Abstract
Study Objectives:
Attendance to sleep clinic appointments is imperative to diagnose sleep-related disorders and to offer appropriate treatment. As part of our quality assurance program, we assessed predictors of no-show rates at our sleep clinic. We hypothesize that no-show rates can be predicted by demographics, appointment type (new vs established) and timing, and insurance status.
Methods:
We performed a 10-month, retrospective chart review of patients scheduled at Saint Louis University’s SLUCare Sleep Disorders Center. Multivariable logistic regression was used to determine which factors were independently associated with no-show.
Results:
A total of 2,532 clinical visits were reviewed, and the overall no-show rate was 21.2%. Factors associated with a higher incidence of no-show rates included younger age (17–40 years: 21.5%; 41–64 years: 23.5%; ≥65 years: 14.0%; P < .0001), appointment type (new: 30.5% vs established: 18.3%; P < .0001), and insurance status (no insurance: 24.6% vs public: 22.6% vs private: 15.9%; P < .0001). Multivariable logistic regression confirmed the independent association between no-show and age ≤ 40 years (adjusted odds ratio = 1.72; 95% confidence interval: 1.44, 2.20), new patient status (adjusted odds ratio = 1.78; 95% confidence interval: 1.44, 2.20), and absence of health insurance (adjusted odds ratio = 1.62; 95% confidence interval: 1.24, 2.11). Sex, appointment time, day of the week, and season did not significantly influence no-show rates.
Conclusions:
Independent predictors of no-show appointments included younger age, new patient status, and lack of health insurance. Our findings will aid future efforts to identify patients with high predictors of nonadherence. Further studies are needed to develop methods to decrease no-show rates once high-risk appointments have been identified.
Citation:
Cheung DL, Sahrmann J, Nzewuihe A, Espiritu JR. No-show rates to a sleep clinic: drivers and determinants. J Clin Sleep Med. 2020;16(9):1517–1521.
Keywords: no-show, sleep clinic, determinant, retrospective, sleep disorder, appointments
BRIEF SUMMARY
Current Knowledge/Study Rationale: Approximately 50–70 million Americans have chronic sleep or wakefulness disorders, leading to impairments in daily activities and increased risk for obesity, heart diseases, depression, and type 2 diabetes. However, to treat patients and provide resources for sleep, it is imperative that they are present at their appointments.
Study Impact: The goal of this study was to highlight possible driving and determining factors of no-show rates in sleep clinics. In doing so, clinics can use the data to implement new initiatives that can decrease no-show rates in their clinics.
INTRODUCTION
Approximately 50–70 million Americans have chronic sleep or wakefulness disorders, leading to impairments in daily activities and increased risk for obesity, heart diseases, depression, and type 2 diabetes.1 The prevalence, incidence, treatment, predictors, pathophysiology, and outcomes of sleep and wakefulness disorders are well known. However, to treat patients and provide resources for sleep, it is imperative that they are present at their appointments. Although an important aspect of care, research of no-show rates among sleep clinics is limited.
From a financial standpoint, no-show rates increase the cost of health care. A study looking at 10 regional hospitals found an average no-show rate to be 18.8%, with larger rates occurring at subspecialty clinics.2 This equated to a cost of about $196 per patient in 2008.2 As part of quality assurance and improvement, evaluating no-show rates can maximize the access to care and reduce the cost of health care.
Previous studies that focused on predictors of no-show rates evaluated a variety of factors. A prospective study from a pain treatment center at John Hopkins Hospital by Odonkor et al3 revealed higher no-show rates among racial and ethnic minorities, among people younger than age 65, among people on Medicare or Medicaid, during snowy or rainy days, among those with lower back pain or headaches, and those that had at least one previous pain provider. Although this study offers general factors to no-show rates at a subspecialty clinic, the study is limited in that it obtained data from a 68% minority population within an inner city and does not include variables such as marital status, employment, insurance, opioid use, or location of residence.3 In a similar prospective study at a breast clinic in Phoenix, Arizona, Knolhoff et al4 found that patients with limited health literacy and who are current smokers had higher rates of no-show. The study, however, is limited in that their population was 98.2% female and widely diverse in sociodemographic characteristics such as race, language, education, employment, and insurance.4 In a retrospective study at a safety-net gastroenterology endoscopy suite at the University of Florida, Jacksonville, Shuja et al5 found predictors of higher no-show rates in unpartnered or single patients, African Americans, and those with noncommercial insurance providers. In contrast, they found a lower no-show rate in patients requiring surveillance colonoscopy vs initial screening.5 The study was limited, however, in that they never factored in level of education, symptom acuity, history of psychiatric illness or substance abuse, and differences between clinic-driven cancellations and patient-driven cancellations.5 Studies also focused on the provider’s side of scheduling appointments. At a pulmonary and gastroenterology clinic in Phoenix Children’s Hospital, Drewek et al6 found that appointments scheduled later than 30 days had a higher chance of no-show compared with appointments earlier than 30 days.
