Abstract
Background and aims
To assess the psychometric properties of the Fear of COVID-19 (FCV–19S) scale and to determine its associated factors among the Pakistani patients with diabetes.
Methods
This observational study was conducted in 24-h helpline service, a department of Baqai Institute of Diabetology and Endocrinology (BIDE). Study duration was from August to September 2020. The target population was registered adult patients with type 2 diabetes aged >16 years. Baseline demographic details were obtained from hospital management system of BIDE. Forward-backward translation method was used to translate the existing Fear scale (FCV–19S). Symptoms of depressive disorder were assessed through Patient Health Questionnaire (PHQ9).
Results
Total of 380 participants with mean age 51.93 ± 12.03 years contributed in the study. Three factors loading and item correlation of fear COVID-19 explained 96% of total variance having unidimensional Cronbach’s alpha of 0.881. All demographic indicators that showed significance in univariate model were included in multivariate model. Females had more fear for COVID-19 compared to males (OR = 1.73, 95% CI (1.15–2.6)), whereas current smokers had also showed 4 times more fear than non-smokers (OR = 4.19, 95% CI (1.18–14.83). Depression assessed by PHQ9 showed maximum fear of COVID-19 in participants with moderate depression.
Conclusion
FCV-19S had adequate psychometric properties for assessing effects of pandemic in people with diabetes attending tertiary care center.
Keywords: Psychometric properties, Fear of COVID-19 scale, Diabetic, Pakistan
1. Introduction
The World Health Organization (WHO) declared Novel Corona virus (COVID19) outbreak a global Pandemic on March 11, 2020 [1]. It is already evident that COVID 19 has profound direct and indirect effects on physical, psychological, and social wellbeing, arising against the backdrop of serious mental disorders in Low middle income countries (LMICs) [2,3]. Furthermore, susceptibility for physical complications and mortality from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is pervasive with underlying chronic non-communicable conditions including diabetes [4].
Diabetes and mental health conditions are established synergistic epidemic with impact of biological, social, and psychosocial factors on general health outcomes [5]. Not-surprisingly, there is a growing concern for consequences of environmental stress as this pandemic on mental health especially psychological strain for self-management in people with diabetes in this unprecedented situation [6,7]. The umbrella review of South Asian studies has reflected the existing prevalence of depressive disorders, which is anticipated to be around 38% in diabetic population, though the impact of external additional stress of COVID19 is yet undetermined [8].
However, considering this contextual concern, Ahorsu et al. developed a Fear of COVID-19 Scale (FCV–19S), a rigorous psychometric testing tool to indicate the fear in populations [9]. Furthermore, epidemiological study from Bangladesh has outlined the relationship of individuals’ mental conditions and FCV-19S10. To prevent high transmission rate as well as morbidity and mortality of COVID-19, the validity of instrument to capture an individual’s fear of COVID-19 is both timely and important. Many of people with diabetes are staying at home during COVID-19 pandemic and have fewer social interactions and exercise which give negative effect on physical and mental health. Therefore, the present study was conducted to assess the psychometric properties of the Fear of COVID-19 (FCV–19S) scale and to determine its associated factors among the Pakistani people with diabetes at a tertiary care unit in Karachi, Pakistan.
2. Methodology
This observational study was conducted in the 24-h helpline service, department of Baqai Institute of Diabetology and Endocrinology (BIDE), Baqai Medical University, Karachi-Pakistan. Duration of recruitment was from August to September 2020. The target population was registered adult patients with type 2 diabetes aged >16 years. Hospital Management System (HMS) was used for anonymized extraction of baseline details. Telephonic audio interview was completed due to limitation of face-to-face meetings. Prior informed consent was obtained from each participant. All candidates were explained about the study and were informed of their right to refuse sharing of data at any point in future. Ethical approval was obtained from the Institutional review board of BIDE (IRB no: BIDE/IRB/KABASIT/10/28/20/0281.
