Abstract
Study Objectives:
To systematically survey the scientific literature concerning the effect of playing a wind instrument or singing on sleep, snoring, and/or obstructive sleep apnea.
Methods:
The PubMed, EMBASE, and Cochrane databases were searched up to December 2019. Observational studies and (Randomized) Controlled Clinical Trials that assessed sleep, snoring, or obstructive sleep apnea as clinical outcome or via a questionnaire were included. For the individual studies, the potential risk of bias was scored. Data between oral musicians and control participants were extracted. Descriptive analysis and meta-analysis were performed.
Results:
Six eligible studies (5 cross-sectional, 1 randomized controlled trial) were retrieved, with an estimated potential bias ranking from low to high. The sample sizes ranged from 25 to 1,105 participants. Descriptive analysis indicated that players of a double-reed instrument have a lower risk of obstructive sleep apnea and that singers snore less compared with control participants. Playing a didgeridoo showed a positive effect on apnea-hypopnea index, daytime sleepiness, and partner’s rating for sleep disturbance. The descriptive analysis could not be substantiated in the meta-analysis. The magnitude of the effect was zero to small, and the generalizability was limited because of long (professional) rehearsal time or small sample size.
Conclusions:
Playing a wind instrument and singing may have a small but positive effect on sleep disorders. Considering the practicality and investment of (rehearsal) time, didgeridoo and singing are the most promising interventions to reduce obstructive sleep apnea and snoring, respectively. However, the results of this review are based on few studies and the synthesis of the evidence is graded to have low certainty.
Citation:
van der Weijden FN, Lobbezoo F, Slot DE. The effect of playing a wind instrument or singing on risk of sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med. 2020;16(9):1591–1601.
Keywords: wind instrument, singing, sleep, snoring, OSA, sleep apnea
INTRODUCTION
Human beings spend about one-third of their life either sleeping or attempting to sleep. Sleep is essential for normal cognitive functioning and survival. Yet it can be disturbed or abnormal.1
The pharyngeal airway lacks substantial bony or rigid support. Thus, the patency of the pharyngeal airway is largely dependent on the activity of various pharyngeal dilator muscles. As long as these muscles are sufficiently active, the patency of the airway is maintained.2 When the muscles relax during sleep, soft tissue in the back of the throat can collapse, causing turbulence and vibration (snoring) or even partial or complete obstruction of the upper airway (obstructive sleep apnea, OSA).3,4 In the case of OSA, the (largely) obstructed pharyngeal airway prevents effective ventilation, producing either partial reductions (hypopneas) or complete stops (apneas) in breathing. In either case, these (hypo)apneas will lead to reduced oxygen levels and elevated carbon dioxide levels in the blood. The brain responds to this by alerting the body, causing a brief arousal from sleep that re-establishes the airway patency and normal breathing. This pattern can occur hundreds of times in 1 night.2,4 The severity of OSA is expressed according to the apnea-hypopnea index (AHI), a measure that represents the combined number of apneas and hypopneas that occur per hour of sleep.4
The result of OSA is a fragmented sleep that often produces excessive daytime sleepiness,4 which in turn can compromise safety on the roads and reduce work productivity.5–7 OSA is also associated with an increased risk of hypertension,8 cardiovascular disease,9 incident heart failure,10 and myocardial infarction,11 among other possible consequences. The susceptibility for OSA may vary by individual and can be influenced by several factors, such as the size of the pharyngeal airway, the size of the tongue and/or the tonsils, and mandibular retrognathism.2
Several treatments have been developed over the years to treat snoring and OSA. Many of them are invasive and involve either surgery or wearing a device during sleep.4,12 Therefore, an alternative treatment approach that is noninvasive, safe, and effective would be beneficial. Because the dilator muscles of the upper airway play a critical role in maintaining an open airway during sleep, researchers have explored exercises that target oral cavity and oropharyngeal structures as an alternative method to treat OSA,13 such as oropharyngeal exercises. These are derived from speech therapy and consist of isomeric (continuous) and isotonic (intermittent) movements involving the tongue, soft palate, and facial muscles, as well as stomatognathic functions like suction, swallowing, chewing, breathing, and speech. The series of exercises are based on the concept that muscle training while awake will reduce upper airway collapsibility during sleep.14 A significant decrease in snoring frequency, snoring intensity, daytime sleepiness, sleep quality score, and OSA severity (measured using AHI) has been observed among patients who had performed these exercises for 3 months, as has a significant reduction in neck circumference. The latter suggests that the exercises induced upper airway remodeling.14 A meta-analysis performed by Camacho et al13 demonstrated that oropharyngeal exercises decrease AHI by approximately 50% in adults and 62% in children. Lowest oxygen saturations, snoring, and sleepiness outcomes improved. The authors concluded that oropharyngeal exercises could serve as an adjunct to other OSA treatments. A more recent systematic review by the same authors based on both subjective questionnaires and objective sleep studies indicated that, with oropharyngeal exercises, a reduction in snoring by approximately 50% in adults can be achieved.15
If oropharyngeal exercises are indeed effective for reducing snoring and the risk of OSA, it could be useful to explore those individuals who have spent years engaging in training of the airway muscles as part of their hobby or profession: wind-instrument musicians. The whole complex of anatomical structures around the mouth, as well as the way in which they are used in playing a wind instrument, is called “embouchure.”16 The 3 main embouchure components are the tongue, the teeth, and the cheek and lip muscles, but the palate and pharynx also play an important role.16,17 Other airway training involves singing, which requires control of the muscles of the larynx, hypopharynx, oral pharynx, and oral cavity.18 To our knowledge, no systematic review or meta-analysis has been published of studies evaluating sleep, snoring, or OSA among oral musicians compared with controls. Therefore, the aim of this systematic review is to comprehensively search the scientific literature to identify, critically appraise, analyze, and synthesize studies that address the effect of playing a wind instrument or singing on sleep, snoring, and/or OSA.
METHODS
Protocol
The recommendations for strengthening reporting were followed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA),19 in combination with the guidelines for Meta-analyses Of Observational Studies in Epidemiology (MOOSE),20 and the PRISMA extension for abstracts.21 The protocol that details the review method was developed a priori following an initial discussion among the members of the research team, and registered in PROSPERO (International Prospective Register of Systematic Reviews) (CRD42019134672).
Focused question and eligibility criteria
The PICOS-question (Population, Intervention, Comparison, Outcomes and Study)22 to be answered in the present review is: In observational studies and (randomized) controlled clinical trials, what is the observed effect on sleep, snoring, and OSA in people who play a wind instrument or are singers compared with those who do not play a wind instrument or do not sing?
The following criteria were imposed for inclusion in the systematic review:
Observational studies and (randomized) controlled clinical trials describing the effect of playing a wind instrument or singing compared with controls.
Any clinical outcome or questionnaire evaluating sleep, snoring, and OSA, such as daytime sleepiness, quality of sleep, snoring score, risk of OSA, diagnosis of OSA, or AHI.
The exclusion criteria were as follows:
Editorial letters, narrative reviews, case series, case reports, protocols, and abstracts.
Information sources and search
The PubMed-MEDLINE, EMBASE, and Cochrane-CENTRAL databases were searched from initiation up to December 2019 (F.N.W.). The search strategy is listed in Table 1. Gray literature was also searched via Google Scholar. Additionally, the reference lists of all selected studies were hand-searched for additional relevant articles (F.N.W., D.E.S.).
Table 1.
