Abstract
This study adapted a chronic illness stigma scale and explored its psychometric properties. The main purposes were to confirm the factor structure of the instrument with this population and address the previous factor intercorrelation discrepancies. Five hundred and fifty-four individuals with myalgic encephalomyelitis or chronic fatigue syndrome completed the adapted stigma scale. Results document the stigma experienced by an international sample of individuals with myalgic encephalomyelitis and chronic fatigue syndrome. Factors demonstrated good internal consistency, and a model fit was found in a confirmatory factor analysis. Participants endorsed high levels of stigma, estrangement, and disclosure. Implications of these findings and future directions are discussed.
Keywords: chronic fatigue syndrome, confirmatory factor analysis, disclosure, estrangement, myalgic encephalomyelitis, stigma
Myalgic encephalomyelitis (ME) and chronic fatigue syndrome (CFS) are debilitating chronic illnesses that involve symptoms such as post-exertional malaise, cognitive impairment, unrefreshing sleep, and other somatic complications (Carruthers et al., 2011; Fukuda et al., 1994; Jason et al., 2001). Several case definitions exist, and each defines slightly different illness profiles (Carruthers et al., 2003, 2011; Fukuda et al., 1994; Institute of Medicine (IOM), 2015; Sunnquist et al., 2017). A number of different diagnostic names have been proposed, including CFS, ME, ME/CFS, and SEID (IOM, 2015; Mihelicova et al., 2016). The lack of consensus for the illness criteria and name may contribute to uncertainty and doubt in physicians and community members (Jason et al., 2018).
If researchers and medical personnel utilize different names and case definitions, the general public may sense this uncertainty and this could contribute to public skepticism for those with the illness. In other words, uncertainty can lead to negative attitudes about people with the illness, as some might misunderstand the illness in spite of its debilitating symptoms and biological impairments (Corradi et al., 2006; Dickson et al., 2007). Shlaes et al. (1999) were the first to create an instrument to measure public attitudes toward ME and CFS. Research utilizing this instrument has found negative public attitudes about patients with ME and CFS (Jason et al., 2002; Nehrke et al., 2017; Shlaes et al., 1999).
As a next step, it is important to understand whether people with ME and CFS feel stigmatized by these public attitudes. Stigmatization is a process in which individuals are the recipients of negative attitudes and discrimination due to attributes that set them apart and mark them as inferior according to people engaged in stigmatization (Crabtree et al., 2010). Perceived stigma refers to beliefs about others’ attitudes toward stigmatized individuals (Busby Grant et al., 2016). It is important for research to explore the perceived stigma of ME and CFS, since people tend to internalize perceived stigma in the form of self-stigma, which has implications for social and health outcomes (Jennings et al., 2015; Lannin et al., 2016). Research has shown that stigma decreases help-seeking and serves as a risk factor for negative well-being, depression, and suicidality (Clement et al., 2015; Hutton et al., 2013; Looper and Kirmayer, 2004; Sehlo and Bahlas, 2013). Patients with ME and CFS who perceive stigma associated with their illness are more likely to experience depression and suicidal ideation (McManimen et al., 2018). There is a need to explore the role of perceived stigma for people with ME and CFS and the related variables that may influence patient experiences.
One instrument that measures perceived stigma and related variables is the Facial Pain Stigma Scale (FPSS), which was developed for patients with Temporomandibular Pain and Dysfunction Syndrome (Lennon et al., 1989). This measure was created based on previously established stigma instruments in combination with clinical experiences as reported in interviews. Problematic items were removed based on feedback from people with lived experience. The instrument included factors measuring perceived stigma and stigma-related constructs, titled psychological attribution, estrangement, and disclosure. Using principal component analysis, Lennon et al. (1989) found that estrangement was significantly correlated with psychological attribution and disclosure, but psychological attribution was not significantly correlated with disclosure. The first factor, psychological attribution, measures perceived stigma. The second factor, estrangement, is most accurately defined as a construct tied to emotional loneliness that involves a lack of relatedness to others (Andersson, 1986). Individuals are likely to feel estranged due to their stigmatized illness because they may be less likely to be understood and more likely to be avoided by others (Mak et al., 2014). The third factor, disclosure, is a complex process for those with stigmatized identities because they may utilize sharing as an attempt to feel understood by others, but they may suffer adverse effects from doing so (Chaudoir and Fisher, 2010).