Based on the literature, there is a wide variety of factors that can lead to no-show rates in subspecialty clinics, but none looked at the attendance to sleep clinics specifically. In this study, we hypothesize that certain demographic characteristics, the appointment type and time, and health insurance coverage may be associated with higher no-show rates. To address the predictors of no-show rates at a sleep disorders clinic, we assessed the effect of sex, age, type and time of appointment, day of the week, season of the year, and type of insurance. The purpose of this study is to identify the factors associated with higher no-show rates at a sleep clinic as part of quality assurance and improvement. By addressing the factors that may predict patient no-show, we hope that sleep clinics could optimize their scheduling practices and be proactive about patients that suggest high risk for missed appointments to ensure quality of care.
METHODS
Our study was reviewed and approved by the Saint Louis University Institutional Review Board on December 11, 2018. The need for informed consent was waived because the project does not constitute Human Subjects Research.
This study was conducted at the SLUCare Sleep Disorders Center at Saint Louis University in St. Louis, MO. The SLUCare Sleep Disorders Center is a multidisciplinary academic sleep facility accredited by the American Academy of Sleep Medicine. The vast majority (80%) of patients were referred by their primary care providers for suspected sleep-related breathing disorders.
We performed a retrospective study over the course of 10 months between the months of July 2017 to April 2018. The study collected a limited deidentified dataset from all patients with a scheduled appointment at the sleep center. All patients who were scheduled for the clinic were included in the study with no exclusions. Data on a total of 2,532 patients were screened from the electronic health record system Epic (Epic System Corporation Released 2019, Epic Systems Corporation, Verona, WI). No patients were contacted for the purposes of this study.
The independent variables collected included the patient’s sex (male or female), age category (17–40, 41–64, ≥65 years), status of the appointment (new vs established clinic visit), time of appointment (AM or PM), day of the week of the appointment (Monday through Friday), season of the year of the appointment (July/Summer, October/Fall, January/Winter, or April/Spring), and health insurance coverage (none, public, or private). Data on clinic visits were collected during the months of July 2018, October 2018, January 2019, and April 2019 to represent each distinct season.
The dependent variable for our analysis was whether the appointment status was completed (show) or missed (no-show). The appointment was completed if the patient arrived at the clinic for their scheduled clinic visit. The appointment was deemed no-show either if the patient failed to show up at their scheduled appointment on time or canceled their appointment. To enhance patient show rates, automated reminder calls were made 7 days before the appointment, but no response was required from the patients. In addition, our practice also mandates the medical assistants to call patients by telephone the day before and the day of the appointment, respectively, to confirm their attendance.
Statistical analysis
χ2 bivariate analyses were conducted to determine the crude association between the independent variables and the outcome (show vs no-show). A multivariate binary logistic regression model was fitted to determine whether the significant independent variables, determined from the univariate analyses, were associated with the outcome (show vs no-show). SPSS (IBM Corp. Released 2015, IBM SPSS for Windows, Version 22.0, Armonk, NY) was used for statistical analysis.
