Abstract
Growing evidence suggests that intimate partner violence (IPV) is a barrier to engagement in HIV care. Bidirectional IPV—being both a perpetrator and victim—may be the most common pattern of IPV, yet no research has examined its effect on engagement in care, which could identify couples in most need of interventions. Married couples (N = 211) with at least one partner on antiretroviral therapy were recruited from HIV clinic waiting rooms in Zomba, Malawi. Partners completed separate surveys on physical, sexual, and emotional IPV, medication adherence, and appointment attendance. We created categorical variables indicating no violence, perpetrator-only, victim-only, and bidirectional violence. Generalized estimating equation regression models tested for associations between IPV and engagement in care. The bidirectional pattern represented 25.4%, 35.5%, and 34.0% of all physical, sexual, and emotional IPV. Physical IPV victimization-only (adjusted odds ratio [AOR]: 0.28, 95% confidence interval [CI]: 0.08, 0.92) was associated with lower adherence, but the association was stronger for bidirectional physical IPV (AOR: 0.10, 95% CI: 0.02, 0.51). Bidirectional sexual IPV was also associated with lower adherence (AOR: 0.14, 95% CI: 0.02, 0.80). Bidirectional physical IPV (AOR: 4.04, 94% CI: 1.35, 12.14) and emotional IPV (AOR: 3.78, 95% CI: 1.78, 8.05) were associated with missing 1+ appointment. Interventions to address the health effects of bidirectional IPV, which may be greater than victim-only or perpetrator-only IPV, should intervene with both partners to break cycles of violence. Couple-based interventions may be a viable option by intervening on both partners’ trauma and aggression simultaneously.
Keywords: intimate partner violence, antiretroviral therapy, adherence, HIV/AIDS, sub-Saharan Africa
Introduction
Despite major gains in access to effective antiretroviral therapy (ART) in sub-Saharan Africa (SSA), only 63%–76% of people living with HIV are engaged in care and virally suppressed (McMahon et al., 2013). The evidence is mounting that victimization of intimate partner violence (IPV), defined as physical, sexual, or emotional abuse by a current or prior partner (Saltzman et al., 1999), is a key barrier to remaining engaged in care and virally suppressed (Hatcher et al., 2015; Leddy et al., 2019). In SSA, the prevalence of IPV is high with an estimated 36%–71% of women having experienced physical or sexual violence over their lifetimes (Garcia-Moreno et al., 2006). IPV is associated with poorer HIV clinical outcomes including detectable viral load, lower CD4 counts, treatment failure, and greater risk of mortality (Espino et al., 2015; Machtinger et al., 2012; Rose et al., 2010; Schafer et al., 2012; Siemieniuk et al., 2013; Trimble et al., 2013; Weber et al., 2012). Among U.S. women, lifetime exposure to violence or trauma (e.g., physical or sexual abuse) was associated with a decreased odds of using ART when medically indicated (Cohen et al., 2004) and maintaining adherence to ART (Mugavero et al., 2006). Moreover, a recent meta-analysis found that IPV victimization had a larger effect on adherence than factors such as stigma, financial constraints, and pill burden (Hatcher et al., 2015).
Despite growing attention to IPV as a barrier to HIV care (Hatcher et al., 2015; Leddy et al., 2019), this area of inquiry is still evolving in comparison to research linking IPV to HIV acquisition and sexual risk behaviors (Campbell et al., 2008; Gielen et al., 2007; Maman et al., 2000). We identified several gaps in knowledge that should be addressed in order to advance violence interventions among people living with HIV in SSA. First, IPV has primarily been examined as an issue affecting women’s health and engagement in HIV care (Anderson et al., 2018; Hampanda, 2016; Hatcher et al., 2015; Wilson et al., 2014). This is reasonable as women generally experience greater frequency and severity of IPV compared to men (Archer, 2000; Stets & Straus, 2017). Because of this focus on women, the majority of studies examine IPV at the individual level despite the fact that relationship violence is a dyadic event involving two partners—a victim, perpetrator, or both (i.e., bidirectional violence). A couple-based approach to studying IPV would help to avoid pseudo-unilaterality, a bias that results from studying one side of a two-way interaction (Lewis et al., 2006). Further, by examining the prevalence and impact of IPV on men and women within the dyad, researchers can gain a more holistic view of IPV and how to effectively intervene with partners (Bates, 2016).
Second, little research has examined female perpetration of IPV, men’s experiences of being victims, bidirectional violence (i.e., experiencing both IPV victimization and perpetration in the same relationship) and how these events impact health behaviors related to HIV. Although motivations for IPV perpetration differ by gender, evidence from settings outside of SSA suggest that women are equally likely to be perpetrators of IPV (Anderson, 2002; Stets & Straus, 2017; Straus, 2008, 2010). An analysis of a nationally representative sample of couples in the U.S. found that among IPV victims, over half had also perpetrated IPV (Anderson, 2002). Langhinrichsen-Rohling (2010) defined three types of bidirectional violence in couples: violence motivated by control and coercion with both partners displaying these behaviors; violence because of issues regulating emotions and controlling their behavior, a function of the level of interdependence between partners; and, a less severe form of violence restricted to partners with little evidence of psychopathology (i.e., “retaliator violence”). Additionally, a review of 200 studies with couples in the U.S. found that bidirectional violence was the most common type of IPV reported (Stets & Straus, 2017; Straus, 2010), a finding that held in another review conducted across 32 nations (Straus, 2008). Although research in SSA is limited, one study in South Africa found similar rates of IPV victimization among men and women (21% vs. 29%) (Gass et al., 2011).
More attention is needed to investigate the intersection of IPV victimization and perpetration in SSA and the cumulative effects of violence on health throughout the life course. Abuse as a child predicts violence perpetration against intimate partners and children later in life, and prior victimization of IPV predicts future perpetration and victimization of IPV (Manchikanti Gómez, 2011; Milaniak & Widom, 2015; Stith et al., 2000). Based on a life course model, women and men who were prior victims of violence could perpetrate violence or become re-victimized in future relationships (Logan-Greene et al., 2015). However, no research has examined these dyadic patterns of IPV in SSA and its potential impact on engagement in HIV care.