2.1. Questionnaires in national language
The forward-backward translation method was used to translate the Fear scale for COVID-19(FCV-19S) and Patient Health Questionnaire (PHQ-9) for depression. The subject expert, Professor of Medicine and a local language expert compiled the translation from English to Urdu after consensus (forward Translation). The final versions of translated forms were asked for translation back into English without reviewing of the original English forms (Backward translation). The approved versions were circulated as pilot to 10 staff members to be completed and then recruited patients.
2.2. Interpretation of the survey forms
FCV-19S screening questionnaire constituted of seven questions, assessing the fear towards COVID19, where higher score is indicative of more fear on the 5-point Likert scale. The indices ranged from scores of 7–35 points [10]. Symptoms of depressive disorder were assessed through Patient Health Questionnaire 9 (PHQ9), each nine-item response is subcategorized on a 4-point Likert scale (0 = not at all, 1 = several days, 2 = more than half of the days, 3 = nearly every day). The scores were categorized into five groups such as no depression (0–4), mild depression (5–9), moderate depression (10–14), moderately severe depression (15–19) and severely severe depression (20–27) [11]. The participants with overall PHQ-9 score of 15 and above were considered for the primary physician review for further management.
2.3. Statistical analysis
All analysis was done using Stata/SE 15.0 for Windows (64bit x86-64). Descriptive statistics as mean ± SD and frequencies with percentages were reported for continuous and categorical data respectively. Descriptive including skewness and kurtosis were also reported, whereas percentage of participants obtaining the highest and lowest possible scores were considered as floor and ceiling, respectively. Psychometric analysis of the scale was performed using two approaches, classical test theory (CTT) and modern test theory (MTT). Item response theory (IRT) using graded response model (GRM) was used to report discrimination and difficulty for the likert scoring items of fear COVID-19 questions. CTT analysis included internal consistency (Cronbach’s α) and confirmatory factor analysis (CFA) was also reported.
Logistic regression analysis for binary categorical outcome variable was performed for establishing the association with the demographic indicators. Multivariate logistic regression model was performed with all demographic indicators having p < 0.05 in univariate logistic analysis.
3. Results
Total of 380 participants with mean age 51.93 ± 12.03 were recruited in the study. Out of these, 205 (53.9%) were males and 175 (46.05%) were females. Almost 92% females were housewife, whereas, out of males, 12% were associated with business, 11.8% were professional and 15% were from labor work. Participants with previous history of smoking or tobacco were 18% whereas 4.5% were observed as current smokers. Depression measured using PHQ9 showed 22.6% of study participants with mild depression and 2.63% had moderate depression (Table 1 ). Table 2 represented descriptive statistics including mean, SD, skewness and kurtosis for all 7 Fear COVID-19 items along with floor and ceiling percentages.
Table 1.
Baseline characteristics of study participants.
| N | 380 |
|---|---|
| Age (Years) | 51.93 ± 12.03 |
| Gender | |
| Male | 205 (53.9) |
| Female | 175 (46.05) |
| Occupational Status | |
| Professional/business | 91 (23.95) |
| Skilled/manual labor | 58 (15.26) |
| Housewife | 161 (42.37) |
| Unemployed/Retired/not known | 70 (18.42) |
| Monthly Income | |
| <30,000 | 17 (4.47) |
| 30,000–60,000 | 41 (10.79) |
| 60,000–90,000 | 65 (17.11) |
| >90,000 | 20 (5.26) |
| Not known | 237 (62.37) |
| Smoking/Tobacco Habit | 68 (17.9) |
| Currently Smoker | 17 (4.5) |
| Depression History | 6 (1.6) |
| Depression assessed by PHQ9 | |
| No/Minimal depression | 284 (74.74) |
| Mild depression | 86 (22.63) |
| Moderate depression | 10 (2.63) |
Data presented as mean ± SD and n (%).
Table 2.