Search strategy for PubMed.
| (<wind instrument*> OR <music AND instrument> OR <didgeridoo OR didjeridu OR yidaki> OR <singing or “singing”[MeSH]>) |
| AND |
| (<“Sleep Apnea, Obstructive” [MeSH]> OR <(sleep OR nocturnal) AND (apnea OR hypopnea OR apnea OR (breath* AND disorder*))> OR <OSA OR OSAS OR OSAHS> OR <”snoring” [MeSH] OR snore> OR <sleepiness OR somnolence OR (quality AND sleep)>) |
The search strategy was customized according to the database being searched. The asterisk was used as a truncation symbol.
Study selection
The titles and abstracts of the studies obtained from the searches were screened independently by two reviewers (F.N.W., D.E.S.) and were categorized as definitely eligible, definitely not eligible, or questionable. No language restrictions were imposed. No attempt was made to conceal the names of authors, institutions, or journals from the reviewers while making the assessment. If eligible criteria were present in the title, the paper was selected for further reading. If none of these criteria were mentioned in the title, the abstract was read in detail to screen for suitability. Papers that could potentially meet the inclusion criteria were obtained and read in detail by the 2 reviewers (F.N.W., D.E.S.). Disagreements in the screening and selection process concerning eligibility were resolved by consensus or, if disagreement persisted, by arbitration through a third reviewer (F.L.). The papers that fulfilled all of the inclusion criteria were processed for data extraction.
Data collection process, summary measures, and synthesis of results
When provided, information about the characteristics of the study sample population, intervention, comparison, and outcomes were extracted independently from the selected studies by two reviewers (F.N.W., D.E.S.). As age, BMI, and male sex are well-known risk factors for snoring and OSA, these data were also extracted when reported for further analysis. Means and standard deviations were extracted (Table S1 and Table S2 in the supplemental material) or, if missing, requested from the original authors. If a confidence interval was reported, the standard deviation was calculated based on the mean and the number of participants.23 As a summary, a descriptive data presentation was used for all the studies.
If feasible, the data from the included studies were synthesized into a meta-analysis (D.E.S., F.N.W.). In studies consisting of multiple comparisons and data from one particular group compared with more than one other group, the number of subjects (n) in the group was divided by the number of comparisons. A meta-analysis was only performed if at least 2 studies could be included. The difference of means or risk ratio between test and control was calculated for each index/scale using a “random effects” model (Review Manager, version 5.3 for Windows, The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). The goal was to estimate the mean effect in a range of studies where the overall estimate was not overly influenced by any one of them.24 A subgroup analysis was conducted relative to the type of musical performance (singing and different types of wind instruments, Figure 1) when possible. In addition, a meta-analysis of common risk factors was performed. Formal testing for publication bias was performed when possible using the method proposed by Egger et al.25
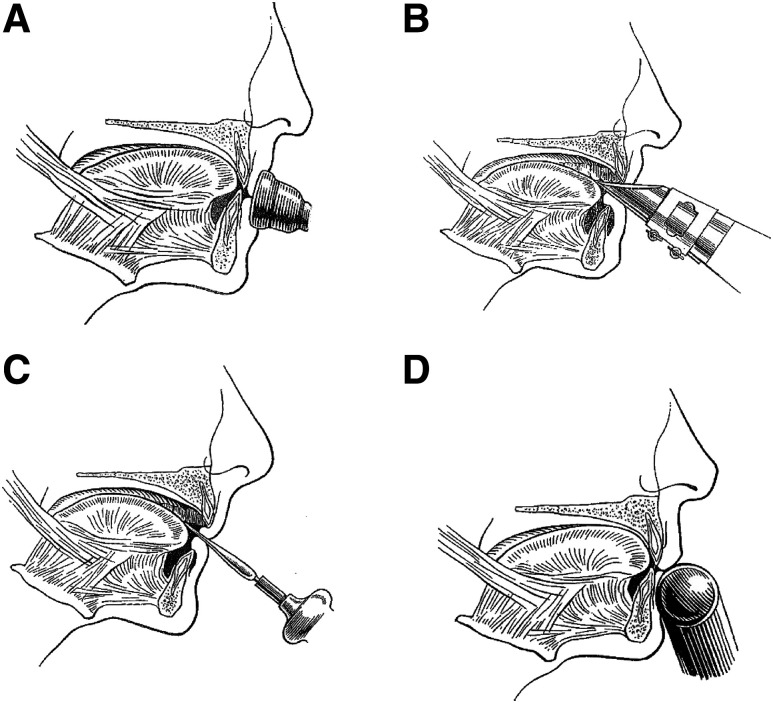
Figure 1. Classification of different types of wind instruments.
(A) Brass instruments (eg, trumpet, trombone, horn, tuba) are placed outside the mouth by pressing the bowl-like mouthpiece against the upper and lower lip. Both upper and lower anterior teeth provide support for the lips. Depending on the height of the tone, the lips are pulled tight and set in vibrato.16,27 (B) With playing single-reed instruments (eg, clarinet, saxophone), a wedge-shaped mouthpiece, on which at the underside a reed is attached, is placed partly in the mouth and between the lips. The maxillary incisors rest on the sloping upper surface of the mouthpiece, while the lower lip is placed between the lower surface of the reed and the mandibular incisal edges (single-lip embouchure).16,27 (C) Double-reed instruments (eg, oboe, bassoon) have a mouthpiece made from 2 bamboo reeds bound together with a cord. The 2 reeds are placed in the mouth, between the upper and lower lips, which cover the underlying incisal edges (double-lip embouchure).16,27 (D) When playing the flute and the piccolo, the mouthpiece is held against the lower lip, whereby the lower anterior teeth serve as a support. The upper lip is pushed downward to form a small slit-shaped opening between the lower and upper lip, through which air is directed toward the opposite rim of the blowhole. The embouchure of the flute is partly controlled by the position of the flute in relation to the upper lip. This is done by a rotation movement of the flute in the plica mentalis in combination with alternating protrusion and retrusion of the mandible.16,27 Reprinted with permission from British Dental Journal.26
Risk of bias in individual studies
Two reviewers (F.N.W., D.E.S.) scored the potential risk of bias for the included studies. For assessment of the studies with a cross-sectional design, a checklist was used as proposed by Van der Weijden et al28 (Table S3). For randomized controlled trials (RCTs), a checklist was used as proposed by Van der Weijden et al29 (Table S4).
Assessment of heterogeneity and sensitivity analysis
Several factors were used to evaluate the clinical and methodological heterogeneity of the characteristics across the different studies: study design, intervention (wind instrument playing/singing), and variables used to assess sleep, snoring, and OSA.
As part of the meta-analysis, heterogeneity was statistically tested using the chi-square test and the I2 statistic. A chi-square test resulting in a P <.1 was considered an indication of significant statistical heterogeneity. As an approximate guide to assessing the possible magnitude of inconsistency across studies, an I2 statistic of 0–40% was interpreted to indicate unimportant levels of heterogeneity. An I2 statistic of 30–60% may represent moderate heterogeneity; an I2 statistic of 50–90% may represent substantial heterogeneity; a statistic of greater than 75% was interpreted to indicate considerable heterogeneity.30
Considerable heterogeneity was evaluated with sensitivity analysis to assess effect modification (F.N.W.). Outliers were explored as being the source of heterogeneity. If there was a significant difference between the test and control group for any of the risk factors, these studies/subgroups were removed in the sensitivity analysis.