This is important to investigate given that over 50% of all people living with HIV globally reside in SSA (UNAIDS, 2018), many of whom are now accessing treatment (Joint United Nations Programme on HIV/AIDS, 2017). Yet to date, the literature has overwhelmingly focused on IPV and engagement in care in settings such as the US (Hatcher et al., 2015). It is critical to understand patterns of IPV victimization and perpetration in African couples living with HIV to identify the most effective ways to intervene (e.g., couples, women) and with whom (e.g., perpetrators, victims, or both). To move towards this goal, we conducted a cross-sectional study with heterosexual couples with at least one partner on ART to test for associations between IPV and engagement in HIV care and treatment. Our first objective is to describe patterns of IPV among couples living with HIV and explore gender differences. Our second objective is to examine the associations between victim-only, perpetrator-only, and bidirectional IPV across three IPV domains (physical, sexual, and emotional) and engagement in HIV care outcomes.
Methods
Study Context
This study takes place in the Zomba district of Southern Malawi, which has an HIV prevalence of around 15% (MDHS, 2016). IPV is pervasive in Malawi. A demographic report featuring a nationally representative sample showed that 25% of women had experienced sexual violence. In the same report, 28% of women had experienced physical violence (National Statistical Office & ICF Macro, 2011). Trends indicate that rates of sexual and physical IPV increase with age (up until 30 years), decrease with education, and are higher within marriage and in rural areas (National Statistical Office & ICF Macro, 2011). Prior research with younger couples in a different region of southern Malawi found that 17% of participants reported sexual violence in the form of sexual coercion and 4% of participants reported being physically abused by their partners (Conroy, 2014b).
A number of social and behavioral conditions shape the context of violence and HIV treatment in Malawi and across SSA. Alcohol use is an important trigger of IPV which in turn, is one of the strongest predictors of adherence to HIV treatment (Hatcher et al., 2015; Koenig et al., 2003; Zablotska et al., 2009). Gender-based power imbalances are one of the most compelling explanations for IPV among women (Blanc, 2001), which are linked to IPV through masculinity, male dominance, and control over women (Choi & Ting, 2008; Jewkes, 2002; Morrell et al., 2013). In Malawi and South Africa, women in relationships with high levels of male control or dominance were more likely to report recent or previous IPV (Conroy, 2014a; Dunkle et al., 2004). Poor economic conditions may also contribute to the experience of IPV through the pathway of masculinity. For example, men in poverty who are unable to live up to traditional gender norms related to the provider role may use violence to express their manhood and male identity (Jewkes, 2002). Other studies in Malawi with couples have described IPV as a part of a complicated web of extramarital relationships, poverty, and food insecurity (Conroy et al., 2018).
Malawi has a well-established ART program with over 780,000 individuals on active treatment (Ministry of Health Malawi, 2018). Since the start of universal test-and-treat in 2016, almost 90% of PLWH have started ART (UNAIDS, 2017). HIV care and treatment is offered free of charge. However, with regards to violence, there are few social and health services for people living with HIV who experience violence with options limited to victim support units at police stations, rape services at large hospitals, and limited legal support for divorcing a violent spouse (unpublished fieldwork data).
Study Procedures
The data come from Umodzi M’Banja (“UMB”; Unity in the Family), which is a dyadic investigation of HIV-positive individuals on ART and their primary partners in Zomba, Malawi (Conroy et al., 2018, 2019). From August to November of 2017, we conducted a cross-sectional survey with 211 couples (422 individuals). Couples were eligible to participate if they were (a) in a non-polygamous union for at least six months; (b) age 18 or older; and (c) had at least one partner (the “index partner”) on ART for at least 2 months who had disclosed their HIV status to the primary partner. Disclosure was required so we could assess social support practices from both partners’ viewpoints. Polygamous couples, comprising around 7% in this region (MDHS, 2016), were excluded for feasibility of recruitment and analysis.
Participants were recruited at two high-volume HIV clinics in the Zomba district: an urban clinic at a large district and regional referral hospital, and a private clinic at a rural community hospital. Research staff announced the study during daily health talks in the waiting rooms and interested patients could approach the staff for more information. If the index patient was eligible, they gave an information card to their primary partner who could contact study staff. Partner eligibility was assessed over the phone and then confirmed in-person at the couples’ interview appointment. Research assistants, matched by gender to the participants, administered the surveys on tablet devices using Survey CTO, a secure, web-based data collection platform (Dobility, Inc., https://www.surveycto.com). Partners were interviewed separately, but simultaneously, in private areas of the HIV clinics, and were asked the same questions on IPV and engagement in care.
Partners were consented separately in private locations of the HIV clinics and were each provided a small incentive (around $2 USD) for their time. Interviewers were trained to assess and respond to couple conflict/violence or coercion, and on how to facilitate referrals for domestic violence assistance. The study was approved by the National Health Science Research Committee in Malawi and the Committee on Human Research at the University of California San Francisco.
Measures
Physical violence.
For victimization, we asked six questions about past 12-month physical violence from the WHO domestic violence module (Garcia-Moreno et al., 2006) (e.g., “Has your husband/wife pushed you, shaken you, or thrown something at you?”). Response options were never (coded as 1), sometimes (coded as 2), and frequently (coded as 3). Respondents who answered “sometimes” or “frequently” to any of the six questions were considered to have experienced victimization. Following each victimization question, we asked the same six questions with regards to perpetration (e.g., “Have you ever done this to your partner?”; responses: never, sometimes, frequently). Respondents who answered “sometimes” or “frequently” to any of the six questions were considered to have engaged in perpetration. Using the victimization and perpetration variables, we created a four-level categorical variable to capture bidirectional physical IPV (0 = no victimization or perpetration; 1 = only victimization; 2 = only perpetration; 3 = bidirectional [both victimization and perpetration]).
Sexual violence.
