Abstract
Adrenal gland trauma is a rare and scarcely reported injury due to its retroperitoneal position and relationship with adjacent tissues. We report a male patient with a history of a thoracoabdominal blunt trauma with adrenal injury as an isolated abdominal viscera. He was hemodynamically stable at admission, with a blush within his adrenal hematoma. The patient was treated nonoperatively and subsequently discharged after 15 days. The available literature reports advantages of a nonoperative approach compared to surgery, which is necessary in only 1% of cases that are predominantly polytrauma patients with multiple intra-abdominal injuries. Therefore, a nonoperative treatment is recommended for patients with an isolated adrenal gland injury who are hemodynamically stable during hospital stay.
Keywords: Adrenal gland, Trauma, Management, Non operative, Abdomen
Introduction
Adrenal gland trauma is a rare and scarcely reported injury, with an incidence of 0.03% to 4.95% of all trauma cases [1,2]. It usually results from blunt and high-impact thoracoabdominal trauma, such as motor vehicle collisions, with a mortality rate of 7% to 32.6% [1]. Contrast computed tomography (CT) of the abdomen and pelvis is the gold standard for such diagnosis [3,4].
A trauma to the adrenal gland is rare due to the retroperitoneal position of the gland and its relationship with adjacent soft tissues [1,2]. When present, it is generally associated with rib, chest, liver, vertebra, kidney, and spleen injuries [1], being more commonly associated with thoracic and rib injuries (>50%) and liver damage (>40%). The right adrenal gland is the most commonly affected [1,2]. An isolated adrenal gland injury without other concomitant injuries is extremely rare, with an incidence of only 1.5% to 4% of all adrenal traumas and less than 0.007% of the total number of traumas [1]. This report describes a case of adrenal gland trauma with blush as a solid isolated viscera due to a thoracoabdominal blunt trauma after a three-meter fall that was diagnosed and treated at the Sorocaba Hospital Complex (CHS), Sorocaba, SP, Brazil.
Material and methods
A bibliographic search was performed using the PubMed database with the Medical Subject Heading method for the following keywords: “Adrenal trauma” and “surgery,” obtaining a total of 11 articles published from 2003 to 2020. Articles on pediatric patients were excluded, resulting in the review of seven articles.
Case report
A 59-year-old male patient, with no previous medical history, was brought by the medical rescue team on a rigid board with a cervical collar 1 h after falling from a three-meter height (stairs). The patient underwent the recommended Advanced Trauma Life Support protocol procedures. The initial evaluation showed patent airways; a well-positioned cervical collar; pulmonary auscultation without changes; peripheral O2 saturation of 90% on room air, which improved to 97% after placement of a V-shaped O2 face mask at 10 L/min; cardiac auscultation without changes; heart rate 100 bpm and blood pressure 130 × 100 mmHg; a stable pelvis; closed pubic symphysis; soft and painful abdomen on palpation in the right hypochondrium but without signs of peritonitis; and an hematoma in the right posterior flank without other apparent lesions. Vesical catheterization did not show hematuria. The patient received intravenous lactated Ringer's solution (500 mL) and analgesia with tramadol.
An Extended Focused Assessment with Sonography for Trauma was performed in the trauma room, which showed an absence of free intraperitoneal fluid, B lines at the apex and base of the right lung, and signs of pneumothorax or fluid collection. Chest and pelvis radiographs showed no acute injuries other than the rib fractures. CT of the skull and cervical spine showed no acute traumatic changes. Chest CT revealed complete fractures in the 2nd, 4th, 5th, 6th, 7th, and 8th right ribs, a piece of a metallic thread in the 4th right rib, and lower pulmonary lobes showing a ground-glass pattern, possibly corresponding to an inflammatory process. Intravenous contrast-enhanced CT of the abdomen and pelvis identified a finding compatible with a blush within a right adrenal hematoma (Fig. 1). The decision for a nonoperative treatment (NOT) and observation was made considering the patient's hemodynamic stability and CT findings.