RESULTS
Our study identified 2,532 patients, with an overall no-show rate of 21.20% for the months of July, October, January, and April. This was comparable to the overall no-show rate of 20%, if all the months between July and April were included. Of all the determinants of no-show, only age, status of appointment (new vs established), and type of insurance played a role in determining whether a patient would show up to their appointment or not. In terms of demographic characteristics, age category (P < .0001) but not sex (P = .351) was significantly associated with no-show rates. Patients ≥65 years were less likely to miss their clinic appointment, with a significantly lower no-show rate (14%) compared with those 17–40 years of age (21.5%) or those 41–64 years of age (23.5%) (Table 1, Figure 1). For status of appointment, new patients who had never been to the clinic had a significantly higher no-show rate than people who returned for a subsequent clinic visit (P < .0001). Over the course of the 10-month study, 187 of 613 (30.5%) new patients failed to attend their appointments compared with 351 of 1,919 (18.3%) established patients who had previously received care at the clinic (Table 1, Figure 1). In terms of health care coverage, patients without health insurance had significantly higher no-show rates than those with either public or private health insurance (P < .0001). Over the course of the 10-month study, 255 of 1,036 (24.6%) of people with no insurance did not show up to their appointment compared with the 130 of 822 patients (15.8%) with private health insurance and the 152 of 674 (22.6%) with public health insurance (Table 1). Other aspects of the appointment, such as sex (P = .351), day of the week (P = .375), time of day (P = .737), and season of the appointment (P = .106), were not associated with appointment attendance (Table 1). Multivariable binary logistic regression analysis incorporating the significant univariate independent variables (age category, type of appointment, and health insurance coverage), confirmed that a younger age category (17–40 years), new clinic visit, and lack of health insurance were independently associated with no-show (Table 2). In terms of age, the adjusted analysis showed patients 17–40 years of age were 1.72 (95% confidence interval: 1.23, 2.40) times more likely to miss their clinic appointment than those ≥65 years of age (Table 2). In contrast, those 41–64 years of age had similar clinic attendance as those ≥65 years (Table 2). A new patient was 1.78 (95% confidence interval: 1.44, 2.20) times more likely not to show up for an initial clinic visit than an established patient coming in for a subsequent clinic visit. Patients without health insurance were 1.62 (95% confidence interval: 1.24, 2.11) times more likely to not show up for a clinic visit than those with private or public health insurance.
Table 1.
Clinical attendance based on demographic characteristics, status of clinic visit, type of health care coverage, and temporal characteristics of appointment.
| Variable | No-Show, n (%) | Show, n (%) | P |
|---|---|---|---|
| Age (yr) | <.0001 | ||
| 17–40 | 137 (21.5) | 501 (78.5) | |
| 41–64 | 334 (23.5) | 1,089 (76.5) | |
| ≥65 | 66 (14.0) | 405 (86.0) | |
| Sex | .351 | ||
| Female | 309 (21.9) | 1,103 (78.1) | |
| Male | 228 (20.4) | 892 (79.6 | |
| Status | <.0001 | ||
| Established clinic visit | 351 (18.3) | 1,568 (81.7) | |
| New clinic visit | 187 (30.5) | 426 (69.5) | |
| Insurance | <.0001 | ||
| Public | 152 (22.6) | 521 (77.4) | |
| Private | 130 (15.9) | 689 (84.1) | |
| None | 255 (24.6) | 781 (75.3) | |
| Day | .276 | ||
| Monday | 134 (22.0) | 476 (78.0) | |
| Tuesday | 134 (24.2) | 419 (75.8) | |
| Wednesday | 115 (20.1) | 456 (79.9) | |
| Thursday | 90 (19.1) | 380 (80.9) | |
| Friday | 54 (20.6) | 208 (79.4) | |
| Time | .737 | ||
| AM | 214 (21.8) | 767 (78.2) | |
| PM | 323 (20.8) | 1,228 (79.2) | |
| Season | .442 | ||
| Summer | 129 (19.3) | 540 (80.7) | |
| Fall | 129 (20.9) | 489 (79.1) | |
| Winter | 144 (22.1) | 508 (77.9) | |
| Spring | 135 (22.8) | 458 (77.2) |
Figure 1. Appointment attendance based on appointment type, age category, and health insurance.