For victimization, we asked three questions on past 12-month sexual violence from the WHO domestic violence module (e.g., “Has your husband/wife physically forced you to have sexual intercourse when you did not want to?”). Response options were never (coded as 1), sometimes (coded as 2), and frequently (coded as 3). Respondents who answered “sometimes” or “frequently” to any of the six questions were considered to have experienced victimization. Following each victimization question, we asked the same six questions with regards to perpetration (e.g., “Have you ever done this to your partner”?). Respondents who answered “sometimes” or “frequently” to any of the six questions were considered to have engaged in perpetration. Using the victimization and perpetration variables, we created a four-level categorical variable to capture bidirectional sexual IPV.
Emotional violence.
For victimization, we asked four questions on past 12-month emotional violence from the WHO domestic violence module (e.g., “Did your husband/wife ever insult you or make you feel bad about yourself?”). Response options were never (coded as 1), sometimes (coded as 2), and frequently (coded as 3). Respondents who answered “sometimes” or “frequently” to any of the four questions were considered to have experienced victimization. Following each victimization question, we asked the same four questions with regards to perpetration (e.g., “Have you ever done this to your partner”?). Respondents who answered “sometimes” or “frequently” to any of the six questions were considered to have engaged in perpetration. Using the victimization and perpetration variables, we created a three-level categorical variable to capture bidirectional emotional IPV. We only used three categories because of small cell sizes, which is justified by other studies finding that the effect of victimization or perpetration only on health outcomes were similar (Ulloa & Hammett, 2016).
Self-reported adherence to ART.
To account for low education levels, we used an innovative “bean method” based off the 30-day Visual Analog Scale. The interviewer gave the respondent two bowls, one with beans and one empty, and stated, “I am going to give you a bowl of beans. Pretend that these are the ARVs you take each month. If you take ARVs once per day, there are 30 beans for the month. If you take ARVs twice per day, there are 60 beans. Please select the number of beans corresponding to the ARVs you did not take in the last month and put them in the second bowl.” A binary variable was created based on treatment regimen (once or twice per day) and number of beans placed in the empty bowl. We considered taking 90% or more of pills to be adherent (90% or higher vs. less than 90% adherence), which is a validated cutoff used in other studies in SSA (Thirumurthy et al., 2012).
Missed clinic appointments.
We asked respondents if they ever missed an appointment with their HIV care provider in the past 6 months and if yes, how many times. We created a binary variable if respondents had missed one or more appointments.
Covariates.
Based on the previous literature, multivariable models controlled for gender, couple HIV status (concordant or discordant), age, education, household wealth score, number of shared children, relationship length, treatment regimen complexity (once vs. twice per day), length of time on ART, and recruitment site (urban vs. rural) (Filmer & Pritchett, 2001; Johnson et al., 2012). To control for any self-reporting bias in the IPV reporting, we also controlled for discrepancies between partners for each of type of IPV (0 = both partners agree on victimization/perpetration; 1 = disagree that wife was victim/perpetrator; 2 = disagree that husband was victim/perpetrator).
Data Analysis
One-way frequency tables and measures of central tendency were generated to characterize the sample. For the binary outcomes of engagement in care, we used generalized estimating equations clustering on the couple identifier with the robust standard error option, a binary distribution, and a logit link function to yield odds ratios. We fit separate multivariable models, controlling for the covariates above, for each type of IPV (physical, sexual, and emotional) in order to isolate the role of different types of violence on engagement in care, which will be useful information for future intervention in this population. Missing data were negligible (<2%). Of the 211 couples (422 individuals) enrolled, 341 individuals were on ART and were therefore included in the regression analysis (Table 2).
Table 2.
Unadjusted and Adjusted Odds Ratios from Generalized Estimating Equations (GEE) Models on IPV and Engagement in HIV Care and Treatment.
| Self-reported 90%−100% ART Adherence | Missed 1+ Clinic Appointment | |||
|---|---|---|---|---|
| IPV Variables | Unadjusted Odds Ratios (95% CI) | Adjusted Odds Ratios (95% CI) | Unadjusted Odds Ratios (95% CI) | Adjusted Odds Ratios (95% CI) |
| Physical IPV | ||||
| No violence | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Victim only | 0.41 (0.10, 1.68) | 0.28 (0.08, 0.92)* | 0.97 (0.47, 2.00) | 1.17 (0.46, 2.99) |
| Perpetrator only | 0.40 (0.07, 2.06) | 0.28 (0.07, 1.08) | 0.87 (0.34, 2.25) | 1.03 (0.35, 3.06) |
| Bidirectional | 0.17(0.04, 0.71)* | 0.10 (0.02, 0.51)** | 2.49 (0.97, 6.39) | 4.04 (1.35, 12.14)* |
| Sexual IPV | ||||
| No violence | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Victim only | 0.91 (0.18,4.52) | 0.58 (0.08, 4.06) | 1.26 (0.66, 2.40) | 1.09 (0.51,2.33) |
| Perpetrator only | 0.79 (0.09, 6.98) | 0.53 (0.05, 5.40) | 0.33 (0.07, 1.40) | 0.28 (0.06, 1.42) |
| Bidirectional | 0.28 (0.08, 0.90)* | 0.14 (0.02, 0.80)* | 2.26 (1.19, 4.31)* | 1.86 (0.90, 3.87) |
| Emotional IPV | ||||
| No violence | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Victim or perpetrator | 2.03 (0.43, 9.65) | 1.62 (0.19,13.64) | 1.42 (0.78, 2.64) | 1.75 (0.82, 3.77) |
| Bidirectional | 0.60 (0.16, 2.32) | 0.90 (0.10, 8.20) | 3.12 (1.64, 5.95)** | 3.78 (1.78, 8.05)** |
| N (couples) | 211 | 210 | 210 | 210 |
| N (persons on ART) | 339 | 333 | 341 | 341 |
Note.
p < .05.
p < .01.
Adjusted models controlled for gender, couple HIV status, discrepancies between partners in violence reporting, age, education level, relationship duration, household wealth, duration of time on ART, treatment regimen complexity, and recruitment site. GEE models assumed an exchangeable correlation structure.