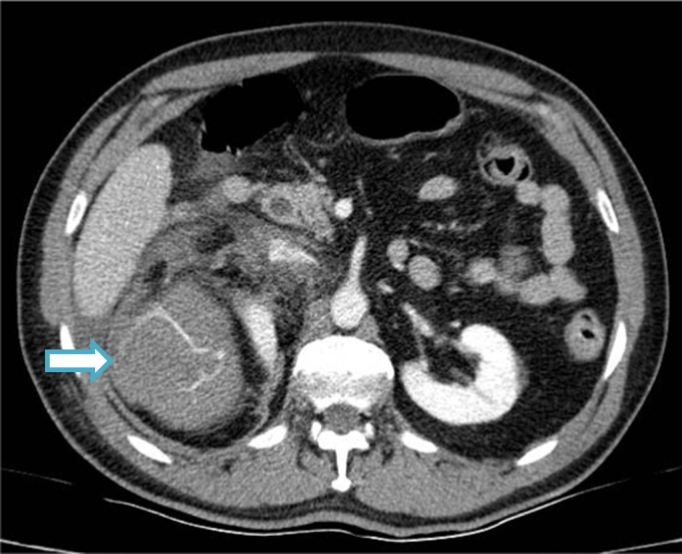
Fig. 1.
CT image at admission showing a 110 × 90 mm hematoma in the upper portion of the right perirenal fat compressing the kidney and right hepatic lobe (arrow), with signs of contrast extravasation due to active bleeding associated with a small amount of liquid/hematic perihepatic content in the anterior and posterior peri- and pararenal fat and right paracolic gutter.
Laboratory tests showed a decreased hemoglobin level from 8.0 mg/dL to 5.2 mg/dL 48 h after the trauma, even though the patient was still hemodynamically stable. Abdominal CT was repeated, which showed a partial enlargement of the hematoma but without new signs of contrast extravasation (blush). Magnetic resonance imaging was contraindicated due to the presence of a piece of a metallic wire in the right costal arch (Fig. 2).
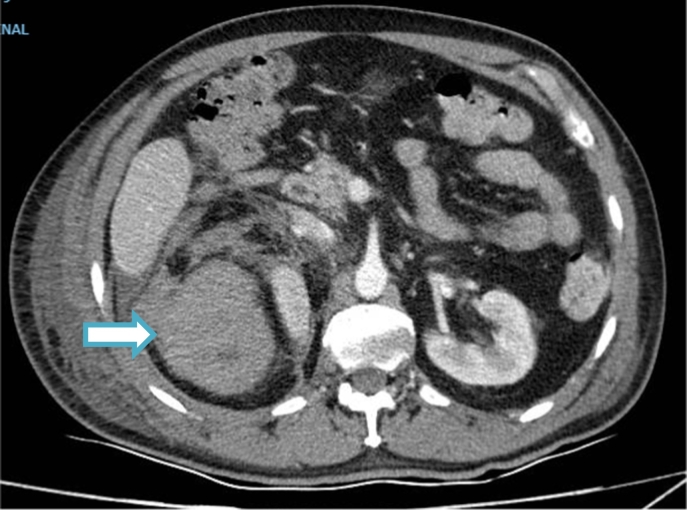
Fig. 2.
Control CT image showing a massive right adrenal hematoma measuring 11.7 × 9.8 cm in the largest axis (arrow). Small right perirenal hematoma measuring 1.2 cm in maximum thickness with obliteration of the perirenal fat and thickening of the pararenal fasciae is seen. The right adrenal hematoma was slightly increased. No active bleeding areas were identified in the present analysis with the evaluation protocol used.
Subsequently, the patient received the transfusion of two units of red blood cells to maintain the stability of his hemodynamic parameters and laboratory findings. Although the patient could have been discharged after trauma treatment, he was kept hospitalized to complete his antibiotic therapy for nosocomial pneumonia.
Discussion
Abdominal trauma due to automotive events is often the main cause of isolated adrenal gland injuries [6]. At admission, the patient's Shock Index was 1.038 and the Injury Severity Score (ISS) was 2. These findings corroborate the results of similar cases reports, which usually have a benign progression and low scores. A review by DiGiacomo et al. postulated that adrenal traumas rarely significantly increase the ISS and that a negative relationship between ISS and adrenal trauma can exist when compared to similar cases considering other factors such as age, year of admission, and race [5,6].
Adrenal trauma was once considered extremely rare and more likely to occur only in severe cases of traumas. New evidence shows that adrenal trauma is a part of a larger group of other underdiagnosed lesions and more substantial use of CT has increased the identification of minor lesions that were previously unidentified [7]. In the present case, CT was indicated due to the patient's hemodynamic stability, trauma mechanism, and abdominal pain. A hematoma of approximately 110 × 90 mm was identified in the right adrenal gland, with a minimal amount of free liquid in the abdominal cavity, but with densification of the perihepatic fat planes. Thus, considering the CT findings combined with the patient's clinical condition, NOT was chosen.