Item properties of the FCV-19S
| Item # | Item description | Mean (SD) | Skewness | Kurtosis | Floor n (%) | Ceiling n (%) |
|---|---|---|---|---|---|---|
| 1 | I am most afraid of corona | 3.16 (1.06) | −0.82 | −0.74 | 1 (0.2) | 40 (9.9) |
| 2 | It makes me uncomfortable to think about corona | 2 (0.57) | 1.12 | 4 | 14 (3.5) | 52 (12.9) |
| 3 | My hands become clammy when I think about corona | 1.94 (0.5) | 0.86 | 5.54 | 8 (2) | 54 (13.4) |
| 4 | I am afraid of losing my life because of corona | 1.96 (0.54) | 1.19 | 5.28 | 13 (3.2) | 54 (13.4) |
| 5 | When I watch news and stories about corona on social media, I become nervous or anxious | 2.26 (0.85) | 0.9 | 0.23 | 57 (14.1) | 48 (11.9) |
| 6 | I cannot sleep because I’m worrying about getting corona | 1.95 (0.51) | 0.95 | 5.5 | 9 (2.2) | 54 (13.4) |
| 7 | My heart races or palpitates when I think about getting corona | 2.02 (0.62) | 1.22 | 3.42 | 20 (4.9) | 55 (13.6) |
Data presented as mean ± SD and n (%).
Table 3 characterized the factor loadings and item correlation of fear COVID-19 according to the factor obtained from the analysis. These three-factor explained 96% of the total variance, where factor 1 explaining 80% of the variance, factor 2 explaining 10% and factor 3 explaining 6% of the variance. A reliability analysis for unidimensional and a three-factor model stated a Cronbach’s alpha of 0.881 for unidimensional, 0.9 for factor 1, 0.924 for factor 2 and 0.679 for factor 3 respectively. Average variance extracted (AVE) was 0.632 and composite reliability (CR) was 0.922 and were acceptable.
Table 3.
Factor loadings and Item total correlations for the three-factor model of the COVID measure.
| Loading | Item correlation | |
|---|---|---|
| Factor 1: Psychological symptoms | ||
| I cannot sleep because I’m worrying about getting corona | 0.862 | 0.841 |
| My heart races or palpitates when I think about getting corona | 0.79 | 0.824 |
| I am afraid of losing my life because of corona | 0.58 | 0.825 |
| Factor 2: Physical symptoms | ||
| It makes me uncomfortable to think about corona | 0.859 | 0.78 |
| My hands become clammy when I think about corona | 0.857 | 0.818 |
| Factor 3: Emotional symptoms | ||
| When I watch news and stories about corona on social media, I become nervous or anxious | 0.661 | 0.77 |
| I am most afraid of corona | 0.515 | 0.764 |
Table 4 represented the univariate and multivariate logistic regression analysis. The outcome variable (COVID-Fear) was computed as binary variable using count of any response as “agree” or “strongly agree” for fear questions. The significant association of presence of fear regarding COVID-19 was seen in females, current smokers and participants with depression (p < 0.05). Females had approximately 2 times more fear for COVID-19 compared to males (OR = 1.73, 95% CI (1.15–2.6)), whereas current smokers were also showed 4 times more fear than non-smokers (OR = 4.19, 95% CI (1.18–14.83)). Depression assessed by PHQ9 had also showed maximum fear of COVID-19 in participants with moderate depression. Severity of depression showed 4 times higher fear of COVID-19 compared to people having no symptoms of depression (OR = 4.2, 95% CI (0.87, 19.99)).
Table 4.