Results
Sample Characteristics
Of the 211 couples (422 individuals), the mean age was 40.5 and the majority (80.8%) had a primary school education or less. All couples were in married or cohabitating unions for an average of 12.5 years. Approximately two-thirds of couples were sero-concordant positive (one-third were sero-discordant). Of participants who were HIV-positive (N = 352), 95.6% reported 90%–100% ART adherence in the past 30 days and 23.6% reported missing at least one HIV clinic appointment in the past six months (Table 1).
Table 1.
Sample Characteristics of Couples in the Umodzi M’Banja Study in Malawi (211 Couples; 422 Individuals).
| Variable | Total Sample %, Mean (SD) | Men %, Mean (SD) | Women %, Mean (SD) | p value for gender differences |
|---|---|---|---|---|
| Individual characteristics | ||||
| Age (years) | 40.5 (10.2) | 43.5 (10.6) | 37.4 (8.8) | <0.001 |
| Education level | ||||
| Primary school or less | 80.8 | 73.5 | 88.2 | |
| Secondary school | 18.7 | 25.6 | 11.8 | |
| Tertiary school or higher | 0.5 | 1.0 | 0.0 | <0.001 |
| Household wealth index (range: 0–8) | 2.8 (1.6) | 3.0 (1.6) | 2.7 (1.6) | 0.04 |
| Religion | ||||
| Muslim | 10.2 | 10.0 | 10.4 | |
| Christian | 89.8 | 90.0 | 89.6 | 0.87 |
| Living with HIV | 83.4 | 81.0 | 85.8 | 0.29 |
| Currently on ART | 82.5 | 79.6 | 85.3 | 0.12 |
| Length of time on ART (years) | 4.8 (3.1) | 4.6 (3.1) | 5.1 (3.1) | 0.05 |
| Relationship characteristics | ||||
| Relationship duration (years) | 12.5 (9.0) | 12.9 (9.2) | 12.1 (8.8) | 0.83 |
| Number of dependent children (range: 0–11) | 3.3 (1.8) | 3.5 (1.9) | 3.2 (1.7) | 0.91 |
| Sero-concordant positive | 66.8 | -- | -- |
Patterns of IPV Victimization and Perpetration in Couples
Using the constructed variables for mutual IPV (victim-only, perpetrator-only, bidirectional, and no violence patterns), we found that 27.0%, 35.3%, and 35.5% of participants reported any physical, sexual, and emotional IPV, respectively. Of this subset, the victim-only pattern was most common, followed by the bidirectional pattern. This held for all three types of IPV. The bidirectional pattern represented 25.4%, 35.5%, and 34.0% of all physical, sexual, and emotional IPV, respectively. For the full sample, we also found significant gender differences in bidirectional physical, sexual, and emotional IPV (all p < .001; see Figure 1). As shown in Figure 1, women were more likely to report being a victim-only than men across all three forms of IPV; whereas men were more likely to report being a perpetrator-only across all three forms of IPV. For physical and emotional IPV, women reported more bidirectional violence than men (9.5% vs. 4.3% and 16.6% vs. 7.6%, respectively). For sexual IPV, men and women reported similar levels of bidirectional violence (12.8% vs. 12.3%).
Figure 1.
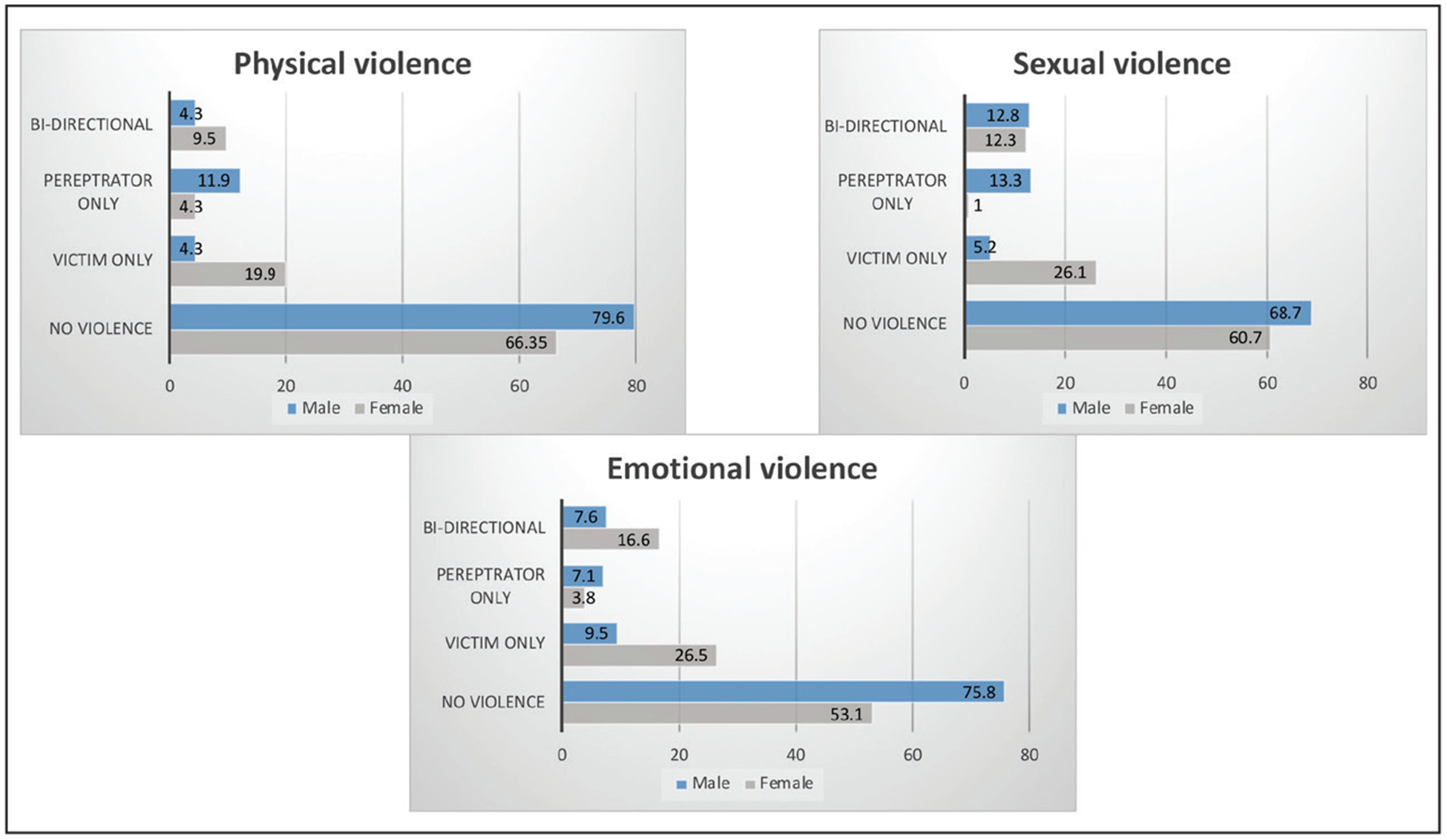
Gender differences in reported violence (%) among couples in Malawi.