Rating the certainty of the evidence (GRADE)
To appraise the evidence emerging from this review, the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system proposed by the GRADE working group was used. Two reviewers (F.N.W., D.E.S.) rated the strength of the evidence according to the following factors: risk of bias, consistency of results, directness of evidence, precision and publication bias, and magnitude of effect.31,32 Any disagreement between the 2 reviewers was resolved with additional discussion.
RESULTS
Study selection
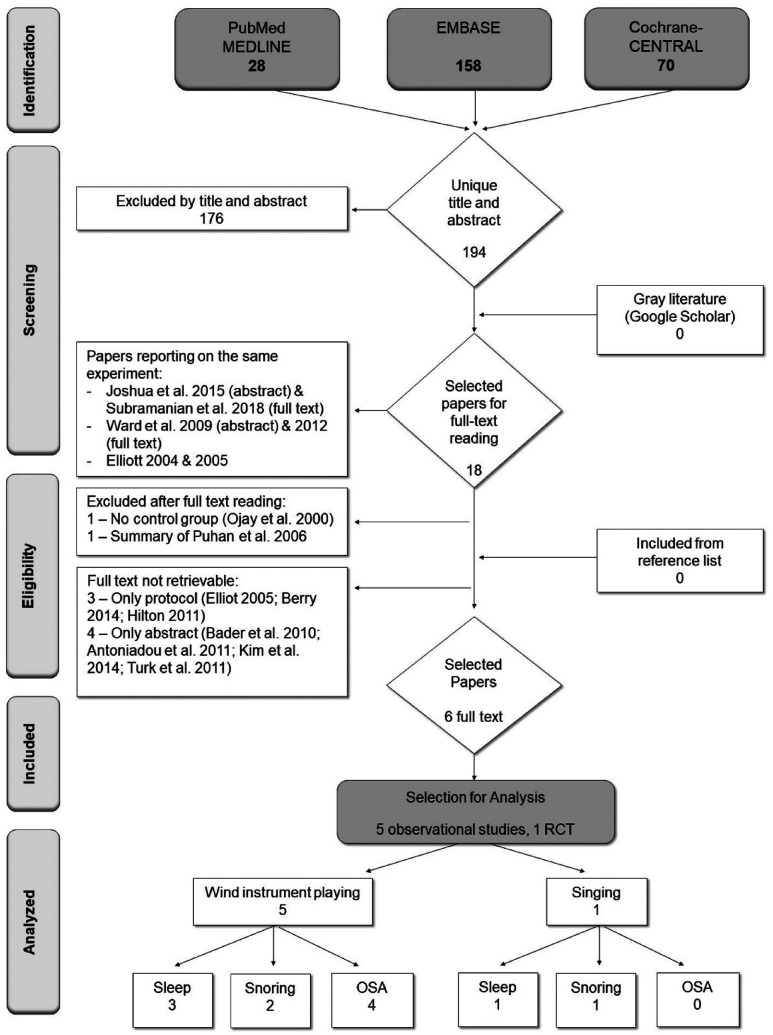
The search on PubMed-MEDLINE, EMBASE, and Cochrane-CENTRAL resulted in 194 unique papers (Figure 2). Screening of the titles and abstracts resulted in 18 potentially suitable papers, of which 3 experiments each had 2 publications. The full text of 7 papers was not retrievable: 3 were registered protocols and could not be retrieved as full manuscripts, and 4 were congress abstracts.33–36 For 8 papers, the full texts were obtained and read in full. Two studies were excluded. One had no control group,37 and the other was a summary of 1 of the included papers.38,39 Google Scholar and the reference lists of the selected full text papers yielded no additional suitable papers. Thus, in total, 6 papers (Figure 2) were included in the present systematic review.39–44
Figure 2. Flowchart of search and selection.
Study characteristics
The study characteristics of the 6 included papers are listed in Table 2. Five of the eligible papers had a cross-sectional study design, whereas one was an RCT. In the RCT, the intervention consisted of didgeridoo lessons. Three cross-sectional studies compared professional wind and nonwind instrument players, one study compared experienced (> 10 years) wind instrument players with participants who did not play a wind instrument and were not singers either, and one study compared singers with healthy volunteers. The sample sizes ranged from 25 to 1,105 participants. Three continents were represented (Europe, North America, Asia).
Table 2.
Study characteristics of the included papers.
| Study (Risk of Bias) | Study Design | Population (Country) | Participants | Conclusions of the Original Authors |
|---|---|---|---|---|
| Brown et al44 (Low) | Cross-sectional | Professional orchestra members registered by the International Conference of Symphony and Opera Musicians (ICSOM). (USA and Puerto Rico) | 369 wind instrument players: 175 brass players, 194 wood-wind instrument players, 233 men, 110 women, 26 missing sex, mean age 46.7 (12.26) years | Playing a wind instrument was not associated with a lower risk of OSA. |
| Internet-based questionnaire | 736 nonwind instrument players: 330 men, 360 women, 46 missing sex, mean age 46.8 (12.46) years | |||
| Pai et al42 (Moderate) | Cross-sectional | Singers from two London-based, mixed-sex choirs. The nonsinger group consisted of healthy volunteers also recruited in London. (United Kingdom) | 52 singers: 20 men, 32 women, mean age 46.3 (26–70) years | Singing practice may have a role in the treatment of snoring but does not appear to influence daytime somnolence. |
| Questionnaires | 55 healthy volunteers: 22 men, 32 women, mean age 43.3 (16–74) years | |||
| Puhan et al39 (Low) | RCT | Participants aged > 18 years with self-reported snoring and an AHI of 15–30 (determined by a specialist in sleep medicine within the past year). (Switzerland) | Intervention group: 12 men, 2 women, mean age 49.9 (6.7) years | Regular didgeridoo playing is an effective treatment alternative well accepted by patients with moderate OSA. |
| Didgeridoo lessons and practice at home (at least 20 minutes on at least 5 days a week) for 4 months | ||||
| Sleep recordings and questionnaires | Nonintervention group: 9 men, 3 women, mean age 47.0 (8.9) years | |||
| Single blinded (person who analyzed the sleep recordings) | ||||
| Subramanian et al43 (Serious) | Cross-sectional | Participants mainly from villages in and around Madurai who have been playing the instrument for nearly more than 10 years. (India) | 64 wind instrument players: 45 Nathasvaram (= double reed instrument), 10 trumpet (= brass instrument), 10 clarinet (= single reed instrument) | OSA risk is reduced in wind instrument players. |
| Questionnaire | 65 controls: participants who did not play any form of wind instrument and singers were also excluded | |||
| Ward et al40 (Moderate) | Cross-sectional | Collegiate instrumental music instructors and other professional musicians. (USA) | 76 double-reed instrument players: 27 men, 49 women, mean age 41.7 (14.5) years | Playing a double-reed musical instrument was associated with a lower risk of OSA. |
| 204 single reed instrument players: 110 men, 94 women, mean age 43.8 (13.6) years | ||||
| Online questionnaire or paper and pencil version | 124 high brass instrument players: 94 men, 30 women, mean age 42.0 (12.8) years | |||
| 122 low brass instrument players: 108 men, 13 women, mean age 44.0 (14.4) years | ||||
| 380 nonwind instrument players: 210 men, 170 women, mean age 42.7 (13.3) years | ||||
| Wardrop et al41 (Low) | Cross-sectional | Professional orchestra members. (United Kingdom) | 81 wind instrument players: mean age 41.58 (10.16) years | No significant difference between the snoring severity or daytime sleepiness of brass/wind players and other professional orchestral musicians. |
| 154 nonwind instrument players: mean age 43.56 (10.19) years | ||||
| Questionnaire undertaken during rehearsal | Significantly more male wind players than nonwind players |
Risk of bias within studies
To estimate the potential risk of bias, the methodological qualities of the included studies were assessed (Table S3 and Table S4). Overall, the potential risk of bias in the included studies was estimated to be “high” for 1,43 “moderate” for 2,39,42 and “low” for the remaining 3.39,41,44 In the studies that were judged to have a moderate risk of bias, the sample size was not justified and satisfactory. Besides that, in the study with an estimated potential high risk of bias, the study participants were not described in detail.
