The use of digital tools and applications is steadily increasing and can support a range of health information needs1–3. As tools such as patient portals, health trackers, and remote monitoring devices see greater use, research suggests that tools such as health apps and patient portals can foster greater patient engagement, better support for patients outside of the clinic visit, and can improve health outcomes3–9. However, greater reliance on digital tools has the potential to increase disparities between those who have skills and access to digital tools and those who do not and thereby existing health disparities.
According to a recent Brookings Institution report, 15–24% of Americans lack any sort of broadband connection to the Internet with which to use mobile health technology. These differences only increase when examining the issue by income groups: 38% of households earning less than $20,000 lack a broadband subscription10. The digital divide by income exists in both rural and urban areas. As practitioners working at the intersection of digital inclusion and health, we would like to highlight some less visible dimensions of the digital divide and offer suggestions to facilitate digital inclusion and ensure equitable and impactful adoption of mobile health technologies.
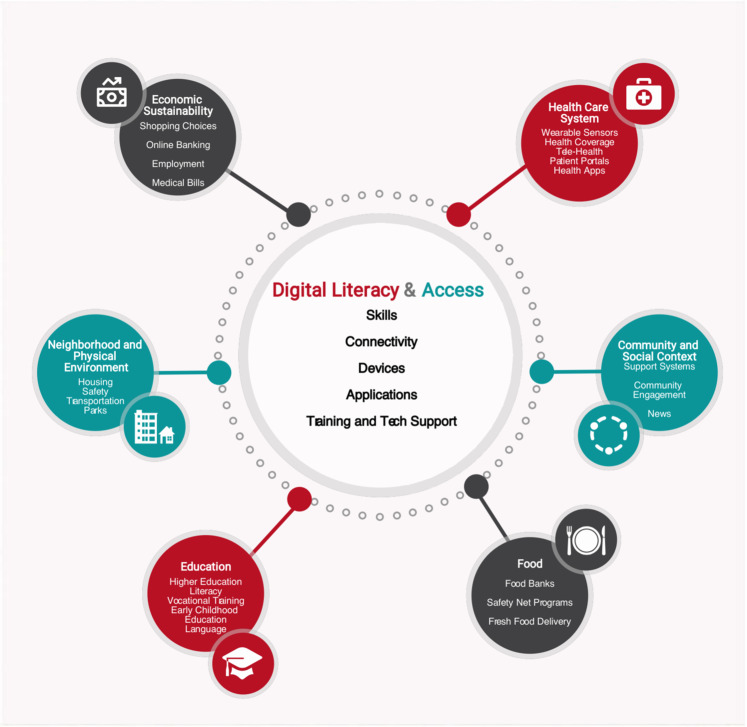
Digital literacies and Internet connectivity have been called the “super social determinants of health” because they address all other social determinants of health (SDOH), as shown in Fig. 111. For example, applications for employment, housing, and other assistance programs, each of which influences an individual’s health, are increasingly, and sometimes exclusively, accessible online. The costs of equipping a person to use the Internet are substantially lower than treating health conditions and the benefits are persistent and significant12, making the efforts to improve digital literacy skills and access valuable tools to reduce disparities.
Fig. 1. Digital literacies and social determinants of health.
Digital literacy and access, including skills, connectivity, devices and training and technical support, relate to all other domains of social determinants of health.
With these challenges in mind, we offer the following recommendations. First, healthcare systems should adopt a digital inclusion-informed strategy regarding mobile health that (1) recognizes their community’s level of access to devices and Internet connectivity and (2) supports patients in their initial and sustained technology use. Digital inclusion refers to the activities necessary to ensure equitable access to and use of information and communication technologies, including (1) affordable broadband Internet service, (2) Internet-enabled devices, (3) access to digital literacy training, (4) quality technical support, and (5) applications and online content designed to enable and encourage self-sufficiency, participation, and collaboration13. These form the foundation for use of mobile technology in healthcare. While knowing whether an individual’s access is important, it is vital for health systems to understand the larger environment shaping patients’ digital experience. Adoption rates are nearing ubiquity among highly educated individuals with at least moderate income, but important pockets of nonadoption remain.
Most mobile health technology requires a data plan and/or home broadband, yet the American Community Survey shows that 40% of low-income households lack a subscription, requiring them to use limited cell plan data or local public wifi hotspots12. These options may appear affordable but they contain important limitations. Using prepaid plans, patients may run out of data or need to prioritize data for specific uses. Even with their lower cost, they may still be unaffordable, particularly for families in need of multiple devices. Open wifi access points are another option but may only be available in public locations in which patients may feel uncomfortable accessing their personal health information.