When examining discrepancies between partners in the reporting of IPV, we found that 60.2% of couples agreed on physical IPV victimization and perpetration in their relationship and 39.8% were discrepant. Of the discrepancies, 27.0% disagreed whether the wife was the victim or perpetrator (e.g., the wife said she perpetrated IPV when the husband said she did not) and 12.8% disagreed whether the husband was the victim or perpetrator (e.g., the husband said he perpetrated IPV when the wife said he did not). Discrepancies between partners were higher for sexual and emotional IPV (47.4% and 49.8%, respectively).
Is IPV Victimization and Perpetration Associated with Adherence to ART?
In the adjusted models for physical IPV (Table 2), individuals who only reported physical IPV victimization had a reduced odds of ART adherence, compared to those who reported no physical IPV (adjusted odds ratio [aOR]: 0.28, 95% confidence interval [CI]: 0.08, 0.92). Individuals who reported bidirectional physical IPV also had a reduced odds of ART adherence, compared to those who reported no physical IPV (aOR: 0.10, 95% CI: 0.02, 0.51). In the adjusted models for sexual IPV, individuals who reported bidirectional sexual IPV had a reduced odds of ART adherence, compared to those who reported no sexual IPV (aOR: 0.14, 95% CI: 0.02, 0.80). Perpetration of physical or sexual IPV was not significantly associated with ART adherence. In the adjusted models for emotional IPV, being a victim or a perpetrator was also not associated with ART adherence, neither was bidirectional violence.
Is IPV Victimization and Perpetration Associated with Missed Clinic Appointments?
After adjusting for covariates, individuals reporting bidirectional physical IPV had an increased odds of missing at least one clinic appointment, compared to those reporting no physical IPV (aOR: 4.04, 94% CI: 1.35, 12.14). Additionally, individuals reporting bidirectional emotional IPV were more likely to report missing at least one clinic appointment compared to those reporting no emotional IPV (aOR: 3.78, 95% CI: 1.78, 8.05). In the adjusted models for sexual IPV, being a victim or a perpetrator was not associated with missed clinic appointments, neither was bidirectional violence.
Discussion
Our findings contribute new information regarding the overlooked importance of bidirectional IPV as a factor shaping engagement in HIV care and treatment. Being a victim of physical IPV—without being a perpetrator— was associated with lower adherence to ART. However, this association was greater in magnitude for bidirectional violence—that is, being both a victim and perpetrator of physical IPV had a greater effect on adherence than being a victim or perpetrator-only. Additionally, bidirectional sexual IPV was associated with lower adherence to ART. Interestingly, these findings did not hold for emotional IPV. In terms of appointment attendance, bidirectional sexual and emotional IPV, but not bidirectional physical IPV, were significantly associated with missed HIV clinic appointments. Together, these findings are consistent with other studies in the U.S. showing a stronger role of bidirectional versus unidirectional IPV and health outcomes including depression, drug use, and suicidality (Graham et al., 2012; Temple et al., 2005; Ulloa & Hammett, 2016). However, it appears that the importance of bidirectional violence for engagement in care and treatment may depend on the type of IPV experienced.
In contrast to literature from non-African settings suggesting that bidirectional violence is the most common pattern of IPV (almost 50%) (Anderson, 2002; Straus, 2008), we found slightly lower bidirectional IPV (less than 35%). Nevertheless, these figures are deserving of attention and are among the first reported data on bidirectional violence in SSA. Although men reported higher perpetration-only than women, and women reported higher victimization-only than men, consistent with predominant IPV discourse, we found that women reported higher bidirectional physical and emotional IPV as compared to men—and also reported very similar levels of bidirectional sexual IPV as men. In recognition that IPV has different impacts on different groups, such as men and women, we would like to highlight that little is known about men’s experiences as victims of IPV in SSA (Leddy et al., 2019). These findings suggest that men’s experiences of IPV victimization are more likely to occur within the context of mutually violent partnerships, rather than by sole female perpetrators; however, more research is needed to explore diverse experiences of IPV by gender including men.
Other studies have found that individuals experiencing unidirectional IPV—victim-only and perpetrator-only—had a similar risk for negative mental health outcomes, but that individuals experiencing bidirectional IPV were at the highest risk for poor mental health outcomes (Ulloa & Hammett, 2016). It is possible that victimization and perpetration independently have negative health implications, but when combined, there is an additive effect. Additionally, it may be that when both partners are actively contributing to violence in the relationship, the violence may be more severe and therefore have greater implications for health as shown elsewhere (Cascardi & Vivian, 1995). More research is warranted to test these hypotheses and understand why these couples are worse off in terms of their engagement in care. Depressive symptoms and post-traumatic stress disorder, for example, may be higher in individuals within mutually violent partnerships than those who are isolated perpetrators or victims—thus acting as an important mediator. Moreover, more research is needed to investigate the upstream determinants of bidirectional violence such as having multiple overlapping stressors (e.g., lack of money, food insecurity), which may, in turn, lead to sub-optimal engagement in care. Finally, it is important to study the impact of violence severity (e.g., intimate terrorism), which may be more harmful for women’s engagement in HIV care than men’s, given that women tend to experience more severe violence in general.