Descriptive analysis
Data extracted from the included studies are presented in Table 3, which provides a summary overview of sleep/snoring/OSA parameters between wind instrument players/singers and a control group. According to the results of 3 of the included studies,40,41,44 there seems generally to be no difference in sleep, snoring, and OSA between wind instrument players and controls. Two exceptions are double-reed instrument players, who are found to have a lower risk of OSA compared with controls,40,43 and didgeridoo players, who are found to have lower AHI, daytime sleepiness, and partners’ rating for sleep disturbance compared with controls.39 Singers are found to have a lower Snoring Scale Score (SSS) compared with controls,42 but no difference was found in daytime sleepiness.
Table 3.
Summary of significant differences between wind instrument players/singers and controls for sleep/snoring/OSA parameters.
| Study | Intervention | Sleep | Snoring | OSA | Comparison | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| PQS | ESS | PRSD | SOS | SSS | AHI | DO | BQ | |||
| Pai et al42 | Singers | 0 | - | Nonsingers | ||||||
| Wardrop et al41 | Wind instrument players | 0 | 0 | Nonwind instrument players | ||||||
| Subramanian et al43 | Wind instrument players (70% double reed) | - | Nonwind instrument players | |||||||
| Ward et al40 | Double-reed instrument players | 0 | 0 | - | Nonwind instrument players | |||||
| Ward et al40 | Single-reed and flute instrument players | 0 | 0 | 0 | Nonwind instrument players | |||||
| Brown et al44 | Woodwind* instrument players | 0 | 0 | Nonwind instrument players | ||||||
| Brown et al44 | Brass instrument players | 0 | 0 | Nonwind instrument players | ||||||
| Ward et al40 | High brass instrument players | 0 | 0 | 0 | Nonwind instrument players | |||||
| Ward et al40 | Low brass instrument players | 0 | 0 | 0 | Nonwind instrument players | |||||
| Brown et al44 | Wind instrument players using circular breathing | 0 | 0 | Nonwind instrument players | ||||||
| Puhan et al41 | Didgeridoo lessons | 0 | - | - | - | Waiting list | ||||
*Woodwind instrument players = double-reed + single-reed + flute. - = significantly lower for the wind instrument/singer group. 0 = no significant difference. Empty boxes indicate that no data are available. AHI = apnea-hypopnea index, BQ = Berlin Questionnaire (Risk of OSA), DO = diagnosis of OSA (by a physician), ESS = Epworth Sleepiness Score (daytime sleepiness), OSA = obstructive sleep apnea, PQS = Pittsburgh Quality of Sleep index, PRSD = Partner’s Rating for Sleep Disturbance, SOS = Snore Outcomes Survey score (snore severity), SSS = Snoring Scale Score.
Meta-analysis
A meta-analysis was feasible for the following outcome parameters: Epworth Sleepiness Scale (ESS), high risk of OSA (measured using the Berlin Questionnaire [BQ]), and diagnosis of OSA (by a physician). The following studies could be included in the meta-analysis: Brown et al,44 Puhan et al,39 Ward et al,40 Wardrop et al,41 and Subramanian et al43 (Table 4). Meta-analysis shows no difference in the ESS, high risk of OSA (BQ), or diagnosis of OSA (by a physician) between wind instrument players and controls, with a heterogeneity of 0%, except for high risk of OSA (I2 = 81%, P <.001).
Table 4.
Meta-analysis for Epworth Sleepiness Scale, high risk of OSA, diagnosis of OSA, and risk factors age, BMI, and male sex.
| Comparison | Included Studies | Outcome Parameters | DiffM | Risk Ratio | Test for Overall | Test for Heterogeneity | Forest Plot | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | P value | I2 | Tau2 | Chi2 | P value | Supplemental Material | |||||
| Wind instrument vs. control | Puhan et al39; Ward et al40 (4 subgroups); Wardrop et al41 | ESS | −0.16 | −0.65, 0.33 | .52 | 0% | 0 | 1.73 | .89 | Figure S1a | |
| BMI | 0.65 | −0.65, 1.91 | .32 | 80% | 1.92 | 24.54 | < .001* | Figure S1b | |||
| Age | 0.10 | −1.37, 1,57 | .90 | 0% | 0 | 4.70 | 0.45 | Figure S1c | |||
| Male sex | 1.14 | 0.90, 1.45 | .27 | 82% | 0.07 | 28.13 | < .001* | Figure S1d | |||
| Wind instrument vs. control | Brown et al44; Subramanian et al43; Ward et al40 (4 subgroups) | High risk of OSA (BQ) | 0.85 | 0.58, 1.24 | .39 | 81% | 0.17 | 26.71 | < .001* | Figure S2a | |
| Diagnosis of OSA (by a physician) | 1.26 | 0.85, 1.87 | .24 | 0% | 0 | 2.86 | .58 | Figure S2b | |||
| BMI | 0.94 | −0.37, 2.24 | .16 | 85% | 1.83 | 25.86 | < .001* | Figure S2c | |||
| Age | 0.06 | −1.11, 1.23 | .92 | 0% | 0 | 1.29 | .86 | Figure S2d | |||
| Male sex | 1.18 | 0.93, 1.49 | .18 | 87% | 0.06 | 30.27 | < .001* | Figure S2e | |||
*Statistically significant difference. BMI = body mass index, BQ = Berlin Questionnaire, CI = confidence interval, DiffM = difference of means, ESS = Epworth Sleepiness Scale.
Risk factors, heterogeneity, sensitivity analysis, and publication bias
A meta-analysis was also performed on the risk factors: age29, body mass index (BMI), and sex (Table 4). There was no significant difference in the means or risk ratio between wind instrument players and controls. BMI and male sex were factors that showed significant heterogeneity (I2 = 80–87%, P < .001).
The large heterogeneity for the high risk of OSA parameter (I2 = 81%, P <.001) is due to the fact that some studies/subgroups point in different directions (Figure S2a). The study by Brown et al44 showed higher risk of OSA among wind instrument players compared with controls, while the study by Subramanian et al43 showed the opposite. The double-reed instrument players subgroup in the study by Ward et al40 also showed a tendency for a lower risk of OSA compared with controls. These discrepancies correspond to the significant heterogeneity of the BMI and male sex risk factors. The wind instrument group in the study by Brown et al44 consisted of more males and a higher BMI compared with the control group (Figure S2, c and e). The double-reed instrument players subgroup in the study by Ward et al40 had more women and a lower BMI compared with the control group, whereas the high and low brass instrument players subgroups had more men and a higher BMI (Figure S1, b and d, Figure S2, c and e). In the study by Wardrop et al,41 the wind instrument group consisted of more men than the control group (Figure S1d).