Prior to the rapid increase in telehealth use due to COVID-19, patient portals to their electronic health record (EHR) were the most common form of mobile health and a gateway to other mobile health applications. However, studies show that lack of Internet access is a leading factor inhibiting use of patient portals14. Smartphones may seem to be a logical and ubiquitous substitute for home Internet, but significant gaps still exist for rural, poor, and older adults. Research shows that nearly one-half of older adults and 30% of those earning less than $30,000 own a smartphone and many low-income households share devices, raising both access and privacy issues15. Understanding the nuances of access in the communities they serve can help healthcare systems implement more inclusive strategies.
Digitally inclusive strategies of health system adoption also support patients in their use of technology at all levels and should include digital skill training, particularly for recent adopters of technology or those who may have devices with limited features. Patients may also need assistance with setting up email and patient portal accounts. In addition, it is critical to provide ongoing support for patients, reduce medical jargon, and provide interpretive resources, and ensure that technology and training are offered equitably to all patients, not just to those who are confident enough to request help16.
Second, we recommend systematically assessing individual patients’ access and digital literacies. This became particularly clear since the rapid and pervasive shift to telehealth during the COVID-19 pandemic. Simply asking patients what devices they own and how they access the Internet is not typical in the clinical context, but this information can shape the type of technology a clinician can recommend. The lack of routine assessment prior to COVID-19 meant that some patients fell between the cracks as care shifted to nearly all virtual17. Incorporating this and other SDOH into the EHR encourages more consistent documentation and allows assessment of population-level metrics of access18. When digital skill and connectivity gaps are assessed systematically and universally, a health system can document overall population-level metrics, examine disparities, and track changes over time.
Third, health systems should partner with community organizations with expertise in training in digital literacy skills and facilitating connectivity. Libraries not only offer the Internet but also provide a spectrum of training services from basic digital literacies to skills required for specific devices and applications. Some communities have leveraged community health workers and patient navigators to screen and refer patients for gaps in basic digital literacies and connectivity19,20. They can provide hands-on training in the use of mobile health technologies for patients who do have adequate digital access. Allied health professional education programs leverage a “train the trainer” model to prepare the future healthcare workforce to undertake these tasks21–23. The National Digital Inclusion Alliance (NDIA) offers a comprehensive list of organizations across the country that provide digital literacy training and national and local resources for free/low-cost Internet and computers13.
Mobile health technologies hold significant promise to increase the efficiency of care and improve health outcomes. Yet, we must be cognizant of their potential to increase health disparities. National efforts have been undertaken to promote broadband, such as the Federal Communications Commission’s (FCC) Lifeline program that subsidizes the cost of smartphones and Internet service for low-income individuals24,25. However, the Lifeline Program’s impact is limited by low consumer awareness, and the qualification process varies by state and by the service provider. In addition, Internet service may still be unaffordable even with the monthly subsidy. Another program, the Federal Broadband Opportunities Program, supported over 4 million people to get online for the first time with a $4 billion program but those one-time dollars are long gone, leaving a gap in the need for adult digital literacy support. BTOP has only two remaining operational programs with no new funding on the horizon25,26. In response to the current COVID-19 pandemic, the FCC also introduced a variety of programs to increase Internet access for the use of telehealth, including paying for devices and access. However, the future of these programs after the COVID-19 pandemic is unclear13. As clinical care incorporates more technology in more contexts, we suggest the recommendations above to facilitate equitable adoption of mobile health technology.