Our findings have significant implications for future interventions targeting IPV among people living with HIV in SSA. Bidirectional IPV in SSA is an area of research that has received little attention in the epidemiological and intervention literature, and our findings signify a need to conceptualize IPV as a dyadic process that unfolds over time while also recognizing that women tend to be victims at higher rates than men. Interventions to address the health effects of bidirectional IPV (which may be greater than victim or perpetrator-only IPV) may need to intervene with both partners to break the cycle of violence. Couple-based interventions for IPV are rare, particularly for addressing engagement in HIV care and treatment, but may be a viable option by intervening on both partners’ prior trauma and aggression at the same time. Such interventions could also focus on strengthening core aspects of the relationship—trust, intimacy, constructive communication and problem-solving skills—that are likely to improve the ability of couples to manage stressful circumstances before escalating to violence. Efficacious couple-based interventions that address IPV and attempt to shift gender norms could be adapted to specifically address bidirectional IPV among couples living with HIV (Minnis et al., 2015; Speizer et al., 2018; Stern & Nyiratunga, 2017). Conversely, couple-based interventions targeting HIV treatment behaviors could be modified for bidirectional IPV (Bazzi et al., 2016).
There are several strengths of our study. First, the findings held after controlling for potential discrepancies between partners in the reporting of IPV. This allowed us to parse out measurement error using reports from a single partner in isolation, which are prone to social desirability bias (Hamby, 2009), obtaining more reliable results. Second, we examined recent IPV rather than lifetime IPV, which is more common in the IPV literature (Hatcher et al., 2015). Global assessment of IPV (e.g., lifetime or “ever experienced IPV”) can mean a large time delay between exposure and outcome, making it difficult to tease out the mechanisms involved and more difficult to determine when to intervene.
Several limitations are noteworthy. First, the study was not powered to test for gender differences in the effect of IPV on engagement in care outcomes. Thus, we were unable to assess whether being a victim, perpetrator, or both on engagement in care was different for men and women. We suggest that future couples’ studies on IPV and HIV care engagement examine these potential differences. A second limitation is our use of cross-sectional data and the inability to demonstrate causal relationships between IPV and engagement in care outcomes. It is possible that missing pills or appointments could lead to IPV but is less plausible than the reverse direction. We also recruited couples from healthcare centers who were already engaged in care and therefore we might find an even larger effect of IPV on engagement in care in a community-based sample.
Conclusions
These findings make a new contribution to our understanding of how bidirectional IPV impacts engagement in HIV care and treatment, particularly in SSA where the number of people living with HIV on ART is increasing significantly (Joint United Nations Programme on HIV/AIDS, 2017). Our findings highlight high levels of IPV—both unidirectional and bidirectional—among couples living with HIV in Malawi. This underscores the need to develop innovative dyadic interventions that simultaneously address issues of IPV, the factors that drive IPV, and sub-optimal engagement in HIV care.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the National Institute of Mental Health (NIMH) under Grants K01MH107331 and T32MH19105.
Author Biographies
Amy A. Conroy, PhD, is behavioral scientist and assistant professor at the Center for AIDS Prevention Studies at the University of California, San Francisco, with an interest in couple-based approaches to understand and intervene upon intimate partner violence and HIV.
Anna M. Leddy, PhD, is a postdoctoral fellow in the Department of Medicine at the University of California San Francisco. Her research interests include understanding and addressing the impact of gender inequality, and its manifestations such as gender-based violence, on HIV prevention, care and treatment behaviors among high-risk women.
Lynae A. Darbes, PhD, is an associate professor in the Department of Health Behavior and Biological Sciences, and the Center for Sexuality and Health Disparities, School of Nursing, University of Michigan. Her research interests include the development and testing of relationship-focused couples-based behavioral interventions, primarily in the area of HIV prevention and treatment, both in the United States and in sub-Saharan Africa.
Torsten B. Neilands, PhD, Center for AIDS Prevention Studies, Division of Prevention Science, Department of Medicine at the University of California, San Francisco, is a quantitative psychologist with research interests in HIV and substance use health disparities and survey scale development.
James Mkandawire, MPH, is the Research Director at a community-based organization in Zomba, Malawi called Invest in Knowledge. He oversees the fieldwork for a number of health-related studies and has a special interest in integrated approaches for family planning and HIV.