For the sensitivity analysis (Table 5), studies/subgroups were removed if there was a significant difference between the test and control group for any of the risk factors. Consequently, for the ESS, 4 of the 6 studies/subgroups were excluded; only the study by Puhan et al39 and the subgroup of single-reed instrument and flute players from the study by Ward et al40 remained. A sensitivity analysis with these 2 groups also showed no significant difference in the ESS between wind instrument players and controls (I2 = 0%) (Figure S3a). The overall result was not affected by the sensitivity analysis, although it did have an effect on the statistical heterogeneity expressed by I2. The result for the ESS can be regarded with a higher degree of certainty. For high risk of OSA (BQ) and diagnosis of OSA (by a physician), 5 of the 6 studies/subgroups were excluded. Only the single-reed instrument and flute players subgroup from the study by Ward et al40 remained. As a result, the predefined minimum of 2 studies for a meta-analysis was not reached.
Table 5.
Sensitivity analysis for Epworth Sleepiness Scale and risk factors age, BMI, and male sex.
| Comparison | Included Studies | Outcome Parameter | DiffM | Risk Ratio | Test for Overall | Test for Heterogeneity | Forest Plot | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | P value | I2 | Chi2 | P value | Supplemental Material | |||||
| Wind instrument vs. control | Puhan et al39; Ward et al40 (only single-reed instrument and flute players) | ESS | −0.50 | −1.39, 0.39 | .27 | 0% | 0.84 | .36 | Figure S3a | |
| BMI | −0.10 | −1.19, 0.99 | .86 | 0% | 0.00 | 1.00 | Figure S3b | |||
| Age | 1.87 | −1.03, 4.77 | .21 | 0% | 0.13 | .72 | Figure S3c | |||
| Male sex | 0.99 | 0.82, 1.19 | .90 | 0% | 0.16 | .69 | Figure S3d | |||
BMI = body mass index, CI = confidence interval, DiffM = difference of means, ESS = Epworth Sleepiness Scale.
Testing for publication bias could not be performed, because fewer than 10 studies could be included in the meta-analysis.25
Rating the certainty of the evidence (GRADE)
Table 6 summarizes the various factors used to rate the strength of the evidence according to the criteria as proposed by the GRADE working group.31,32 Table S3 and Table S4 show that the estimated potential risk of bias is low to high. The data that emerged are rather consistent and rather precise; however, the generalizability is limited because of long (professional) rehearsal time or small sample size. Reporting bias could not be ruled out. The magnitude of the effect is zero to small. Consequently, the degree of certainty surrounding the effect is low.
Table 6.
| Determinants of Quality | Overall |
|---|---|
| Study design | Cross-sectional, RCT |
| Number of studies | 6 |
| Risk of bias | Low to high |
| Consistency | Rather consistent |
| Directness | Limited generalizability |
| Precision | Rather precise |
| Reporting bias | Cannot be ruled out |
| Magnitude of the effect | Zero to small |
| Strength of the propositions emerging from this review | Low |
| Overall recommendation | Considered advising patients who snore or have (risk of developing) obstructive sleep apnea to practice singing or to play the digeridoo or a double-reed instrument. However, the degree of certainty surrounding the expected effect is low. |
DISCUSSION
Answer to the focused question
This review was initiated to evaluate various aspects of sleep disturbance in oral musicians. The results of the descriptive analysis (Table 3) show that playing a double-reed instrument or didgeridoo as well as singing have a positive effect on sleep, snoring, and/or OSA. The descriptive analysis could not be substantiated by meta-analysis (Table 4 and Table 5), in which all wind instruments were pooled. The single study that evaluated the effect of singing (Table 3) showed a positive effect on snoring compared with nonsingers. The only RCT that evaluated the effect of playing a didgeridoo showed a positive effect on AHI, daytime sleepiness, and partner’s rating for sleep disturbance.
Risk factors
Well-known risk factors for snoring and OSA are ageing,45–47 excess body weight,46–50 and male sex.45–48,51 A systematic review found a prevalence of OSA (AHI ≥ 5 events/h) to be 9–38% and higher in men. It increased with age and, in some groups of older people, was as high as 90% in men and 78% in women. With an AHI ≥ 15 events/h, the prevalence in the general adult population ranged from 6 to 17%, and was as high as 49% in advanced ages. OSA prevalence was also greater in men and women with obesity.46
The meta-analysis showed a large heterogeneity for high risk of OSA, which can be explained by the heterogeneity for BMI and male sex between the study groups. The results of 2 included studies did not show a difference between wind instrument players and control participants (Table 3). These 2 studies, however, did confirm that age, BMI, and male sex were positively associated with snoring severity,41 a high risk of OSA,44 or physician’s diagnosis of OSA.44
Of the 4 studies that did show a positive effect of singing or playing the didgeridoo or a double-reed instrument, 3 studies adjusted outcomes for the risk factors of age, BMI, and sex distribution. In the study that showed that singers have a lower SSS compared with controls,42 the findings were adjusted for age and BMI. The sex ratio was comparable between the singer group (20:32, men to women) and nonsinger group (23:32, men to women). In the RCT in which didgeridoo players were found to have lower AHI, daytime sleepiness, and partners’ rating for sleep disturbance compared with controls, findings were adjusted for weight change during the study.39 In 1 of the 2 studies in which double-reed instrument players showed a lower risk of OSA, the double-reed group was majority women.40 However, the covariate-adjusted regression model indicated that the observed effect was not the result of sex distribution differences.40 The other study that found that wind instrument players (70% double-reed) had a lower risk of OSA did not report on the age, BMI, or sex of the participants.43 However, this was the only study taking into account smoking as a potential risk factor. There was a trend toward a higher number of smokers in the wind instrument group compared with the control group (P = .06). Whether smoking is a risk factor for OSA remains a matter of debate.52 A study containing 3,509 patients who were treated in a university hospital sleep clinic revealed that heavy smokers (> 30 pack-year) had almost twice the risk of having an AHI > 50 events/h compared with nonsmokers. However, after adjusting for age, BMI, and sex, this difference was no longer significant.53 On the other hand, a recent study of 660 participants observed that there is an increased risk of OSA in heavy smokers.54
Different types of wind instruments and circular breathing
Strayer,55 an orthodontist and professional bassoonist, established a classification of 4 groups of wind instrument players with different embouchure techniques: brass, single-reed, double-reed, and flute (Figure 1). In the included studies, the data were not analyzed in accordance with this classification. Wardrop et al41 considered all wind instrument players as one group and did not report on the different types of wind instruments. Subramanian et al43 examined players of three types of wind instruments (nadhaswaram, trumpet, and clarinet), but pooled them all together in their analysis. Brown et al made a distinction between woodwind and brass instrument players and also performed a subgroup analysis.44 However, that study did not consider different types of woodwind instruments. Ward et al40 distinguished between high brass, low brass, and double-reed instruments, but considered players of a single-reed instrument and flute as one group.
One wind instrument that cannot be assigned to any of the 4 groups defined by Strayer is the didgeridoo, an instrument developed by Indigenous Australians. Playing the didgeridoo requires the use of circular breathing. This is a technique used to produce a continuous tone without break, achieved by using the cheeks as a reservoir of air that is expelled to continue the note while the player breathes in through the nose.39,41,44 The results of one of the included studies suggest that practicing the didgeridoo/circular breathing may train airway muscles, leading to less collapse of oropharyngeal tissues during sleep, which results in a beneficial effect on OSA.39 However, another included study compared players of wind instrument who used circular breathing with all other wind instrument players. The use of circular breathing was not found to be related to either the risk of OSA or OSA diagnosis.44 One explanation might be that didgeridoo players use the technique much more consistently and thus may achieve a greater level of oropharyngeal muscle training.
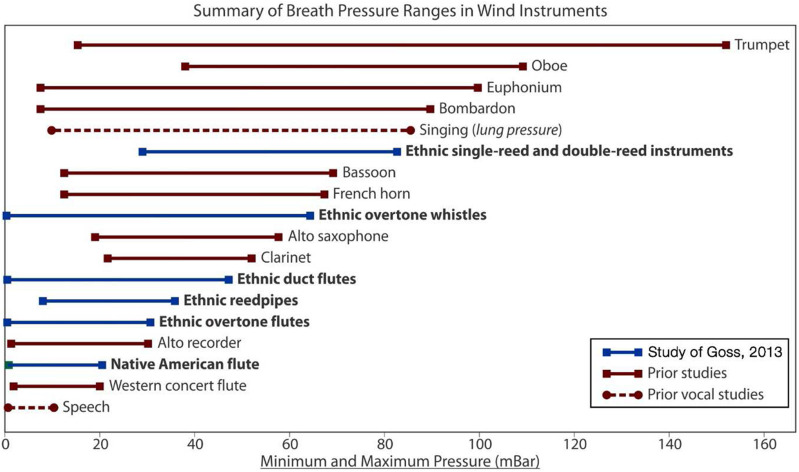
Players of double-reed instruments are found to have a lower risk of OSA compared with controls,40,43 although no such association was found for the other groups of wind instruments. The mechanism behind this selective difference might be the different types of embouchure, i.e., different patterns of muscle activation used in various types of orchestral wind instruments (Figure 1). Another explanation might be the difference in air pressure required to make a sound. Goss56 provided an overview of intraoral pressure ranges in wind instruments and subglottal pressure of singing based on his own data and a survey of the literature (Figure 3). At the top is the trumpet (maximum of 150 mbar), followed by the oboe (110 mbar), euphonium (100 mbar), singing (85 mbar), bassoon and French horn (70 mbar), saxophone (55 mbar), clarinet (50 mbar), and flute (20 mbar). This clearly marks that brass and double-reed instruments (in particular the trumpet and oboe), together with singing, are associated with the highest maximum pressures. This could also explain the association between singing and a lower SSS.42 The included studies, however, do not show an association between brass instrument playing and lower risk of OSA, whereas such an association was observed for double-reed instruments. This could be explained by the fact that oboe players need to generate higher minimum pressure to start a note than brass players (Figure 3).
Figure 3. Overview of intraoral pressure ranges in wind instruments and subglottal pressure of singing.
Reprinted with permission from the author.56
Compliance and practice time
Playing a wind instrument or singing to train the oropharyngeal musculature is an attractive approach to reducing OSA, because these recreational activities are potentially enjoyable in their own right.41 However, these treatments are not effective unless they are practiced consistently.40 In one of the studies analyzed for the present review, participants had to practice the didgeridoo at home for at least 20 minutes at least 5 days a week.39 This might be an achievable schedule. Conventional orchestral instruments might have greater appeal and relevance to western patients.41 However, another study showed that among double-reed instrument players, the number of hours per week the instrumentalist played was a significant predictor of the level of OSA risk. Double-reed instrumentalists at low risk for OSA played on average 16.5 hours per week, while those at a higher risk played on average 9.1 hours per week.40 Practicing 16.5 hours per week is likely far too much for amateur musicians with OSA. Additionally, proper double-reed instrument playing is not something that can be learned easily.40 Singing, however, might be very accessible. In a third study included in this review, semiprofessional singers were included, all of whom had received formal training in singing. The fewest number of years of choir singing was 5.42 The question is whether amateur singing has the same positive effect as semiprofessional singing.
Comparison with studies not included in this systematic review
One study was excluded from this systematic review because of the lack of a control group.37 In that study, 20 people who were chronic snorers received instruction in singing technique and singing exercises that they were instructed to practice for 20 minutes a day for 3 months. The duration of snoring was recorded by a voice-activated tape recorder for 7 nights, both before and after treatment. Snoring was, on average, reduced, especially in those who performed the exercises accurately and consistently, were not overweight, had no nasal problems, and began snoring only in middle age.
Four potentially interesting paper titles were identified in the initial search, but only the abstracts for these papers were retrievable.33–36 In the study by Turk et al,36 10 patients with OSA received didgeridoo lessons and practiced for 4 months. Strong associations were found between didgeridoo playing and a decrease in AHI (polysomnography) and in volume of parapharyngeal fat pads. Only a moderate association was found with decrease in daytime sleepiness. This in itself is not surprising because clinical symptoms such as daytime sleepiness correlate poorly with OSA severity as measured by AHI.57,58 In the study by Kim et al,35 19 Korean patients with OSA received didgeridoo lessons and practiced for 16 weeks. A significant improvement in snoring was found, but not in the AHI index. Bader et al33 collected completed questionnaires of 213 professional and 318 amateur musicians, of which 50% were singers, 34% wind instrument players, and 16% controls. A marked difference between sexes, but no significant difference between the groups, was found for SSS, ESS, and score and diagnosis of OSA. Antoniadou et al34 observed a low risk of OSA (BQ) among 25 players of wind instruments and 5 singers; however there was no control group in this study. The findings reported in these abstracts are comparable with the results of the studies included in the present systematic review.
Limitations
Following the search and selection, only 1 RCT could be included.39 This was the only study that provided direct data on the sleep of the participants. However, this study also contributed to clinical and methodological heterogeneity, which may negatively impact the representativeness of the results.
Because of the cross-sectional design of 4 of the 5 studies included in this review, conclusions were drawn on associations and not on causal relationships. Furthermore, the results of these 4 studies are based on questionnaires. Therefore, OSA was not diagnosed according to the gold standard, polysomnography. However, all studies used validated scales. The response rate varied per study from 10–30% by email to up to 70–90% by direct solicitation.40,41,44 Respondents may have been more likely than nonrespondents to be interested in OSA or snoring.
While the sample sizes of the studies by Brown et al44 (n = 1,105) and Ward et al40 (n = 906) are large, the sample size of the study by Puhan et al39 is very small (n = 25). Consequently, this small sample size may have a negative impact on generalizability and on study power.
The control group of the RCT performed by Puhan et al39 was generated randomly with stratification from OSA severity. The cross-sectional study among singers had a control group consisting of healthy volunteers.42 This is less than ideal compared with a control group consisting of nonwind instrument players (i.e., string, percussion, keyboard), which was used in the 3 cross-sectional studies among orchestra members.40,41,44 Fellow orchestral musicians are likely to have similar lifestyles and work patterns to the participants, which should therefore reduce the effect of any confounding variables. Subramanian et al43 did not specify the background characteristics of their control group. However, this was the only study examining players of wind instrument that properly excluded singers in the control group.
The study by Puhan et al39 showed a clinically significant improvement in ESS score (mean change score in the didgeridoo group was 4.4 and the difference between the intervention and control groups was 3.0). In the study by Pai et al,42 however, SSS values were low in both the singer and nonsinger groups, and it is possible that many participants in this study were unlikely to have problems with snoring anyway. Although there is a statistically significant difference between the 2 groups in SSS values (singers 2.5 vs. nonsingers 3.6 on a scale of 0 to 9), the magnitude of this difference is small, and it is not possible to determine whether or not it is clinically relevant. The Snore Outcomes Survey Score and ESS scores in the study by Wardrop et al41 and the ESS scores in the study by Ward et al40 were also low for all groups.