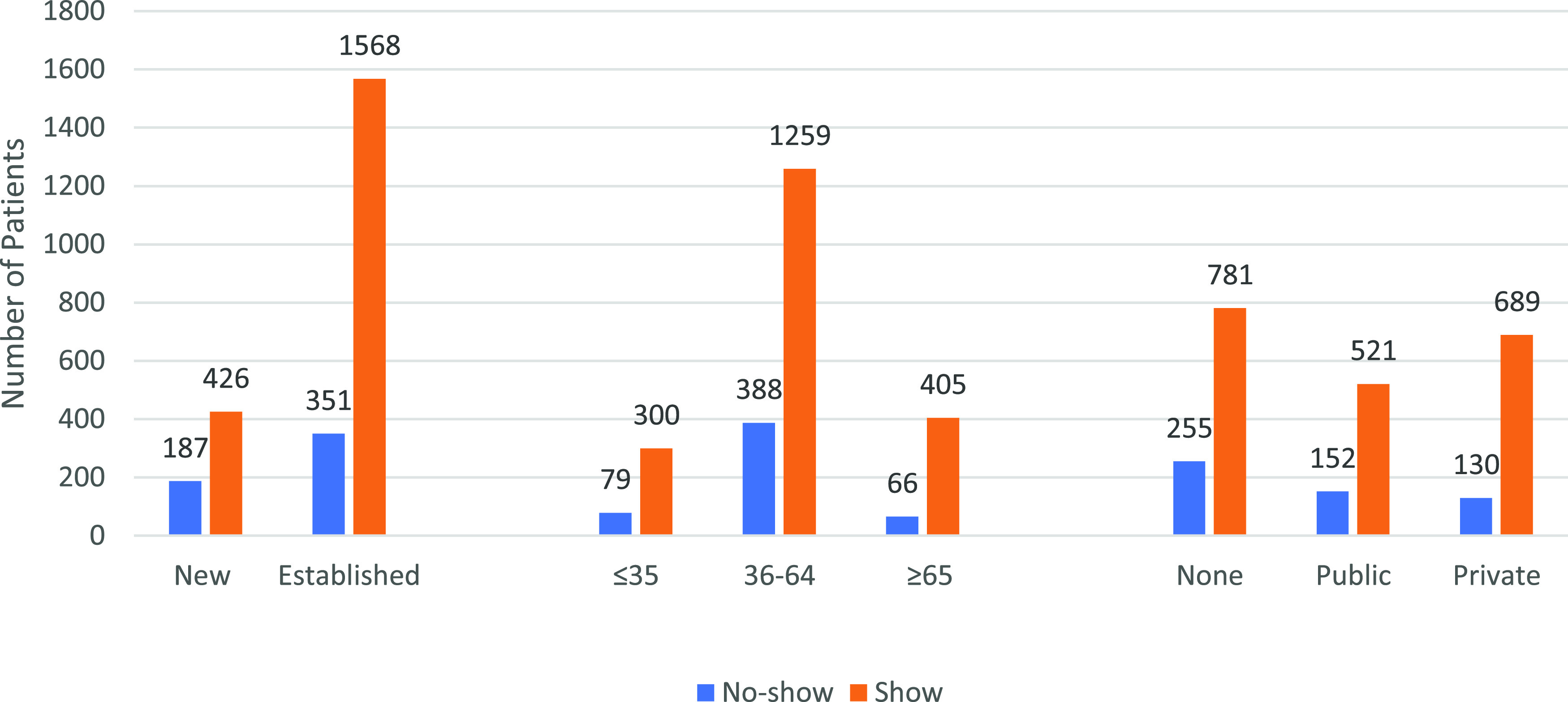
The bar graph illustrates the appointment attendance (number of patients who show vs no-show) based on appointment type (new vs established), age category, and type of health insurance coverage (none, public, or private). New patients were 1.96 times more likely to not show up than established patients. Age (≤35, 36–64, and ≥65 years) and appointment attendance (show vs no-show). Younger patients (≤ 35 years) were 1.53 times more likely to not show up than older patients aged 36–64 and ≥65 years. Type of insurance coverage and appointment attendance. Patients with no health insurance were 1.55 times more likely to not show up for a clinic visit than those with private or public health insurance. All statistical analysis showed P < .0001.
Table 2.