Association between fear of COVID-19 with demographic characteristics.
| Characteristics | COVID-Fear |
Univariate Analysis |
Multivariate Analysis |
|||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Age (years) | ||||||||
| ≤40 | 35 (17.95) | 27 (16.56) | Ref. | |||||
| 41–65 | 134(68.72) | 105(64.42) | 0.98 | 0.56–1.73 | 0.957 | – | – | – |
| >65 | 26 (13.33) | 31 (19.02) | 0.65 | 0.31–1.33 | 0.238 | – | – | – |
| Sex | ||||||||
| Male | 99 (47.83) | 106(61.27) | Ref. | Ref. | ||||
| Female | 108(52.17) | 67 (38.73) | 1.73 | 1.15–2.6 | 0.009 | 1.77 | 1.15–2.73 | 0.009 |
| Occupation | ||||||||
| Professional/business | 45 (21.74) | 46 (26.59) | Ref. | |||||
| Skilled/manual labor | 24 (11.59) | 34 (19.65) | 0.72 | 0.37–1.4 | 0.336 | – | – | – |
| Housewife | 100(48.31) | 61 (35.26) | 1.68 | 1–2.82 | 0.052 | – | – | – |
| Unemployed/Retired/not known | 38 (18.36) | 32 (18.5) | 1.21 | 0.65–2.27 | 0.543 | – | – | – |
| Currently Smoker | ||||||||
| No | 185(89.37) | 166(95.95) | Ref. | Ref. | ||||
| Yes | 14 (6.76) | 3 (1.73) | 4.19 | 1.18–14.83 | 0.026 | 5.58 | 1.53–20.29 | 0.009 |
| Not known | 8 (3.86) | 4 (2.31) | 1.79 | 0.53–6.07 | 0.347 | 1.88 | 0.54–6.61 | 0.320 |
| Depression assessed by PHQ9 | ||||||||
| No/Minimal depression | 145(83.82) | 139(67.15) | Ref. | Ref. | ||||
| Mild depression | 26(15.03) | 60(28.99) | 2.4 | 1.43–4.03 | 0.001 | 2.11 | 1.24–3.6 | 0.006 |
| Moderate depression | 2(1.16) | 8(3.86) | 4.2 | 0.87–19.99 | 0.074 | 4.68 | 0.96–22.68 | 0.055 |
Data presented as n (%).
Ref: Reference category.
All significant demographic variables of univariate analysis were included in multivariate model that showed significant association of females, current smokers and depression severity with fear COVID-19 (p < 0.05).
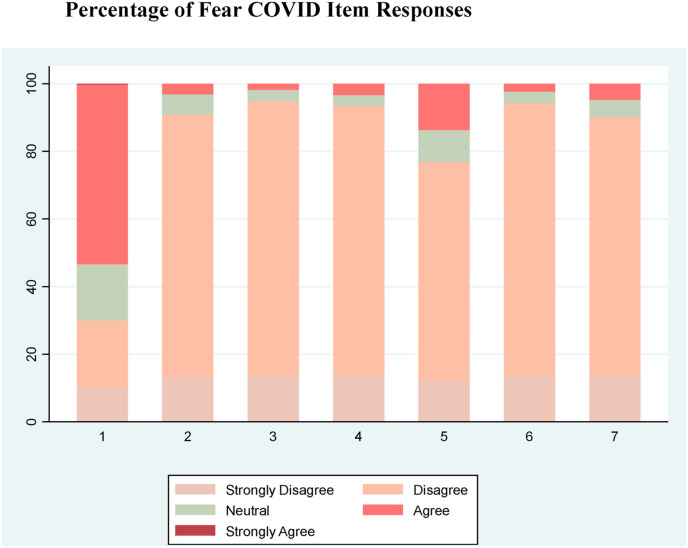
Fig. 1 showed all seven item responses of fear COVID-19 in stacked bar graph. Majority of participants were observed disagreeing for all questions except fear of corona, where 53% participants accepted that they were afraid of corona.
Fig. 1.
Distribution of Fear COVID-19 item responses.
4. Discussion
Initial psychometric results of the Pakistani version of the FCV-19S showed good properties from different types of testing (i.e., CTT, MTT) and internal consistency (as demonstrated by Cronbach’s alpha) in our diabetic population. Factor loadings and item correlation of fear COVID-19 explained 96% of the total variance, representing psychological symptoms, physical symptoms and emotional symptoms.
