Abstract
Introduction
Biased language influences health care providers' perceptions of patients, impacts their clinical care, and prevents vulnerable populations from seeking treatment. Training clinicians to systematically replace biased verbal and written language is an essential step to providing equitable care.
Methods
We designed and implemented an interactive workshop to teach health care professionals a framework to identify and replace stigmatizing language in clinical practice. The workshop included a reflective exercise, role-play, brief didactic session, and case-based discussion. We developed the program for a broad target audience of providers and initially delivered it at three academic conferences. We used descriptive statistics to analyze Likert-style items on course evaluations and identified themes in open-text responses.
Results
A total of 66 participants completed course evaluations; most believed the workshop met its objectives (4.8 out of 5.0) and strongly agreed that they would apply skills learned (4.8). Participants planned to incorporate reflection into their verbal and written language. Potential barriers to applying course content included perceived difficulty in changing entrenched practice habits, burnout, and fatigue. Suggestions for improvement included more time for group discussions and strategies to teach skills to colleagues.
Discussion
Participants found the course material highly engaging and relevant to their clinical practice. Learners left the workshop feeling motivated to engage in more mindful word choice and to share key concepts with their colleagues.
Keywords: Health Disparities, Bias, Language, Communication Skills, Cultural Competence, Diversity, Inclusion, Health Equity, Professionalism, Case-Based Learning, Anti-racism
Educational Objectives
By the end of this activity, learners will be able to:
-
1.
Explain the impact of providers' language biases on patient care.
-
2.
Describe strategies that can be used to mitigate providers' language biases.
-
3.
Apply strategies from the Mindful Language Toolkit to address stigmatizing language.
Introduction
There is increasing evidence that biased spoken and written language influences perceptions of patients and negatively affects treatment plans.1–5 Goddu and colleagues' 2018 study exploring the impact of biased documentation found that medical students and residents randomized to read a clinical vignette using biased language to describe a patient with sickle cell disease were more likely to have a negative perception of the patient and less likely to recommend opioid analgesicss.1 A similar pattern was found among mental health professionals who read a clinical vignette of a patient referred to as a substance abuser versus substance user; participants who read descriptions of a substance abuser were more likely to make character judgments and recommend punitive measures.2 Biased language in the electronic health record may negatively influence future provider perceptions and patient care as well.
Patients with stigmatizing conditions such as diabetes, obesity, substance use disorder, and chronic pain are affected by the language of their health care providers.6–11 Biased language can worsen feelings of shame, decreasing patients' motivations to complete their treatment plans or engage in treatment at all.9,12 Therefore, biased language, likely due to assumptions made from the environment and throughout training, plays a central role in perpetuating health care disparities. As medical records become increasingly accessible to patients and their families, the importance of unbiased documentation that supports patient agency is magnified.
MedEdPORTAL has several examples of workshops promoting antioppressive language use. For example, Mayfield and colleagues' LGBTQ-inclusive sexual history taking curriculum teaches the importance of using appropriate terms and gender-neutral language.13 Stagno, Crapanzano, and Schwart's workshop for mental health audiences highlights the importance of using person-first language and removing judgmental words such as denies or claims.14 However, there are no antibias workshops that provide a framework for identifying verbal and written bias in other clinical contexts.
Here, we describe the development of a language-based, antibias workshop and provide the materials necessary to present this training program. The course specifically addresses stigmatizing language in both written and verbal communication, including health records and clinical presentations, using a framework that reinforces antibias and antioppressive skills. The target audience is broad, including any provider, trainee, or staff member who works with patients in a clinical environment. We describe the power of stigmatizing language in medicine and situations in which clinicians often use biased language, as well as providing learners with tools to replace biased language.
Methods
This workshop was designed by participants and facilitators at the Stanford School of Medicine Leadership Education in Advancing Diversity (LEAD) program, including residents, fellows, program administrators, and teaching faculty.15 Several members of this team had prior experience developing and facilitating antibias trainings. Three investigators were clinician educators with experience in workshop design and faculty development; three investigators were LEAD program instructors with content expertise in equity and inclusion; one trainee had prior experience developing and presenting an antibias workshop. Team members completed an extensive literature review of stigmatizing language in medicine to identify workshop content; search terms included the specific conditions of obesity, addiction, and chronic pain. We selected Sukhera and Watling's framework for integrating implicit bias recognition into health professions education16 as our conceptual model, including these key recommendations: (1) create a safe space for learning, (2) emphasize how biased language impacts patient outcomes, (3) increase self-awareness of personal biases, (4) discuss strategies to overcome these patterns, and (5) enhance awareness of influence of implicit biases on others.