Multivariate logistic regression predicting no-show based on age category, status of appointment, and health care coverage.
| Independent Variable | Adjusted Odds Ratio (95% Confidence Interval) |
|---|---|
| Age (yr) | |
| 17–40 | 1.72 (1.23, 2.40) |
| 41–64 | 0.87 (0.69, 1.09) |
| ≥65 | 1.00 (reference) |
| Status of appointment | |
| Established | 1.00 (reference) |
| New | 1.78 (1.44, 2.20) |
| Health care coverage | |
| Public | 1.00 (reference) |
| Private | 0.88 (0.70, 1.12) |
| None | 1.62 (1.24, 2.11) |
DISCUSSION
This retrospective study estimated that approximately 1 of 5 adult patients do not show up for their appointment at our sleep disorders clinic, which is a university-based specialty clinic located within a major city in the midwestern United States. We reviewed our multispecialty academic practice quality assurance report from July 2017 to July 2018 at the Pulmonary Clinic, which is situated at a different geographic location (the Doctors’ Office Building) from our sleep disorders center, and it listed a no-show rate of 22.2%, a rate similar to ours at the Sleep Disorders Clinic (A. Kosydor, written communication, September 2018). Our no-show rate also tracks closely to the overall 18.8% no-show rate reported by subspecialty clinics at regional health care centers in the United States.2
Our study found higher no-show rates in patients who are younger (age ≤ 40 years), new to the sleep disorder clinic, or without health insurance. Potential reasons for younger patients missing their appointments include employment demands or a lack of sense of urgency, although we were unable to ascertain these factors in the study. Adults younger than 40 years may have lower level jobs that do not allow for flexible medical leave compared with older adults ≥65 years, who are more likely to be retired. Younger patients may also perceive themselves as healthier and less vulnerable to the complications of their sleep disorders and do not feel the urgency to seek medical evaluation. Furthermore, new patients may be looking into different sleep centers, perhaps closer to their homes or places of work, and do not feel obligated to stick to the same health care system provider. It is also understandable that patients without health insurance miss appointments because of the exorbitant cost of health care and the financial burden of clinic visits. Our data align with similar studies about no-show rates in different types of clinics. The study of Odonkor et al3 mirrored our results of higher no-show rates in patients who are younger or have limited or no health care coverage. The study of Shuja et al5 also found that patients with noncommercial insurance (eg, Medicare, Medicaid, city contract) had statistically higher no-show rates than those with commercial insurance. Although the study of Shuja et al5 did not investigate patients without insurance, their findings corroborate the poor no-show rates for individuals who struggle to obtain health insurance.
There are several strengths to our study. Although studies have looked at determinants of no-show rates, none has ever looked at the determinants that affect a sleep disorder clinic. A sleep disorder clinic can involve time-extensive procedures, such as sleep studies, and no-shows can have a large impact on poor workflow and wasted resources. This study offers insight in combating no-show rates and improving patient outcomes. Our large sample provided statistical power to detect statistically significant differences and allowed us to conduct a multivariable logistic regression analysis of potentially significant independent variables.
There are also several limitations of this study. As a retrospective study based on abstraction of electronic health records, only a finite number of independent variables were collected to determine factors associated with patient no-show. Hence, there might be unknown confounding determinants that were not included in our analysis. One potential confounder is the appointment lag time, which may result in memory decay for the scheduled appointment with the passage of time.7 The average appointment lag time at our sleep disorders clinic during the study period from August 2017 to August 2018 was 19.8 days (A. Kosydor, written communication, September 2018). In comparison, Drewek et al6 observed higher no-show rates at pulmonary and gastrointestinal pediatric clinics with an appointment lag time longer than 30 days. It is thus unlikely that a 20-day appointment lag time at our adult sleep disorders clinic could have influenced our no-show rate. Meanwhile, none of the patients were contacted after their clinic visit to discern the reason of no-show and our data never distinguished between cancellations and no-show. Thus, our results did not determine the potential psychosocial mechanisms behind the no-show. In addition, our results cannot be broadly generalized to other sleep centers that serve populations with demographic distributions different from ours. However, our findings may prove to be similar to certain academic sleep centers located in Midwestern urban areas that cover more diversified and underserved populations. Another purported confounder that might influence show rate is the underlying diagnosis. We queried the frequency of billing diagnoses at our center over 6 months during the study time period, and we found that the vast majority of our patients were being evaluated for sleep-related breathing disorders (ie, obstructive sleep apnea [75.12%], central sleep apnea [3.40%], and sleep-related hypoxemia/hypoventilation [<1%]), whereas the remainder, for non–respiratory-related sleep disorders (20%). (R. C. Craig, written communication, November 2018). The much larger proportion of obstructive sleep apnea diagnosis compared with other diagnoses in our cohort would not have allowed us to statistically compare the no-show rates among the different sleep disorder diagnoses. The source and reason for referral (eg, patient self-referral because of sleepiness, referral by spouse because of patient’s snoring, referral by surgeon for preoperative evaluation, primary care provider vs specialist referral for concern about sleep-related risk factors) might have also played a role in show rates but were not expeditiously ascertained from the electronic health record. Finally, although the overall no-show rate was calculated over a period of 10 months, only data from the months of July, October, January, and April. If the data between these months were included, it could underestimate or overestimate the no-show rate per season.