The FCV-19S is considered to be a valid tool for assessing fear of COVID-19. Cronbach’s alpha for unidimensional three-factor model was 0.881 in our study consistent to Bitan et al., study [12]. Comparing demographic factors, females showed approximately twice more fear for COVID-19 compared to males, current smokers showed 4 times more fear than non-smokers also similar to previous reported data [13]. Our results oppose to Ahorsu et al., study who presented that gender had no effect on the FCV-19S [9]. However, age and socioeconomic status showed no effect on FCV-19S, can be relied upon to assess and deal with the psychological issues emanating from COVID-19 among individuals of all ages and any socioeconomic state. Our results opposed earlier study which showed significant correlation for younger age and higher education levels towards higher coronavirus anxiety scale (CAS) [14].
Previously, it was reported that fear triggers psychological reactions and help people to respond to a threatening agent [15]. We assessed depression using PHQ9, showed the maximum fear of COVID-19 in participants with moderate depression, thus indicating participant’s depression was significantly associated with fear of COVID-19 and concerns regarding lockdown. Our results are similar to Iranian, Italian and Bangla validation studies, who reported significant positive associations between depression and FCV-19S score [10,12,16],. In previous study, the FCV-19S was significantly correlated with depression, anxiety, perceived infectability, and germ aversion also suggesting that individuals with severe fear of COVID-19 may have these underlying comorbid disorders [17]. The Centers for Disease Control and Prevention (CDC) had also reported that fear and anxiety of COVID-19 patients can be overwhelming about their health [18]. Psychological disorders such as symptoms of depression are more likely to developed due to lack of clarity about different risk levels including privacy concerns, treatment plans and difficulty in approaching to physician [19,20]. We are also in agreement with previous studies that showed unclear statement as “to whether being depressed heightens the fear concerning COVID-19 or whether the fear concerning COVID-19 heightens depression (or both)” [21].
In conclusion, depression assessed by PHQ9 showed the maximum fear of COVID-19 in participants with moderate depression suggesting that FCV-19S has good psychometric properties and can be utilized in studies assessing the effects of the pandemic in people with diabetes visiting tertiary care center in Pakistan.
We used convenience sampling and no formal diagnosis on mood disorders e.g., anxiety, so the sensitivity and specificity of the scale was not determined and is in our limitations Also this is a single centered study so the findings could not be generalized to whole population. Further multicentered studies in patients with diabetes and in the general population are needed. In our study, single-factor structure of the scale was based, though confirmatory factor analysis on its factor structure are still essential.
Funding source
No funding sources.
Author contributions:
Abdul Basit K: Concept, design, study conducted, literature search, wrote the manuscript
Bin Zafar A: Concept, design, edited and approved the manuscript
Fawwad A: Concept, design Edited and approved the manuscript
Waris N: Literature search, wrote the manuscript
Shaheen F: Analysis & interpretation of data, edited and approved the manuscript
Basit A: Concept, design reviewed and approved the manuscript
Declaration of competing interest
There is no declaration of interest or conflict of interest.