Several studies have applied the FPSS to patients with ME and CFS. For example, Green et al. (1999) surveyed 44 patients with ME and CFS and found high reports of stigma, as most participants felt estranged, many reported that others attributed their illness to psychological problems, and disclosure was the most common coping mechanism (Green et al., 1999). Although these authors used the FPSS to study the instrument’s relationship to causes of stigma, the sample size was small (preventing the use of factor analysis), and these investigators did not report intercorrelations of the factors that had been found by Lennon et al. (1989). The FPSS was also used by Looper and Kirmayer (2004), who found that 42 people with CFS reported higher stigma than those with fibromyalgia, irritable bowel syndrome, multiple sclerosis, rheumatoid arthritis, and irritable bowel disease. In addition to the small sample size, intercorrelations among the factors were also not reported. In another study of individuals with CFS or fibromyalgia, mental illness, or other chronic illness, McInnis et al. (2015) also used the FPSS and found that 40 women with CFS and fibromyalgia reported similar levels of psychological attribution to those with mental illness, and higher levels than those with other chronic illness. Women with CFS and fibromyalgia experienced more estrangement than those with mental illness and other chronic illness. Once again, the small sample size precluded any factor analytic investigation, and as this study combined CFS with fibromyalgia, it is unclear whether the stigma found is attributable to CFS exclusively.
There is a need for factor analytic studies as well as the reporting of intercorrelations among the factors for patients with ME and CFS, similar to those that have been conducted with Temporomandibular Pain and Dysfunction Syndrome (Lennon et al., 1989). A better understanding of the ways in which stigma and related variables relate to those with ME and CFS might help target efforts toward improving patient experiences. This study had an adequate sample size of ME and CFS patients for confirming the factor structure and intercorrelations among the factors of the FPSS. In accordance with the results from Lennon et al. (1989), we predicted significant correlations between estrangement and psychological attribution, as well as estrangement and disclosure; however, no significant correlations were predicted for psychological attribution and disclosure.
Method
Procedure
Participants were recruited with convenience sampling through social media, patient advocacy newsletters, Internet forums, and patient organization websites. The study was approved by the DePaul University Institutional Review Board and participants provided written informed consent. Participants were English speakers with current, self-reported diagnoses of ME or CFS. Participants completed a battery of tests that included the adapted ME and CFS Stigma Scale analyzed in this study. The survey was completed using an online survey tool, Research Electronic Data Capture (Harris et al., 2009).
Participants
Data from 554 individuals with ME and/or CFS were analyzed in this study (Mage = 48.06, SD = 12.96). Females made up 87.9 percent of the sample, 12.0 percent identified as male, and 0.2 percent as other. The international sample included individuals from the United States (33.0%) and other countries (67.0%), such as Norway, the United Kingdom, Australia, and Canada. The sample was 98.2 percent White, 1.1 percent Asian/Pacific Islander, 1.1 percent American Indian or Alaska Native, 0.2 percent other, and 2.2 percent were of Latino or Hispanic origin. Participants had the option to endorse multiple races and ethnicities; therefore, the race/ethnicity total is greater than 100 percent. These demographic characteristics are representative of the population of ME and CFS participants in research.
Measures
ME and CFS Stigma Scale.
The original FPSS (Lennon et al., 1989) was adapted for this study. First, ME and CFS–relevant language was applied to items (Lennon et al., 1989). For instance, the original item, “Many people assume that having facial pain is a sign of personal weakness” was replaced with “Many people assume that having ME or CFS is a sign of personal weakness.” In addition, the responses were adapted to a 4-point Likert scale (Strongly Disagree–Strongly Agree) to remain consistent with other scales in the battery.