Further studies should explore other reasons behind the no-show rates in sleep disorders clinics. Purported reasons include long appointment lag times, long wait times, and patient satisfaction from previous clinic visits; aversion to treatment recommendations (eg, continuous positive airway pressure therapy); comorbid medical conditions; educational attainment; employment status; job schedule; availability of evening/weekend hours; and alternative clinic locations. Additionally, modifications and policies can be made to address the determinants of no-show. In our practice, for example, patients who have no health insurance are referred by our clinic staff to the billing department to discuss professional fees and payment plans. Health care provider systems should also use social workers to assist the patient in applying for government-subsidized health insurance (eg, Medicaid) to reduce disparities to health care access in underserved groups. Newly referred patients can be offered additional appointment reminders via telephone call, text messaging, or email to decrease the chance of a no-show. Moreover, for practices that have a long appointment lag time, new patients could be given priority slots in the appointment schedule so that they can quickly address their sleep complaints. An alternative approach to improving access is through the use of virtual clinic visits via telemedicine. Telemedicine visits may improve show rates by obviating the need for transportation to the sleep disorders clinic. In contrast, technological access to telemedicine equipment may be limited, particularly in underserved groups. Systematically investigating the determinants of no-show and implementing evidence-based approaches to mitigate these factors can enhance health care participation and thereby improve health-related outcomes in patients with sleep disorders.
CONCLUSIONS
Independent predictors of no-show appointments included younger age, new patient status, and lack of health insurance. Our findings will aid future efforts to identify patients with high predictors of nonadherence. Further studies are needed to develop methods to decrease no-show rates once high-risk appointments have been identified.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Work for this study was performed at SLUCare Sleep Disorders Center, Saint Louis University School of Medicine, St Louis, MO. The authors report no conflicts of interest.
REFERENCES
- 1.Colten HR, Altevogt BM, eds. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 2.Kheirkhah P, Feng Q, Travis LM, Tavakoli-Tabasi S, Sharafkhaneh A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv Res. 2016;16(1):13. 10.1186/s12913-015-1243-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Odonkor CA, Christiansen S, Chen Y, et al. Factors associated with missed appointments at an academic pain treatment center: a prospective year-long longitudinal study. Anesth Analg. 2017;125(2):562–570. 10.1213/ANE.0000000000001794 [DOI] [PubMed] [Google Scholar]
- 4.Knolhoff JB, Djenic B, Hsu CH, Bouton ME, Komenaka IK. Missed appointments in a breast clinic: patient-related factors. Am J Med Sci. 2016;352(4):337–342. 10.1016/j.amjms.2016.07.003 [DOI] [PubMed] [Google Scholar]
- 5.Shuja A, Harris C, Aldridge P, Malespin M, de Melo SW, Jr. Predictors of no-show rate in the GI endoscopy suite at a safety net academic medical center. J Clin Gastroenterol. 2019;53(1):29–33. 10.1097/MCG.0000000000000928 [DOI] [PubMed] [Google Scholar]
- 6.Drewek R, Mirea L, Adelson PD. Lead time to appointment and no-show rates for new and follow-up patients in an ambulatory clinic. Health Care Manag (Frederick). 2017;36(1):4–9. [DOI] [PubMed] [Google Scholar]
- 7.Ricker TJ, Vergauwe E, Cowan N. Decay theory of immediate memory: from Brown (1958) to today (2014). Q J Exp Psychol Hove. 2016;69(10):1969–1995. 10.1080/17470218.2014.914546 [DOI] [PMC free article] [PubMed] [Google Scholar]