Our target audience was all health professionals caring for patients and documenting in the electronic medical record, including novice learners. There were no prerequisites for learners. We piloted the workshop with a diverse group of learners at three different professional conferences: the Stanford Medicine Second Annual Diversity and Inclusion Forum,17 the Academy for Professionalism in Heath Care (APHC) Seventh Annual Meeting,18 and the Academic Pediatric Association (APA) Region 9/10 Annual Meeting.19 The LEAD program provided our workshop facilitators with trainings that included reducing unconscious bias and microaggressions and addressing privilege and allyship. We recommend that facilitators have experience with these topics. Audience participation was voluntary, and there were no incentives.
The workshop was designed to be 90 minutes, and course materials were inexpensive to duplicate. The facilitator's guide (Appendix A) provided a detailed agenda, and the PowerPoint presentation (Appendix B) contained detailed presenter notes below each slide. Key features of the workshop included the deliberate creation of a brave space,20 a skit demonstrating biased language in a clinical presentation (Appendix C), a short didactic to define important terms, introduction of the Mindful Language Toolkit (Appendix D), group discussions, and opportunities to practice learned skills (Appendix E). Clinical cases can be adapted to the clinical discipline of the audience. However, we believe that the cases represent a wide variety of biased language commonly encountered in any discipline or position in health care.
All workshop attendees completed course evaluations (Appendix F) consisting of four 5-point Likert-style items (1 = strongly disagree, 5 = strongly agree), which were analyzed using descriptive statistics. Additionally, participants were asked four short-answer questions that were analyzed using the thematic content approach, which included data familiarization, identifying themes, developing and applying a coding scheme, and organizing codes and themes.21 One investigator (Ria Pal) developed the coding framework, and two other investigators (Julia Raney and Kim Hoang) reviewed the coding scheme and made adjustments as necessary. This project was deemed exempt by the Stanford School of Medicine Institutional Review Board (Protocol #55660).
Results
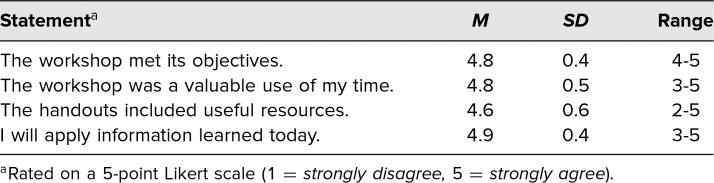
We collected course evaluations from 66 participants (12 APHC, 32 Stanford Diversity Day, and 22 APA conference attendees). Participants agreed that the workshop met its objectives (M = 4.8, SD = 0.4), was a valuable use of time (M = 4.8, SD = 0.5), and provided useful participant handouts and resources (M = 4.6, SD = 0.7). Most participants intended to apply information from the workshop in their future practice (M = 4.8, SD = 0.4; Table 1).
Table 1. Quantitative Evaluations (N = 66).
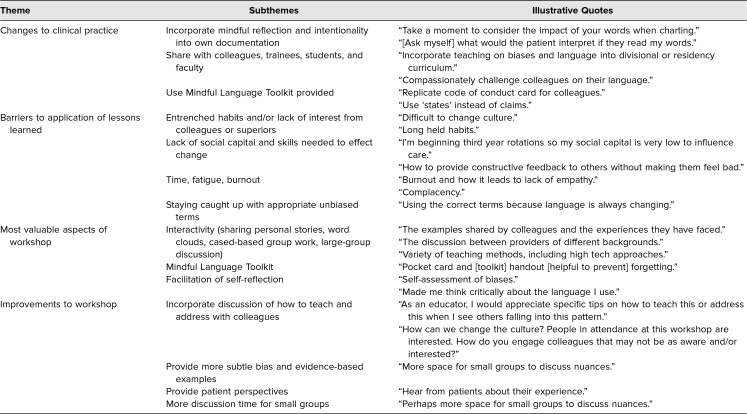
Most participants found the sharing of personal stories, display of stigmatizing language on word clouds, and case-based examples to be particularly helpful activities (Table 2). Participants also enjoyed learning from group discussions with their colleagues and identified the Mindful Language Toolkit as a course highlight. Several participants offered feedback to better structure the workshop, including more time for small-group discussion. Many participants planned to teach lessons learned in the workshop to their colleagues and trainees, and some participants recommended adding dedicated workshop time to learn teaching and implementation strategies. Additionally, some participants suggested including more subtle and nuanced examples of bias and patient perspectives on the topic.
