regulation of the right brain. Attach Hum Dev. 2000;2(1):23–47. 10.1080/146167300361309. [DOI] [PubMed] [Google Scholar]
- 23.Bergman NJ. Birth practices: maternal-neonate separation as a source of toxic stress. Birth Defects Res. 2019;111(15):1087–1109. 10.1002/bdr2.1530. [DOI] [PubMed] [Google Scholar]
- 24.Schore AN. Effects of a secure attachment relationship on right brain development, affect regulation, and infant mental health. Infant Ment Health J. 2001;22(1 2):7–66. . [DOI] [Google Scholar]
- 25.Schore JR, Schore AN. Modern attachment theory: the central role of affect regulation in development and treatment. Clin Soc Work J. 2007;36(1):9–20. 10.1007/s10615-007-0111-7. [DOI] [Google Scholar]
- 26.Lisanti AJ. Parental stress and resilience in CHD: a new frontier for health disparities research. Cardiol Young. 2018;28(9):1142–1150. 10.1017/S1047951118000963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ryan KR, Jones MB, Allen KY, et al. Neurodevelopmental outcomes among children with congenital heart disease: at-risk populations and modifiable risk factors. World J Pediatr Congenit Heart Surg. 2019;10(6):750–758. 10.1177/2150135119878702. [DOI] [PubMed] [Google Scholar]
- 28.Harrison TM. Improving neurodevelopment in infants with complex congenital heart disease. Birth Defects Res. 2019;111(15):1128–1140. 10.1002/bdr2.1517. [DOI] [PubMed] [Google Scholar]
- 29.Marino BS, Lipkin PH, Newburger JW, et al. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation. 2012;126(9):1143–1172. 10.1161/CIR.0b013e318265ee8a. [DOI] [PubMed] [Google Scholar]
- 30.Gaynor JW, Stopp C, Wypij D, et al. Neurodevelopmental outcomes after cardiac surgery in infancy. Pediatrics. 2015;135(5):816–825. 10.1542/peds.2014-3825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gaynor JW, Wernovsky G, Jarvik GP, et al. Patient characteristics are important determinants of neurodevelopmental outcome at one year of age after neonatal and infant cardiac surgery. J Thorac Cardiovasc Surg. 2007;133(5).. 1344–1353, 1353 e1341–1343; 10.1016/j.jtcvs.2006.10.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldberg CS, Lu M, Sleeper LA, et al. Factors associated with neurodevelopment for children with single ventricle lesions. J Pediatr. 2014;165(3).. 490–496 e498; 10.1016/j.jpeds.2014.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.International Cardiac Collaborative on Neurodevelopment I. Impact of operative and postoperative factors on neurodevelopmental outcomes after cardiac operations. Ann Thorac Surg. 2016;102(3):843–849. 10.1016/j.athoracsur.2016.05.081. [DOI] [PubMed] [Google Scholar]
- 34.McCusker CG, Doherty NN, Molloy B, et al. A controlled trial of early interventions to promote maternal adjustment and development in infants born with severe congenital heart disease. Child Care Health Dev. 2010;36(1):110–117. 10.1111/j.1365-2214.2009.01026.x. [DOI] [PubMed] [Google Scholar]
- 35.Chang LY, Chiu SN, Wang CC, Weng WC, Chang HY. Parenting stress mediates the association between cyanotic congenital heart disease and internalising problems in children and adolescents. Eur J Cardiovasc Nurs. 2020;19(4):301–309. 10.1177/1474515119881871. [DOI] [PubMed] [Google Scholar]
- 36.Lazarus RS, Folkman S. Stress, Appaisal and Coping. New York, NY: Springer; 1984. [Google Scholar]
- 37.Miles MS, Carter MC. Assessing parental stress in intensive care units. MCN. 1983;8:354–359. [DOI] [PubMed] [Google Scholar]
- 38.Miles MS, Holditch-Davis D. Parenting the prematurely born child: pathways of influence. [Review] [105 refs]. Semin Perinatol. 1997;21(3):254–266. [DOI] [PubMed] [Google Scholar]
- 39.Lisanti AJ, Allen LR, Kelly L, Medoff-Cooper B. Maternal stress and anxiety in the pediatric cardiac intensive care unit. Am J Crit Care. 2017;26(2):118–125. 10.4037/ajcc2017266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lisanti AJ, Golfenshtein N, Medoff-Cooper B. The pediatric cardiac intensive care unit parental stress model: refinement using directed content analysis. ANS Adv Nurs Sci. 2017;40(4):319–336. 10.1097/ANS.0000000000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rickham PP. Human experimentation. Code of ethics of the World Medical Association. Declaration of Helsinki. Br Med J. 1964;2(5402):177. 10.1136/bmj.2.5402.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Applied Psychological Measurements. 1977;1:385–401. [Google Scholar]
- 43.Howland LC, Pickler RH, McCain NL, Glaser D, Lewis M. Exploring biobehavioral outcomes in mothers of preterm infants. MCN Am J Matern Child Nurs. 2011;36 (2):91–97. 10.1097/NMC.0b013e318205587e. [DOI] [PubMed] [Google Scholar]
- 44.Canady RB, Stommel M, Holzman C. Measurement properties of the centers for epidemiological studies depression scale (CES-D) in a sample of African American and non-Hispanic White pregnant women. J Nurs Meas. 2009;17(2):91–104. 10.1891/1061-3749.17.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miles MS, Brunssen SH. Psychometric properties of the parental stressor scale: infant hospitalization. Adv Neonatal Care. 2003;3(4):189–196. 10.1016/s1536-0903(03)00138-3. [DOI] [PubMed] [Google Scholar]
- 46.Franck LS, McQuillan A, Wray J, Grocott MP, Goldman A. Parent stress levels during children’s hospital recovery after congenital heart surgery. Pediatr Cardiol. 2010;31(7):961–968. 10.1007/s00246-010-9726-5. [DOI] [PubMed] [Google Scholar]