References
- 1.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed: Atenei Parmensis. 2020 Mar 19;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020 Apr 15;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel V., Saxena S., Lund C., Thornicroft G., Baingana F., Bolton P. The Lancet Commission on global mental health and sustainable development. Lancet. 2018 Oct 27;392(10157):1553–1598. doi: 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]
- 4.Katulanda P., Dissanayake H.A., Ranathunga I., Ratnasamy V., Wijewickrama P.S., Yogendranathan N. Prevention and management of COVID-19 among patients with diabetes: an appraisal of the literature. Diabetologia. 2020 May 14:1–3. doi: 10.1007/s00125-020-05164-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bădescu S.V., Tătaru C., Kobylinska L., Georgescu E.L., Zahiu D.M., Zăgrean A.M. The association between diabetes mellitus and depression. J Med Life. 2016 Apr;9(2):120. [PMC free article] [PubMed] [Google Scholar]
- 6.Morgan C., Rose N. Multidisciplinary research priorities for the COVID-19 pandemic. The lancet. Psychiatry. 2020 Jul;7(7):e33. doi: 10.1016/S2215-0366(20)30230-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mukhtar S., Mukhtar S. Letter to the editor: mental health and psychological distress in people with diabetes during COVID-19. Metab Clin Exp. 2020 Jul 1:108. doi: 10.1016/j.metabol.2020.154248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hossain M., Purohit N., Sultana A., Ma P., McKyer E.L., Ahmed H.U. Prevalence of mental disorders in South Asia: an umbrella review of systematic reviews and meta-analyses. Asian J Psychiatr. 2020 Apr 8:102041. doi: 10.1016/j.ajp.2020.102041. [DOI] [PubMed] [Google Scholar]
- 9.Ahorsu D.K., Lin C.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addiction. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sakib N., Bhuiyan A.I., Hossain S., Al Mamun F., Hosen I., Abdullah A.H. Psychometric validation of the Bangla fear of COVID-19 scale: confirmatory factor analysis and rasch analysis. Int J Ment Health Addiction. 2020 May 11;11:1–12. doi: 10.1007/s11469-020-00289-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gallis J.A., Maselko J., O’Donnell K., Song K., Saqib K., Turner E.L. Criterion-related validity and reliability of the Urdu version of the patient health questionnaire in a sample of community-based pregnant women in Pakistan. PeerJ. 2018 Jul 17;6:e5185. doi: 10.7717/peerj.5185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bitan D.T., Grossman-Giron A., Bloch Y., Mayer Y., Shiffman N., Mendlovic S. Fear of COVID-19 scale: psychometric characteristics, reliability and validity in the Israeli population. Psychiatr Res. 2020 May 15:113100. doi: 10.1016/j.psychres.2020.113100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hossain M.A., Jahid M.I., Hossain K.M., Walton L.M., Uddin Z., Haque M.O. Knowledge, attitudes, and fear of COVID-19 during the rapid rise period in Bangladesh. PloS One. 2020;15(9) doi: 10.1371/journal.pone.0239646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee S.A. Coronavirus Anxiety Scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020 Jul 2;44(7):393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- 15.Ferraro K.F., Grange R.L. The measurement of fear of crime. Socio Inq. 1987;57(1):70–97. [Google Scholar]
- 16.Kwasi Ahorsu D., Ying Lin C., Saffari M., Griffiths D., H Pakpour A. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addiction. 2020 Mar 20:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pakpour A.H., Griffiths M.D. The fear of COVID-19 and its role in preventive behaviors. J Concurr Disorders. 2020 Apr 3;2(1):58–63. https://concurrentdisorders.ca/2020/04/03/the-fear [Google Scholar]
- 18.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19). Daily life and coping. Stress and Coping. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Fmanaging-stress-anxiety.html#stressful Available from.
- 19.Desclaux A., Badji D., Ndione A.G., Sow K. Accepted monitoring or endured quarantine? Ebola contacts’ perceptions in Senegal. Soc Sci Med. 2017;178:38–45. doi: 10.1016/j.socscimed.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 20.Samrah S.M., Al-Mistarehi A.H., Aleshawi A.J., Khasawneh A.G., Momany S.M., Momany B.S. Depression and coping among COVID-19-infected individuals after 10 Days of mandatory in-hospital quarantine, Irbid, Jordan. Psychol Res Behav Manag. 2020;13:823. doi: 10.2147/PRBM.S267459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Menzies R.E., Menzies R.G. Death anxiety in the time of COVID-19: theoretical explanations and clinical implications. Cognit Behav Ther. 2020;13 doi: 10.1017/S1754470X20000215. [DOI] [PMC free article] [PubMed] [Google Scholar]