Abstract
Objective
The purpose of this article is to review the orthopedic literature regarding patient understanding of articular cartilage disease, interpret literature reporting patient expectations for surgical management of articular cartilage injuries of the knee, and review patient-reported outcomes and patient satisfaction with management of these injuries.
Design
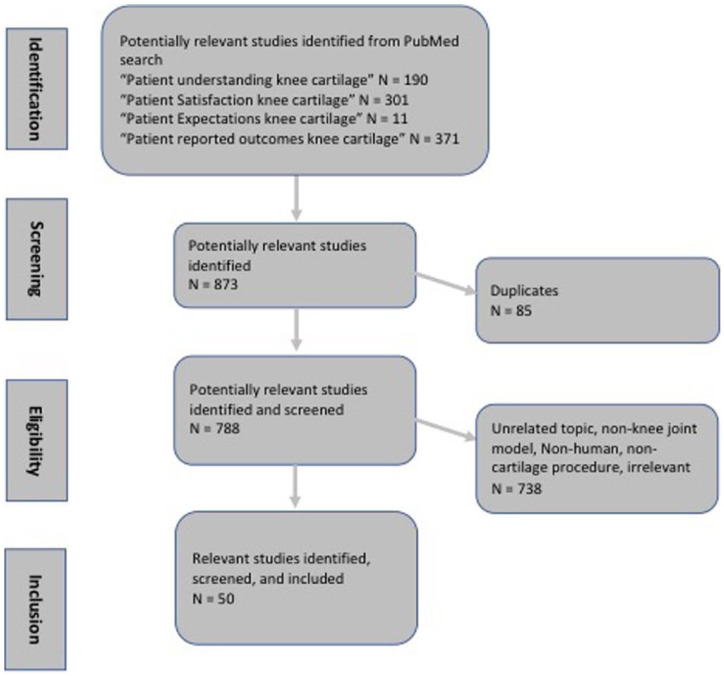
A retrospective review of the current literature using the PubMed database (1980-current) was performed on July 15, 2017. The search terms used were “patient understanding knee cartilage,” “patient satisfaction knee cartilage,” “patient expectation knee cartilage,” and “patient reported outcomes knee cartilage.” All searches were filtered to human studies and English language only and were reviewed by 2 independent reviewers. Studies not relevant to articular cartilage injury and/or surgical management in the knee were excluded. Additional references were found by backtracing references from obtained articles.
Results
The published study search results for the terms: “patient understanding knee cartilage,” “patient satisfaction knee cartilage,” “patient expectation knee cartilage,” and “patient reported outcomes knee cartilage” displayed a total of 873 studies. Two independent reviewers screen all studies A total of 50 published studies were relevant and included.
Conclusion
The subjective and objective clinical outcomes reported are inconsistently obtained resulting in difficulty drawing comparisons between studies. While the relationship between preoperative patient expectations and patient-reported outcomes and patient satisfaction has yet to be well developed, authors have reported patient and injury specific variables associated with superior and inferior outcomes. In conclusion, more work is needed to correlate patient-reported outcomes and satisfaction for cartilage treatments with preoperative expectations and health literacy.
Keywords: patient expectations, patient satisfaction, patient-reported outcomes, articular cartilage, knee
Introduction
Focal cartilage defects of the knee are common and continue to present clinical challenges despite technological and biological advancements. These patients are often young, physically active individuals who may also be affected by concomitant ligamentous, meniscal, or soft tissue injury further complicating the treatment algorithm.1 Recently, there has been interest in evaluating the relationship between patients’ preoperative expectations of clinical outcomes and their actual outcomes. Although within orthopedics there are studies evaluating preoperative expectations, investigations specific to knee articular cartilage repair are sparse with the few existing studies demonstrating that expectations for these procedures are quite high.2 Patient preoperative expectations have been well known to affect the postoperative satisfaction of various orthopedic procedures, with several authors noting a relationship between overly optimistic preoperative expectations and low patient satisfaction.3-9 These investigations highlight the importance of patient education and careful shared decision making in helping set realistic preoperative patient expectations.10-14
The importance of understanding patient expectations prior to surgical intervention has led to the development of validated patient expectation tools such as the Patient Expectations of Shoulder Surgery survey.15 While this tool is specific to shoulder surgery, it represents a movement within orthopedics to attempt to quantify and analyze patient expectations and it seems likely future questionnaires will expand to other joints such as the knee. To adequately evaluate the effects of patient expectations, patient understanding or knowledge of their injury, patient-reported outcome metrics (PROs), and patient satisfaction all must also be evaluated. As authors have recently reported, PROs and patient satisfaction are important metrics for defining successful clinical outcomes, quality of care for insurance and internal control purposes, and provider reimbursement.16-21 Increased patient satisfaction has been suggested to improve patient assessments of their treating physicians and increased compliance with follow-up and treatment regimens, which potentially could improve outcomes.9
The purpose of this article is to review the orthopedic literature regarding patient understanding of articular cartilage disease and interpret literature reporting patient expectations for surgical management of articular cartilage injuries of the knee. In addition, PROs and patient satisfaction with surgical management of these injuries will be reviewed. It is our hypothesis that there will be a paucity of literature regarding patient understanding of articular cartilage injuries and patient expectations for surgical management. An aim of this article is to identify gaps in the literature and offer suggestions on what needs to be done moving forward to help patients understand their chondral injuries, set realistic preoperative expectations and ultimately, achieve high patient satisfaction and associated PROs following surgical management.
Relevant literature was identified using the PubMed database (1980-current) on July 17, 2017. Articles pertaining to patient health literacy regarding articular cartilage in the knee, patient expectations for orthopedic surgery as it pertains to cartilage repair and/or restoration procedures, and subjective and objective outcome studies for these procedures. More specifically, the type of information we were looking for in each article was information pertinent to patient health literacy, patient expectations for treatment of articular cartilage injuries in the knee, current state of outcome reporting in articular cartilage studies, and PROs and patient satisfaction data for articular cartilage surgical treatments. Additional references were found by backtracing references from obtained articles. Of the 873 identified articles, only 50 were relevant and included ( Fig. 1 ). In total, patient preoperative expectations, patient satisfaction, patient education, and PROs where discussed or reported in 52.0% (26/50), 88.0% (44/50), 52.0% (26/50), and 72.0% (36/50) of the included literature, respectively. A concise summary of key findings is included in Table 1 .
Figure 1.
Search algorithm used to identify and screen studies to be included in the review of published literature.
Table 1.
Summary of Key Health Literacy, Patient Expectations, and Clinical Outcomes Findings.
| Summary of Key Findings |
|---|
| • The relationship between health literacy,
preoperative expectations, and patient subjective
outcomes has been well described. • Several patient and injury specific variables, such as increased age and defect size, may be useful to predict patient-reported outcomes (PROs) following cartilage repair or restoration procedures. • Currently, there is a paucity of literature that identifies specific patient demographic variables or PROs that predict patient satisfaction following cartilage restoration. • Future reproducible, efficient point of care education tools may significantly affect preoperative expectations, patient satisfaction, and PROs following articular cartilage surgery. |
Patient Health Literacy of Articular Cartilage and Preoperative Expectations
While numerous studies, including a recent systematic review by Flanigan et al.,22 report approximately 36% incidence of full-thickness chondral defects of the knee on arthroscopy or magnetic resonance imaging (MRI), there remains staggeringly few investigations into patient comprehension of basic anatomy and physiology of articular cartilage and the various treatment options for cartilage injuries. Patient health literacy of cartilage injuries is likely to influence their expectations for treatment, including surgical intervention, as authors have recently reported for anterior cruciate ligament (ACL) reconstruction,17 in addition to improving the informed consent process. In a randomized controlled trial investigation of the informed consent process, Rossi et al.14 demonstrated that providing video informed consent had superior comprehension levels compared to verbal informed consent prior to knee arthroscopy suggesting an avenue through which to engage patients more fully regarding their injury and what to expect from the agreed-upon treatment. Furthermore, Cole et al.16,17 discussed the importance of this relationship between patient comprehension or health literacy, and patient expectations for surgery in influencing PRO metrics and patient satisfaction in patients with ACL17 and rotator cuff injuries.16 The authors were able to identify patient-specific variables associated with high or poor satisfaction with their outcome. Others have evaluated a related topic within orthopedics, namely patient health literacy regarding carpal tunnel surgery and compliance with recommended postoperative care. Waryasz et al.23 administered a questionnaire asking patients who underwent carpal tunnel surgery regarding basic principles of the injury and expected postoperative course demonstrating patients had significant knowledge gaps despite standard preoperative informed consent and standardized postoperative instruction document.
Articular cartilage injuries of the knee are less common and often present with a complex collection of pathologies that does not achieve the same mainstream media attention paid to other orthopedic injuries such as ACL or rotator cuff tears. Given the poor public understanding of ACL injuries and surgical management,24 it is likely to be no different for articular cartilage injuries. The lack of literature in this regard is surprising considering the frequency with which patient satisfaction and PROs are being reported in clinical investigations.25 Significant work is needed going forward to first define weaknesses in basic articular cartilage injury knowledge in these patients, then work to devise reproducible, efficient point of care education tools such as targeted videos or mini-classes taught by ancillary staff (physician assistants, nurse practitioners) to help patients better understand their injury. This in turn should be correlated with preoperative expectations and ultimately, clinical outcomes. It is worth noting, when we use the term “basic knowledge” this is in reference to information regarding location of articular cartilage, ability to regenerate or heal on its own, and its purpose as a smooth surface allowing for bones to articulate without accumulating changes consistent with osteoarthritis.
Current State of Outcome Reporting in Cartilage Repair and Restoration
Makhni et al.26 recently demonstrated substantial variability in outcome reporting for cartilage studies, including PROs and patient satisfaction, in a systematic review of 5 high-impact orthopedic journals. Essentially, outcomes reporting is disjointed within the cartilage repair and restoration literature stagnating the ability to identify demographic, injury, operative, and postoperative variables influencing PROs and patient satisfaction. If the ultimate goal is to provide the highest quality care for patients, how patients perceive their care and their satisfaction with their outcome are of paramount importance.
Many authors have sought to elucidate the impact of specific demographic, preoperative, operative, and postoperative factors on PROs and patient satisfaction. Increased patient age is arguably the most common demographic variable associated with decreased PROs in cartilage repair procedures.27-29 In prospective studies involving osteochondral autograft transplantation (OATs), investigators described significantly better International Knee Documentation Committee (IKDC) scores in patients aged 16 to 30 years when compared with patients older than 40 year.27 Similarly, when comparing microfracture with autologous chondrocyte implantation (ACI) outcomes, it was demonstrated that patients younger than 30 to 40 years had improved IKDC and modified Cincinnati scores regardless of procedure.28 In addition, preoperative factors such as history of previous surgery, number of lesions, location of lesions, and defect size have also been proposed to lower PRO scores.27-30 In a recent retrospective study including 152 mosiacplasty patients (mean lesion size of 3.25 cm2), correlation analysis revealed that increasing patient age (P < 0.001), female sex (P = 0.028), increasing lesion size (P = 0.004), or increasing number of concomitant surgeries (P = 0.0001) were all associated with decreased Lysholm scores independently. In addition, no correlation was found between localization of the lesion, grade of the lesion, or follow-up time.29 Conversely, a systematic review investigating OATs, described significant decrease in Lysholm scores in patellofemoral OATs procedures when compared with those performed to the femoral condyle.27 Moreover, in a systematic review of 36 publications, Erggelet et al.28 demonstrated that the average International Cartilage Repair Society (ICRS) score of patients with femoral condyle lesions improved significantly more than patients with trochlea, tibia, or patella lesions following microfracture at the 36-month follow-up.
When further examining size of cartilage lesions, a systematic review investigating OATs found larger lesions that required plug sizes of between 6.5 and 8.5 mm displayed worse IKDC scores than smaller lesions.27 Similarly, PROs following microfracture has been shown to suffer when the cartilage lesion is greater than 2 to 3 cm2.28,31,32 In a review encompassing randomized controlled trials for surgical treatment of cartilage defects, it was found that 2-year outcomes indicated by Knee injury and Osteoarthritis Outcome Score (KOOS) were better for all procedures involving lesions <2 cm2 in size, but matrix-assisted ACI (MACI)/ACI obtained significantly superior PROs when compared with microfracture in lesions >4.5 cm2.33 Physician understanding of these independent factors and their effects on outcomes such as the role of age, procedure type, and defect size will undoubtedly assist in optimizing and managing patient expectations related to outcomes following the treatment of their chondral disease.
Currently, there is ample documentation to prove that the general postoperative patient satisfaction outcomes for major cartilage repair procedures (ACI, osteochondral allograft transplantation [OCA], OATs, microfracture) have been positive34-37; however, specific demographic, preoperative, operative, and postoperative factors that could significantly affect and predict patient satisfaction with knee cartilage repair techniques has yet to be clearly delineated. The association between preoperative factors such as history of prior cartilage procedure and satisfaction has been variable.38,39 In a cohort study with a total of 56 patients, satisfaction in patients undergoing ACI with history of prior microfracture were compared to patients with no history of prior cartilage repair by using a 4-point Likert-type scale. The group with a history of prior microfracture had significantly lower average satisfaction (P = 0.032) than the group with ACI as primary therapy.38 However, conflicting results were found in a similar cohort study examining OCA in patients with a history of prior microfracture. Patient satisfaction, according to a 5-point Likert-type scale, was recorded at a 10-year follow-up and prior history of microfracture had no significant impact on OCA patient satisfaction.39
The presence of concomitant procedures40,41 on patient satisfaction in cartilage procedures has been variable and is an important consideration considering the frequency with which concomitant meniscal, malalignment, and ligamentous pathology exists with chondral injury. In a case series by Pascual-Garrido et al.,40 86% of patients who received an ACI with anteromedialization tibial tubercle osteotomy with a history of failed microfracture procedure endorsed that they were mostly or completely satisfied with the procedure. In contrast, only 45% of the patients who received an ACI alone reported they were mostly or completely satisfied with the procedure.40 Furthermore, in a study including 396 patients who underwent microfracture, no significant difference was found in satisfaction amongst those who underwent concomitant procedures at the time of microfracture.41 The conflicting data for the majority of cartilage restoration procedures make drawing meaningful conclusions regarding patient specific and injury specific factors associated with inferior or superior outcomes very challenging.
Ebert et al.42 performed a multivariable analysis of demographic, preoperative, or operative variables were examined in MACI patients at 5-year follow-up. The authors reported that factors such as age, sex, body mass index, duration of symptoms, number of previous procedures, defect size, graft compartment, or concomitant procedures had no impact on patient satisfaction. The Torbit regression analysis did reveal that taking longer to full weightbearing (12 vs. 8 weeks) was significantly correlated (P = 0.027) with decreased mean satisfaction on 5-year follow-up satisfaction survey, bringing to light the potential importance of adherence to rehabilitation protocol.42 Currently, there is a paucity of information on specific demographic variables that are significantly connected to satisfaction with articular cartilage repair procedures broadly, but 1 study did display a significant difference between the increased rate dissatisfaction among patients who smoked when compared to nonsmokers.41
Relationship between PROs and Patient Satisfaction
Interestingly, when attempting to predict postoperative patient satisfaction rates, PROs are not generally a reliable method.36,41-43 In a case series of patients who underwent an ACI procedure, Niemeyer et al.36 reported contrast between patient satisfaction and subjective functional outcomes. In the study, a mean IKDC of 74.0 and a mean Lysholm of 71.0 were established at a 5-year follow-up. When evaluating these scores compared with patient satisfaction rates, the authors suggested long-term follow-up satisfaction rates were far higher than the recorded PROs should have indicated. A possible reason for the discordance between satisfaction and PROs, as described by Balain et al.,43 is a response shift. Response shift refers to the hypothesis that a patient’s subjective internal standard of the measurement of symptoms is fluid and can shift over time. This is thought to occur because of the fact that patients think, in retrospect, that they had felt worse preoperatively than they actually did at that time.43 Balain suggests that response shifts can confound PROs and may be responsible for discordance between patient satisfaction and PROs. In an effort to further examine the inconsistencies between patient satisfaction and PROs, Ebert et al.44 designed a cohort study to compare the responsiveness of four commonly used knee PROs at 5 years after cartilage defect repair. Their results indicated that PROs were variable in their ability to significantly predict satisfaction, but the KOOS sports/recreation subscale and “improving in the ability to perform recreationally” were the most predictive PROs of patient satisfaction.44 Not only can this study serve as a guide to improve PROs in order to better predict satisfaction, but it can also help to identify aspects of PROs to target for better patient satisfaction.
Future Directions
Many reports have shown that current patient education materials are insufficient or too advanced for the general population.45-49 Recently, many studies have been aimed at improving the patient education materials we currently use, such as reading resources, websites, and video consents for arthroscopic procedures.14,46,47 Interestingly, in an investigation by Bayar et al.,50 63 patients were randomly divided into 2 groups: one where patients were allowed to watch their own arthroscopic procedures (mostly meniscal surgery), and another group that was not allowed to watch the procedure. The groups then proceeded to fill out the study questionnaire designed to, in part, evaluate patient satisfaction both preoperatively and postoperatively. The group that viewed their own procedure had significantly less dissatisfaction (P = 0.0078). Only 2 of 31 patients (6%) in the watch group had moderate or higher dissatisfaction while this ratio was 12/32 (38%) in group that did not watch. This is just one example of an innovated approach to improving patient engagement and health literacy with their care that led to improved satisfaction. Many physicians including the senior author (BJC), use preoperative electronic education materials, including short videos about the injury and procedure to help prepare patients for surgery from both a health literacy and expectation standpoint. It is important for authors to investigate and track their current methods of education and setting of patient expectations so that these methods may be shared in some form or another with other surgeons to improve our current approaches. As the summation of the aforementioned studies demonstrate, there is significant room for improvement.
Limitations
There are several limitations of this study. This is level V evidence and was designed as a narrative review not a true systematic review given the relative abstract nature of several subtopics. Two independent reviewers conducted systematic literature searches and consensus was used if there was any disagreement in inclusion. It is our belief that the nature of patient health literacy, patients’ preoperative expectations for management and the PROs and patient satisfaction of management are interconnected topics and thus were synthesized in this article.
Conclusion
There exist extremely limited data evaluating patient understanding of their cartilage lesions of the knee and treatment options. While the cartilage literature is robust with patient reported outcome data and patient satisfaction studies, the outcomes reported are disjointed and inconsistently reported resulting in difficulty in comparing and contrasting results between studies. While the relationship between preoperative patient expectations and PROs and patient satisfaction is yet to be well developed, authors have reported patient and injury specific variables associated with superior and inferior outcomes including patient age <40 years resulting in higher satisfaction for many of the most common cartilage repair options. In conclusion, more work is needed going forward to go beyond reporting only PROs and satisfaction for cartilage treatments of the knee and correlate these outcome metrics with preoperative expectations and health literacy of patients for their injury.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Eric J. Cotter  https://orcid.org/0000-0003-2206-8754
https://orcid.org/0000-0003-2206-8754
References
- 1. Mall NA, Harris JD, Cole BJ. Clinical evaluation and preoperative planning of articular cartilage lesions of the knee. J Am Acad Orthop Surg. 2015;23(10):633-40. [DOI] [PubMed] [Google Scholar]
- 2. Niemeyer P, Porichis S, Salzmann G, Südkamp NP. What patients expect about autologous chondrocyte implantation (ACI) for treatment of cartilage defects at the knee joint. Cartilage. 2012;3(1):13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Frouzakis R, Herren DB, Marks M. Evaluation of expectations and expectation fulfillment in patients treated for trapeziometacarpal osteoarthritis. J Hand Surg Am. 2015;40(3):483-90. [DOI] [PubMed] [Google Scholar]
- 4. Harris IA, Harris AM, Naylor JM, Adie S, Mittal R, Dao AT. Discordance between patient and surgeon satisfaction after total joint arthroplasty. J Arthroplasty. 2013;28(5):722-7. [DOI] [PubMed] [Google Scholar]
- 5. Mannion AF, Impellizzeri FM, Naal FD, Leunig M. Fulfilment of patient-rated expectations predicts the outcome of surgery for femoroacetabular impingement. Osteoarthritis Cartilage. 2013;21(1):44-50. [DOI] [PubMed] [Google Scholar]
- 6. Rosenberger PH, Jokl P, Cameron A, Ickovics JR. Shared decision making, preoperative expectations, and postoperative reality: differences in physician and patient predictions and ratings of knee surgery outcomes. Arthroscopy. 2005;21(5):562-9. [DOI] [PubMed] [Google Scholar]
- 7. Pihl K, Roos EM, Nissen N, JøRgensen U, Schjerning J, Thorlund JB. Over-optimistic patient expectations of recovery and leisure activities after arthroscopic meniscus surgery. Acta Orthop. 2016;87(6):615-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tilbury C, Haanstra TM, Leichtenberg CS, Verdegaal SH, Ostelo RW, de Vet HC. et al. Unfulfilled expectations after total hip and knee arthroplasty surgery: there is a need for better preoperative patient information and education. J Arthroplasty. 2016;31(10):2139-45. [DOI] [PubMed] [Google Scholar]
- 9. Shirley ED, Sanders JO. Patient satisfaction: implications and predictors of success. J Bone Joint Surg Am. 2013;95(10):e69. [DOI] [PubMed] [Google Scholar]
- 10. Anderson R, Barbara A, Feldman S. What patients want: a content analysis of key qualities that influence patient satisfaction. J Med Pract Manage. 2007;22(5):255-61. [PubMed] [Google Scholar]
- 11. Bagley CH, Hunter AR, Bacarese-Hamilton IA. Patients’ misunderstanding of common orthopaedic terminology: the need for clarity. Ann R Coll Surg Engl. 2011;93(5):401-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yin B, Goldsmith L, Gambardella R. Web-based education prior to knee arthroscopy enhances informed consent and patient knowledge recall: a prospective, randomized controlled study. J Bone Joint Surg Am. 2015;97(12):964-71. [DOI] [PubMed] [Google Scholar]
- 13. Greene KA, Harwin SF. Maximizing patient satisfaction and functional results after total knee arthroplasty. J Knee Surg. 2011;24(1):19-24. [DOI] [PubMed] [Google Scholar]
- 14. Rossi MJ, Guttmann D, MacLennan MJ, Lubowitz JH. Video informed consent improves knee arthroscopy patient comprehension. Arthroscopy. 2005;21(6):739-43. [DOI] [PubMed] [Google Scholar]
- 15. Koorevaar RCT, Haanstra T, Van’t Riet E, Lambers Heerspink OFO, Bulstra SK. The development of the Patient Expectations of Shoulder Surgery survey. J Shoulder Elbow Surg. 2017;26(10):1701-7. [DOI] [PubMed] [Google Scholar]
- 16. Cole BJ, Cotter EJ, Wang KC, Davey A. Patient understanding, expectations, and satisfaction regarding rotator cuff injuries and surgical management. Arthroscopy. 2017;33(8):1603-6. [DOI] [PubMed] [Google Scholar]
- 17. Cole BJ, Cotter EJ, Wang KC, Davey A. Patient understanding, expectations, outcomes, and satisfaction regarding anterior cruciate ligament injuries and surgical management. Arthroscopy. 2017;33(5):1092-6. [DOI] [PubMed] [Google Scholar]
- 18. Hudak PL, Wright JG. The characteristics of patient satisfaction measures. Spine (Phila Pa 1976). 2000;25(24):3167-77. [DOI] [PubMed] [Google Scholar]
- 19. Hageman MG, Briët JP, Bossen JK, Blok RD, Ring DC, Vranceanu AM. Do previsit expectations correlate with satisfaction of new patients presenting for evaluation with an orthopaedic surgical practice? Clin Orthop Relat Res. 2015;473(2):716-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ayers DC, Zheng H, Franklin PD. Integrating patient-reported outcomes into orthopaedic clinical practice: proof of concept from FORCE-TJR. Clin Orthop Relat Res. 2013;471(11):3419-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wright RW. Knee injury outcomes measures. J Am Acad Orthop Surg. 2009;17(1):31-9. [DOI] [PubMed] [Google Scholar]
- 22. Flanigan DC, Harris JD, Trinh TQ, Siston RA, Brophy RH. Prevalence of chondral defects in athletes’ knees: a systematic review. Med Sci Sports Exerc. 2010;42(10):1795-801. [DOI] [PubMed] [Google Scholar]
- 23. Waryasz GR, Gil JA, Chiou D, Ramos P, Schiller JR, DaSilva MF. Patient comprehension of carpal tunnel surgery: an investigation of health literacy. Hand (N Y). 2017;12(2):175-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Matava MJ, Howard DR, Polakof L, Brophy RH. Public perception regarding anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2014;96(10):e85. [DOI] [PubMed] [Google Scholar]
- 25. Makhni EC, Meadows M, Hamamoto JT, Higgins JD, Romeo AA, Verma NN. Patient Reported Outcomes Measurement Information System (PROMIS) in the upper extremity: the future of outcomes reporting? J Shoulder Elbow Surg. 2017;26(2):352-7. [DOI] [PubMed] [Google Scholar]
- 26. Makhni EC, Meyer MA, Saltzman BM, Cole BJ. Comprehensiveness of outcome reporting in studies of articular cartilage defects of the knee. Arthroscopy. 2016;32(10):2133-9. [DOI] [PubMed] [Google Scholar]
- 27. Pareek A, Reardon PJ, Maak TG, Levy BA, Stuart MJ, Krych AJ. Long-term outcomes after osteochondral autograft transfer: a systematic review at mean follow-up of 10.2 years. Arthroscopy. 2016;32(6):1174-84. [DOI] [PubMed] [Google Scholar]
- 28. Erggelet C, Vavken P. Microfracture for the treatment of cartilage defects in the knee joint—a golden standard? J Clin Orthop Trauma. 2016;7(3):145-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Emre TY, Ege T, Kose O, Demircioglu DT, Seyhan B, Uzun M. Factors affecting the outcome of osteochondral autografting (mosaicplasty) in articular cartilage defects of the knee joint: retrospective analysis of 152 cases. Arch Orthop Trauma Surg. 2013;133(4):531-6. [DOI] [PubMed] [Google Scholar]
- 30. Roos EM, Engelhart L, Ranstam J, Anderson AF, Irrgang JJ, Marx RG. et al. ICRS recommendation document: patient-reported outcome instruments for use in patients with articular cartilage defects. Cartilage. 2011;2(2):122-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Knutsen G, Drogset JO, Engebretsen L, Grøntvedt T, Isaksen V, Ludvigsen TC. et al. A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am. 2007;89(10):2105-12. [DOI] [PubMed] [Google Scholar]
- 32. Mithoefer K, Williams RJ, 3rd, Warren RF, Wickiewicz TL, Marx RG. High-impact athletics after knee articular cartilage repair: a prospective evaluation of the microfracture technique. Am J Sports Med. 2006;34(9):1413-8. [DOI] [PubMed] [Google Scholar]
- 33. Devitt BM, Bell SW, Webster KE, Feller JA, Whitehead TS. Surgical treatments of cartilage defects of the knee: systematic review of randomised controlled trials. Knee. 2017;24(3):508-17. [DOI] [PubMed] [Google Scholar]
- 34. Steadman JR, Hanson CM, Briggs KK, Matheny LM, James EW, Guillet A. Outcomes after knee microfracture of chondral defects in alpine ski racers. J Knee Surg. 2014;27(5):407-10. [DOI] [PubMed] [Google Scholar]
- 35. Chahal J, Gross AE, Gross C, Mall N, Dwyer T, Chahal A. et al. Outcomes of osteochondral allograft transplantation in the knee. Arthroscopy. 2013;29(3):575-88. [DOI] [PubMed] [Google Scholar]
- 36. Niemeyer P, Porichis S, Steinwachs M, Erggelet C, Kreuz PC, Schmal H. et al. Long-term outcomes after first-generation autologous chondrocyte implantation for cartilage defects of the knee. Am J Sports Med. 2014;42(1):150-7. [DOI] [PubMed] [Google Scholar]
- 37. Espregueira-Mendes J, Pereira H, Sevivas N, Varanda P, da Silva MV, Monteiro A. et al. Osteochondral transplantation using autografts from the upper tibio-fibular joint for the treatment of knee cartilage lesions. Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1136-42. [DOI] [PubMed] [Google Scholar]
- 38. Pestka JM, Bode G, Salzmann G, Südkamp NP, Niemeyer P. Clinical outcome of autologous chondrocyte implantation for failed microfracture treatment of full-thickness cartilage defects of the knee joint. Am J Sports Med. 2012;40(2):325-31. [DOI] [PubMed] [Google Scholar]
- 39. Gracitelli GC, Meric G, Briggs DT, Pulido PA, McCauley JC, Belloti JC. et al. Fresh osteochondral allografts in the knee: comparison of primary transplantation versus transplantation after failure of previous subchondral marrow stimulation. Am J Sports Med. 2015;43(4):885-91. [DOI] [PubMed] [Google Scholar]
- 40. Pascual-Garrido C, Slabaugh MA, L’Heureux DR, Friel NA, Cole BJ. Recommendations and treatment outcomes for patellofemoral articular cartilage defects with autologous chondrocyte implantation: prospective evaluation at average 4-year follow-up. Am J Sports Med. 2009;37(Suppl 1):33S-41S. [DOI] [PubMed] [Google Scholar]
- 41. Balain B, Kerin C, Kanes G, Roberts SN, Rees D, Kuiper JH. Effects of knee compartment, concomitant surgery and smoking on medium-term outcome of microfracture. Knee. 2012;19(4):440-4. [DOI] [PubMed] [Google Scholar]
- 42. Ebert JR, Smith A, Edwards PK, Hambly K, Wood DJ, Ackland TR. Factors predictive of outcome 5 years after matrix-induced autologous chondrocyte implantation in the tibiofemoral joint. Am J Sports Med. 2013;41(6):1245-54. [DOI] [PubMed] [Google Scholar]
- 43. Balain B, Ennis O, Kanes G, Singhal R, Roberts SN, Rees D. et al. Response shift in self-reported functional scores after knee microfracture for full thickness cartilage lesions. Osteoarthritis Cartilage. 2009;17(8):1009-13. [DOI] [PubMed] [Google Scholar]
- 44. Ebert JR, Smith A, Wood DJ, Ackland TR. A comparison of the responsiveness of 4 commonly used patient-reported outcome instruments at 5 years after matrix-induced autologous chondrocyte implantation. Am J Sports Med. 2013;41(12):2791-9. [DOI] [PubMed] [Google Scholar]
- 45. Badarudeen S, Sabharwal S. Assessing readability of patient education materials: current role in orthopaedics. Clin Orthop Relat Res. 2010;468(10):2572-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cassidy JT, Baker JF. Orthopaedic patient information on the World Wide Web: an essential review. J Bone Joint Surg Am. 2016;98(4):325-38. [DOI] [PubMed] [Google Scholar]
- 47. Brophy RH, Gefen AM, Matava MJ, Wright RW, Smith MV. Understanding of meniscus injury and expectations of meniscus surgery in patients presenting for orthopaedic care. Arthroscopy. 2015;31(12):2295-300.e5. [DOI] [PubMed] [Google Scholar]
- 48. Daniels AH, Leopold SS. Editor’s Spotlight/Take 5: Most American Academy of Orthopaedic Surgeons’ online patient education material exceeds average patient reading level. Clin Orthop Relat Res. 2015;473(4):1177-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Feghhi DP, Agarwal N, Hansberry DR, Berberian WS, Sabharwal S. Critical review of patient education materials from the American Academy of Orthopaedic Surgeons. Am J Orthop (Belle Mead NJ). 2014;43(8):E168-74. [PubMed] [Google Scholar]
- 50. Bayar A, Tuncay I, Atasoy N, Ayoğlu H, Keser S, Ege A. The effect of watching live arthroscopic views on postoperative anxiety of patients. Knee Surg Sports Traumatol Arthrosc. 2008;16(11):982-7. [DOI] [PubMed] [Google Scholar]