Rob Stephenson, PhD, is a professor in the School of Nursing and Center for Sexuality and Health Disparities at the University of Michigan, USA, with research interests in violence and sexual health.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Anderson JC, Campbell JC, Glass NE, Decker MR, Perrin N, & Farley J (2018). Impact of intimate partner violence on clinic attendance, viral suppression and CD4 cell count of women living with HIV in an urban clinic setting. AIDS Care, 30(4), 399–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson KL (2002). Perpetrator or victim? Relationships between intimate partner violence and well-being. Journal of Marriage and Family, 64(4), 851–863. [Google Scholar]
- Archer J (2000). Sex differences in aggression between heterosexual partners: A meta-analytic review. APA Psychological Bulletin, 126, 651–680. [DOI] [PubMed] [Google Scholar]
- Bates EA (2016). Current controversies within intimate partner violence: Overlooking bidirectional violence. Journal of family violence, 31(8), 937–940. [Google Scholar]
- Bazzi AR, Fergus KB, Stephenson R, Finneran CA, Coffey-Esquivel J, Hidalgo MA, Hoehnle S, Sullivan PS, Garofalo R, & Mimiaga MJ (2016). A dyadic behavioral intervention to optimize same sex male couples’ engagement across the HIV care continuum: Development of and protocol for an innovative couples-based approach (partner steps). JMIR Research Protocols, 5(3), e168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanc A (2001). The effect of power in sexual relationships on sexual and reproductive health: An examination of the evidence. Studies in Family Planning, 32(3), 189–213. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Baty M, Ghandour RM, Stockman JK, Francisco L, & Wagman J (2008). The intersection of intimate partner violence against women and HIV/AIDS: A review. International Journal of Injury Control and Safety Promotion, 15(4), 221–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascardi M, & Vivian D (1995). Context for specific episodes of marital violence: Gender and severity of violence differences. Journal of Family Violence, 10(3), 265–293. [Google Scholar]
- Choi SYP, & Ting K-F (2008). Wife beating in South Africa: An imbalance theory of resources and power. Journal of Interpersonal Violence, 23(6), 834–852. [DOI] [PubMed] [Google Scholar]
- Cohen MH, Cook JA, Grey D, Young M, Hanau LH, Tien P, Levine AM, & Wilson TE (2004). Medically eligible women who do not use HAART: The importance of abuse, drug use, and race. American Journal of Public Health, 94(7), 1147–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy AA (2014a). Gender, power, and intimate partner violence: A study on couples from rural Malawi. Journal of Interpersonal Violence, 29(5), 866–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy AA (2014b). Marital infidelity and intimate partner violence in rural malawi: A dyadic investigation. Archives of Sexual Behavior, 43(7), 1303–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy AA, McKenna SA, Comfort ML, Darbes LA, Tan JY, & Mkandawire J (2018). Marital infidelity, food insecurity, and couple instability: A web of challenges for dyadic coordination around antiretroviral therapy. Social Science and Medicine, 214, 110–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy AA, Mckenna SA, & Ruark A (2019). Couple interdependence impacts alcohol use and adherence to antiretroviral therapy in Malawi. AIDS and Behavior, 23(1), 201–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntyre JA, & Harlow SD (2004). Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. The Lancet, 363(9419), 1415–1421. [DOI] [PubMed] [Google Scholar]
- Espino SR, Fletcher J, Gonzalez M, Precht A, Xavier J, & Matoff-Stepp S (2015). Violence screening and viral load suppression among HIV-positive women of color. AIDS Patient Care and STDS, 29(S1), S36–S41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filmer D, & Pritchett LH (2001). Estimating wealth effects without expenditure data–or tears: An application to educational enrollments in states of India. Demography, 38(1), 115–132. [DOI] [PubMed] [Google Scholar]
- Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, & Watts CH (2006). Prevalence of intimate partner violence: Findings from the WHO multi-country study on women’s health and domestic violence. The Lancet, 368(9543), 1260–1269. 10.1016/S0140-6736(06)69523-8 [DOI] [PubMed] [Google Scholar]
- Gass JD, Stein DJ, Williams DR, & Seedat S (2011). Gender differences in risk for intimate partner violence among South African adults. Journal of Interpersonal Violence, 26(4), 2764–2789. 10.1177/0886260510390960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, & O’Campo P (2007). HIV/AIDS and intimate partner violence: Intersecting women’s health issues in the United States. Trauma, Violence, & Abuse, 8(2), 178–198. [DOI] [PubMed] [Google Scholar]
- Graham K, Bernards S, Flynn A, Tremblay PF, & Wells S (2012). Does the relationship between depression and intimate partner aggression vary by gender, victim–perpetrator role, and aggression severity? Violence and Victims, 27(5), 730–743. [DOI] [PubMed] [Google Scholar]
- Hamby S (2009). The gender debate about intimate partner violence: Solutions and dead ends. Psychol Trauma, 1, 24–34. [Google Scholar]
- Hampanda KM (2016). Intimate partner violence and HIV-positive women’s non-adherence to antiretroviral medication for the purpose of prevention of mother-to-child transmission in Lusaka, Zambia. Social Science and Medicine, 153, 123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher AM, Smout EM, Turan JM, Christofides N, & Stocki H (2015). Intimate partner violence and engagement in HIV care and treatment among women: A systematic review and meta-analysis. AIDS, 29(16), 2183–2194. [DOI] [PubMed] [Google Scholar]
- Jewkes R (2002). Intimate partner violence: Causes and prevention. The Lancet, 359, 1423–1429. 10.1016/S0140-6736(02)08357-5 [DOI] [PubMed] [Google Scholar]
- Johnson MO, Dilworth SE, Taylor JM, Darbes LA, Comfort ML, & Neilands TB (2012). Primary relationships, HIV treatment adherence, and virologic control. AIDS and Behavior, 16(6), 1511–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. (2017). Ending AIDS: Progress towards the 90-90-90 targets. Global AIDS Update. https://www.unaids.org/en/resources/campaigns/globalAIDSupdate2017
- Koenig MA, Lutalo T, Zhao F, Nalugoda F, Wabwire-Mangen F, Kiwanuka N, Wagman J, Serwadda D, Wawer M, & Gray R (2003). Domestic violence in rural Uganda: Evidence from a community-based study. Bulletin of the World Health Organization, 81(1). [PMC free article] [PubMed] [Google Scholar]
- Langhinrichsen-Rohling J (2010). Controversies involving gender and intimate partner violence in the United States. Sex Roles, 62(3–4), 179–193. [Google Scholar]
- Leddy AM, Weiss E, Yam E, & Pulerwitz J (2019). Gender-based violence and engagement in biomedical HIV prevention, care and treatment: A scoping review. BMC Public Health, 19(1), 897. 10.1186/s12889-019-7192-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, & Emmons KM (2006). Understanding health behavior change among couples: An interdependence and communal coping approach. Social Science and Medicine, 62(6), 1369–1380. [DOI] [PubMed] [Google Scholar]