The adapted scale consisted of three factors with 16 items. The psychological attribution factor measured perceived stigma, while the other two factors, estrangement and disclosure, measured stigma-related experiences. An item representing psychological attribution is: “Many people believe that a person with ME or CFS is just as emotionally stable as the average person.” An example of the estrangement items is: “I often feel totally alone with my illness.” An example of the disclosure items is: “I feel it is my duty to help educate the public about problems involving ME or CFS.” The original FPSS demonstrated good internal consistency when tested on individuals with Temporomandibular Pain and Dysfunction Syndrome (disclosure α = .72; psychological attribution α = .82; and estrangement α = .84).
Sociodemographics.
Participants completed sociodemographic questions regarding age, sex, race, ethnicity, and nationality.
Statistical analysis
Confirmatory factor analysis (CFA) was conducted with MPlus, Version 7, to determine the model’s fit with a population of individuals with ME and CFS. While universal cut-off points do not exist for fit indices, our study abided by the following guidelines. Adequate or good fit was indicated by a root mean square error approximation (RMSEA) less than or equal to .05, a standardized root mean square residual (SRMR) less than or equal to .08, and a Comparative Fit Index (CFI) or Tucker–Lewis Index (TLI) greater than or equal to .90 (Brown, 2006). An insignificant chi-square test of model fit result indicated good fit. Reporting this result is standard practice, although this test is not a reliable measure of fit with large sample sizes (Brown, 2006). Assuming adequate properties of the adapted measure, we used descriptive statistics to explore the endorsement of stigma items. Means and standard deviations of item and factor endorsement were examined.
Results
Previous research utilized orthogonal rotation (Lennon et al., 1989); however, factors were found to be correlated; therefore, a CFA was conducted with oblique rotation. After examination of modification indices, a covariation between items 1 and 2 was added, and item 7 was loaded onto both the psychological attribution and estrangement factors, which are strategies recommended by McDonald and Ho (2002). Fit indices were re-examined with these modifications. The three-factor model demonstrated good fit across fit indices, χ2 (99, N = 554) = 214.203, p < .05, RMSEA = .046, CFI = .954, TLI = .944, SRMR = .042. Cronbach’s alpha found acceptable internal consistency for each factor (psychological attribution = .80, estrangement = .78, and disclosure = .74). Factor loadings indicated adequate fit (see Figure 1).
Figure 1.
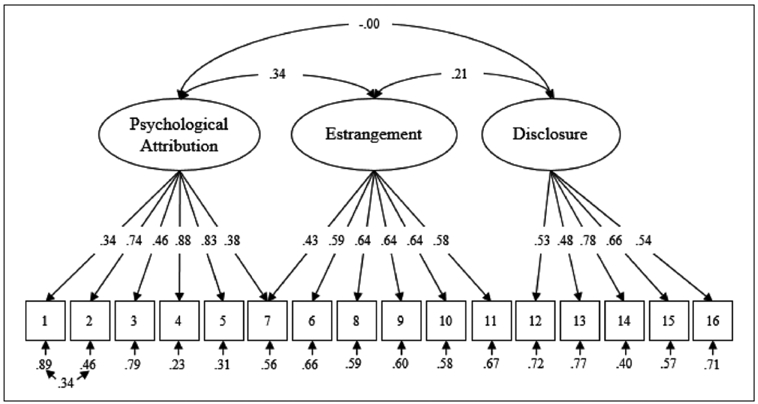
SEM model of relationships among psychological attribution, estrangement, and disclosure for people with ME and CFS.
Table 1 illustrates the descriptive results of the three-factor model. Response choices of Agree and Strongly Agree were considered to endorse an item. All three factors received high mean endorsement, with estrangement (M = 3.48, SD = .45) receiving the highest endorsement, followed by psychological attribution (M = 2.75, SD = .51), and disclosure (M = 2.73, SD = .74). Notably, no participants endorsed item 1. As hypothesized, there was a significant correlation between the psychological attribution and estrangement factors (r(554) = .34, p < .05), as well as estrangement and disclosure (r(554) = .21, p < .05), and no significant correlation was found between psychological attribution and disclosure (r(554) = −.00, p > .05).
Table 1.