Table 2. Themes From Open-Ended Course Evaluations (N = 66).
Participants planned to use the Mindful Language Toolkit, workshop handouts, or reflective exercises to practice language substitutions discussed in the presentation. However, participants also identified several barriers to change, including the rigid social structure in medicine, cultural norms, entrenched practice habits, normalization of stigmatizing language, and assumptions that colleagues or supervisors would lack interest in the topic. Time, fatigue, and burnout were also cited barriers. Interestingly, participants were concerned about staying caught up with appropriate terminology and being unaware of antibias language choices.
Discussion
Based on our experience piloting this course, we believe it fills an important gap by providing health professionals with a practical framework to identify and replace biased language. Stigmatizing language is normalized in medicine, and providers require concrete skills to make meaningful changes to their long-standing language use. Most of our participants learned new actionable skills in the workshop that they intended to incorporate in their practices, such as avoiding labeling patients, reframing situations, and reflecting before documenting. Prior implicit bias research has shown that teaching intentional strategies, such as those in our workshop, is key to reducing biased behaviors following an intervention.22 Our workshop offers antibias skills and strategies in the Mindful Language Toolkit and provides activities that allow participants to practice these techniques in a safe environment. However, the Mindful Language Toolkit should not stand alone without interactive teaching and facilitated discussion.
Participants described important barriers to the implementation of antibiased language in their workplaces. This feedback emphasizes the need to engage key stakeholders, such as unit supervisors and hospital administrators, who can facilitate normative practice changes. In response to this identified barrier, we lengthened the final group discussion to include strategies for building institutional support.
Participants offered several suggestions for how to overcome cultural barriers to practice change. For example, they recommended including discussion of how to educate colleagues about stigmatizing language. This topic is often included in implicit bias trainings23,24 but was not initially covered in our workshop. However, given that social pressure is one of the most commonly cited barriers to addressing implicit bias, we modified our workshop to address this topic.
Lessons learned from piloting the workshop include the importance of providing ample time for practice of new skills and discussion with peer learners, as well as the broad application of the material to learners from different stages of training and discipline. The Mindful Language Toolkit is a critical feature of the training that summarizes key content and implementation strategies. We will extend the length of the workshop to better address potential barriers to change and to offer teaching techniques to participants interested in disseminating content to their colleagues and trainees.
Limitations
The setting of the workshop likely introduces some selection bias, as participants who attended may have been motivated to reduce disparities. Course evaluations focused on participants' self-reported reactions to the workshop, and we are unable to comment on knowledge or behavioral changes. One way to evaluate these in future studies would be to query electronic medical records for biased words such as alcoholic or frequent flyer following a training. In addition, course evaluations did not assess the impact of the interprofessional learning environment. Anecdotally, the presenters remember many interdisciplinary small groups and rich interprofessional discussions, so we believe the content translated well to our broad audience. Lastly, there was no presession assessment for pre/post comparisons, and we did not record the total number of participants, which would have allowed for a calculation of course evaluation response rate. We recommend that future course evaluations include presession surveys, the professions of the learners, and their experiences with the interprofessional education.
Conclusion
Learners in our workshop on stigmatizing language in health care were highly engaged and found the material clinically relevant. Participant feedback suggests that the workshop provided actionable skills for replacing biased language in clinical presentations and electronic health records. Barriers to practice change are important to address in future iterations of the workshop.
Appendices
- Facilitator's Guide.docx
- PowerPoint Presentation.pptx
- Sign-out Skit.docx
- Mindful Language Toolkit.docx
- Clinical Cases.docx
- Course Evaluation.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Acknowledgments
We wish to thank the Stanford University Leadership Education in Advancing Diversity (LEAD) program and Natalie Kirilcuk, MD, for their mentorship.
Disclosures
None to report.
Funding/Support
None to report.
Ethical Approval
The Stanford University School of Medicine Institutional Review Board approved this study.