- Logan-Greene P, Nurius PS, Hooven C, & Thompson EA (2015). Life course associations between victimization and aggression: Distinct and cumulative contributions. Child and Adolescent Social Work Journal, 32(3), 269–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machtinger E, Haberer J, Wilson T, & Weiss D (2012). Recent trauma is associated with antiretroviral failure and HIV transmission risk behavior among HIV-positive women and female-identified transgenders. AIDS and Behavior, 16(8), 2160–2170. [DOI] [PubMed] [Google Scholar]
- Maman S, Campbell J, Sweat MD, & Gielen AC (2000). The intersections of HIV and violence: Directions for future research and interventions. Social Science and Medicine, 50(4), 459–478. [DOI] [PubMed] [Google Scholar]
- Manchikanti Gómez A (2011). Testing the cycle of violence hypothesis: Child abuse and adolescent dating violence as predictors of intimate partner violence in young adulthood. Youth & Society, 43(1), 171–192. [Google Scholar]
- McMahon JH, Elliott JH, Bertagnolio S, Kubiak R, & Jordan MR (2013). Viral suppression after 12 months of antiretroviral therapy in low-and middle-income countries: A systematic review. Bulletin of the World Health Organization, 91(5), 377–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MDHS. (2016). Malawi demographic and health survey 2015–16. NSO and ORC Macro. [Google Scholar]
- Milaniak I, & Widom CS (2015). Does child abuse and neglect increase risk for perpetration of violence inside and outside the home? Psychology of Violence, 5(3), 246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health Malawi. (2018). Malawi guidelines for clinical management of HIV in children and adults (4th ed.). [Google Scholar]
- Minnis AM, Doherty IA, Kline TL, Zule WA, Myers B, Carney T, & Wechsberg WM (2015). Relationship power, communication, and violence among couples: Results of a cluster-randomized HIV prevention study in a South African township. International Journal of Women’s Health, 7, 517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrell R, Jewkes R, Lindegger G, & Hamlall V (2013). Hegemonic masculinity: Reviewing the gendered analysis of men’s power in South Africa. South African Review of Sociology, 44(1), 3–21. [Google Scholar]
- Mugavero M, Ostermann J, Whetten K, Leserman J, Swartz M, Stangl D, & Thielman N (2006). Barriers to antiretroviral adherence: The importance of depression, abuse, and other traumatic events. AIDS Patient Care and STDS, 20(6), 418–428. [DOI] [PubMed] [Google Scholar]
- Rose RC, House AS, & Stepleman LM (2010). Intimate partner violence and its effects on the health of African American HIV-positive women. Psychological Trauma: Theory, Research, Practice, and Policy, 2(4), 311. [Google Scholar]
- Saltzman LE, Fanslow JL, McMahon PM, & Shelley GA (1999). Intimate partner violence surveillance: Uniform definitions and recommended data elements. Version 1.0. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. [Google Scholar]
- Schafer KR, Brant J, Gupta S, Thorpe J, Winstead-Derlega C, Pinkerton R, Laughon K, Ingersoll K, & Dillingham R (2012). Intimate partner violence: A predictor of worse HIV outcomes and engagement in care. AIDS Patient Care and STDS, 26(6), 356–365. 10.1089/apc.2011.0409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siemieniuk RA, Krentz HB, Miller P, Woodman K, Ko K, & Gill MJ (2013). The clinical implications of high rates of intimate partner violence against HIV-positive women. JAIDS Journal of Acquired Immune Deficiency Syndromes, 64(1), 32–38. [DOI] [PubMed] [Google Scholar]
- Speizer IS, Zule WA, Carney T, Browne FA, Ndirangu J, & Wechsberg WM (2018). Changing sex risk behaviors, gender norms, and relationship dynamics among couples in Cape Town, South Africa: Efficacy of an intervention on the dyad. Social Science and Medicine, 209, 95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern E, & Nyiratunga R (2017). A process review of the Indashyikirwa couples curriculum to prevent intimate partner violence and support healthy, equitable relationships in Rwanda. Social Sciences, 6(2), 63. [Google Scholar]
- Stets JE, & Straus MA (2017). Gender differences in reporting marital violence and its medical and psychological consequences. In Physical violence in American families (pp. 151–166). Routledge. [Google Scholar]
- Stith SM, Rosen KH, Middleton KA, Busch AL, Lundeberg K, & Carlton RP (2000). The intergenerational transmission of spouse abuse: A meta-analysis. Journal of Marriage and Family, 62(3), 640–654. [Google Scholar]
- Straus MA (2008). Dominance and symmetry in partner violence by male and female university students in 32 nations. Children and Youth Services Review, 30(3), 252–275. [Google Scholar]
- Straus MA (2010). Thirty years of denying the evidence on gender symmetry in partner violence: Implications for prevention and treatment. Partner Abuse, 1(3), 332–362. [Google Scholar]
- Temple JR, Weston R, & Marshall LL (2005). Physical and mental health outcomes of women in nonviolent, unilaterally violent, and mutually violent relationships. Violence and Victims, 20(3), 335. [DOI] [PubMed] [Google Scholar]
- Thirumurthy H, Siripong N, Vreeman RC, Pop-Eleches C, Habyarimana JP, Sidle JE, Siika AM, & Bangsberg DR (2012). Differences between self-reported and electronically monitored adherence among patients receiving antiretroviral therapy in a resource-limited setting. AIDS (London, England), 26(18), 2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trimble DD, Nava A, & McFarlane J (2013). Intimate partner violence and antiretroviral adherence among women receiving care in an urban Southeastern Texas HIV clinic. Journal of the Association of Nurses in AIDS Care, 24(4), 331–340. [DOI] [PubMed] [Google Scholar]
- Ulloa EC, & Hammett JF (2016). The effect of gender and perpetrator–victim role on mental health outcomes and risk behaviors associated with intimate partner violence. Journal of Interpersonal Violence, 31(7), 1184–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. (2017). UNAIDS AIDS Data 2017.
- UNAIDS. (2018). Global AIDS Update.
- Weber K, Cole A, Anastos K, Burke-Miller J, Agniel D, & Schwartz R (2012). The effect of gender based violence (GBV) on mortality: A longitudinal study of US women with and at risk for HIV. AIDS, 17–22. [Google Scholar]
- Wilson SM, Sikkema KJ, & Ranby KW (2014). Gender moderates the influence of psychosocial factors and drug use on HAART adherence in the context of HIV and childhood sexual abuse. AIDS Care, 26(8), 959–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zablotska IB, Gray RH, Koenig MA, Serwadda D, Nalugoda F, Kigozi G, Sewankambo N, Lutalo T, Wabwire-Mangen F, & Wawer M (2009). Alcohol use, intimate partner violence, sexual coercion and HIV among women aged 15–24 in Rakai, Uganda. AIDS and Behavior, 13(2), 225–233. [DOI] [PubMed] [Google Scholar]