ME and CFS Stigma Scale: factor and item endorsement (N = 554).
| ME and CFS Stigma Scale | % endorsed | Mean (SD) | |
|---|---|---|---|
| Psychological attribution subscale | 88.41 | 2.75 (.51) | |
| 1 | When people learn that you have been treated for ME or CFS, they begin to search for flaws in your personality. | 0.00 | 1.91 (.29) |
| 2 | Many people assume that having ME or CFS is a sign of personal weakness. | 73.54 | 2.90 (.77) |
| 3 | Most people believe that a person with ME or CFS is just as emotionally stable as the average person. (R) | 72.28 | 2.91 (.67) |
| 4 | Many people assume that a person who suffers from ME or CFS has a deep-seated psychological problem as well. | 76.18 | 2.94 (.79) |
| 5 | People have a way of associating the occurrence of ME or CFS with psychiatric difficulties. | 82.45 | 3.09 (.75) |
| Estrangement subscale | 99.10 | 3.48 (.45) | |
| 6 | There is a part of me that only other people who have experienced ME or CFS can understand. | 95.12 | 3.63 (.60) |
| 7 | One problem with having ME or CFS is that people don’t believe that you are really ill. | 91.64 | 3.45 (.67) |
| 8 | I have sometimes wished that people could see my illness. | 96.01 | 3.60 (.58) |
| 9 | Having ME or CFS has made me feel very different from other people. | 88.59 | 3.37 (.70) |
| 10 | Most people have no idea what it is like to have ME or CFS. | 99.45 | 3.80 (.42) |
| 11 | I often feel totally alone with my illness. | 74.09 | 3.07 (.88) |
| Disclosure subscale | 87.20 | 2.73 (.58) | |
| 12 | I have found that it is a good idea to help the people close to me understand what treatment for ME or CFS entails. | 78.97 | 3.01 (.74) |
| 13 | When I talk to people close to me about my experience with ME or CFS, I make a special effort to tell them about the experiences I have had that may have caused the illness. | 46.98 | 2.46 (.84) |
| 14 | After I started treatment for ME or CFS, I found myself educating others about the experience. | 67.47 | 2.84 (.84) |
| 15 | I feel it is my duty to help educate the public about problems involving ME or CFS. | 70.26 | 2.96 (.85) |
| 16 | If I were to make a new friend, one of the first things I would do is educate him or her about my ME or CFS. | 42.96 | 2.36 (.86) |
ME: myalgic encephalomyelitis; CFS: chronic fatigue syndrome.
Responses ranged from 1 (Strongly Disagree) to 4 (Strongly Agree). Response choices 3 and 4 endorsed an item. (R) indicates a reverse coded item.
Discussion
This study adapted the existing FPSS Stigma Scale and explored stigma and related experiences of patients with ME and CFS. CFA supported the factor structure of the adapted instrument for people with ME and CFS. The resulting ME and CFS Stigma Scale comprised 16 items and 3 factors (psychological attribution, estrangement, and disclosure). The confirmed factor structure supports previous suggestions that people with ME and CFS experience stigma (Green et al., 1999). Invisible illnesses with unexplained causes are stigmatized more than other medical illnesses (Looper and Kirmayer, 2004), and the present results support stigma-related experiences for patients with ME and CFS.
All factors received high endorsement, indicating high levels of perceived stigma and stigma-related outcomes in people with ME and CFS (see Table 1). This large, international sample showed slightly higher endorsement of all factors than previous research (Green et al., 1999). Similar to findings by Green et al. (1999), estrangement received the most endorsement from participants of all factors. Nearly all (99.1%) participants with ME and CFS felt estranged from others due to their illness. Declining social support may contribute to the high level of estrangement among people with ME and CFS, as patients often feel isolated as a result of social rejection and low energy for relationships (Dickson et al., 2007).
In addition to estrangement, a majority of participants with ME and CFS reported that others attribute their illness to psychological problems. The complicated nature of ME and CFS symptom profiles, case definitions, and lack of known etiology may contribute to a belief that this illness is attributed to the individual’s mental state. Other conditions often attributed to the mental state, such as drug addiction, are also subject to stigma (Corrigan et al., 2009). Individuals with such conditions are often blamed for causing their illness (Åsbring and Närvänen, 2002; Corrigan et al., 2009), suggesting they could simply overcome their condition if they were mentally strong enough. This belief system may negatively impact health outcomes for these stigmatized individuals.