References
- 1.Goddu AP, O'Conor KJ, Lanzkron S, et al. Do words matter? Stigmatizing language and the transmission of bias in the medical record. J Gen Intern Med. 2018;33(5):685–691. 10.1007/s11606-017-4289-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Policy. 2010;21(3):202–207. 10.1016/j.drugpo.2009.10.010 [DOI] [PubMed] [Google Scholar]
- 3.Samulowitz A, Gremyr I, Eriksson E, Hensing G. “Brave men” and “emotional women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag. 2018;2018:6358624. 10.1155/2018/6358624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broyles LM, Binswanger IA, Jenkins JA, et al. Confronting inadvertent stigma and pejorative language in addiction scholarship: a recognition and response. Subst Abuse. 2014;35(3):217–221. 10.1080/08897077.2014.930372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shattell MM. Stigmatizing language with unintended meanings: “persons with mental illness” or “mentally ill persons”? Issues Ment Health Nurs. 2009;30(3):199. 10.1080/01612840802694668 [DOI] [PubMed] [Google Scholar]
- 6.Dickinson JK, Guzman SJ, Maryniuk MD, et al. The use of language in diabetes care and education. Diabetes Care. 2017;40(12):1790–1799. 10.2337/dci17-0041 [DOI] [PubMed] [Google Scholar]
- 7.Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between Blacks and Whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–4301. 10.1073/pnas.1516047113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schäfer G, Prkachin KM, Kaseweter KA, Williams AC. Health care providersʼ judgments in chronic pain: the influence of gender and trustworthiness. Pain. 2016;157(8):1618–1625. 10.1097/j.pain.0000000000000536 [DOI] [PubMed] [Google Scholar]
- 9.Goodyear K, Haass-Koffler CL, Chavanne D. Opioid use and stigma: the role of gender, language and precipitating events. Drug Alcohol Depend. 2018;185:339–346. 10.1016/j.drugalcdep.2017.12.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit bias in health care: a narrative review. Group Process Intergroup Relat. 2016;19(4):528–542. 10.1177/1368430216642029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper A, Kanumilli N, Hill J, et al. Language matters. Addressing the use of language in the care of people with diabetes: position statement of the English Advisory Group. Diabet Med. 2018;35(12):1630–1634. 10.1111/dme.13705 [DOI] [PubMed] [Google Scholar]
- 12.Pont SJ, Puhl R, Cook SR, Slusser W; Section on Obesity; Obesity Society. Stigma experienced by children and adolescents with obesity. Pediatrics. 2017;140(6):e20173034. 10.1542/peds.2017-3034 [DOI] [PubMed] [Google Scholar]
- 13.Mayfield JJ, Ball EM, Tillery KA, et al. Beyond men, women, or both: a comprehensive, LGBTQ-inclusive, implicit-bias-aware, standardized-patient-based sexual history taking curriculum. MedEdPORTAL. 2017;13:10634. 10.15766/mep_2374-8265.10634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stagno S, Crapanzano K, Schwartz A. Keeping the patient at the center: teaching about elements of patient-centered care. MedEdPORTAL. 2016;12:10500. 10.15766/mep_2374-8265.10500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leadership Education in Advancing Diversity. Stanford Medicine. Accessed April 1, 2020. https://med.stanford.edu/pediatrics/education/events/lead.html [Google Scholar]
- 16.Sukhera J, Watling C. A framework for integrating implicit bias recognition into health professions education. Acad Med. 2018;93(1):35–40. 10.1097/ACM.0000000000001819 [DOI] [PubMed] [Google Scholar]
- 17.Bhushan D, Leahy P, Lee T, et al. Words hurt: identifying and removing stigmatizing language from clinical settings. Workshop presented at: Stanford Medicine Annual Diversity and Inclusion Forum; May 10, 2019; Stanford, CA. [Google Scholar]
- 18.Lee T, Bhushan D, Leahy P, et al. Words hurt: identifying and removing stigmatizing language from clinical settings. Workshop presented at: Academy for Professionalism in Health Care Annual Meeting; May 15–17, 2019; New Orleans, LA. [Google Scholar]
- 19.Raney J, Saenz SR, Kapphahn C, et al. “The sickler in room 202 is a poor historian”: exploring how stigmatizing language reflects implicit bias. Workshop presented at: Academic Pediatric Association Region 9/10 Annual Meeting; Spring 2019; Monterey, CA. [Google Scholar]
- 20.Ali D. Safe Spaces and Brave Spaces: Historical Context and Recommendations for Student Affairs Professionals. National Association of Student Personnel Administrators; 2017. NASPA Policy and Practice Series no. 2. [Google Scholar]
- 21.Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ. 2000;320(7227):114–116. 10.1136/bmj.320.7227.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.FitzGerald C, Martin A, Berner D, Hurst S. Interventions designed to reduce implicit prejudices and implicit stereotypes in real world contexts: a systematic review. BMC Psychol. 2019;7:29. 10.1186/s40359-019-0299-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maurer MJ, Goldstein RL, Riveros LFV, et al. