Abstract
Purpose
Best practices and guidance are provided for standardizing dosing instructions on prescription container labels of oral liquid medications by eliminating use of U.S. customary (household) units and adopting metric units universally, with the goal of decreasing the potential for error and improving safety and outcomes when patients and caregivers take and administer these medications.
Summary
Despite decades of best practice use of metric units in organized healthcare settings and advocacy by various professional societies, medication safety experts, and standards setting organizations, use of household units (e.g., teaspoon) on prescription container labeling instructions for oral liquid medications persists in community pharmacy settings. Five years after publication of the National Council for Prescription Drug Programs’ (NCPDP’s) original white paper advocating metric-only dosing, very few community pharmacy companies appear to require oral liquid dosing instructions be presented in metric-only units (mL). Error-prone dosing designations contribute to medication errors and patient harm. Use of both multiple volumetric units (e.g., teaspoonsful, tablespoonsful) and multiple abbreviations for the same volumetric units (e.g., mL, cc, mls; tsp, TSP, t) increases the likelihood of dosing errors. Opportunities for error exist with each administration of an oral liquid medication and, unless coordinated with dispensing of appropriate oral dosing devices and optimal counseling, can result in use of household utensils (e.g., uncalibrated teaspoons) or discordantly marked devices that can further exacerbate the risk of error. Since publication of NCPDP’s original white paper, new standards have been adopted governing official liquid volume representation, calibrated dosing devices, and e-prescribing software which support the elimination of non-metric units to reduce use of dosing practices that are error-prone. In each case, U.S. customary (household) units have been eliminated in official standards and certification requirements. Therefore, use of non-metric units for oral dosing of liquid medications no longer is an acceptable practice.
Conclusion
Key factors contributing to dosing errors with oral liquid medications include use of multiple volumetric units and abbreviations; failure to institute policies and procedures that eliminate the use of non-metric (e.g., household) units and universally adopt metric-only dosing instructions in all settings; failure to coordinate dosing instructions with dosing device markings, appropriate type (oral syringe versus cup), and optimal volumes (e.g., 1-, 5-, or 10-mL devices); failure to adequately counsel patients about appropriate measurement and administration of oral liquid medication doses; and use or error-prone practices such as missing leading zeros and elimination of trailing zeros in prescriptions and container labels. Adoption of this white paper’s recommendations will align dosing designations for oral liquid medications in all settings with current standards and attain universal metric-only practice.
Keywords: Administration, Oral, Comprehension, Drug Labeling/Standards, Electronic Prescribing, Medication Errors/Prevention & Control, Parents, Pediatricians, Pharmaceutical Solutions/Administration & Dosage, Pharmacists, Physicians, Primary Care, Practice Guidelines as Topic, Syringes/Standards, Weights and Measures
KEY POINTS.
Despite decades of best practice use of metric units in organized healthcare settings, use of household units on prescription container labeling instructions for oral liquids continues in community pharmacy settings.
Error-prone dosing designations contribute to medication errors and patient harm.
Best practices and guidance are provided for universal standardization of dosing instructions in metric units for oral liquid medications.
The purpose of this white papera is to provide recommendations and guidance for standardizing the dosing designation (the amount and volumetric units) used on prescription container labels of oral liquid medications dispensed from community pharmacies. The goal is to improve patient safety and outcomes by decreasing the potential for error when patients and caregivers take and administer these medications. To accomplish this, the white paper advocates harmonizing prescribing, transcribing, labeling, dispensing, and administering these medications in the community setting with the universal standard of metric dosing used in hospital and other healthcare settings, recommendations for over-the-counter (OTC) medications, and international standards of expressing volumetric measurement.
The audience for this white paper is all stakeholders who: dispense oral liquid prescription medication; review, revise, or generate prescription container labels; develop, produce, deploy, certify, or use pharmacy system software, prescribing software, or drug information content; design or manufacture oral liquid medication dosing devices; and/or educate healthcare professionals, patients, and caregivers on the appropriate use of oral liquid medications.
In September 2012, NCPDP hosted a stakeholder meeting involving 27 participants representing a wide range of perspectives to discuss the possibility of improving the standardization and consistency of dosing designations used on prescription container labels of oral liquid medications. This stakeholder meeting was catalyzed by the U.S. Centers for Disease Control and Prevention’s (CDC’s) PRevention of Overdoses and Treatment Errors in Children Taskforce (PROTECT) Initiative, a public-private partnership, which has as one of its objectives to reduce the likelihood of patient and caregiver errors by standardizing dose designations of oral liquid medications. Based on the success of NCPDP’s previous efforts to promote patient safety through improving prescription container labels, this effort was assigned to a task group of the NCPDP Professional Pharmacy Services Work Group (WG10).
Dosing errors involving oral liquid medications administered by patients and caregivers in home settings have been a source of concern for many years. Of particular concern are medication errors involving young children, as they may be more susceptible to harm from measurement errors and overdoses. To administer most oral liquid medications, patients and caregivers must rely on the container label dosing instructions to guide them in measuring out the proper dose with a dosing device. This additional step introduces numerous opportunities for error with each administration of an oral liquid medication and, unless coordinated with dispensing of appropriate (e.g., type, volume and unit markings) oral dosing devices and optimal counseling of patients and caregivers, can result in use of household utensils (e.g., uncalibrated teaspoons) or discordantly marked devices that can further exacerbate the risk of error.
Error-prone dosing designations contribute to medication errors and patient harm. The use of both multiple volumetric units (e.g., teaspoonsful, tablespoonsful, droppersful) and multiple abbreviations for the same volumetric units (e.g., mL, cc, mls; tsp, TSP, t) increases the likelihood of dosing errors by healthcare professionals, patients, and caregivers. One of the most common dosing errors is a patient or caregiver confusing teaspoons and tablespoons, resulting in three-fold dosing errors. In addition, the use of teaspoons and tablespoons as units of measure on labels may encourage the inappropriate use of non-calibrated household spoons for dosing medications.
Since publication of the original white paper, new standards have been adopted (e.g., from the United States Pharmacopeia [USP] and Office of the National Coordinator for Health Information Technology [ONC]) governing official liquid volume representation, oral liquid dosing devices, and e-prescribing software which support the elimination of non-metric units, including on calibrated dosing devices, to reduce the use of dosing practices that are error-prone. In each case, U.S. customary (household) units have been eliminated in official standards and certification requirements. Therefore, use of non-metric units for oral dosing of liquid medications no longer is an acceptable practice.
The omission of leading zeros for decimal amounts less than one and the use of unnecessary trailing zeros after whole number or decimal amounts can lead to potentially more serious ten-fold dosing errors by patients or caregivers. Further, assuming a patient or caregiver does use a calibrated dosing device, there is another opportunity for administration error if the numeric graduations and units of measure on the device do not correspond to the amounts and units of the container label dosing designation. Finally, the combination of multiple volumetric units and automation in some community pharmacy computer systems may facilitate dosing designation misinterpretations by healthcare professionals when translating a prescription to a dosing designation on a container label.
This white paper outlines a concise set of recommendations and guidance that can be applied to the practices, systems, and procedures for processing electronic prescriptions; printing prescription container labels; encouraging the use of appropriate dosing devices for oral liquid medications; and educating healthcare professionals, patients, and caregivers.
| NCPDP Recommendations for Standardizing the Dosing Designation on Prescription Container Labels for Oral Liquid Medications | |
|---|---|
| 1 |
Milliliter (mL) should be the universal standard unit of measure used on prescription container labels for oral liquid medications. e-Prescribing software must not permit prescriber override for U.S. customary (household) units (e.g., teaspoon). Pharmacy systems should only generate dosing instructions for oral liquids in metric units. |
| 2 | Dose amounts should always use leading zeros before the decimal point for amounts less than one and should not use trailing zeros after a decimal point on prescription container labels for oral liquid medications. |
| 3 |
Dosing devices with numeric graduations and mL units that correspond to the prescription container labeling should be made easily and universally available such as including a device each time oral liquid prescription medications are dispensed. Dosing devices should be of appropriate volume and graduated accuracy for the amount prescribed and should not use multiple units of measure (i.e., metric only, not metric plus household units). For volumes up to 10 mL, oral syringes generally are the preferred dosing devices. |
The NCPDP Task Group Call to Action maps out roles for many stakeholders, but particularly relies on local and corporate pharmacy leadership to:
Adopt the recommendations in this white paper.
Communicate these recommendations as standards of practice in policies to all pharmacy staff.
Measure the performance of your organization in achieving these recommendations and stress accountability across your organization for adhering to them.
Explore innovative patient-centered communication and education initiatives that encourage pharmacist-to-patient education at the point of dispensing.
Facilitate communication by stakeholders outside the community pharmacy system, including prescribers, with a role in patient and healthcare professional education on using standardized metric-only dosing designations and devices for prescribed oral liquid medications.
A stakeholder map identifies all the relevant stakeholders who need to play a role in adopting, communicating, adhering, and educating others regarding these best practice standards. The map outlines a call to action and identifies some of the challenges and opportunities for each stakeholder group.
Adoption of this white paper’s recommendations will standardize dosing designations for prescription container labels of oral liquid medications in the community setting with practice standards for metric dosing used in hospital and other healthcare facilities, recommendations for OTC medications, and international standards of volumetric measurement to attain universal metric-only standard practice.
NCPDP calls on all the relevant stakeholders to support efforts to adopt, implement, and adhere to the recommendations in this white paper, and to educate healthcare professionals, patients, and caregivers on how to accurately measure and administer oral liquid medications.
1. AUDIENCE
The audience for this white paper includes all stakeholders who:
Dispense oral liquid prescription medication
Review, revise, or generate prescription container labels
Develop, produce, deploy, use, or certify pharmacy system software
Develop, produce, deploy, use, or certify prescribing software
Develop, produce, deploy, or use drug information content
Design or manufacture oral drug dosing devices
Develop standards for prescription container labeling, official units of measure, and oral liquid dosing devices
Educate healthcare professionals, patients, and other caregivers on the appropriate administration of prescribed oral liquid medications
2. PURPOSE, GOALS, AND KEY RECOMMENDATIONS
The purpose of this white paper is to provide recommendations and guidance for standardizing dosing designation (the amount and volumetric units) used on prescription container labels of oral liquid medications dispensed from community pharmacies.
The immediate goals of the recommendations are to:
(1) Reduce variability in dosing designations on prescription container labels of oral liquid medications dispensed from community pharmacies by harmonizing the dosing designations with widely endorsed metric-only practice standards used in hospital and other healthcare facilities, recommendations for OTC medications, and international standards of volumetric measurement to attain universal metric-only standard practice.
(2) Facilitate proper administration by patients and caregivers of oral liquid medications dispensed from community pharmacies.
The ultimate goal of the recommendations is to improve patient safety and patient outcomes by decreasing the potential for overdoses, underdoses, and other errors when patients and caregivers measure and administer oral liquid prescription medications dispensed from community pharmacies.
To meet these goals, NCPDP outlines below a set of recommendations and guidance that can be applied to practices, systems, and procedures for processing prescriptions; printing of prescription container labels; encouraging the use of appropriate dosing devices for oral liquid medications; and educating healthcare professionals, patients, and caregivers.
| Recommendations | |
|---|---|
| 1 |
Milliliter (mL) should be the universal standard unit of measure used on prescription container labels of oral liquid medications. e-Prescribing software must not permit prescriber override for U.S. customary (household) units (e.g., teaspoon). Pharmacy systems should only generate dosing instructions for oral liquids in metric units. |
|
• Metric units should be adopted as the standard units of measure. Non-metric and non-volumetric units of measure should not be used. • When the prescription Sig (signatura) contains dosing designations in mL, mL dosing instructions should be used on the prescription container label. • When the prescription Sig contains dosing designations in non-metric (e.g., U.S. customary or household units such as teaspoonful) or non-standard (e.g., dropperful) units, convert to only volumetric metric units (mL) for dosing instructions on the prescription container label. • When the prescription Sig contains dosing instructions in non-volumetric units (e.g., mg), convert the dosing instructions to mL, and use only mL dosing instructions on the prescription container label. • When dispensing non-standardized concentrations of extemporaneously prepared formulations, it is critical that caregivers be instructed carefully about the volume to administer since it may differ from instructions they received with previous formulations of the oral liquid. They should be instructed to follow the current dosing instructions to avoid inadvertent underdosing or overdosing. • The standard abbreviation “mL” should be used on the prescription container label. Other abbreviations for milliliter (e.g., mls, cc) should not be used. If use of mixed case is not possible (e.g., because of legacy software limitations), lowercase (“ml”) or uppercase (“ML”) may be used while changes to the preferred “mL” are implemented. • Mnemonics, Sig codes, or any defaults used in computer systems to print prescription labels should produce dosing designations using mL. • e-Prescribing software should present prescribers with Sig options that apply metric volumetric units only and must not permit an option for prescribers to override metric with U.S. customary (household) units (e.g., teaspoon). |
|
| 2 |
Dose amounts should always use leading zeros before a decimal point for amounts less than one and should not use trailing zeros after a decimal point on prescription container labels of oral liquid medications. • The dose designation on a prescription container label should be “0.5” mL, NOT “.5” mL. • The dose designation on a prescription container label should be “5” mL, NOT “5.0” mL. Do not use trailing zeros in the hundredths, or thousandths position (e.g., “2.5” mL NOT “2.50” mL or “2.500” mL) either. • Place adequate space between the dose and unit of measure (e.g., “5 mL” NOT “5mL”). |
| 3 |
Dosing devices with numeric graduations and mL units that correspond to the prescription container labeling should be made easily and universally available such as including a device each time oral liquid prescription medications are dispensed. Dosing devices should be of appropriate volume and graduated accuracy for the amount prescribed and should not use multiple units of measure (i.e., metric only not metric plus household). For volumes up to 10 mL, oral syringes generally are the preferred dosing devices. |
| • The standard abbreviation “mL” should be used on the dosing device to correspond with the prescription container label. • Leading zeros before a decimal point should always be used on dosing devices and trailing zeros after a decimal point should never be used on dosing devices to correspond to the prescription container label. |
|
3. Background
Despite decades of best practice use of metric units in organized healthcare settings and advocacy by various professional societies (e.g., American Academy of Pediatrics [AAP], American Society of Health-System Pharmacists [ASHP]), medication safety experts (e.g., Institute for Safe Medication Practices [ISMP]), and standards setting organizations (e.g., USP, the Joint Commission [TJC]), use of household units (e.g., teaspoon) on prescription container labeling instructions for oral liquid medications persists in community pharmacy settings.
Five years after publication of its original white paper advocating metric-only dosing, an environmental scan completed by NCPDP in 2019 of 31 chain pharmacy companies representing over 35,000 community stores revealed that only 2 chains (out of 12 respondents) required oral liquid dosing instructions be presented in metric-only units (mL). While nearly half of responding chains indicated they recommended conversion to mL as a preferred practice, there remained a reluctance to require such conversion as pharmacy policy. Instead, it often was left to each individual pharmacist’s judgment to decide whether to use household or metric units in the prescription dosing instructions.
Most chains did report a policy to provide an appropriate oral dosing device (e.g., oral syringe) with each prescription dispensed, and to counsel the parent or caregiver on its proper use. Few reported using pharmacy information system software to automatically default to mL dosing, and none reported implementing a staff performance measure on adoption of metric-only dosing instructions as a best practice.
Thus, there remains an ongoing need for broad-based adoption of recommended best practices for oral liquid dosing instructions. As this latest revision of NCPDP’s white paper on standardized dosing designations for oral liquid medications details, substantial evidence and national standards and policy have accumulated in further support of universal adoption of metric-only dosing in community pharmacies.
3.1 Why an NCPDP White Paper?
In September 2012, NCPDP hosted a stakeholder meeting involving 27 participants representing a wide range of perspectivesb to discuss the possibility of improving the standardization and consistency of dosing designations (i.e., the amount to be given and the unit of measure to use) on prescription container labels of oral liquid medications. This stakeholder meeting was catalyzed by the PROTECT Initiative,1 a public-private partnership led by CDC, which seeks to reduce the likelihood of pediatric medication overdoses and errors by healthcare professionals, patients, and caregivers.
NCPDP has previously played a key role in efforts to clarify information on the labels of prescription drugs. An NCPDP white paper on improving prescription container labels for medications containing acetaminophen2 has, along with subsequent implementation efforts by partner organizations, helped lead to the use of “acetaminophen” instead of the more confusing acronym “APAP” on the labels of hundreds of prescription products. NCPDP also has led the way in promoting a universal medication schedule (UMS) for use on prescription medication labels, with a white paper recommending the removal of arcane notations, such as BID, or confusing instructions, such as “take 1 tablet twice daily,” and substituting plain language, explicit instructions, such as “take 1 pill in the morning and take 1 pill in the evening.” 3
Based on the success of these previous NCPDP efforts to promote patient safety through improving prescription container labels, NCPDP determined that best practices also could be developed to decrease the variability of dosing designations used for oral liquid medications. This effort was assigned to a task group of the NCPDP Professional Pharmacy Services Work Group (WG10), which published NCPDP Recommendations and Guidance for Standardizing the Dosing Designations on Prescription Container Labels of Oral Liquid Medications in 2014.
Since 2014, professional organizations, safety organizations, standards setting organizations, and federal health agencies have issued additional recommendations supporting standardization of dosing designations, and new research has provided further best practice guidance on the role of dosing designations and appropriately designed devices for oral liquid medication administration accuracy.4 Therefore, the NCPDP Professional Pharmacy Services Work Group (WG10) reconvened a task group to provide updated recommendations.
3.2 Standardizing Dosing Designations on Prescription Container Labels of Oral Liquid Medications
While healthcare professionals usually measure and administer medications within healthcare facilities, it is up to patients or caregivers to accurately measure and administer liquid medications outside of these settings. When patients or caregivers administer oral liquid medications, the dosing designations on the medication container labels and consistency with accompanying dosing devices are particularly important because container labels often provide the only instructions they use when administering medications.
For many decades, ASHP and other practice organizations (e.g., American Health Care Association [AHCA], American Pharmacists Association [APhA]) have recommended the use of metric units and metrically marked dosing devices for the measurement and administration of oral liquid medications in healthcare settings.5-9 Confusion and resultant medication errors (e.g., unit conversions) from multiple systems of measure was the principal rationale for the recommended use of metric units in the healthcare setting. In fact, in some studies, most dosing errors were associated with administration of wrong doses of liquid medications.
TJC also has required the healthcare settings it accredits to standardize dosing designations in order to reduce medication administration errors.10-11 Other organizations, including ISMP12-18 and the National Coordinating Council for Medication Error Reporting and Prevention (NCC-MERP)9,19 have supported using the same or similar recommendations in all healthcare settings.
Beginning in 2011, a series of initiatives have focused on reducing medication administration errors outside of healthcare facilities, when OTC oral liquid medications are used. A Consumer Healthcare Products Association (CHPA) guideline20-21 and U.S. Food and Drug Administration (FDA) guidances for industry22-24 have provided recommendations for standardization and consistency in medication dosing designations for OTC product labels and dosing devices and recommended dosing devices be included with every liquid OTC product.
A recent study of the most commonly used pediatric OTC liquid medications demonstrated that just 2 years after these voluntary standards were finalized, 91% of dosing directions and 62% of dosing devices adhered to all top-tier recommendations, suggesting that voluntary initiatives can promote adherence to safety recommendations.25 Universal adoption rates are the goal for prescription oral liquid medications.
3.3 Efforts to Move from Standardized Dosing Designations to Metric-only Dosing Designations
3.3.1 Commercial container labels
In 2013, FDA released a draft guidance for industry on safety considerations for commercial container labels and carton labeling design to minimize medication errors.26 This guidance includes details for standardization and consistency of dosing designations for commercial containers and carton labeling of prescription drug and biological products. It states the dose should appear in metric units of measure rather than apothecary or U.S. customary (household) measurements (e.g., teaspoon or tablespoon), but does not specifically address those containers or cartons dispensed from community pharmacies.26 In 2015, the AAP Committee on Drugs recommended pharmaceutical manufacturers eliminate labeling dosing instructions and dosing devices that contain units other than metric.27 Similarly, official actions by USP28-30 and guidance from CHPA20,21 have directed or recommended manufacturers eliminate non-metric dosing, labeling, and administration devices.
While some medications are dispensed from community pharmacies in the original carton or container, many, if not most, are dispensed from community pharmacies in other containers filled by the pharmacy. In addition, even when medications are dispensed in the original container or carton, labels created in the community pharmacy with dosing directions that are ordered for the specific patient are added and may differ in units of measure and other dosing instructions as well as with markings on any accompanying dosing device provided by the manufacturer.
3.3.2 Over-the-counter products
In 2014, CHPA updated their OTC product guidance to clarify that standardized dosing directions should specifically use milliliter (mL) as the only unit of measure in the dosing directions and the included standardized dosing device should use mL as the only unit of measure.21
To address the specific problem of liver toxicity from acetaminophen dosing errors, in 2015, FDA released a guidance for industry for OTC pediatric oral liquid drug products containing acetaminophen which recommends the dosing directions in the Drug Facts label should be provided only in mL.31
3.3.3 Electronic health records (EHR)/e-prescribing
Because more and more community prescriptions are ordered by electronic transmission of prescriptions from the prescriber to the community pharmacy (e-prescribing), in 2013, AAP issued a policy statement outlining safe practices for e-prescribing which recommended using metric-only label instructions for medication dosing designations transmitted to community pharmacies.32 AAP further recommended in 2015 that electronic health record (EHR) vendors use metric units for orally administered liquid medications and eliminate the option of prescribers to order using non-mL-based dosing regimens.27
In 2015, ONC issued the 2015 Edition Health Information Technology (Health IT) Certification Criteria.33 These certification criteria are required to determine EHR eligibility under Medicare EHR Incentive Programs. ONC added a certification criterion that limits the user’s ability to prescribe oral liquid medication to only metric standard units of mL (Charles D, Office of the National Coordinator for Health Information Technology, personal communication; July 2, 2020).33 Further, ONC clarified that this criterion requires prescribers must only be presented with Sig options for oral liquid medications that apply metric units and must preclude prescriber override that would apply U.S. customary (household) units instead (Charles D, Office of the National Coordinator for Health Information Technology, personal communication; July 2, 2020). In addition, this criterion would preclude the substitution of cc for mL.33 Thus, along with federal partners (including FDA and CDC), ONC now encourages pharmacies to ensure prescription container labels maintain the metric standard for dosing instructions (Charles D, Office of the National Coordinator for Health Information Technology, personal communication; July 2, 2020).33
In 2018, ASHP recommended the U.S. healthcare system adopt and only use the International System of Units (SI units), which would apply metric (e.g., mL) dosing units, for all patient- and medication-related measurements and calculations, and healthcare organizations use clinical decision support systems, equipment, and devices that allow input and display of patient- and medication-related measurements and calculations in SI format only.34 Further, ASHP recommended health information technology vendors use only SI units in their product designs for patient- and medication-related measurements and education in the use of SI units and the importance of using SI units to prevent medical errors be promoted.34
In 2019, the American Medical Association (AMA) updated their policy on e-prescribing to now encourage healthcare stakeholders to improve their electronic prescribing practices in meaningful ways that will increase patient safety, reduce medication errors, improve quality care, and reduce administrative burden associated with e-prescribing processes and requirements.35 AMA recommended prioritized adoption of features like structured and codified Sig that help address quality issues and that e-prescribing be designated as the default prescription method.35 As a result, AMA supports sending mL-only as the volume value in e-prescriptions for oral liquids and eliminating non-metric units like teaspoon and tablespoon.35-36
3.3.4 Pediatric prescribing
In 2015, the AAP Committee on Drugs expanded their 2013 recommendation beyond e-prescribing and devoted an entire Academy policy statement to designate metric units as the exclusive dosing unit for all orally administered liquid medications.27 Whether prescriptions are transmitted electronically or not, AAP now recommends oral liquid medications should be dosed exclusively using metric-based dosing with mL to avoid confusion and dosing errors associated with common household spoons.27 The AAP policy statement also recommends pediatricians review mL-based dosing with patients and families to ensure adequate health literacy for metric dosing units; pharmacies, hospitals, and health centers should distribute dosing devices, preferably oral syringes, with all orally administered liquid medications; and devices should not be substantially larger than the recommended dose to reduce the risk of multi-fold overdose.27
The American Academy of Family Physicians (AAFP) also recommends oral dosing of liquid medications be standardized using mL to avoid unintended dosing errors in children.37
As early as 1975, AAP was warning about the inaccuracies and inconsistent volumes that were being administered when teaspoons, particularly household spoons, were being used to deliver oral liquid medication doses.38 AAP acknowledged while pediatricians took great care in accurately calculating medication doses for their patients, they often overlooked the important processes of accurately measuring and administering the doses by parents and caregivers.38 They further acknowledged the advantages gained by using liquid products in children were often lost because of the inaccuracy of the devices used to measure the doses.38 One important innovation AAP acknowledged at the time was the advent of oral syringes as a more precise alternative to measuring spoons and cups, lamenting however that the syringes principally were available only in hospitals and not for widespread use in the home.27,38 As described later, oral syringes now are widely available for home use and are the preferred dosing devices with oral liquid medications.
3.4 Application to Community Pharmacy Practice
This white paper seeks to align recommendations for portraying dosing designations on the prescription container label of oral liquid medications dispensed from community pharmacies with existing universal standards for inpatient pharmacy settings, for OTC medications, for commercial container and carton labeling, for e-prescribing, and with the latest evidence from medication safety research.
4. RATIONALE FOR KEY RECOMMENDATIONS: 4.1 Recommendation 1:
Milliliter (mL) should be the universal standard unit of measure used on prescription container labels of oral liquid medications. e-Prescribing software must not permit prescriber override for U.S. customary (household) units (e.g., teaspoon). Pharmacy systems should only generate dosing instructions for oral liquids in metric units.
4.1.1 The need to measure oral liquid medication volumes makes accurate use more challenging than for solid medications
Using oral liquid prescription medications is more complicated than using solid medication dosage forms.27,38,39 Unlike oral solid dosage forms, most liquid medications generally are not packaged in unit-of-use containers or dosing units. Oral liquid medications typically must be measured by a patient or caregiver at every administration. This additional step requires further manipulation of the product and introduces opportunities for error.27,38-41
Healthcare professionals often rely on liquid formulations when prescribing medications for young children.27,32,38 Because of their small body mass, young children may be more susceptible to harm from measurement errors leading to overdoses and underdoses.27,39,42 In any given week in the U.S., over half of children younger than 12 years of age receive at least one medication, including 20% taking at least one prescription medication.42 This high rate of medication use in children indicates the importance of addressing the issue of dosing errors, including caregiver medication administration errors.
There also is some evidence that Hispanic parents may be more likely to perform dosing errors with oral liquid medications, particularly those with limited health literacy and/or limited English proficiency.41 However, despite such challenges, parents generally perform better with metric-only dosing devices, particularly with oral syringes compared with cups, and promoting the use of oral syringes (especially for smaller doses) is recommended as part of a comprehensive pediatric labeling and dosing strategy aimed at reducing medication errors in children.27,43
4.1.2 The use of multiple volumetric measures contributes to oral liquid medication dosing errors
While essentially all solid dosage form medications have been measured in metric units (e.g., mg for milligrams) for decades, dosing designations for oral liquid medications still use, and patients and caregivers are still instructed to administer medications using, a variety of U.S. customary (household) units (teaspoons, tablespoons), non-standard units (droppersful), apothecary units (drams), other non-metric units (e.g., ounces), and metric units (mL).13-16,22,44-46 The use of non-standard metric abbreviations or terminology unfamiliar to parents and other caregivers, such as cubic centimeters (cc), creates an additional potential source of confusion. Patients and caregivers can be further confused when provided oral dosing devices bearing markings that are inconsistent with the labeled dosage instructions.22 Such confusion in oral liquid medication dose measurements and instructions can lead to potentially fatal medication dosing errors, particularly when converting from one unit of measure to another (e.g., from household to metric units, from mg to mL).15-16,24,26,39,47,48
Because of the long-standing traditional use of customary (household) units (e.g., teaspoons) to express doses of oral liquid medications in community settings, healthcare practitioners have been conditioned to anticipate dosing instructions to be expressed in teaspoons or occasionally tablespoons.13 As a result, a prescriber may unintentionally write a prescription in teaspoons when a number of mL was intended or a pharmacist or pharmacy technician may accidentally input prescription container label instructions in teaspoons when mL was intended.13
The use of multiple volumetric measures increases the likelihood of multifold dosing errors by patients, caregivers, and healthcare professionals.22 For example, a hurried prescriber or pharmacist who switches mL and teaspoon may mistakenly prescribe or dispense a five-fold overdose or underdose. A caregiver who confuses teaspoon and tablespoon can accidentally administer a three-fold overdose or underdose.
During pharmacy dispensing, numerous cases have been reported of errors involving multiple volumetric measures, most frequently due to a prescriber’s order being changed from an mL dose to a teaspoon dose.13,49 The design of some community pharmacy computer systems may facilitate confusion involving multiple volumetric measures.13 For efficiency, some pharmacy computer systems may default to a dose expressed in teaspoon amounts in the directions when oral liquids are selected.13 (Some prescribing systems may default to teaspoons as well.)13 If this happens when an mL dose is intended, pharmacists and pharmacy technicians may not remember to change the instructions for the container label back to mL when teaspoons automatically appear.13 Distractions and confirmation bias will most likely contribute to pharmacy personnel and prescribers forgetting to change the dosing designations from these error-prone default settings.13 Such mix-ups can result in either underdoses or overdoses, which often are serious and can be fatal.13
Sometimes these errors occur when community pharmacy staff believe it is helpful to “translate” prescription liquid dosing instructions for patients from metric (e.g., mL) to household measures (e.g., teaspoon). For example, when the pharmacy receives a prescription with dosing in mL, staff may intentionally change it to teaspoon dosing or list both teaspoonful and mL (in parentheses) on the pharmacy label, believing most patients and caregivers are more familiar with household measures than metric dosing. However, adding such conversions between units increases the likelihood of a dispensing error. Also, as more oral dosing devices display an mL scale exclusively, providing dosing instructions in teaspoons, or listing both teaspoons and mL on labels, will cease to be helpful to patients and will instead lead to mismatches between dosing instructions and dosing devices, contributing to home medication administration errors.27,50
When oral liquid medications are administered in home settings, volumetric measure confusion by parents and other caregivers has been a source of concern for ISMP, FDA, and other safe medication use experts for many years.13-17,22,24,26-27,32,38-43,45,51 From 2008 through 2014, an average of 7,900 calls were made each year to U.S. poison control centers because of confusion around units of measurement when giving medicine to children 12 years of age or younger. Since 2014, however, both the number of calls because of unit confusion and the proportion of all calls for therapeutic errors due to unit confusion have declined. By 2018, the number of calls because of confusion around units of measurement declined to 5,500 calls involving medicine given to children 12 years of age or younger.52-63 Volumetric dosing errors and use of incorrect dosing delivery devices are common sources of preventable medication errors in children,15-16,27,39 particularly in children 5 years of age or younger.52-63 Errors attributed to confusion around units of measure have been associated with sometimes severe adverse events in young children.15-16,39,64
ISMP has reported over 50 cases, sometimes serious, in which confusion with units of measure has led to errors, primarily attributed to transcription/dispensing errors.13-16,51,65
Example: A pharmacist accidentally put on a child’s prescription container label that the child should be given 3.5 teaspoons of an antibiotic instead of the 3.5 mL that the doctor had ordered, resulting in administration of a 5-fold overdose for 3 days.13,51
Example: A pharmacist typed out instructions on the prescription container label as “take 4 cc (4/5 teaspoon) three times a day.” The parents of the child did not understand the term “cc” and mistook the slash mark to mean 4.5 teaspoons. The child was given 4.5 teaspoons three times daily, almost five times more than intended.65
4.1.3 Parents measure liquids more accurately using mL
Although prescribers and pharmacists may assume parents and other caregivers are uncomfortable dosing with mL, and have difficulty administering liquid medications accurately using mL, several recent studies indicate these are highly likely to be false assumptions.27,43,66-68 To the contrary, there is evidence parents are in fact less likely to make dosing errors using mL-only dosing compared with teaspoon- or tablespoon-based dosing.27,43,66-68 In addition, these studies have shown more precise dosing can be achieved with oral syringes than with dosing cups or spoons27,67,69-71 and, when faced with prescription container labeling instructions that are in teaspoons or tsp, parents are more likely to choose inaccurate uncalibrated spoons.40
One study of parents whose children were prescribed liquid medications in the emergency department setting found that parents who reported their dose in mL were not only more likely to use a standardized dosing device over a household spoon, but also had half the odds of making a dosing error.69 In another study where parents were randomly assigned to receive labels and dosing devices with ‘mL’-only or both ‘mL’ and ‘tsp’ units, parents who had ‘mL’-only labels and dosing devices had less than half the odds of making a two-fold dosing error compared with those who used labels and devices that included both units.67
While there has been limited study of parent experiences and perceptions of mL-only dosing, a recent study of parents seen in 3 urban pediatric clinics (where over two-thirds of parents had limited health literacy) found over 80% had prior mL-dosing experience, and over 80% perceived mL-only dosing to be easy.68
4.1.4 Milliliter (mL) has been endorsed as the standard unit of measure for oral liquid medications by many professional and patient safety organizations
TJC has required the healthcare settings it accredits (e.g., hospitals, long-term care facilities, rehabilitation centers, ambulatory clinics) to standardize dosing designations in order to reduce medication administration errors and has suggested organizations avoid apothecary units (e.g., dram), using metric units instead, and also avoid non-standard abbreviations (e.g., do not use cc; mL is preferred).10,11 Based on reports of errors and patient harm, ISMP,13-14,17,48 NCC-MERP,9 and ASHP6-9,11,47 have issued or endorsed recommendations to only use metric units (mL) in all settings. Other patient safety, professional, and standards setting organizations that have endorsed recommendations to use only metric units in all clinical settings include APhA,6,72 AAP,27,32 AAFP,37 AMA,35,72 and ONC (Charles D, Office of the National Coordinator for Health Information Technology, personal communication; July 2, 2020).33 (eAppendix A)
USP adopted the use of metric units as a standard almost 40 years ago.c USP has published standards stating prescriptions for medications should be written to state the quantity and/or strength of the medication in metric units unless otherwise indicated in an individual monograph.73 USP also states if an amount of a medication is prescribed by any other system of measure, only the metric equivalent amount should be dispensed and labeled accordingly.73
In April 2010, USP deleted its General Chapter <1221> on the teaspoon, which defined the volumetric unit of measure for teaspoon based on the American Standard Teaspoon to be regarded as representing 5 mL; this chapter deletion eliminated teaspoon as an official alternative to metric units in dosing.74,75 Even when the teaspoon was a recognized unit of measure by USP, it warned about the risks of inaccurate measurement associated with household units and advised a household spoon was not an acceptable alternative to a calibrated teaspoon.74,75
The most recent update to USP General Chapter <659>, which became effective in May 2019, removed teaspoon as an official unit of measure as a component of drug packaging.28-29,75 One important consequence of this latter retirement of official status for the teaspoon as a unit of measure is that pharmaceutical manufacturers must now adopt mL and eliminate teaspoon in packaging and accompanying manufacturer-provided dosing devices (defined by USP as an “associated packaging component”).28-29,75
ONC also recently addressed safety issues associated with non-metric dosing of oral liquid medications (Charles D, Office of the National Coordinator for Health Information Technology, personal communication; July 2, 2020).33 The ONC EHR certification now requires e-prescribing software present Sig options to prescribers that apply metric units (e.g., mL) only and must not permit prescriber override to use household units (e.g., teaspoon) instead (Charles D, Office of the National Coordinator for Health Information Technology, personal communication; July 2, 2020).33 This change was implemented to support more precise prescription dosing and thus reduce dosing errors and improve patient outcomes and aligns with other federal partners (including FDA and CDC).33
ISMP recommends all electronic communication of medication information (e.g., EHR, e-prescribing) use metric-only units and USP abbreviations (e.g., mL; never cc or pluralized forms like mLs) and never use apothecary units or abbreviations (e.g., drams, minims, ounces) or household units (e.g., teaspoons, tablespoons).48 AMA also recommends against the use of apothecary units and symbols.76
4.1.5 Community pharmacy practices may decrease use of milliliter units
Unfortunately, changes made in the volumetric units during community pharmacy dispensing may decrease the use of mL on the prescription container labeling. In a study of liquid medications dispensed to children 12 years of age or younger from 4 community pharmacies, the vast majority (68%) of instructions were prescribed using mL, while only 24% were prescribed using teaspoon and 7% using other units (e.g., mg, cc, “dose”).45 When the corresponding container labels were examined, 62% used mL and 29% used teaspoon, suggesting that at least 5% of prescriptions were switched from mL to teaspoons.45 Overall, 25% of dispensed pharmacy labels differed from the prescribed unit instructions.45
In a second study involving liquid medications prescribed to children 8 years of age or younger in the emergency department and filled in community pharmacies, over a third of the labels did not include the same units as the prescription.66 Of prescriptions written in mL-only, 42% of pharmacy-generated labels matched the prescription and provided instructions in mL-only, whereas 50% of pharmacy-generated labels translated the instructions into teaspoon only and the remainder provided both mL and teaspoon units.66 Parents who used teaspoon or tablespoon dosing had twice the odds of a dosing error compared with those who used mL dosing.66
4.2 Recommendation 2:
Dose amounts should always use leading zeros before a decimal point and should not use trailing zeros after a decimal point on prescription container labels of oral liquid medication.
4.2.1 How amounts are expressed can cause significant overdoses
Error-prone methods of expressing doses have contributed to medication errors and patient harm.7-8,11-12,22-24,26-27,77,78 The inclusion of a decimal point and trailing zero for whole number doses (e.g., 5.0 instead of 5) and the failure to include a zero before the decimal point for doses less than a whole unit (e.g., .5 instead of 0.5) have resulted in 10-fold dosing errors. Such errors can be fatal.12,73,79
Example: A 9-month-old girl tragically died following a 10-fold overdose of morphine. The baby’s physician wrote an order, without the use of a leading zero, for morphine “.5 mg.” However, the decimal point was missed, and the order misinterpreted. Two 5-mg doses were administered to the baby.80
4.2.2 Existing healthcare standards recommend dose designations always use leading zeros and never use trailing zeros
TJC’s Information Management Standard IM.02.02.01 requires accredited organizations to adhere to TJC’s official “Do Not Use” list.10-11,45 This list dictates that when the amount of medication is a whole number, the amount should never be designated with a trailing zero (e.g., express as 5 not 5.0).10-11,65 If the amount of medication is less than 1, the amount should always include a leading zero (e.g., express as 0.5 not .5).10-11,65 USP has published similar standards when expressing the active ingredients of drug products.81
In addition, ISMP, FDA, ASHP, NCC-MERP, APhA, AAP, USP, ONC, American College of Obstetricians and Gynecologists (ACOG), World Health Organization (WHO), and others (eAppendix B) have issued statements or endorsed recommendations to use leading zeros and eliminate trailing zeros in dose designations in all settings.9-10,12,19,22,26-27,33,48,77,82-84 The adage “always lead, never follow” has been suggested to help recall this recommendation in mitigating errors.77
4.3 Recommendation 3:
Dosing devices with numeric graduations and mL units that correspond to the prescription container labeling should be made easily and universally available such as including a device each time oral liquid prescription medications are dispensed. Dosing devices should be of appropriate volume and graduated accuracy for the amount prescribed and should not use multiple units of measure (i.e., metric only not metric plus household units). For volumes up to 10 mL, oral syringes generally are the preferred dosing devices.
4.3.1 How dosing designations are represented on dosing devices contributes to medication administration errors
Non-metric units of measure presented, alone or in combination, on dosing devices have contributed to medication errors. Inclusion of units such as drams, minims, fluid ounces, cc, TSP (teaspoon), TBSP (tablespoon), and DSSP (dessertspoon) has caused mistakes when healthcare professionals, patients, and caregivers confuse the unit of measure on a measuring device with the unit of measure specified on a prescription container label or other set of instructions.22,24,26,85-87
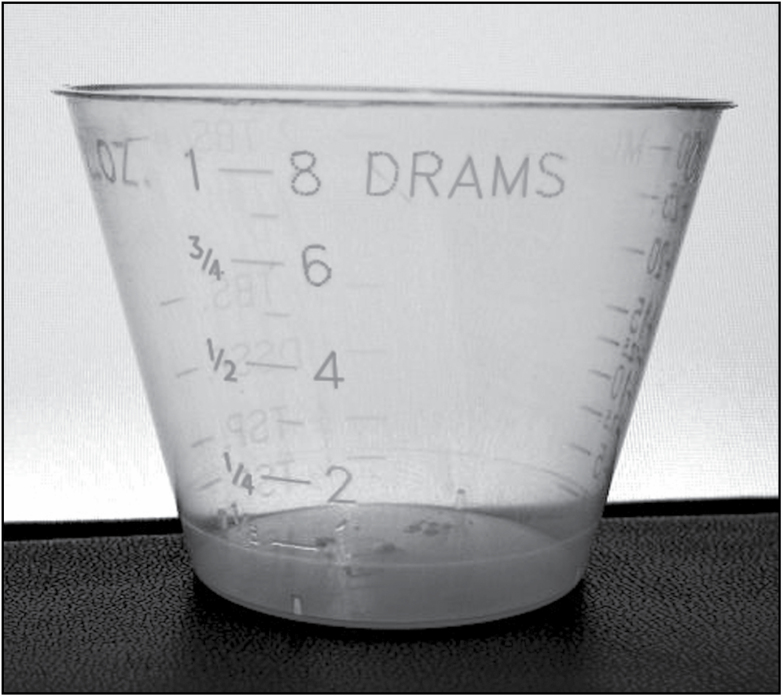
Example: A nurse administered five drams of acetaminophen concentrate liquid (100 mg/mL) instead of 5 mL because of inclusion of multiple units of measure on the dosing cup (Figure 1). As a result, the patient received 18.45 mL or 1.845 g of acetaminophen, almost four times the intended amount.85
Example: The aunt of a 7-month-old child unintentionally gave her nephew a 5-fold overdose of flecainide. She used an oral syringe that had both a teaspoon and mL scale to measure the dose and measured one teaspoon (5 mL) instead of 1 mL. The child was hospitalized and suffered a cardiac arrest but was successfully resuscitated.86
Figure 1.
Dose cup used to measure liquid acetaminophen (Image courtesy of ISMP).
4.3.2 Use of household spoons or other utensils can cause administration errors
Household teaspoons and tablespoons have proven to be inaccurate and error-prone when used by patients and caregivers as medication measuring tools since volumes in these household devices are not standardized.21-22,27,38-39,75-76,87 Although some kitchen cooking and measuring sets include a volumetric measure along with the household measure, these too cannot be relied on to provide accurate dosing, and calibrated oral dosing devices were preferred even when teaspoon was recognized.74,75
In addition, the use of teaspoons or tablespoons in dosing designations on prescription container labels may encourage patients and caregivers to believe that using household spoons or other kitchen utensils is advisable if a pharmacy-provided dosing device is not available.75,76,87 A recent study found when “tsp” units were used on the label, parents had a 3-fold increased odds of choosing a kitchen spoon for dosing compared with parents who had only “mL” units on the label; when “teaspoon” was spelled out on the label, parents had a 5-fold increased odds of choosing a kitchen spoon.40 Dispensing dosing devices with numeric graduations and units (mL) that correspond with the container labeling can reinforce use of a calibrated dosing device rather than household spoons or kitchen utensils.28-29,48,74,75,87
Patients should be encouraged to contact their healthcare professional (e.g., pharmacist) rather than substituting an alternative tool on their own when they are unsure about the best dosing device to use such as when they have misplaced the device they received with the prescription.74,75 Notably, caregiver access to dosing devices in the home appears to be high. In a recent multisite study in 3 urban pediatric clinics serving low income families, the vast majority of caregivers had access to standardized dosing devices in their homes, including dosing cups (≈85%) and oral syringes (≈90%). These may have been used with previously obtained medications and collected over time.
It may not be appropriate or optimal to use dosing devices left over from prior medications as these tools may only include markings specific to the dosing instructions for a specific medication for which it came (e.g., OTC medications), or may have been uniquely calibrated to account for medication-specific properties (e.g., viscosity and surface-tension of medication).28-29,74,75 In fact because of such variations even with medicine cups, USP has recommended a calibrated oral syringe or dropper be used when accurate dosage is required.74,75
4.3.3 Caregivers, even low health literacy caregivers, do dose accurately with ml-only devices, although characteristics of device provided also play an important role
Studies have found parents are able to dose accurately when given mL-only instructions with mL-only dosing devices.27,43,67 In an experimental study, parents who were randomly assigned to receive ‘mL’-only labels and devices had less than half the odds of making a two-fold dosing error compared with those who used labels and devices that included both ‘mL’ and ‘tsp’ units; caregivers across health literacy levels benefited from having ‘mL’-only labels and dosing devices.67
Provision of dosing devices that more closely match recommended dose volumes is important for reducing dosing errors.67,71 Dosing devices provided should be large enough to measure the full recommended dose (should not require multiple measurements for a single dose), but should not be too large:
For a 2-mL dose, for example, provision of a 5-mL oral syringe would be more optimal than a 10-mL syringe. In a recent study, a 0.3-fold reduction in odds of error was observed when a 5-mL capacity syringe rather than a 10-mL capacity syringe was used.
For a 7.5-mL dose, a 10-mL capacity syringe would be more optimal than a 5-mL syringe. In a recent study, parents using a 5-mL capacity syringe to dose a 7.5-mL volume had a 4-fold increase in odds of a dosing error compared with parents who used a 10-mL capacity syringe.67
Optimizing the capacity of dosing device provided to the dose volume is beneficial to caregivers across health literacy levels, but especially helpful for those with lower marginal health literacy.27,43,67,71,88
4.3.4 Guidelines for over-the-counter (OTC) medications already recommend milliliter (ml) should be the standard unit of measure used for oral liquid medication dosing devices
Guidelines from CHPA and FDA in 2011 recommended dosing devices should always accompany OTC oral liquid medications, and these devices should include the units and numeric doses as described in the dosing directions.20,22 In addition, the units of liquid measure marked on the dosing device should be stated consistently in all labeling, accompanying written instructions, packaging (e.g., outside carton), and containers (e.g., bottle). CHPA subsequently strengthened their recommendations to now specify that mL should be the only volumetric unit of measure in dosing directions.21
To address the specific problem of liver toxicity from acetaminophen dosing errors, the 2015 FDA guidance for industry on OTC pediatric oral liquid drug products containing acetaminophen recommends the product package should include an appropriate dosage delivery device with calibrated units of liquid measurement expressed in mL only.31 FDA also has recommended in other guidance that dosages of all other liquid medications should be in metric only.24,26
Recent retirement of an official definition of a teaspoon by USP and their retirement of teaspoon calibration in dosing devices included as commercial packaging components will result in the need for any existing non-metric oral dosing devices included in the packaging of a drug product to be replaced with metric devices by manufacturers.28-29,74,75
4.3.5 Guidelines extend the recommendation milliliter (ml) should be the standard unit of measure used for oral liquid medication dosing devices to prescription oral liquid medications
In 2016, FDA clarified the principles outlined in its 2011 guidance for industry for OTC products generally are applicable to orally ingested prescription liquid products as well.24 Specifically, dosing amounts of prescription liquid products, as well as OTC products, should be able to be measured with a standard dosing device, and dosing devices should utilize metric volumetric units.24 And in May 2019, USP strengthened its standards for oral liquid dosing devices (“associated components”) to require the volumetric markings should only be in metric units and limited to a single measurement scale that corresponds to the dosing instructions on the OTC or prescription container product.28
Healthcare professional organizations also recommend standardized dosing devices be included with all liquid medications to allow parents and other caregivers to measure liquid medications in mL and patients and caregivers be effectively instructed on how to properly measure and administer oral liquid medications.15,27,47,72,81
In 2014, ISMP introduced its Targeted Medication Safety Best Practices for Hospitals which included a recommendation to purchase dosing devices that only display the metric scale and, if patients are taking an oral liquid medication after discharge, supply them with oral syringes to enable them to measure oral liquid volumes in mL.15 This recommendation remains present in the ISMP 2020–2021 Targeted Medication Safety Best Practices for Hospitals.16 (If an enteral syringe is provided instead, the pharmacy should ensure it meets the International Organization for Standardization [ISO] 80369 standard, such as ENfit, in order to help reduce the risk of cross connections to non-enteral tubing.)16
The 2015 AAP policy designating metric units as the preferred measure for dosing oral liquids calls upon pharmacies, hospitals, and health centers to dispense orally administered liquid medicines with metric dosing on the label, and pharmacies, hospitals, and health centers should distribute appropriate-volume mL-based dosing devices with all orally administered liquid medications.27 The 2016 APhA House of Delegates policy to guide labeling and measurement of oral liquid medication also supports access to and universal availability of dosing devices (eAppendix C).72 As part of the ABIM Foundation’s national Choosing Wisely initiative, ASHP recommended to patients and prescribers that metric-only oral dosing devices be used.47
4.3.6 Guidelines recommend dosing devices of appropriate volume and accuracy
A USP general chapter <659> update, which became effective in May 2019, specifically states for oral dosing devices (defined by USP as ‘graduated components’) packaged with the drug product:
“[u]nder expected conditions of use, the volume error incurred in measuring liquids for individual dose administration by means of such graduated components should be not more than 10% of the indicated amount of the liquid preparation with which the graduated component will be used.” 28
CHPA,20,21 FDA,22 AAP,27 and USP28,71 all recommend the use of dosing devices of appropriate size for measuring the recommended doses.
While it is not possible to make available a dose-specific device for each specific volume of medication that might be dispensed, to attain reasonable accuracy for doses ranging from an mL or less through 30 mL or more requires having more than a single size of dosing device available. Based on the dosing studies described in 4.3.3, which recommend the provision of an optimal dosing device that is not substantially larger than the recommended dose, and does not require measurement of multiple instrumentsful for provision of a single dose, a recommended approach is to ensure a dosing device is available of appropriate volume and accuracy for administering 1 mL or less; greater than 1 mL to 5 mL; greater than 5 mL to 10 mL; and greater than 10 mL.
See Table 1 for an approach for selecting dosing tools for prescription medications that has been adopted at several large pharmacy chains.
Table 1.
Approach to Selecting Dosing Tools for Prescription Medications Adopted by Several Large Pharmacy Chains
| Dose Volume | Device Volume |
|---|---|
| For administering doses 1 mL or less | Use a 1-mL syringe |
| For administering doses greater than 1 mL to 5 mL | Use a 5-mL syringe |
| For administering doses greater than 5 mL to 10 mL | Use a 10-mL syringe |
| For administering doses greater than 10 mL | Use a greater than 10-mL syringe or dosing cup |
In general, oral syringes are considered to be the best dosing device to use when dosing accuracy is important (e.g., drugs with narrow therapeutic index), and are especially recommended for small doses of 5 mL or less.27,43,71 Recommending oral syringes over dosing cups should be part of a comprehensive strategy to avoid pediatric medication errors, except for doses exceeding 10 mL where cups may be an alternative.27,43
In agreement with these volume-centric recommendations, USP recently proposed in an in-process revision notice for its general chapter <17> on prescription container labeling that the above algorithm be used to guide the choice of an appropriately sized oral dosing device that can most accurately measure the specific prescribed dose.71 This proposed change would replace the existing USP recommendation for providing an oral dosing tool (e.g., oral syringe, dosing cup) for oral liquid medications with more specific recommendations that an oral syringe be provided when dosing accuracy is important, particularly for doses of 5 mL or less, and that the capacity of the device should be considered in the context of the prescribed dose volume.71 The dosing device volume should be the smallest one capable of holding the entire dose as noted above.71
The volume markings on the dosing device should be legible, indelible, on an extraoral surface, and limited to a single metric measurement scale that corresponds with the dose instructions on the prescription container label.75
Unfortunately, a large percentage of parents and caregivers believe dosing cups are best for dosing accuracy.88 In a recent study, 1 in 4 caregivers believed cups were best for accuracy, and caregivers with low health literacy had a greater than 10-fold increased odds of choosing a dosing cup most of the time, with this misperception playing a large role in the relationship between low health literacy and dosing cup use.88 Caregiver education about the superiority of oral syringes for dosing accuracy, especially for small doses, is critically important and should be a priority during counseling about oral liquid medications by healthcare providers.88
5. REGULATION OVERVIEW
The content of prescription container labels is subject to both federal and state authorities. Examples of federal statutes and regulations concerning prescription labels include:
Food, Drug, and Cosmetic (FD&C) Act89 – “Exemptions and consideration for certain drugs, devices, and biological products”
Controlled Substances Act – Labeling and Packaging90 which includes “Statement of required warning” 91 and “Labeling of substances and filling of prescriptions” 92
Additional provisions are mandated by the individual state governments.
The Model State Pharmacy Act and Model Rules of the National Association of Boards of Pharmacy (NABP Model Act)93 identify critical and important information for patients that must appear, as well as additional information that may appear, on all prescription labels. While these model documents currently do not specifically comment on metric volumes in prescription labeling, NABP endorses the use of mL and supports pharmacists in exercising their professional prerogative to select mL as the standard unit of measure.d
As previously mentioned, oral liquid medications may be prescribed in a variety of units of measure. Although federal and state laws mandate the required elements of prescription container labels, including directions for use, it is the pharmacist’s professional prerogative to use their judgment to determine the appropriate units of measure, such as mL, to include on the prescription container label to ensure oral liquid medications are dosed accurately.
A review of state labeling requirements indicates there are no existing laws or regulations that expressly prohibit a pharmacist from changing the unit of measure or notation of decimal amounts to be used on a prescription labele and both medical and pharmacy practice organizations as well as regulatory and standards setting organizations currently recommend metric units be used exclusively for dosing instructions (Charles D, Office of the National Coordinator for Health Information Technology, personal communication; July 2, 2020).6-9,11,13-14,17,27,32,33,35,37,47,72,73,88,94 Therefore, as a best practice application of the widely endorsed practice standard of using mL for oral liquid medications, pharmacists should routinely convert prescriptions written in customary (household) units (e.g., teaspoon) to mL.
Most states provide for labels to contain “directions for use,” and therefore by interpretation, would allow pharmacists to use mL as the unit of measure. In fact, translation of the prescriber’s Sig into understandable instructions for the patient has historically been the professional prerogative of the pharmacist. One need only look at the historic method for Sig notation in Latin to document this. Certainly, in instances where the prescriber has indicated the dosage in mL, pharmacists should prepare the prescription label according to the prescription and dispense appropriately calibrated and volumetrically designed metric-only oral dosing devices. Importantly, if the dose is prescribed in household units, the pharmacist should change the patient instruction to the corresponding metric amount (e.g., 5 mL for one teaspoonful).
6. STAKEHOLDER CHALLENGES AND OPPORTUNITIES
Variations in how a liquid medication is ordered, transcribed, and transmitted, and then interpreted, entered, and printed, provide opportunities for errors in what appears on the prescription container labels of oral liquid prescription medications. Mitigation of these errors requires consistent use of mL as the universal standard unit of measure, use of leading zeros, and elimination of trailing zeros in dose designations by all the stakeholders who play a role in prescribing or providing patient instructions on the prescription container label. This consistency needs to extend to any oral instructions given to the patient at the time of prescribing and dispensing.
Even when the prescription container label utilizes mL as the standard unit of measure and standard notation of decimal amounts in dosing designations, an oral dosing device with numeric graduations, metric-only units, and appropriate volume that corresponds to the container labeling should be made available and its use explained to the patient or caregiver so the dose can be correctly interpreted and measured. Otherwise, if the patient or caregiver does not understand how to use the measuring device, he or she may resort to the use of the familiar and available household teaspoon or tablespoon. Because the volumes of these household utensils are not standardized, they have proven to be inaccurate and error-prone when used as medication measuring tools. Even sets of kitchen measuring spoons are not designed to accurately deliver oral doses of medications. As a result, steps should be taken to ensure consistent and standardized use of appropriately graduated metric-only oral dosing devices, and these devices should be made easily and universally available such as including a device each time oral liquid prescription medications are dispensed.
6.1 Pharmacy System Software Companies
Pharmacy system software can automate and speed outpatient medication dispensing. Pharmacy system software also can help standardize dosing units of measure and notation of amounts that display and print on container labels, as well as provide suggestions regarding optimal oral dosing device provision, but current software systems may have limitations.
In 2018, ASHP recommended the U.S. healthcare system adopt and only use the SI units, which would apply metric (e.g., mL) dosing units, for all patient- and medication-related measurements and calculations, and healthcare organizations use clinical decision support systems, equipment, and devices that allow input and display of patient- and medication-related measurements and calculations in SI format only.34 Further, ASHP recommended health information technology vendors use only SI units in their product designs for patient- and medication-related measurements, and education in the use of SI units and the importance of using SI units to prevent medical errors be promoted.34
ISMP recently issued guidelines for safe electronic communication of medication information via EHRs, e-prescribing, and other health information technology (HIT)-related tools in healthcare because of concerns that non-standardized communication conventions for medication information could contribute to medication errors.48 The importance of adopting recommended standards is particularly important in the setting of electronic communication about medications since a principal intent of such technologies is to mitigate risks.48 ISMP’s guidelines present a series of recommendations on safe electronic presentation of drug names, product selection menus and search options, complete medication orders and prescriptions, electronic system design features, and, importantly, doses, dosing weights, measures, and instructions for use.48 Included in these guidelines are recommendations for metric-only units such as mL, use of leading zeros and elimination of trailing zeros for doses, and elimination of apothecary and household units.48
6.1.1 Assessment of input and output of standard dosing designations
Pharmacy systems may need to make modifications to Sig or directions components to be able to use mL as the standard unit of measure for oral liquid prescription medications, instead of teaspoon, tablespoon, cc, dram, and others, and to express dose amounts per the white paper recommendations. For a pharmacy system to output the recommended standardized dosing designations, consideration must be given to the inputs into the pharmacy system. A key first step is to confirm the pharmacy system can accept, and is in fact receiving, dose designation information input as recommended from: drug databases, prescribing system software (particularly in the case of true e-prescribing), directly inputted data from the user, and other data input sources (e.g., payer claim responses, other interfaces such as electronic Medication Administration Record (eMAR)/HL7 data sources.)
Because pharmacy systems also may output data to other systems, the impact of changing pharmacy systems to output recommended standardized dosing designations also should be assessed. For example, some legacy pharmacy software systems may be unable to fully support mixed-case character sets in text strings, including drug descriptions and units of measure. These legacy limitations may require all UPPERCASE drug descriptions when displaying information on a computer monitor, printing on prescription labels and in patient education materials, and other situations. Furthermore, systems may not be able to programmatically convert internal use of UPPERCASE characters to lowercase or mixed-case immediately prior to transmitting data to a third party via NCPDP SCRIPTf transactions, continuity of care documentation, or electronic medical records and health information exchange. Typically, systems that have this type of limitation may be able to receive lowercase or mixed-case text, but once received, these are converted automatically to uppercase so the internal applications can properly process the data, and the data may not be able to be converted back.
While lowercase “ml” is not optimal or recommended due to the potential confusion between the lowercase letter “el” and the number one (“1”) in some printer and display fonts, “ml” still is preferable to the use of teaspoon, tablespoon, cc, dram, liquid ounce, oz, pint, etc. Therefore, although ISMP, USP, NCPDP, and others recommend milliliter be represented in mixed case (i.e., “mL”), some legacy systems currently have no option other than to represent milliliter in uppercase, or “ML”, and some may only be able to represent milliliter in all lowercase, or “ml”. These limiting situations currently may affect systems’ programmatic testing, error testing, and compliance reporting. However, NCPDP recommends the pharmacy system industry respond to these challenges by working to resolve these limitations to enable universal use of mL as the standard unit of measure and dosing and move as expeditiously as possible toward explicitly mandating mixed case support in future interface standards.
6.1.2 Enhancing systems for standardizing dosing designations
After it is confirmed that pharmacy systems can receive standardized dosing designation inputs, it still is likely that not all dosing information will be input as recommended. Appropriate decimal notation for amounts and mL as the unit of measure can be input manually by users by utilizing a “free form Sig” in combination with standard system Sig codes. However, manual data input by pharmacy system users takes more time, introduces a new opportunity for error, requires workflow changes, and asks for 100% compliance by users.
Pharmacy systems can facilitate standardized dosing designations by removing non-standard designations from the “Sig file” and setting default values to standardized dose designations.
Use of the NCPDP Structured and Codified Sigg within SCRIPT in conjunction with the recommendations in this white paper for standardizing dosing designations for oral liquid medication could further reduce ambiguity of the instructions. It is notable that at least one major professional physician organization (AMA) now recommends adoption of features like structured and codified Sig that help address quality issues be prioritized and e-prescribing be designated as the default prescription method.35
Until widespread adoption of Structured and Codified Sig is achieved, implementation of enhanced pharmacy system logic can help standardize (“edit” or “scrub”) inputs by users. Enhanced system logic may be designed to automatically express the Sig in desired “mL” units when oral liquids are selected. When a user inputs “.5,” enhanced system logic also can ‘auto-correct’ and store/output the data as “0.5”. In addition, when a user inputs “ML”, enhanced system logic can ‘auto-correct’ and store/output the data as “mL”.
Because of strong national advocacy for metric-only dosing, including mL-only dosing requirements in certified EHR prescribing software and retirement by USP of teaspoon as an official unit of measure, steps should be taken to automatically convert any teaspoon dosing presented at the pharmacy fulfillment level to mL dosing programmatically through dispensing software.
6.2 Electronic Drug Database Publishers
Pharmacy system software must reference accurate and timely drug databases to safely dispense medications as well as efficiently process medication claims. For claims processing, the NCPDP Billing Unit Standard contains mL as one of three billing units. Use of “mL” is indicated when a product is measured by its liquid volume, including liquid non-injectable products of 1 mL or greater.95 For safe and accurate medication dispensing, drug database publishers often offer dosing-related modules, such as structured Sig strings, Sig building tools, and dose-screening databases. These dosing-related modules also can be used by payers and pharmacy benefit managers (PBMs) to process drug claims, but when embedded into workflow applications for use by prescribers, pharmacists, nurses, and other healthcare professionals, they can help ensure medications are dispensed in appropriate doses and labeled with appropriate dosing designations.
Drug database modules and tools such as structured Sig strings, Sig builders, and dose screening should consistently represent liquid volumes in metric units and use the metric designation “mL” as a unit of measure for liquids where appropriate. In 2009, and again in 2011, ISMP issued a call to action for healthcare professionals, prescribing software companies, and pharmacy system software companies to eliminate the use of non-metric measurements, such as “teaspoon” and “tablespoon,” or associated variations like “tsp,” to prevent medication errors in prescription instructions.13-14,17 As supported by ISMP case reports, the disparity between the actual volume measured by using a household teaspoon or tablespoon as well as the possible confusion between the two easily can lead to incorrect dosing, with potentially serious consequences, especially in the pediatric population. In support of the ISMP initiative, drug database publishers reviewed their clinical database offerings to make sure no non-metric measurements were included, and metric units were used in dose screening databases and Sig databases.
All drug database publishers should be encouraged to re-review drug databases, modules, and tools for use of the standardized dosing designations for oral liquid medication recommended in this white paper. Pharmacy system software companies that use drug database publishers’ flat file data in their software can then adopt “mL” for use in structured Sig strings, just as “mL” is used in application programming interfaces (APIs) units for alert messages. To support the limitations noted in 6.1.1 as well as multiple end-user needs that are beyond the scope of this white paper, the drug database publishers may also offer their customers fields that use all uppercase and/or all lowercase text strings, in addition to the preferred mixed-case text strings, but should encourage migration as soon as feasible to the preferred mixed-case representation.
6.3 Prescribing Software Companies (including EHR with prescribing applications)
Electronic transmission of prescriptions from the prescriber to the community pharmacy affords numerous benefits to prescribers, pharmacies, and patients. The goal of e-prescribing is to have an electronic prescription arrive at the pharmacy with complete and clear instructions, eliminating the need for the pharmacy staff to interpret a prescriber’s handwritten instructions and prevent transcribing errors. It has been shown to improve quality and safety by decreasing dispensing errors associated with handwritten prescriptions. Reinforcing the importance of metric-only dosing for oral liquid medications, ONC EHR certification now requires e-prescribing software present Sig options to prescribers that apply metric units (e.g., mL) only and must not permit prescriber override to use household units (e.g., teaspoon) instead (Charles D, Office of the National Coordinator for Health Information Technology, personal communication; July 2, 2020).33 This change was implemented to support more precise prescription dosing and thus reduce dosing errors and improve patient outcomes and aligns with other federal partners (including FDA and CDC).33 Implementation of ONC EHR-certified prescribing software (Charles D, Office of the National Coordinator for Health Information Technology, personal communication; July 2, 2020)33 and adoption of ISMP’s guidelines for safe electronic communication of medication information48 are best practices that should be adopted.
Unfortunately, some segments of the industry may not have recognized the benefits or may not have embraced e-prescribing because of training, implementation, or software issues. To help address some of these concerns, a task group of the NCPDP e-Prescribing & Related Transactions Work Group (WG11), has produced a best practice guidance for the SCRIPT standard.36 The implementation guidance is intended for prescribing software companies, prescribers, and pharmacists to assist them in the proper use of fields within the SCRIPT standard. It also now references the recommendations of this white paper for implementing best practices aimed at addressing patient safety concerns associated with dispensing medications using non-metric measures such as teaspoon and tablespoon. Implementers of NCPDP’s Structured and Codified Sig are encouraged to review this white paper and support sending oral liquid prescriptions using only mL as the volume value. As of January 2020, when industry moved to SCRIPT 2017071, teaspoon, tablespoon, and other non-metric values were eliminated from the available code set in order to systematically support this patient safety initiative.36
e-Prescribing can provide the additional benefit of encouraging standardized dosing designations at the point of prescribing. By incorporating standard dosing designations (units using mL and amounts using decimals and zeros appropriately), e-prescribing software may be designed so that non-metric and non-volumetric units are never presented to the prescriber in any of the structured selection menus of Sig builders, drug description menus, or quantity qualifiers. In addition, the prescriber technology vendors could implement natural language processing and clinical decision support modules to alert their users if inappropriate values are selected.
The complete guidance may be viewed in the current “NCPDP SCRIPT Implementation Recommendations” at https://ncpdp.org/NCPDP/media/pdf/SCRIPT-Implementation-Recommendations.pdf?ext=.pdf.36
6.4 Pharmacy Leadership
NCPDP encourages community pharmacy leadership to adopt and implement the recommendations of this white paper in their pharmacies. The rationale and research cited in this white paper provide the basis for enhancing patient safety and positive medical outcomes through the use of mL as the universal standard unit of measure for oral liquid medications.
While NCPDP recognizes the adoption and implementation of these recommendations may pose a number of challenges and opportunities for community pharmacies in the areas of pharmacy computer systems, workflow, support of pharmacy staff and patient education, and consistency across products and care settings, the goal should be to take the necessary steps to put in place a transformation strategy in the interest of optimal use of oral liquid medication dosing and adoption of widely endorsed standard practices.
6.4.1 Pharmacy system software
Pharmacy leadership needs to make a commitment to make appropriate programming changes and create policies and procedures that will support universal adoption of these best practice recommendations. There are always challenges to system changes, but such change is possible and the corporate leadership of several pharmacy chains has decided to support the use of the mL, and has started by encouraging their pharmacists to migrate prescription directions from teaspoon and tablespoon to mL units and to provide appropriately sized and mL-marked dosing devices with all oral liquid prescription medications.
6.4.2 Workflow
Flagging of prescription receipts and sale procedures are considerations that may require changes in the workflow to allow for dispensing of appropriate calibrated oral dosing devices. Prescription data entry and selection of the proper Sig/direction codes for patient label directions reside in the workflow procedure and should support safety and process efficiency. Because of evidence supporting preferred oral dosing devices and volumes designed to minimize dosing errors, it would be optimal if pharmacy dispensing software could alert technicians and pharmacists to the most appropriate volume capacity device to dispense based on the prescribed dose volume.
6.4.3 Support of pharmacy staff and patient education
One important way pharmacy leadership can support this initiative is to inform, educate, and empower pharmacy staff by:
Establishing policies and procedures that support the widely endorsed standard metric dose designations for all oral liquid medications dispensed in pharmacies and convey these as standard best practices or policies to all the staff.
Providing pharmacies with adequate numbers of appropriately calibrated and metric-only marked dosing devices for distribution at dispensing of oral liquid prescription medication.
Provide guidance (e.g., through automated messaging) to help pharmacy staff select the most appropriate dosing device to accurately measure the volume of the prescribed dose. See Table 2.
Sharing the expectation that staff should routinely:
Provide appropriate dosing devices with oral liquid prescription medication.
Explain to patients/caregivers how to appropriately use the device to measure oral liquid medication.
Ensure patients and caregivers understand the use of the device, through the use of a teach back method, before leaving the pharmacy.
Providing ready access to this white paper (Web site link or printed copies) or other documentation of the:
Three white paper recommendations (See Section 2).
Dangers of improper dosing measurement and administration of oral liquid medications, especially in children and infants, and the rationale for the recommendations (See Section 4).
NABP endorsement of the use of mL as a professional prerogative and support of pharmacists to select mL as the standard unit of measure (See Section 5).
USP endorsement and support of mL as the universal standard unit of measure for oral liquid medications (See eAppendix A).
ONC EHR certification requirements that e-prescribing software only present metric doses for oral liquid medications and that prescribers not be permitted to override metric doses with household units (e.g., teaspoon).
Other documents and resources from professional, patient safety, and standard setting organizations, and government agencies, consistent with the white paper recommendations (See eAppendixes A-C).
Call to Action for pharmacy staff in this white paper (See Section 7.1, Stakeholder Map).
Table 2.
Guidance on Selecting Most Appropriate Dosing Device to Measure Volume of Prescribed Dose
| Dose Volume | Device Volume |
|---|---|
| For administering doses 1 mL or less | Use a 1-mL syringe |
| For administering doses greater than 1 mL to 5 mL | Use a 5-mL syringe |
| For administering doses greater than 5 mL to 10 mL | Use a 10-mL syringe |
| For administering doses greater than 10 mL | Use a dosing cup of volume greater than 10-mL syringe or dosing cup or if no larger volume dosing devices available, instruct patient/caregiver on performing multiple draws of 10-mL syringe |
Pharmacy leaders are encouraged to support pharmacist—patient counseling, communication, and education at point-of-dispensing. Community pharmacies can provide brochures or other patient-centered printed information to patients and caregivers and can emphasize these patient safety measures are being implemented to ensure proper dosing and patient safety.
6.4.4 Consistency across care settings and products
In the acute care inpatient setting and other healthcare facilities, mL is the widely endorsed standard oral liquid unit of measure and the use of leading zeros and avoidance of trailing zeros in dose designations is a requirement for accreditation by TJC. Responding to FDA and industry recommendations, OTC manufacturers have made substantial gains in moving to the use of mL for the standard unit of measure and standard notation of decimal amounts on package labels and dosing devices packaged with oral liquid OTC medications.20-22,25 Also, device manufacturers are producing more dosing devices that display an mL scale, some exclusively. Implementing the dose designation recommendations in this white paper will harmonize the labeling and administration of oral liquid prescription medications in the community setting with the standards used in inpatient and other healthcare settings, the standards for OTC medications, and international practices. This standardization should decrease patient, caregiver, and health professional confusion, and therefore improve patient safety.
7. STAKEHOLDER CALL TO ACTION: ADOPT, IMPLEMENT, ADHERE, COMMUNICATE, AND EDUCATE
The NCPDP Task Group Call to Action maps out roles for many stakeholders, but particularly relies on local and corporate community pharmacy leadership to:
Adopt and implement the recommendations in this white paper.
Communicate these as standard best practices or policies to all pharmacy staff.
Measure the performance of your organization in achieving these recommendations and stress accountability across your organization for adhering to them.
Engage pharmacy information system vendors and drug database producers to facilitate adoption of the standards on prescription container labels.
Explore implementation of innovative patient-centered communication and education solutions that target and encourage pharmacist-to-patient conversations and education at point of dispensing.
Facilitate communication by stakeholders outside the community pharmacy system, including prescribers, with a role in patient and healthcare professional education on using standardized dosing designations for prescribed oral liquid medications universally.
The “Stakeholder Map” (Table 3) identifies all the relevant stakeholders, listed alphabetically, who need to play a role in adopting, communicating, adhering, and educating. The map outlines a call to action and identifies some of the associated challenges and opportunities for each stakeholder group.
Table 3.
Stakeholder Map: Call to Action, Challenges, and Opportunities
| Stakeholder(s) | Call to Action | Challenges and Opportunities |
|---|---|---|
| Certification organizations — professional and systems | • Incorporate the white paper mL dose designation recommendations for oral liquid prescription medication into criteria for professional certification to attain universal metric-only standard practice • Incorporate the white paper widely endorsed dose designation recommendations for oral liquid prescription medications into updates, inspections, and testing of pharmacy system software, drug databases, and prescribing software |
• Provide education for healthcare professionals involved in dispensing medication, prescribing medication, and instructing patients and caregivers to administer medication • Provide education for system developers and designers |
| Dosing device manufacturers | Manufacture calibrated oral dosing devices for the pharmacy customer that have metric (mL) only dose designations and appropriate volumetric capacities as recommended in this white paper | Call for and participate in discussion about the standardization of devices, such as elimination of extraneous markings and inclusion of leading but not trailing zeros |
| Electronic drug database publishers and e-prescribing software vendors | • Review drug databases, modules, and tools for use of the standardized dosing designations for oral liquid medication. If not already used, update dosing designations to use mL as the universal standard unit of measure and to use leading zeros and not use trailing zeros for oral liquid prescription medication • Provide electronic referential drug information products using metric units (such as “mL”) in lieu of non-metric units (such as “teaspoon”) • Provide quantity qualifier mappings between proprietary internal codes and NCPDP codes so technology vendors can send accurate codes in all outbound messages • Offer customers fields that use the preferred mixed-case text strings rather than only uppercase and/or all lowercase text strings • Present dosing Sig options to prescribers that are metric-only for oral liquid medications and eliminate the option for prescriber override of the metric standard using household units (e.g., teaspoon) in e-prescribing software • Provide automated messaging capabilities that can alert pharmacy personnel concerning the most appropriate dosing capacity device (usually an oral syringe) to dispense based on the specific dose volume prescribed (e.g., 1-mL syringe for doses 1 mL or less, 5-mL syringe for doses greater than 1 mL to 5 mL, 10-mL syringe for doses greater than 5 mL to 10 mL, greater than 10-mL syringe or dosing cup for doses greater than 10 mL) |
• Provide consistency for all healthcare professionals in both inpatient and outpatient practice settings, eliminate confusion, and deliver a safer patient experience • A coordinated effort with pharmacy system software companies is required to overcome any existing challenges with field lengths designated for drug names • A coordinated effort with e-prescribing software vendors to adopt the universal metric-only standard is required to overcome any existing resistance to permitting prescriber override to household units |
| Government agencies | • Incorporate dosing designations that only use mL as the universal standard unit of measure and use leading zeros and not use trailing zeros for oral liquid prescription medication into standards, guidance, and software certification requirements • Collaborate with standards setting organizations and device manufacturers to develop standards for dosing devices for oral liquid prescription medications aligned with existing guidelines and guidance for OTC medications • Collaborate with industry e-prescribing leaders and organizations to promote universal adoption of the metric-only standard for dosing oral liquid medications • Provide a coordinated announcement and/or distribution mechanism that will effectively communicate the recommendations of this white paper to all relevant stakeholders |
• Provide guidance to healthcare organizations and professionals to support the transition to mL as the universal standard unit of measure for oral liquid prescription medications • Drive elimination of units of measure that are already in use through a widespread coordinated effort to overcome any existing challenges |
| National Association of Boards of Pharmacy and state boards of pharmacy | • Reiterate supportive stance for the use of mL as the universal standard unit of measure for oral liquid prescription medications • Find opportunities to incorporate metric recommendations into NABP Model Act and Rules • Provide an announcement and/or distribution mechanism that will effectively communicate the recommendations of this white paper to the state board of pharmacies and pharmacists • Collaborate with state and national medical board organizations to promote universal adoption of the metric-only standard for dosing oral liquid medications |
|
| Pharmacists and pharmacy technicians | • Use mL as the universal standard unit of measure on prescription container labels. Avoid other abbreviations (cc, ml, ML) and the spelled-out term milliliters ◦ When the prescription Sig contains dosing designations in mL, mL dosing instructions should be used on the prescription container label and an appropriately calibrated and volumetrically designed metric-only oral dosing device should be dispensed ◦ When the prescription Sig contains dosing instructions in non-volumetric units (e.g., mg) or non-standard volumetric units (e.g., teaspoonful, tablespoonful, dropperful), convert the dosing instructions to mL, use mL dosing instructions on the prescription container label, and dispense an appropriately calibrated and volumetrically designed metric-only oral dosing device |
• Communicating with healthcare professionals and educating and counseling patients and caregivers takes additional time • Seek synergies and innovative solutions to improve patient education and communication at point-of-dispensing through collaboration with pharmacy system as well as other stakeholders • Periodically perform quality control checks by observing processes in the pharmacy to ensure adherence to the standardized work practices |
|
• Always use leading zeros before a decimal point, and never use trailing zeros after a decimal point on prescription container labels for oral liquid medications ◦ Do not use trailing zeros (e.g., “2” mL not “2.0” mL and “2.5” mL not “2.50” mL or “2.500” mL) ◦ Place adequate space between the dose and unit of measure (e.g., “10 mL” not “10mL”) |
||
| • When dispensing an oral liquid medication, include a dosing device with numeric graduations and units that apply the mL standard, correspond to the container labeling, and are of appropriate volume to accurately measure the prescribed dose (or tell patients or caregivers where an appropriate device can be obtained) • Ensure verbal patient counseling, communication, and education at point-of-dispensing using dosing designations that are consistent with the prescription container label and the dosing device • Ensure patients or caregivers have access to an appropriate dosing device before they leave the pharmacy • Use a teach-back method to educate patients or caregivers on how to use dosing devices correctly and • Educate other pharmacy staff regarding importance of using mL as the universal standard unit of measurement for all oral liquid medications |
||
| Pharmacy leadership — local and corporate | • Commit to adopting and implementing widely recommended dose designation standards for prescription container labels for oral liquid medications dispensed from their pharmacies to attain universal metric-only standard practice ◦ Make appropriate computer system programming changes that will support the dose designation standards ◦ Make required changes in the workflow to ensure dispensing of appropriately calibrated and volumetrically designed metric-only oral dosing devices ◦ Establish policies and procedures that support the standard dose designations for all oral liquid medications dispensed in pharmacy ◦ Convey the standard best practices and policies to all the staff ◦ Provide pharmacies with adequate numbers of oral dosing devices with numeric graduations and units that apply the mL standard, correspond with the container labels, and are of appropriate volumes for distribution at the dispensing of oral liquids; a range of dosing devices (e.g., 1-, 5-, and 10-mL oral syringes) should be readily available for dispensing |
• Seek synergies and innovative solutions to improve patient education and communication at point-of-dispensing through collaboration with both pharmacy systems, as well as other stakeholders (such as local prescribers) • Test and update pharmacy system software to ensure it incorporates the standards and recommendations in this white paper • Educate staff regarding the importance of standardizing to universal use of mL as the unit of measure, the use of leading zeros, and the elimination of trailing zeros for oral liquid prescription medications • Periodically perform quality control checks by observing processes in the pharmacy to ensure adherence to the standardized work practices |
|
◦ Share expectations with staff that they should distribute dosing devices with all oral liquid prescription medication, teach patients and caregivers how to use the device, and ensure patients and caregivers understand the use of the device and importance of not substituting household utensils • Inform pharmacy staff where they can access this white paper readily (Web site or printed copies) or other documentation of the white paper’s recommendations and the rationale for them; the dangers of improper dosing; the NABP endorsement and support of pharmacists exercising professional prerogative in selecting mL as the universal standard unit of measure; USP’s endorsement and support; ONC’s certification requirement for metric-only e-prescribing of oral liquid medications; other documentation and resources from professional, patient safety and standards setting organizations, and from government agencies, that are consistent with the white paper recommendations; and this white paper’s call to action for pharmacy staff • Collaborate with pharmacy system software developers and companies to incorporate the recommended labeling changes • Optimize pharmacist—patient counseling, communication, and education at point-of-dispensing |
||
| Pharmacy system software companies | • Eliminate “teaspoon” and other non-metric volumetric units of measure from data files for all oral liquid medications • Modify the Sig or directions components of the systems program to ensure use of mL as the universal standard unit of measure for oral liquid medication instead of teaspoon or other non-metric measures and to express dose amounts per the white paper recommendations ◦ Use free text Sig in combination with standard system Sig codes ◦ Automate the change as a system default in the “Sig file” • Assure that mnemonics, Sig codes, or any defaults used in computer systems to generate prescriptions and prescription labels uniformly produce directions using mL • Use “mL” in any alert messages, just as the drug database publishers’ APIs use “mL” units for alert messages • Address legacy limitations to representing milliliter in mixed case (mL) to enable universal use of mL as the standard unit of measure |
• Eliminate “teaspoon” and other non-metric volumetric units of measure from data files for all oral liquid medications • Collaborate with drug database publishers on the timing of system change for the elimination of non-metric measures for liquid oral medications • Test and update pharmacy system software to ensure it incorporates the recommendations in this white paper |
| Prescribing software companies (including EHR with prescribing applications) | • Provide default dosing designations that use mL, use leading zeros, and do not use trailing zeros in prescribing software • Eliminate “teaspoon” and other non-metric volumetric units of measure from data files for all oral liquid medications • Use “mL” in dosing-related modules (such as structured Sig strings, Sig building tools, and dose screening databases) that can be embedded into workflow applications and e-prescribing whenever appropriate • Develop documentation for end users on creation of basic and complex e-prescription messages and provide training to users • Work with certification organizations to incorporate the white paper recommendations in the testing criteria • Incorporate best practices from the NCPDP SCRIPT Implementation Recommendations (https://ncpdp.org/NCPDP/media/pdf/SCRIPT-Implementation-Recommendations.pdf) • Eliminate prescriber opportunities for overriding metric-only dosing in e-prescribing software |
Communicate this white paper’s recommendations to all prescribers that use your prescribing software, emphasizing the patient safety benefits |
| Professional organizations and trade associations | • Incorporate or reiterate supportive stance on the white paper dose designation and dosing device-related recommendations for oral liquid prescription medications into policy statements or statements of professional standards | • Provide an announcement and/or distribution mechanism that would effectively communicate the recommendations of this white paper to all members • Obtain organizational consensus to publish support and advocate for the elimination of non-metric volumetric units of measure and adoption of the use of mL as the universal standard unit of measure for oral liquid medications |
| Standards setting organizations | • Incorporate or reiterate supportive stance on the white paper dose designation and dosing device-related recommendations for oral liquid prescription medications | • Provide an announcement and/or distribution strategy to effectively communicate the recommendations of this white paper to healthcare organizations and professionals • Provide guidance to healthcare organizations and professionals to support the transition to the use of mL as the universal standard unit of measure for oral liquid medications, the use of leading zeros, and elimination of the use of trailing zeros |
Abbreviations: API, active pharmaceutical ingredient; NABP, National Association of Boards of Pharmacy; NCPDP, National Council for Prescription Drug Programs; ONC, Office of the National Coordinator for Health Information Technology; OTC, over-the-counter; USP, United States Pharmacopeia.
8. Conclusions
Although metric units (e.g., mg for milligrams) have been the universal standard unit of measure for solid dose form medications for decades, oral liquid medications continue to be prescribed, transcribed, dispensed, measured, and administered using a variety of volumetric units, which continues to lead to confusion, dosing errors, and overdosing or underdosing by healthcare professionals, patients, and caregivers. Standard dosing designations used consistently on prescriptions and container labels of oral liquid medications, the dosing devices used to measure and administer them, and the routine provision of dosing devices of appropriate volume and graduation to support accurate dosing, could help improve patient safety and patient outcomes.
The adoption of this white paper’s recommendations will harmonize the transcription, labeling, dispensing, measuring, and administration of oral liquid prescription medications in the community setting with standards used in hospital and other healthcare facilities, recommendations for OTC medications, and international standards of volumetric measurement to finally attain universal metric-only standard practice for oral liquids across all care settings.
The NCPDP mL Task Group Call to Action is directed first and foremost to the local and corporate pharmacy leadership, as they can catalyze many of the changes required to implement the best practices described in this white paper.
NCPDP recognizes there are challenges for pharmacy leadership to adopt and implement the recommendations, as well as for many of the other stakeholders.
A concerted effort of all stakeholders is necessary to realize the opportunities and overcome the challenges. NCPDP calls on all the relevant stakeholders to support efforts to adopt, implement, and adhere to the recommendations and standards in this white paper, and to educate healthcare professionals, patients, and caregivers on how to accurately measure and administer oral liquid medications.
All stakeholders are encouraged to ensure implementation of the recommendations and call to action of this white paper and to collaborate to achieve standardized dosing designations for prescription container labels of oral liquid medications dispensed from community pharmacies, and promote the provision of appropriate oral dosing devices that support accurate medication administration.