To cope with stigma, most patients (87.2%) with ME and CFS disclosed their illness in some capacity. It is likely that these patients disclose only to their peers with whom they perceive trust, connectedness, and unconditional acceptance (Kaushansky et al., 2017). These patterns are logical, as invisible illness disclosure requires people to expose themselves to scrutiny (Oldfield et al., 2016). As such, risks are heavily weighed and disclosure is often tailored to immediate circumstances (Oldfield et al., 2016).
Regarding correlations among the factors, this study corroborated prior results with Temporomandibular Pain and Dysfunction Syndrome, another invisible illness (Lennon et al., 1989). Estrangement correlated with psychological attribution. The relationship between estrangement and psychological attribution is to be expected, because when patients believe that others attribute their illness to psychological flaws, they are likely to experience social strains and feel estranged due to their illness (Marbach et al., 1990). Estrangement was also correlated with disclosure. The disclosure processes model (DPM) provides a framework to understand this relationship (Chaudoir and Fisher, 2010). According to the DPM, the success of concealable stigmatized identity disclosure is determined by the goals of disclosing, the actual disclosure, and the mediating processes and outcomes, ultimately creating a feedback loop. For instance, an individual who has avoidant disclosure goals may disclose in a style that emphasize negative components of their condition, priming a negative response. This negative disclosure experience is likely to motivate the person to conceal their identity, leading to estrangement, and perpetuating this feedback loop. An individual with more positive disclosure goals may share a more holistic description of their illness during disclosure, which may result in positive outcomes if the confidant is supportive (Chaudoir and Fisher, 2010). The DPM feedback loop illustrates the influence of successful disclosure and highlights the importance of supportive responses from family, friends, and medical professionals.
As hypothesized, disclosure did not relate to psychological attribution. This finding may differentiate invisible illness populations from those with psychological disorders. Perceived stigma relates to disclosure-related constructs in psychological disorders (Blais and Renshaw, 2012); however, these factors did not significantly correlate in a sample of Temporomandibular Pain and Dysfunction Syndrome (Lennon et al., 1989) or in our current sample. Perceived stigma may not directly relate to disclosure in invisible physiological illnesses as one might assume. Perceived stigma has been found to only account for a small proportion of variance in disclosure in physiological illness (Lee and Lee, 2017). Therefore, other factors may be more influential in whether someone chooses a disclosure coping mechanism. For individuals with ME and CFS, these factors may include variables such as level of suffering. In addition, people’s disclosure decisions may be heavily influenced by previous disclosure experiences (Chaudoir and Fisher, 2010).
Perceived stigma and related variables have several implications for individuals with ME and CFS. Stigma decreases quality of life and emotional well-being for those with and without chronic illness (Earnshaw and Quinn, 2012; Hutton et al., 2013; Link et al., 1997). Perceived stigma relates to depression and suicidal ideation for individuals with ME and CFS, which suggests that perceived stigma may be especially dangerous in this population (McManimen et al., 2018). In the workplace, chronic illness stigma leads to identity threat, which ultimately predicts stress and perceived work ability (McGonagle and Barnes-Farrell, 2014). In addition to mental health effects from stress, the long-term impacts can also contribute to flares in autoimmune diseases (McCray and Agarwal, 2011). Emerging research highlights the autoimmune properties of ME and CFS, suggesting that patients may be susceptible to negative health outcomes from stress (Morris et al., 2014). Allostatic load from stress relates to higher ME and CFS symptom severity and frequency (Goertzel et al., 2006).
There were several limitations of this study. Of note, all participants either disagreed or strongly disagreed with item 1, “When people learn that you have been treated for ME or CFS, they begin to search for flaws in your personality.” All other items on the psychological attribution factor received endorsement, suggesting that the phrasing of item 1 may not have resonated with an ME and CFS sample. This item asks about treatment, and it is likely that many participants have not been able to receive treatment, and thus, cannot relate to this portion of the item. Future investigations may also reexamine item 7, “One problem with having ME or CFS is that people don’t believe that you are really ill.” This item loaded on both the psychological attribution and estrangement factors. While this is not ideal, it is reasonable given the item includes components that relate to both constructs. The item was intended for the estrangement factor, but it also overlaps with the psychological attribution construct because it addresses the idea that people may not believe the illness is real. An additional issue is that we used only three of the four factors from the original FPSS. The factor measuring secrecy was not included in the battery because an advocate of the patient community suggested it would be uncomfortable for patients with ME and CFS to fill out, and it had the unwitting iatrogenic possibility of encouraging them to keep their illness to themselves. In addition, the secrecy factor had the lowest endorsement rates in previous studies (Green et al., 1999), which suggests this factor may not describe this construct in a way that is most relevant to ME and CFS.
In summary, the newly confirmed ME and CFS Stigma Scale demonstrated high levels of stigma and related variables for people with the illness. Stigma may serve as a risk factor for a variety of social and health problems (Clement et al., 2015; Hutton et al., 2013; Looper and Kirmayer, 2004; Sehlo and Bahlas, 2013). This article’s findings bring attention to the high levels of perceived stigma in ME and CFS. Healthcare professionals, co-workers, friends, and family members need to work together to decrease the stigmatization of patients with ME and CFS. On a structural level, educational interventions can be implemented to decrease physician stigma. These interventions may involve seminars with factual information and videotaped cases, as such interventions have demonstrated effectiveness in improving attitudes toward ME and CFS (Friedberg et al., 2008). Peer-led approaches may be most successful at combatting stigma, so interventions may emphasize the importance of participant research and bringing in guests with lived experience (Murman et al., 2014). In addition to developing a consensus on the name and research case definition, which would reduce some of the ambiguity that professionals have with ME and CFS (Jason et al., 2018), there is also a need to develop treatment interventions that are not stigmatizing to patients, such as pacing and learning to stay within one’s energy envelope (Jason et al., 2013). On an interpersonal level, individuals can focus on active listening when people disclose challenges with ME and CFS. As demonstrated through the DPM, positive disclosure experiences may have profound effects in a patient’s future experiences. Future research can examine the effectiveness of these efforts on perceived stigma and well-being.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of Allergy and Infectious Diseases (Grant number AI05781).
Footnotes
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Andersson L (1986) A model of estrangement—Including a theoretical understanding of loneliness. Psychological Reports 58(3): 683–695. [DOI] [PubMed] [Google Scholar]
- Åsbring P and Närvänen A (2002) Women’s experiences of stigma in relation to chronic fatigue syndrome and fibromyalgia. Qualitative Health Research 12(2): 148–160. [DOI] [PubMed] [Google Scholar]
- Blais RK and Renshaw KD (2012) The association of biological and psychological attributions for depression with social support seeking intentions in individuals with depressive symptoms. Behavioural and Cognitive Psychotherapy 40(5): 605–617. [DOI] [PubMed] [Google Scholar]
- Brown TA (2006) Confirmatory Factor Analysis for Applied Research. New York: Guilford Publications. [Google Scholar]