Most adrenal traumas are unilateral and on the right side [8]. They are usually associated with other abdominal intraperitoneal traumas, such as those of the liver (41.6%), kidney (27.8%), and spleen (22%) [7], and are rarely found in isolation, occurring in only 1.5% of the traumas [[6], [7], [8]]. The right adrenal gland is more likely to be affected than the contralateral gland due to its anatomical position close to the spinal bone structures and drainage through the vena cava. The usual trauma mechanism of the organ can be either by tissue compression against the spine or by compression of the vena cava during trauma, which would retrogradely increase the intra-adrenal venous pressure [7,9].
The patient remained hospitalized for 15 days, remaining stable throughout the period. The successful NOT in this patient confirms the benign progression in most of the similar cases. Raup et al. analyzed 7791 cases, where surgical management was needed for only 1% of patients, mostly in polytrauma patients with multiple intra-abdominal injuries. In recent years, mortality due to adrenal gland trauma has been actually lower than previously assumed. When the adrenal gland is the only injured organ, there is a 20% decrease in the number of deaths during hospitalization compared to that with injuries associated with other abdominal organs [7].
Conclusion
Isolated adrenal trauma has a low incidence and is now being increasingly diagnosed by CT. The good clinical outcome of the patient shows the possibility of a conservative management in patients with hemodynamic stability during the initial care.
References
- 1.Lehrberg A., Kharbutli B. Isolated unilateral adrenal gland hemorrhage following motor vehicle collision: a case report and review of the literature. J. Med. Case Rep. 2017 Dec 26;11(1):358. doi: 10.1186/s13256-017-1506-x. 29277157 PMC5742871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karwacka I.M., Obołończyk Ł., Sworczak K. Adrenal hemorrhage: a single center experience and literature review. Adv. Clin. Exp. Med. 2018 May;27(5):681–687. doi: 10.17219/acem/68897. 29616752 [DOI] [PubMed] [Google Scholar]
- 3.Papadopoulos K.S., Strigklis K., Kordeni K., Xaplanteri P., Zacharis G. Adrenal gland injury after blunt abdominal trauma: two case series and review of the literature. Int. J. Surg. Case Rep. 2020;67:34–38. doi: 10.1016/j.ijscr.2020.01.021. 32004901 PMC7076276. (Epub 2020 Jan 27) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raup V.T., Eswara J.R., Vetter J.M., Brandes S.B. Epidemiology of traumatic adrenal injuries requiring surgery. Urology. 2016 Aug;94:227–231. doi: 10.1016/j.urology.2016.03.022. 27017900 (Epub 2016 Mar 24) [DOI] [PubMed] [Google Scholar]
- 5.DiGiacomo J.C., Angus L.D., Coffield E. Adrenal injuries: historical facts and modern truths. World J. Surg. 2017 Apr;41(4):975–979. doi: 10.1007/s00268-016-3840-3. 27882417 [DOI] [PubMed] [Google Scholar]
- 6.DiGiacomo J.C., Gerber N., Angus L.D.G., Munnangi S., Cardozo-Stolberg S. Blunt adrenal injury: results of a state trauma registry review. Am. Surg. 2019 Apr 1;85(4):390–396. 31043200 [PubMed] [Google Scholar]
- 7.Karwacka I.M., Obołończyk Ł., Sworczak K. Adrenal hemorrhage: a single center experience and literature review. Adv. Clin. Exp. Med. 2018 May;27(5):681–687. doi: 10.17219/acem/68897. 29616752 [DOI] [PubMed] [Google Scholar]
- 8.Untereiner O., Charpentier C., Grignon B., Welfringer P., Garric J., Mertes P.M. Adrenal trauma: medical and surgical emergency. Emerg. Med. J. 2013 Apr;30(4):329–330. doi: 10.1136/emermed-2012-201438. 22609698 (Epub 2012 May 19) [DOI] [PubMed] [Google Scholar]
- 9.Lin Y.-H., Wu T. Isolated adrenal hemorrhage after blunt trauma: case report and literature review. Urol. Sci. 2013 Mar;24(1):27–29. doi: 10.1016/j.urols.2013.01.002. [DOI] [Google Scholar]