DISCLAIMER
While all information in this document is believed to be correct at the time of writing, the writers may review and possibly update their recommendations should any significant changes occur. This document is for educational and awareness purposes only and does not purport to provide legal advice. Readers requiring legal advice should consult an attorney. The information provided here is for reference use only and does not constitute the rendering of legal, financial, or other professional advice or recommendations by NCPDP. The listing of an organization does not imply any sort of endorsement, and NCPDP takes no responsibility for the products or tools. The existence of a link or organizational reference in this document should not be assumed as an endorsement by the NCPDP
Supplementary Material
Appendix—Contributors to this white paper
Note: The organizations listed below should not be considered endorsers of this white paper.
WG10 Professional Pharmacy Services Co-Chairs
Catherine Graeff, RPh, MBA, Sonora Advisory Group
Larry King, Surescripts
Lisa Schwartz, National Community Pharmacists Association (NCPA)
mL White Paper Task Group Lead
Gerald K. McEvoy, PharmD, Consultant, former Assistant Vice President, Drug Information, American Society of Health-System Pharmacists (ASHP)
Leslie Carr, CPhT, NCPDP Staff
mL White Paper Primary Contributors
Thomas R. Bizzaro, RPh, Retired, former Vice President, Health Policy and Industry Relations, FDB
Donna Bohannon, United States Pharmacopeial Convention (USP)
Catherine Graeff, RPh, MBA, Sonora Advisory Group
Michael J. Gaunt, PharmD, Institute for Safe Medication Practices (ISMP)
Gerald K. McEvoy, PharmD, Consultant, former Assistant Vice President, Drug Information, American Society of Health-System Pharmacists (ASHP)
H. Shonna Yin, MD, MS, Associate Professor of Pediatrics and Population Health, NYU Grossman School of Medicine
mL White Paper Federal Government Liaison
CAPT Daniel Budnitz, MD, MPH, Centers for Disease Control and Prevention (CDC), USPHS
Developed by National Council for Prescription Drug Programs, Scottsdale, AZ
Footnotes
The original 2014 version 1.0 of this white paper was titled “NCPDP recommendations and guidance for standardizing the dosing designations on prescription container labels of oral liquid medications.”
Participants included electronic drug database publishers, chain pharmacies, mail order pharmacies, drug distributors, community pharmacy system software vendors, drug manufacturers (McNeil Healthcare), government (US Food and Drug Administration [FDA] and Centers for Disease Control and Prevention [CDC]), and non-governmental organizations (American Society of Health-System Pharmacists [ASHP], Institute for Safe Medication Practices [ISMP], National Association of Boards of Pharmacy [NABP], National Association of Chain Drug Stores [NACDS], and United States Pharmacopeial Convention [USP])
The USP-NF adopted the use of metric units as a standard as expressed in the International System of Units (SI) as established and revised by the Conference generale des poid et measures almost 40 years ago. The convention includes milliliter (mL) as a standard metric unit. The convention has been incorporated into standards for prescribing and dispensing that state that compendial articles (drug/drug product) must be written to state the quantity and/or strength desired in metric units.
National Association of Boards of Pharmacy (NABP; Mount Prospect, IL): Personal communication; 2020 Jul 1.
National Association of Boards of Pharmacy (NABP; Mount Prospect, IL): Personal communication; 2020 Jul 1.
The SCRIPT is an NCPDP standard developed for transmitting prescription information electronically between prescribers, pharmacies, payers, and other entities for new prescriptions, changes of prescriptions, prescription refill requests, prescription fill status notifications, cancellation notifications, relaying of medication history, transactions for long-term care, electronic prior authorization and other transactions
The Structured and Codified Sig Format is intended to facilitate communication between prescribers and pharmacists, improve the efficiency of the prescribing and dispensing activities, and help reduce the opportunity for errors. It provides standardization of the portion of an electronic prescription containing the directions for use, using existing, accepted electronic transmission standards. The structured and codified is available in NCPDP SCRIPT Standard 10.4 and above.
References
- 1. Centers for Disease Control and Prevention. The PROTECT Initiative: advancing children’s medication safety. Accessed November 29, 2013. http://www.cdc.gov/medicationsafety/protect/protect_Initiative.html.
- 2. National Council for Prescription Drug Programs. NCPDP Recommendations for improved prescription container labels for medicines containing acetaminophen Version 1.1. Accessed November 29, 2013. http://www.ncpdp.org/Whitepaper.aspx.
- 3. National Council for Prescription Drug Programs. Universal medication schedule white paper. Accessed October 24, 2013. http://www.ncpdp.org/Whitepaper.aspx.
- 4. Budnitz DS, Lovegrove MC, Geller R. Prevention of Unintentional Medication Overdose Among Children: Time for the Promise of the Poison Prevention Packaging Act to Come to Fruition. JAMA. 2020; 324:550-551. [DOI] [PubMed] [Google Scholar]
- 5. American Society of Hospital Pharmacists. Guidelines for single unit packages of drugs. Approved by the ASHP Board of Directors 1966 Dec 2. Am J Hosp Pharm. 1971; 28:110-112. [PubMed] [Google Scholar]
- 6. American Health Care Association, American Pharmaceutical Association, and American Society of Hospital Pharmacists. Pharmaceutical services in the long-term care facility. 7th ed. second printing. American Pharmaceutical Association; 1975. [Google Scholar]
- 7. Barker KN, Heller WM. The development of a centralized unit-dose dispensing system for UMAC. Part III: an editing center for physicians’ medication orders. Am J Hosp Pharm. 1964; 21:66-67. [Google Scholar]
- 8. Hynniman CE, Conrad WF, Urch WA, Parker PF. A comparison of errors under the University of Kentucky unit dose system and traditional drug distribution systems in four hospitals. Am J Hosp Pharm. 1970; 27:802-814. [PubMed] [Google Scholar]
- 9. American Society of Health-System Pharmacists. ASHP guidelines on preventing medication errors in hospitals. (Supersedes ASHP guidelines on preventing medication errors 1993 Jun 23.) Am J Health-Syst Pharm. 2018; 75:1493-1517. Accessed April 21, 2020. https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/preventing-medication-errors-hospitals.ashx?la=en&hash=CFDD375E109297517C3CB96BDADE7B0D59E2560A30257844 [Google Scholar]
- 10. The Joint Commission. Official “do not use” list fact sheet. Chicago, IL: the Joint Commission. Published June 2019. Accessed February 18, 2021. https://www.jointcommission.org/-/media/tjc/documents/fact-sheets/do-not-uselist-fact-sheet-06-28-19.pdf?db=web&hash=043C80759207C3EC9616DDD3D5557113 [Google Scholar]
- 11. The Joint Commission. E-dition ambulatory information standards. IM.02.02.01. Chicago, IL: the Joint Commission. Published August 25, 2014. Accessed April 22, 2020. https://www.jointcommission.org/standards/national-patient-safety-goals/-/media/5d62fa0f81e8459e9e156378d992b7c6.ashx [Google Scholar]
- 12. Institute for Safe Medication Practices. ISMP’s list of error-prone abbreviations, symbols, and dose designations. Accessed April 22, 2020. https://www.ismp.org/recommendations/error-prone-abbreviations-list.
- 13. Institute for Safe Medication Practices. Safety standards needed for expressing/measuring doses of liquid medications. ISMP Med Saf Alert Com/Amb. 2011; 10(6):1-4. [Google Scholar]
- 14. Institute for Safe Medication Practices. ISMP statement on use of metric measurements to prevent errors with oral liquids. Horsham, PA: Institute for Safe Medication Practices. Published October 1, 2011. Accessed May 20, 2020. https://www.ismp.org/news/ismp-statement-usemetric-measurements-prevent-errorsoral-liquids [Google Scholar]
- 15. Institute for Safe Medication Practices. Still outside the bull’s eye: 2014-2015 Targeted medication safety best practices. ISMP Med Saf Alert Acute Care. 2014; 19(6):1-5. Accessed April 26, 2020. https://www.ismp.org/resources/still-outside-bulls-eye-2014-2015-targeted-medication-safety-best-practices-baseline [Google Scholar]
- 16. Institute for Safe Medication Practices. 2020–2021 Targeted medication safety best practices for hospitals.Horsham, PA: Institute for Safe Medication Practices. Accessed April 26, 2020. https://www.ismp.org/guidelines/best-practices-hospitals [Google Scholar]
- 17. Institute for Safe Medication Practices. A teaspoon of medicine? ISMP Med Saf Alert Com/Amb Care. 2009; 8(5):1-2. [Google Scholar]
- 18. Institute for Safe Medication Practices. ISMP guidelines for safe and electronic communication of medication information. Horsham, PA: Institute for Safe Medications Practices. Published 2019. Accessed April 26, 2020. https://ismp.org/resources/guidelines-safe-electronic-communication-medication-information [Google Scholar]
- 19. National Coordinating Council for Medication Error Reporting and Prevention. Recommendations to enhance accuracy of prescription/medication order writing. Adopted September 4, 1996. Updated October 22, 2014. Accessed April 22, 2020. https://www.nccmerp.org/recommendations-enhance-accuracy-prescription-writing
- 20. Consumer Healthcare Products Association. Guideline volumetric measures for dosing of over-the-counter liquid oral drug products for children ≤12 years of age. Washington, DC: Consumer Healthcare Products Association. Published November 17, 2009. Accessed February 18, 2021. https://www.chpa.org/public-policy-regulatory/voluntary-codes-guidelines/chpa-voluntary-guideline-volumetric-measures [Google Scholar]
- 21. Consumer Healthcare Products Association. Standard terminology and format for labeling of volumetric measures on OTC pediatric orally ingested liquid drug products. In: CHPA voluntary codes and guidelines. Washington, DC: Consumer Healthcare Products Association. Updated November 14, 2014. Accessed April 23, 2018. https://www.chpa.org/VoluntaryCodesandGuidelines.aspx [Google Scholar]
- 22. Food and Drug Administration. Guidance for industry: dosage delivery devices for orally ingested OTC liquid drug products. Final. Silver Spring, MD: Food and Drug Administration; Published May 2011. Accessed November 29, 2013. https://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm188992.pdf [Google Scholar]
- 23. Food and Drug Administration. Medication errors related to CDER-regulated drug products. Silver Spring, MD: Food and Drug Administration. Published January 6, 2020. Accessed April 22, 2020. https://www.fda.gov/drugs/drug-safety-and-availability/medication-errors-related-cder-regulated-drug-products [Google Scholar]
- 24. Food and Drug Administration. Safety considerations for product design to minimize medication errors: guidance for industry. Silver Spring, MD: Food and Drug Administration. Published April 2016. Accessed April 16, 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/safety-considerations-product-design-minimize-medication-errors-guidance-industry [Google Scholar]
- 25. Budnitz DS, Lovegrove MC, Rose KO. Adherence to label and device recommendations for over-the-counter pediatric liquid medications. Pediatrics. 2014; 133:e283-90. doi: 10.1542/peds.2013-2362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Food and Drug Administration. Guidance for industry: safety considerations for container labels and carton labeling design to minimize medication errors. Draft. Silver Spring, MD: Food and Drug Administration. Published April 2013. Accessed April 16, 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/safety-considerations-container-labels-and-carton-labeling-design-minimize-medication-errors [Google Scholar]
- 27. American Academy of Pediatrics. Policy statement. Metric units and the preferred dosing of orally administered liquid medications. Pediatrics. 2015; 135:785-787. doi: 10.1542/peds.2015-0072 [DOI] [Google Scholar]
- 28. United States Pharmacopeia. USP-NF general chapter <659> Packaging and storage requirements. Associated components section. In: USP 42 – NF 37. Rockville, MD: United States Pharmacopeial Convention. Published May 1, 2019. Accessed April 16, 2020. https://online.uspnf.com/uspnf/document/1_GUID-48C0134E-8117-4B3B-8DC4-EA70C93EEE8F_3_en-US?source=TOC [Google Scholar]
- 29. United States Pharmacopeial Convention. 44(4) In-process revision: general chapter <659> Packaging and storage requirements. Briefing. Pharmacopeial Forum. 2018; 44:(USP 41 p 6384) [Google Scholar]
- 30. Consumer Healthcare Products Association. AHPA Board of Directors approves changes to industry’s voluntary guidelines for pediatric liquid products. Press release. Washington, DC: Consumer Healthcare Products Association. Published November 19, 2014. Accessed April 16, 2020. https://www.chpa.org/volguid.aspx [Google Scholar]
- 31. Food and Drug Administration. Over-the-counter pediatric oral liquid drug products containing acetaminophen: guidance for industry. Silver Spring, MD: Food and Drug Administration. Published April 2015. Accessed April 23, 2018. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM417568.pdf. [Google Scholar]
- 32. American Academy of Pediatrics. Policy statement. Electronic prescribing in pediatrics: toward safer and more effective medication management. Pediatrics. 2013;131:824-826. doi: 10.1542/peds.2013-0192 [DOI] [PubMed] [Google Scholar]
- 33. Department of Health and Human Services Office of the National Coordinator for Health Information Technology (ONC). 2015 Edition health information technology (health IT) certification criteria, 2015 edition base electronic health record (EHR) definition, and ONC health IT certification program modifications. 45 CFR 170 (RIN 0991-AB93). Final rule. Fed Regist. 2015; 80:62602-62759. PMID:26477063. [PubMed] [Google Scholar]
- 34. American Society of Health-System Pharmacists. Policy positions and guidelines. Use of International System of Units for patient- and medication- related measurements (ASHP policy 1811. Supersedes ASHP policy 1312). Bethesda, MD: American Society of Health-System Pharmacists. Published 2018. Accessed April 16, 2020. https://www.ashp.org/-/media/assets/policy-guidelines/docs/policy-positions/policy-positions-organization-and-delivery-of-services.ashx [Google Scholar]