- Busby Grant J, Bruce CP and Batterham PJ (2016) Predictors of personal, perceived and self-stigma towards anxiety and depression. Epidemiology and Psychiatric Sciences 25(3): 247–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carruthers BM, Jain AK, de Meirleir KL, et al. (2003) Myalgic encephalomyelitis/chronic fatigue syndrome: Clinical working case definition, diagnostic and treatment protocols. Journal of Chronic Fatigue Syndrome 11(1): 7–115. [Google Scholar]
- Carruthers BM, van de Sande MI, De Meirleir KL, et al. (2011) Myalgic encephalomyelitis: International consensus criteria. Journal of Internal Medicine 270(4): 327–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudoir SR and Fisher JD (2010) The disclosure processes model: Understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity. Psychological Bulletin 136(2): 236–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clement S, Schauman O, Graham T, et al. (2015) What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine 45(1): 11–27. [DOI] [PubMed] [Google Scholar]
- Corradi KM, Jason LA and Torres-Harding SR (2006) Exploratory subgrouping in CFS: Infectious, inflammatory, and other. In: Columbus A (ed.) Advances in Psychology Research. Hauppauge, NY: Nova Science Publishers, pp. 115–127. [Google Scholar]
- Corrigan PW, Kuwabara SA and O’Shaughnessy J (2009) The public stigma of mental illness and drug addiction: Findings from a stratified random sample. Journal of Social Work 9(2): 139–147. [Google Scholar]
- Crabtree JW, Haslam SA, Postmes T, et al. (2010) Mental health support groups, stigma, and selfesteem: Positive and negative implications of group identification. Journal of Social Issues 66(3): 553–569. [Google Scholar]
- Dickson A, Knussen C and Flowers P (2007) Stigma and the delegitimation experience: An interpretative phenomenological analysis of people living with chronic fatigue syndrome. Psychology & Health 22(7): 851–867. [Google Scholar]
- Earnshaw VA and Quinn DM (2012) The impact of stigma in healthcare on people living with chronic illnesses. Journal of Health Psychology 17(2): 157–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedberg F, Sohl SJ and Halperin PJ (2008) Teaching medical students about medically unexplained illnesses: A preliminary study. Medical Teacher 30(6): 618–621. [DOI] [PubMed] [Google Scholar]
- Fukuda K, Straus SE, Hickie I, et al. (1994) The chronic fatigue syndrome: A comprehensive approach to its definition and study. Annals of Internal Medicine 121(12): 953–959. [DOI] [PubMed] [Google Scholar]
- Goertzel BN, Pennachin C, de Souza Coelho L, et al. (2006) Allostatic load is associated with symptoms in chronic fatigue syndrome patients. Pharmacogenomics 7(3): 485–494. [DOI] [PubMed] [Google Scholar]
- Green J, Romei J and Natelson BH (1999) Stigma and chronic fatigue syndrome. Journal of Chronic Fatigue Syndrome 5(2): 63–95. [Google Scholar]
- Harris PA, Taylor R, Thielke R, et al. (2009) Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics 42(2): 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton VE, Misajon R and Collins FE (2013) Subjective wellbeing and “felt” stigma when living with HIV. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation 22(1): 65–73. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) (2015) Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Jason LA, Brown M, Brown A, et al. (2013) Energy conservation/envelope theory interventions to help patients with myalgic encephalomyelitis/chronic fatigue syndrome. Fatigue: Biomedicine, Health & Behavior 1(1–2): 27–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jason LA, Fox PA and Gleason KD (2018) The importance of a research case definition. Fatigue: Biomedicine, Health & Behavior 6(1): 52–58. [Google Scholar]
- Jason LA, Taylor RR, Plioplys S, et al. (2002) Evaluating attributions for an illness based upon the name: Chronic fatigue syndrome, myalgic encephalopathy and Florence Nightingale disease. American Journal of Community Psychology 30(1): 133–148. [DOI] [PubMed] [Google Scholar]
- Jason LA, Taylor RR, Stepanek Z, et al. (2001) Attitudes regarding chronic fatigue syndrome: The importance of a name. Journal of Health Psychology 6(1): 61–71. [DOI] [PubMed] [Google Scholar]
- Jennings KS, Cheung JH, Britt TW, et al. (2015) How are perceived stigma, self-stigma, and self-reliance related to treatment-seeking? A three-path model. Psychiatric Rehabilitation Journal 38(2): 109–116. [DOI] [PubMed] [Google Scholar]
- Kaushansky D, Cox J, Dodson C, et al. (2017) Living a secret: Disclosure among adolescents and young adults with chronic illnesses. Chronic Illness 13(1): 49–61. [DOI] [PubMed] [Google Scholar]