- 47.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual For the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 48.Boztepe H, Ay A, Kerimoglu Yildiz G, Cinar S. Does the visibility of a congenital anomaly affect maternal-infant attachment levels. J Spec Pediatr Nurs. 2016;21 (4):200–211. 10.1111/jspn.12157. [DOI] [PubMed] [Google Scholar]
- 49.Muller ME. Prenatal and postnatal attachment: a modest correlation. J Obstet Gynecol Neonatal Nurs. 1996;25(2):161–166. 10.1111/j.1552-6909.1996.tb02420.x. [DOI] [PubMed] [Google Scholar]
- 50.Ylmaz HB, Kavlak O, Isler A, Liman T, Van Sell SL. A study of maternal attachment among mothers of infants with congenital anomalies in Turkey. Infants & Young Children. 2011;24(3):259–266. 10.1097/IYC.0b013e31821b465b. [DOI] [Google Scholar]
- 51.Uzger A, Baspinar O, Bulbul F, Yavuz S, Kilinc M. Evaluation of depression and anxiety in parents of children undergoing cardiac catheterization. Turk Kardiyol Dern Ars. 2015;43(6):536–541. 10.5543/tkda.2015.28928. [DOI] [PubMed] [Google Scholar]
- 52.Simeone S, Pucciarelli G, Perrone M, et al. Comparative analysis: implementation of a pre-operative educational intervention to decrease anxiety among parents of children with congenital heart disease. J Pediatr Nurs. 2017;35:144–148. 10.1016/j.pedn.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 53.Sood E, Karpyn A, Demianczyk AC, et al. Mothers and fathers experience stress of congenital heart disease differently: recommendations for pediatric critical care. Pediatr Crit Care Med. 2018;19(7):626–634. 10.1097/PCC.0000000000001528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alkozei A, McMahon E, Lahav A. Stress levels and depressive symptoms in NICU mothers in the early postpartum period. J Matern Fetal Neonatal Med. 2014;27 (17):1738–1743. 10.3109/14767058.2014.942626. [DOI] [PubMed] [Google Scholar]
- 55.Holditch-Davis D, White-Traut RC, Levy JA, O’Shea TM, Geraldo V, David RJ. Maternally administered interventions for preterm infants in the NICU: effects on maternal psychological distress and mother-infant relationship. Infant Behav Dev. 2014;37(4):695–710. 10.1016/j.infbeh.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Holditch-Davis D, Miles MS, Weaver MA, et al. Patterns of distress in African-American mothers of preterm infants. J Dev Behav Pediatr. 2009;30(3):193–205. 10.1097/DBP.0b013e3181a7ee53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Holditch-Davis D, Santos H, Levy J, et al. Patterns of psychological distress in mothers of preterm infants. Infant Behav Dev. 2015;41:154–163. 10.1016/j.infbeh.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kasparian NA, Kan JM, Sood E, Wray J, Pincus HA, Newburger JW. Mental health care for parents of babies with congenital heart disease during intensive care unit admission: systematic review and statement of best practice. Early Hum Dev. 2019;139: 104837. 10.1016/j.earlhumdev.2019.104837. [DOI] [PubMed] [Google Scholar]
- 59.Cano Gimenez E, Sanchez-Luna M. Providing parents with individualised support in a neonatal intensive care unit reduced stress, anxiety and depression. Acta Paediatr. 2015;104(7):e300–e305. 10.1111/apa.12984. [DOI] [PubMed] [Google Scholar]
- 60.Lisanti AJ, Vittner D, Medoff-Cooper B, Fogel J, Wernovsky G, Butler S. Individualized family-centered developmental care: an essential model to address the unique needs of infants with congenital heart disease. J Cardiovasc Nurs. 2019;34 (1):85–93. 10.1097/JCN.0000000000000546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Peterson JK, Evangelista LS. Developmentally supportive care in congenital heart disease: a concept analysis. J Pediatr Nurs. 2017;36:241–247. 10.1016/j.pedn.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tallon MM, Kendall GE, Snider PD. Development of a measure for maternal confidence in knowledge and understanding and examination of psychosocial influences at the time of a child’s heart surgery. J Spec Pediatr Nurs. 2015;20(1):36–48. 10.1111/jspn.12096. [DOI] [PubMed] [Google Scholar]
- 63.Wray J, Cassedy A, Ernst MM, Franklin RC, Brown K, Marino BS. Psychosocial functioning of parents of children with heart disease-describing the landscape. Eur J Pediatr. 2018;177(12):1811–1821. 10.1007/s00431-018-3250-7. [DOI] [PubMed] [Google Scholar]
- 64.Doherty N, McCusker CG, Molloy B, et al. Predictors of psychological functioning in mothers and fathers of infants born with severe congenital heart disease. J Reprod Infant Psychol. 2009;27(4):390–400. 10.1080/02646830903190920. [DOI] [Google Scholar]
- 65.Howell EA, Mora PA, Horowitz CR, Leventhal H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol. 2005;105(6):1442–1450. 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cole JC, Moldenhauer JS, Berger K, et al. Identifying expectant parents at risk for psychological distress in response to a confirmed fetal abnormality. Arch Womens Ment Health. 2016;19(3):443–453. 10.1007/s00737-015-0580-6. [DOI] [PubMed] [Google Scholar]
- 67.Hoffman MF, Karpyn A, Christofferson J, et al. Fathers of children with congenital heart disease: sources of stress and opportunities for intervention. Pediatr Crit Care Med. 2020. 10.1097/PCC.0000000000002388. [DOI] [PMC free article] [PubMed] [Google Scholar]