Didgeridoo playing appeared to be the most promising musical intervention for positively affecting sleep-breathing disorders. A survey among patients with OSA demonstrated that two-thirds of respondents expressed interest in participating in a didgeridoo program.59 More and larger studies are needed to assess the generalizability, long-term compliance, and implementation of didgeridoo playing as alternative for current OSA treatments.
CONCLUSIONS
Playing a wind instrument and singing may have a positive but small effect on sleep disorders. Considering the practicality and investment of (rehearsal) time, didgeridoo and singing are the most promising interventions to reduce OSA and snoring, respectively. However, the results of this review are based on few studies and the synthesis of the evidence is graded to have low certainty.
DISCLOSURE STATEMENT
All authors gave their final approval and agreed to be held accountable for all aspects of the work, ensuring integrity and accuracy. The authors report no conflicts of interest.
SUPPLEMENTARY MATERIAL
ACKNOWLEDGMENTS
The authors gratefully acknowledge Alexander Verhelst (dentist, periodontist, and accredited OSA specialist) for help while preparing the manuscript and the following authors for their response, time, and effort to search for additional data: Dr. P.J.C. Wardrop, Dr. D.L. Brown, and Dr. Irumee Pai. The authors are also grateful to Clint Goss for granting permission to reuse his figure and providing us with a high-quality version and to Stephen Hancocks, editor-in-chief of the British Dental Journal, for granting permission to reuse the figures of Porter.26
F.N.W. contributed to conception and design, search and selection, analysis and interpretation, and drafted the manuscript. F.L. contributed to interpretation and critically revised the manuscript. D.E.S. contributed to conception and design, selection, analysis and interpretation, and critical revision of the manuscript.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- BQ
Berlin Questionnaire
- ESS
Epworth Sleepiness Score
- GRADE
Grading of Recommendations Assessment, Development and Evaluation
- OSA
obstructive sleep apnea
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
Randomized Controlled Trial
- SSS
Snoring Scale Score
REFERENCES
- 1.Aminoff MJ, Boller F, Swaab DF. We spend about one-third of our life either sleeping or attempting to do so. Handb Clin Neurol. 2011;98:vii. 10.1016/B978-0-444-52006-7.00047-2 [DOI] [PubMed] [Google Scholar]
- 2.White DP. Sleep-related breathing disorder. 2. Pathophysiology of obstructive sleep apnoea. Thorax. 1995;50(7):797–804. 10.1136/thx.50.7.797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stuck BA, Dreher A, Heiser C, et al. Diagnosis and treatment of snoring in adults-S2k Guideline of the German Society of Otorhinolaryngology, Head and Neck Surgery. Sleep Breath. 2015;19(1):135–148. 10.1007/s11325-014-0979-8 [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Sleep Medicine (AASM). Obstructive Sleep Apnea. 2008 Available at: https://aasm.org/resources/factsheets/sleepapnea.pdf Accessed Aug 6, 2019.
- 5.Filtness AJ, Reyner LA, Horne JA. One night’s CPAP withdrawal in otherwise compliant OSA patients: marked driving impairment but good awareness of increased sleepiness. Sleep Breath. 2012;16(3):865–871. 10.1007/s11325-011-0588-8 [DOI] [PubMed] [Google Scholar]
- 6.Nena E, Steiropoulos P, Constantinidis TC, Perantoni E, Tsara V. Work productivity in obstructive sleep apnea patients. J Occup Environ Med. 2010;52(6):622–625. 10.1097/JOM.0b013e3181e12b05 [DOI] [PubMed] [Google Scholar]
- 7.Omachi TA, Claman DM, Blanc PD, Eisner MD. Obstructive sleep apnea: a risk factor for work disability. Sleep. 2009;32(6):791–798. 10.1093/sleep/32.6.791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378–1384. 10.1056/NEJM200005113421901 [DOI] [PubMed] [Google Scholar]
- 9.Peker Y, Hedner J, Norum J, Kraiczi H, Carlson J. Increased incidence of cardiovascular disease in middle-aged men with obstructive sleep apnea: a 7-year follow-up. Am J Respir Crit Care Med. 2002;166(2):159–165. 10.1164/rccm.2105124 [DOI] [PubMed] [Google Scholar]
- 10.Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122(4):352–360. 10.1161/CIRCULATIONAHA.109.901801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garcia-Rio F, Alonso-Fernández A, Armada E, et al. CPAP effect on recurrent episodes in patients with sleep apnea and myocardial infarction. Int J Cardiol. 2013;168(2):1328–1335. 10.1016/j.ijcard.2012.12.015 [DOI] [PubMed] [Google Scholar]
- 12. Vos PJE, Machiels HA, Pevernagie DAA, et al. Obstructief slaapapneu (OSA) bij volwassenen. 2018. Available at: https://richtlijnendatabase.nl/richtlijn/osa_bij_volwassenen/startpagina_-_obstructief_slaapapneu_osa.html Accessed Aug 6, 2019.
- 13.Camacho M, Certal V, Abdullatif J, Zaghi S, Ruoff CM, Capasso R, Kushida CA. Myofunctional therapy to treat obstructive sleep apnea: a systematic review and meta-analysis. Sleep. 2015;38(5):669–675. 10.5665/sleep.4652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guimarães KC, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filho G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2009;179(10):962–966. 10.1164/rccm.200806-981OC [DOI] [PubMed] [Google Scholar]
- 15.Camacho M, Guilleminault C, Wei JM, et al. Oropharyngeal and tongue exercises (myofunctional therapy) for snoring: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2018;275(4):849–855. 10.1007/s00405-017-4848-5 [DOI] [PubMed] [Google Scholar]
- 16.Berkhout FRU. The dentition is part of the instrument. Ned Tandartsenbl. 2016;2:16–19. [Google Scholar]
- 17.Porter MM. Dental aspects of orchestral wind instrument playing with special reference to the embouchure. Br Dent J. 1952;93:66–73. [Google Scholar]
- 18.Lovetri J, Lesh S, Woo P. Preliminary study on the ability of trained singers to control the intrinsic and extrinsic laryngeal musculature. J Voice. 1999;13(2):219–226. 10.1016/S0892-1997(99)80024-1 [DOI] [PubMed] [Google Scholar]
- 19. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses. 2009. Available at: http://www.prisma-statement.org/ Accessed Dec 20, 2019.
- 20.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 21.Beller EM, Glasziou PP, Altman DG, et al.; PRISMA for Abstracts Group . PRISMA for Abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med. 2013;10(4):e1001419. 10.1371/journal.pmed.1001419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amir-Behghadami M, Janati A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. 2020;37(6):387. [DOI] [PubMed] [Google Scholar]
- 23. Haponiuk B. Confidence Interval Calculator. Available at: https://www.omnicalculator.com/statistics/confidence-interval Accessed May 28, 2019.
- 24.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 25.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Porter MM. Dental problems in wind instrument playing. 1. Dental aspects of embouchure. Br Dent J. 1967;123:393–396. [PubMed] [Google Scholar]
- 27.Yeo DK, Pham TP, Baker J, Porters SA. Specific orofacial problems experienced by musicians. Aust Dent J. 2002;47(1):2–11. 10.1111/j.1834-7819.2002.tb00296.x [DOI] [PubMed] [Google Scholar]
- 28.van der Weijden FN, Kuitert RB, Berkhout FRU, van der Weijden GA. Influence of tooth position on wind instrumentalists’ performance and embouchure comfort: A systematic review. J Orofac Orthop. 2018;79(3):205–218. 10.1007/s00056-018-0128-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van der Weijden F, Dell’Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol. 2009;36(12):1048–1058. 10.1111/j.1600-051X.2009.01482.x [DOI] [PubMed] [Google Scholar]
- 30. Ryan R; Cochrane Consumers and Communication Review Group. Heterogeneity and subgroup analyses in Cochrane Consumers and Communication Group reviews: planning the analysis at protocol stage. 2016 Available at: https://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/public/uploads/heterogeneity_subgroup_analyses_revising_december_1st_2016.pdf Accessed Jun 10, 2019.