- Lannin DG, Vogel DL, Brenner RE, et al. (2016) Does self-stigma reduce the probability of seeking mental health information? Journal of Counseling Psychology 63(3): 351–358. [DOI] [PubMed] [Google Scholar]
- Lee S and Lee B (2017) Disclosure management behaviors in Korean adults with well-controlled epilepsy: Their relation to perception of stigma. Epilepsy & Behavior 67: 28–32. [DOI] [PubMed] [Google Scholar]
- Lennon MC, Link BG, Marbach JJ, et al. (1989) The stigma of chronic facial pain and its impact on social relationships. Social Problems 36(2): 117–134. [Google Scholar]
- Link BG, Struening EL, Rahav M, et al. (1997) On stigma and its consequences: Evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. Journal of Health and Social Behavior 38(2): 177–190. [PubMed] [Google Scholar]
- Looper KJ and Kirmayer LJ (2004) Perceived stigma in functional somatic syndromes and comparable medical conditions. Journal of Psychosomatic Research 57(4): 373–378. [DOI] [PubMed] [Google Scholar]
- McCray CJ and Agarwal SK (2011) Stress and autoimmunity. Immunology and Allergy Clinics of North America 31(1): 1–18. [DOI] [PubMed] [Google Scholar]
- McDonald RP and Ho MR (2002) Principles and practice in reporting structural equation analyses. Psychological Methods 7(1): 64–82. [DOI] [PubMed] [Google Scholar]
- McGonagle AK and Barnes-Farrell JL (2014) Chronic illness in the workplace: Stigma, identity threat and strain. Stress and Health: Journal of the International Society for the Investigation of Stress 30(4): 310–321. [DOI] [PubMed] [Google Scholar]
- McInnis OA, McQuaid RJ, Bombay A, et al. (2015) Finding benefit in stressful uncertain circumstances: Relations to social support and stigma among women with unexplained illnesses. Stress: The International Journal on the Biology of Stress 18(2): 169–177. [DOI] [PubMed] [Google Scholar]
- McManimen SL, McClellan D, Stoothoff J, et al. (2018) Effects of unsupportive social interactions, stigma, and symptoms on patients with myalgic encephalomyelitis and chronic fatigue syndrome. Journal of Community Psychology 46(8): 959–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak WS, Chong EK and Wong CY (2014) Beyond attributions: Understanding public stigma of mental illness with the common sense model. American Journal of Orthopsychiatry 84(2): 173–181. [DOI] [PubMed] [Google Scholar]
- Marbach JJ, Lennon MC, Link BG, et al. (1990) Losing face: Sources of stigma as perceived by chronic facial pain patients. Journal of Behavioral Medicine 13(6): 583–604. [DOI] [PubMed] [Google Scholar]
- Mihelicova M, Siegel Z, Evans M, et al. (2016) Caring for people with severe myalgic encephalomyelitis: An interpretative phenomenological analysis of parents’ experiences. Journal of Health Psychology 21(12): 2824–2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris G, Berk M, Galecki P, et al. (2014) The emerging role of autoimmunity in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Molecular Neurobiology 49(2): 741–756. [DOI] [PubMed] [Google Scholar]
- Murman NM, Buckingham KE, Fontilea P, et al. (2014) Let’s Erase the Stigma (LETS): A quasi-experimental evaluation of adolescentled school groups intended to reduce mental illness stigma. Child & Youth Care Forum 43(5): 621–637. [Google Scholar]
- Nehrke PI, Fox PA and Jason LA (2017) Research volunteers’ attitudes toward chronic fatigue syndrome and myalgic encephalomyelitis. EC Neurology 7(4): 172–178. [PMC free article] [PubMed] [Google Scholar]
- Oldfield M, MacEachen E, Kirsh B, et al. (2016) Impromptu everyday disclosure dances: How women with fibromyalgia respond to disclosure risks at work. Disability and Rehabilitation 38(15): 1442–1453. [DOI] [PubMed] [Google Scholar]
- Sehlo MG and Bahlas SM (2013) Perceived illness stigma is associated with depression in female patients with systemic lupus erythematosus. Journal of Psychosomatic Research 74(3): 248–251. [DOI] [PubMed] [Google Scholar]
- Shlaes JL, Jason LA and Ferrari JR (1999) The development of the chronic fatigue syndrome attitudes test. A psychometric analysis. Evaluation & the Health Professions 22(4): 442–465. [DOI] [PubMed] [Google Scholar]
- Sunnquist M, Jason LA, Nehrke P, et al. (2017) A comparison of case definitions for myalgic encephalomyelitis and chronic fatigue syndrome. Journal of Chronic Diseases and Management 2(2): 1013. [PMC free article] [PubMed] [Google Scholar]