- 35. American Medical Association Board of Trustees. Safe and efficient e-prescribing. Health policy H-120.921. Chicago, IL: American Medical Association. Updated 2019. Accessed April 29, 2020. https://policysearch.ama-assn.org/policyfinder/detail/medication%20errors%20?uri=%2FAMADoc%2FHOD.xml-H-120.921.xml [Google Scholar]
- 36. National Council for Prescription Drug Programs. NCPDP SCRIPT implementation recommendations. Version 1.56. Scottsdale, AZ. Published February 2021. Accessed February 18, 2021. https://www.ncpdp.org/NCPDP/media/pdf/SCRIPT-Implementation-Recommendations.pdf [Google Scholar]
- 37. American Academy of Family Physicians. AAFP policy. Preferred unit of measurement for liquid medications. (2016 Congress of Delegates). (Board Chair September 21, 2011. Accessed April 22, 2020. https://www.aafp.org/about/policies/all/preferred-unit.html
- 38. Yaffe SJ, Bierman CW, Cann HMet al. for the American Academy of Pediatrics Committee on Drugs . Inaccuracies in administering liquid medication. Pediatrics. 1975; 56:327-8. PMID:1161381. [PubMed] [Google Scholar]
- 39. Food and Drug Administration. Important information for safe use of Tussionex Pennkinetic extended-release suspension─full version. Podcast transcript. FDA archive. Silver Spring, MD: Food and Drug Administration. Published March 11, 2008. Accessed April 22, 2020. https://wayback.archive-it.org/7993/20171105113645/https://www.fda.gov/Drugs/DrugSafety/DrugSafetyPodcasts/ucm078908.htm [Google Scholar]
- 40. Yin HS, Parker RM, Sanders LMet al. Effect of medication label units of measure on parent choice of dosing tools: a randomized experiment. Acad Pediatr. 2016; 16:734-741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Harris LM, Dreyer BP, Mendelson ALet al. liquid medication dosing errors by Hispanic parents; role of health literacy and English proficiency. Acad Pediatr. 2017; 17:403-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Vernacchio L, Kelly JP, Kaufman DW, Mitchell AA. Medication use among children <12 years of age in the United States: results from the Slone Survey. Pediatrics. 2009; 124:446-454. [DOI] [PubMed] [Google Scholar]
- 43. Yin HS, Parker RM, Sanders LMet al. Liquid medication errors and dosing tools: a randomized controlled experiment. Pediatrics 2016; 138(4):e20160357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sobhani S, Christopherson J, Ambrose PJ, Corelli RL. Accuracy of oral liquid measuring devices: comparison of dosing cup and oral dosing syringe. Ann Pharmacother. 2008;42:46-52. [DOI] [PubMed] [Google Scholar]
- 45. Shah R, Blustein L, Kuffner E, Davis L. Communicating doses of pediatric liquid medicines to parents/caregivers: a comparison of written dosing directions on prescriptions with labels applied by dispensed pharmacy. J Pediatr. 2014; 164:596-601. doi: 10.1016/j.jpeds.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 46. American Society of Health-System Pharmacists. Policy positions and guidelines. Elimination of apothecary system (ASHP policy 8613; reaffirmed in 2016). Bethesda, MA: American Society of Health-System Pharmacists. Published 2016. Accessed April 27, 2020. https://www.ashp.org/-/media/assets/policyguidelines/docs/policy-positions/policy-positions-drug-productslabeling-packaging.ashx [Google Scholar]
- 47. ABIM Foundation. Choosing wisely. American Society of Health-System Pharmacists: five things physicians and patients should question. Philadelphia, PA: ABIM Foundation. Updated June 20, 2019. Accessed April 26, 2020. https://www.choosingwisely.org/wp-content/uploads/2017/05/ASHP-Choosing-Wisely-List.pdf [Google Scholar]
- 48. Institute for Safe Medication Practices. ISMP guidelines for safe and electronic communication of medication information. Horsham, PA: Institute for Safe Medications Practices; 2019. Accessed April 26, 2020. https://ismp.org/resources/guidelines-safeelectronic-communication-medicationinformation [Google Scholar]
- 49. Seifert SA, Jacobitz K. Pharmacy prescription dispensing errors reported to a regional poison control center. J Toxicol Clin Toxicol. 2002; 40:919-923. [DOI] [PubMed] [Google Scholar]
- 50. Institute for Safe Medication Practices. Please, no more teaspoon dosing. ISMP Med Saf Alert Com/Amb. 2017; 16(11):4-5. [Google Scholar]
- 51. Institute for Safe Medication Practices. Another TEAspoon—mL mix-up. ISMP Med Saf Alert Acute Care. 2011; 16(19):3. [Google Scholar]
- 52. Bronstein AC, Spyker DA, Cantilena LR Jret al. 2010 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 28th Annual Report. Clin Toxicol (Phila). 2011; 49:910-941. [published correction appears in Clin Toxicol (Phila). 2014; 52:1285] [DOI] [PubMed] [Google Scholar]
- 53. Bronstein AC, Spyker DA, Cantilena LR Jret al. American Association of Poison Control Centers. 2011 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 29th Annual Report. Clin Toxicol (Phila). 2008; 46:927-1057. [DOI] [PubMed] [Google Scholar]
- 54. Bronstein AC, Spyker DA, Cantilena LR Jret al. 2008 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 26th Annual Report. Clin Toxicol (Phila). 2009; 47:911-1084. [DOI] [PubMed] [Google Scholar]
- 55. Bronstein AC, Spyker DA, Cantilena LR Jret al. 2009 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 27th Annual Report. Clin Toxicol (Phila). 2010; 48:979-1178. [DOI] [PubMed] [Google Scholar]
- 56. Bronstein AC, Spyker DA, Cantilena LR Jret al. 2010 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 28th Annual Report. Clin Toxicol (Phila). 2011; 49:910-941. [DOI] [PubMed] [Google Scholar]
- 57. Gummin DD, Mowry JB, Spyker DAet al. 2018 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 36th Annual Report. Clin Toxicol (Phila). 2019; 57:1220-1413. [DOI] [PubMed] [Google Scholar]
- 58. Mowry JB, Spyker DA, Cantilena LR Jret al. 2012 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th Annual Report. Clin Toxicol (Phila). 2013; 51:949-1229. [DOI] [PubMed] [Google Scholar]
- 59. Mowry JB, Spyker DA, Cantilena LR Jret al. 2013 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 31st Annual Report. Clin Toxicol (Phila). 2014; 52:1032-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mowry JB, Spyker DA, Brooks DEet al. 2014 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd Annual Report. Clin Toxicol (Phila). 2015; 53:962-1147. [published correction appears in Clin Toxicol (Phila). 2016;54:607] [DOI] [PubMed] [Google Scholar]
- 61. Mowry JB, Spyker DA, Brooks DEet al. 2015 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd Annual Report. Clin Toxicol (Phila). 2016; 54:924-1109. [DOI] [PubMed] [Google Scholar]
- 62. Gummin DD, Mowry JB, Spyker DAet al. 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin Toxicol (Phila). 2017; 55:1072-1252. [published correction appears in Clin Toxicol (Phila). 2017; 55:1256] [DOI] [PubMed] [Google Scholar]
- 63. Gummin DD, Mowry JB, Spyker DAet al. 2017 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th Annual Report. Clin Toxicol (Phila). 2018; 56:1213-1415. [DOI] [PubMed] [Google Scholar]
- 64. Tzimenatos L, Bond GR for the Pediatric Therapeutic Error Study Group . Severe injury or death in young children from therapeutic errors: a summary of 238 cases from the American Association of Poison Control Centers. Clin Toxicol (Phila). 2009; 47:348-354. [DOI] [PubMed] [Google Scholar]
- 65. Institute for Safe Medication Practices. Misunderstood abbreviations. ISMP Med Saf Alert Com/Amb Care. 2005; 4(8):2. [Google Scholar]
- 66. Yin HS, Dreyer BP, Ugboaja Det al. Units of measurement used and parent medication dosing errors. Pediatrics. 2014; 134:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Yin HS, Parker RM, Sanders LMet al. Pictograms, units and dosing tools, and parent medication errors: a randomized study. Pediatrics 2017; 140:e20163237. doi: 10.1542/peds.2016-3237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Torres A, Parker RM, Sanders LMet al. Parent preferences and perceptions of mLs and teaspoons: role of health literacy and experience. Acad Pediatr. 2018; 18:26-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Yin HS, Dreyer BP, Ugboaja DCet al. Unit of measurement used and parent medication dosing errors. Pediatrics. 2014; 134:e354-e361. doi: 10.1542/peds.2014-0395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ryu GS, Lee YJ. Analysis of liquid medication dose errors made by parents and caregivers using alternative dosing devices. J Manag Care Pharm. 2012; 18:439-445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. United States Pharmacopeial Convention. 46(2) In-process revision: general chapter <17>. Prescription container labeling (USP). Pharmacopeial Forum. 2020; 46(2). DocID: GUID-46BF6E02-E3E3-492E-A344-8194C8ACC17F_10101_en-US. https://online.usppf.com/usppf/document/GUID-46BF6E02-E3E3-492E-A344-8194C8ACC17F_10101_en-US?highlight=general%20chapter%2017 [Google Scholar]
- 72. American Pharmacists Association. APhA House of Delegates adopt policy to guide labeling and measurement of oral liquid medications. Washington, DC: American Pharmacists Association. Published March 17, 2016. Accessed April 15, 2020. https://www.pharmacist.com/press-release/apha-house-delegates-adopt-policyguide-labeling-and-measurementoral-liquid [Google Scholar]
- 73. United States Pharmacopeia. General notices and requirements applying to standards, tests, assays, and other specifications of the United States Pharmacopeia. 9: Prescribing and dispensing. 9.10: Use of metric units. In: USP 42 – NF 37. United States Pharmacopeial Convention; Official 2019. May 1. [Google Scholar]
- 74. United States Pharmacopeial Convention. 36(2) In-process revision: general chapter <1221> Teaspoon (USP34-NF29 1S). Briefing. Pharmacopeial Forum. 2010; 36:534 (USP 32:728). Accessed April16, 2020. http://www.usppf.com/pf/pub/index.html [Google Scholar]
- 75. United States Pharmacopeial Convention. 41(3) In-process revision: general chapter <659>. Packaging and storage requirements (USP38). Pharmacopeial Forum. 2015; 41:(USP 38:443). Accessed April 16, 2020. http://www.usppf.com/pf/pub/index.html [Google Scholar]
- 76. American Medical Association Council on Science and Public Health. Medication (drug) errors in hospitals. Prescribing and dispensing policy H-120.968. Chicago, IL: American Medical Association; 2014. Accessed April 27, 2020. https://policysearch.amaassn.org/policyfinder/detail/%20AMA%20Policies%20medication%20errors?uri=%2FAMADoc%2FHOD.xml-0–181.xml. [Google Scholar]
- 77. American College of Obstetrics and Gynecology Committee on Patient Safety and Quality Improvement. Committee opinion No. 531: improving medication safety. Obstet Gynecol. 2012; 120:406-410. doi: 10.1097/AOG.0b013e3182680478 [DOI] [PubMed] [Google Scholar]
- 78. Levine SR, Cohen MR, Blanchard NRet al. for the Institute of Safe Medication Practices and the Pediatric Pharmacy Advocacy Group . Guidelines for preventing medication errors in pediatrics. J Pediatr Pharmacol Ther. 2001; 6:427-443. Accessed April 27, 2020. [Google Scholar]
- 79. Gaunt MJ, Cohen MR. Error-prone abbreviations and dose expressions. In: Cohen MR, ed. Medication errors. 2nd ed. American Pharmacists Association; 2007:165. [Google Scholar]
- 80. Institute for Safe Medication Practices. Please don’t sleep through this wake-up call. ISMP Med Saf Alert Acute Care. 2001; 6(9):1. Accessed November 18, 2018. https://www.ismp.org/resources/please-dontsleep-through-wake-call [Google Scholar]
- 81. American Society of Health-System Pharmacists. Policy positions and guidelines. Standardization of oral liquid medication concentrations (ASHP policy 1401; reaffirmed 2019). Bethesda, MD: American Society of health-System Pharmacists. Published 2014. Accessed April 16, 2020. https://www.ashp.org/-/media/assets/policy-guidelines/docs/browse-by-document-type-policypositions-1982-2019-with-rationalespdf.ashx?la=en&hash=8AC3BD24C9CA40CF1958C38A0D60DD66462D0A88 [Google Scholar]
- 82. Institute for Safe Medication Practices. ISMP and FDA campaign to eliminate the use of error-prone abbreviations. Horsham, PA: Institute for Safe Medication Practices. Published 2006. Accessed November 6, 2013. http://www.ismp.org/tools/abbreviations/ [Google Scholar]
- 83. United States Pharmacopeia. <7> Labeling: Use of leading and terminal zeros. In: USP 42–NF 37. US Pharmacopeial Convention; September 1, 2019. Accessed April 27, 2020. https://online.uspnf.com/uspnf [Google Scholar]
- 84. World Health Organization. Drug and therapeutics committees: a practical guide. Holloway K (ed). Geneva, Switzerland: World Health Organization; 2003:53. https://apps.who.int/iris/bitstream/handle/10665/68553/WHO_EDM_PAR_2004.1.pdf?sequence=1&isAllowed=y [Google Scholar]
- 85. Institute for Safe Medication Practices. Archaic liquid measure a factor in medication errors. ISMP Med Saf Alert Com/Amb. 2012; 11(7):1-2. [Google Scholar]
- 86. Kwan D, Vohra R, Dyer JEet al. An infant with a heartbreaking medication error. Pediatr Emerg Care. 2014; 30:e1-e5. [DOI] [PubMed] [Google Scholar]
- 87. Dewalt DA. Ensuring safe and effective use of medication and health care: perfecting the dismount. JAMA. 2010; 304:2641-2642. [DOI] [PubMed] [Google Scholar]
- 88. Williams TA, Wolf MS, Parker RMet al. Parent dosing toll use, beliefs, and access: a health literacy perspective. J Pediatr. 2019; 215:244-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.21 United States Code (USC) §353 (b) (2)
- 90.21 USC §825 (c)
- 91.21 CFR §290.5
- 92.21 CFR §1306.24
- 93. NABP. Model State Pharmacy Act and Model Rules of the National Association of Boards of Pharmacy (NABP Model Act). Mount Prospect, IL: National Association of Boards of Pharmacy. Published August 2020. Accessed September 11, 2020. https://nabp.pharmacy/publicationsreports/resource-documents/modelpharmacy-act-rules/. [Google Scholar]
- 94. United States Pharmacopeial Convention. General notices and requirements applying to standards, tests, assays, and other specifications of the United States Pharmacopeia. Terms and definitions. 8.240: Weights and measures. In: USP 42 – NF 37. Official 2019. May 1. [Google Scholar]
- 95. National Council for Prescription Drug Programs. NCPDP billing unit standard fact sheet. Scottsdale, AZ: National Council for Prescription Drug Programs; published July 2013. Accessed January 22, 2020. https://www.ncpdp.org/NCPDP/media/pdf/BUS_fact_sheet.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.