Author contributions
All authors contributed to the writing of this paper. C.S. conceived the paper and created an initial draft. A.S., J.A., J.C., B.C., and A.S. shaped future drafts and development of the figure included in the paper. All authors approved the final draft.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gordon WJ, Landman A, Zhang H, Bates DW. Beyond validation: getting health apps into clinical practice. npj Digit. Med. 2020;3:1–6. doi: 10.1038/s41746-019-0212-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahern DK, Woods SS, Lightowler MC, Finley SW, Houston TK. Promise of and potential for patient-facing technologies to enable meaningful use. Am. J. Prev. Med. 2011;40:S162–S172. doi: 10.1016/j.amepre.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Alessa T, Abdi S, Hawley MS, de Witte L. Mobile apps to support the self-management of hypertension: systematic review of effectiveness, usability, and user satisfaction. JMIR mHealth uHealth. 2018;6:e10723. doi: 10.2196/10723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cahn A, Akirov A, Raz I. Digital health technology and diabetes management. J. Diabetes. 2018;10:10–17. doi: 10.1111/1753-0407.12606. [DOI] [PubMed] [Google Scholar]
- 5.Whitehead L, Seaton P. The effectiveness of self-management mobile phone and tablet apps in long-term condition management: a systematic review. J. Med. Internet Res. 2016;18:e97. doi: 10.2196/jmir.4883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cottrell E, Cox T, O’Connell P, Chambers R. Patient and professional user experiences of simple telehealth for hypertension, medication reminders and smoking cessation: a service evaluation. BMJ Open. 2015;5:e7270. doi: 10.1136/bmjopen-2014-007270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shimada S. L., et al. Patient-provider secure messaging in VA: variations in adoption and association with urgent care utilization. Med. Care S21–S28 (2013). [DOI] [PubMed]
- 8.McAlearney AS, et al. Empowering patients during hospitalization: perspectives on inpatient portal use. Appl. Clin. Inform. 2019;10:103–112. doi: 10.1055/s-0039-1677722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mattingly TJ, Tom SE, Stuart B, Onukwugha E. Examining patient-provider relationship (PPR) quality and patient activation in the Medicare population. Aging Clin. Exp. Res. 2017;29:543–548. doi: 10.1007/s40520-016-0600-z. [DOI] [PubMed] [Google Scholar]
- 10.Tomer, A., Fishbane, L., Siefer, A., Callahan, B. Digital Prosperity: How Broadband can Delvier Health and Equity to All Communities. (Metropolitan Infrastructure Initiative: Brookings Institution, 2020).
- 11.Gibbons, C. Digital Access Disparities: Policy and Practice Overview. Panel Discussion, Digital Skills and Connectivity as Social Determinants of Health. Sheon, A Conference Report: Digital Skills: A Hidden “Super” Social Determinant of Health: Interdisciplinary Association for Population Health Science. (2018).
- 12.Schartman-Cycyk, S., Meisser, K. Bridging the gap: what affordable, uncapped internet means for digital inclusion. In (ed Beacon M.) (2017).
- 13.National Digital Inclusion Alliance. https://www.digitalinclusion.org/definitions/ (2019).
- 14.Perzynski AT, et al. Patient portals and broadband internet inequality. J. Am. Med. Inform. Assoc. 2017;24:927–932. doi: 10.1093/jamia/ocx020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raine, L. Digital Divides 2016. In: Pew Research Center, 2016.
- 16.Grossman LV, et al. Interventions to increase patient portal use in vulnerable populations: a systematic review. J. Am. Med. Inform. Assoc. 2019;26:855–870. doi: 10.1093/jamia/ocz023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sundar KR. A patient with COVID-19 is left behind as care goes virtual. Health Aff. 2020;39:1453–1455. doi: 10.1377/hlthaff.2020.00447. [DOI] [PubMed] [Google Scholar]
- 18.Zhang X, et al. Role of health information technology in addressing health disparities: patient, clinician, and system perspectives. Med. Care. 2019;57:S115–S120. doi: 10.1097/MLR.0000000000001092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheon A., Carrol L. How can health systems leverage technology to engage patients?. in (ed Marx E. W.) Voices of Innovation: Fulfilling the Promise of Information Technology in Healthcare. (Taylor and Francis, Washington, DC, 2018).
- 20.McAlearney AS, et al. High touch and high tech (HT2) proposal: transforming patient engagement throughout the continuum of care by engaging patients with portal technology at the bedside. JMIR Res. Protoc. 2016;5:e221. doi: 10.2196/resprot.6355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Winkle B, Carpenter N, Moscucci M. Why aren’t our digital solutions working for everyone? AMA J. Ethics. 2017;19:1116–1124. doi: 10.1001/journalofethics.2017.19.11.stas2-1711. [DOI] [PubMed] [Google Scholar]
- 22.Harris K, Jacobs G, Reeder J. Health systems and adult basic education: a critical partnership in supporting digital health literacy. Health Lit. Res. Pract. 2019;3:S33–S36. doi: 10.3928/24748307-20190325-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheon AR, Bolen SD, Callahan B, Shick S, Perzynski AT. Addressing disparities in diabetes management through novel approaches to encourage technology adoption and use. JMIR Diabetes. 2017;2:e16. doi: 10.2196/diabetes.6751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Commission FC. Lifeline Support for Affordable Communications. Secondary Lifeline Support for Affordable Communications. https://www.fcc.gov/consumers/guides/lifeline-support-affordable-communications (2020).
- 25.Administration. AANTaI. Final report: social and economic impacts of the Broadband Technology Opportunities Program. (2014).
- 26.Jayakar K, Park E-A. Reforming the lifeline program: regulatory federalism in action? Telecommun. Policy. 2019;43:67–75. doi: 10.1016/j.telpol.2018.04.001. [DOI] [Google Scholar]