- 31. The GRADE working group. Grading of recommendations assessment, development and evaluation. 2000. Available at: https://www.gradeworkinggroup.org/ Accessed Jun 17, 2019.
- 32.Guyatt GH, Oxman AD, Kunz R, et al.; GRADE Working Group . Incorporating considerations of resources use into grading recommendations. BMJ. 2008;336(7654):1170–1173. 10.1136/bmj.39504.506319.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bader G, Bodden A, Ullrich H. Does singing or playing a wind instrument have any impact on snoring or OSA? Eur Sleep Res Soc. 2010;19(Suppl. 2):233. [Google Scholar]
- 34.Antoniadou M, Michailidis V, Perantoni E, Chloros D, Prinza A, Gegas T, Tsara V. Respiratory symptoms and risk for obstructive sleep apnea in professional musicians. Eur Respir J. 2011;38(Suppl.55):2279. [Google Scholar]
- 35.Kim D, Kim JH, Cho YJ, Seo JG, Kim H, Hong SB. Didgeridoo therapy for Korean patients with obstructive sleep apnea. Eur Sleep Res Soc. 2014;23(Suppl. 1):195. [Google Scholar]
- 36.Turk A, Zuercher A, Zahn F, Frauenfelder T, Puhan M. Didgeridoo may lower apnea hypopnea index through reducing parapharyngeal fat pads. Eur Respir J. 2011;38(Suppl. 55):4954. [Google Scholar]
- 37.Ojay A, Ernst E. Can singing exercises reduce snoring? A pilot study. Complement Ther Med. 2000;8(3):151–156. 10.1054/ctim.2000.0376 [DOI] [PubMed] [Google Scholar]
- 38.Möllers MM, Spronk PE. Didgeridoo playing is moderately effective in patients with sleep apnea syndrome. Ned Tijdschr Geneeskd. 2006;150(33):1856. [Google Scholar]
- 39.Puhan MA, Suarez A, Lo Cascio C, Zahn A, Heitz M, Braendli O. Didgeridoo playing as alternative treatment for obstructive sleep apnoea syndrome: randomised controlled trial. BMJ. 2006;332(7536):266–270. 10.1136/bmj.38705.470590.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ward CP, York KM, McCoy JG. Risk of obstructive sleep apnea lower in double reed wind musicians. J Clin Sleep Med. 2012;8(3):251–255. 10.5664/jcsm.1906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wardrop PJ, Ravichandran S, Hair M, Robertson SM, Sword D. Do wind and brass players snore less? A cross-sectional study of snoring and daytime fatigue in professional orchestral musicians. Clin Otolaryngol. 2011;36(2):134–138. 10.1111/j.1749-4486.2011.02297.x [DOI] [PubMed] [Google Scholar]
- 42.Pai I, Lo S, Wolf D, Kajieker A. The effect of singing on snoring and daytime somnolence. Sleep Breath. 2008;12(3):265–268. 10.1007/s11325-007-0159-1 [DOI] [PubMed] [Google Scholar]
- 43.Subramanian RK, Saikumar P, Joshua SD, Devaki PR, Jagadeesh Marthandam L. Estimation of lung functions and risk of developing obstructive sleep apnoea in wind instrument players. Indian J Physiol. Pharmacol. 2018;62(1):59–65. [Google Scholar]
- 44.Brown DL, Zahuranec DB, Majersik JJ, Wren PA, Gruis KL, Zupancic M, Lisabeth LD. Risk of sleep apnea in orchestra members. Sleep Med. 2009;10(6):657–660. 10.1016/j.sleep.2008.05.013 [DOI] [PubMed] [Google Scholar]
- 45.Wali SO, Abaalkhail BA. Prevalence and predictors of habitual snoring in a sample of Saudi middle-aged adults. Saudi Med J. 2015;36(8):920–927. 10.15537/smj.2015.8.11848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev. 2017;34:70–81. 10.1016/j.smrv.2016.07.002 [DOI] [PubMed] [Google Scholar]
- 47.Young T, Shahar E, Nieto FJ, et al.; Sleep Heart Health Study Research Group . Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med. 2002;162(8):893–900. 10.1001/archinte.162.8.893 [DOI] [PubMed] [Google Scholar]
- 48.Knuiman M, James A, Divitini M, Bartholomew H. Longitudinal study of risk factors for habitual snoring in a general adult population: the Busselton Health Study. Chest. 2006;130(6):1779–1783. 10.1378/chest.130.6.1779 [DOI] [PubMed] [Google Scholar]
- 49.Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015–3021. 10.1001/jama.284.23.3015 [DOI] [PubMed] [Google Scholar]
- 50.Joosten SA, Hamilton GS, Naughton MT. Impact of weight loss management in OSA. Chest. 2017;152(1):194–203. 10.1016/j.chest.2017.01.027 [DOI] [PubMed] [Google Scholar]
- 51.Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310–318. 10.1016/S2213-2600(15)00043-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Deleanu OC, Pocora D, Mihălcuţă S, Ulmeanu R, Zaharie AM, Mihălţan FD. Influence of smoking on sleep and obstructive sleep apnea syndrome. Pneumologia. 2016;65(1):28–35. [PubMed] [Google Scholar]
- 53.Hoflstein V. Relationship between smoking and sleep apnea in clinic population. Sleep. 2002;25(5):519–524. 10.1093/sleep/25.5.517 [DOI] [PubMed] [Google Scholar]
- 54.Zhu HM, Yi HL, Guan J, et al. Relationship between smoking and the severity of OSA. 2019;33(9):862-865;869. [DOI] [PubMed] [Google Scholar]
- 55.Strayer ER. Musical instruments as an aid in the treatment of muscle defects and perversions. Angle Orthod. 1939;9:18–27. [Google Scholar]
- 56. Goss C. Intraoral pressure in ethnic wind instruments. 2013 Available at: http://www.Flutopedia.com/breath_pressure.htm Accessed Jun 10, 2019.
- 57.Arnardottir ES, Bjornsdottir E, Olafsdottir KA, Benediktsdottir B, Gislason T. Obstructive sleep apnoea in the general population: highly prevalent but minimal symptoms. Eur Respir J. 2016;47(1):194–202. 10.1183/13993003.01148-2015 [DOI] [PubMed] [Google Scholar]
- 58.Crinion SJ, Ryan S, McNicholas WT. Obstructive sleep apnoea as a cause of nocturnal nondipping blood pressure: recent evidence regarding clinical importance and underlying mechanisms. Eur Respir J. 2017;49(1):1601818. 10.1183/13993003.01818-2016 [DOI] [PubMed] [Google Scholar]
- 59.Petro A, Dzierzewski JM, Martin JL, et al. A survey to assess patients’ interest in the didgeridoo as an alternative therapy for obstructive sleep apnea. Sleep. 2017;40(Suppl. 1):A213. 10.1093/sleepj/zsx050.572 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.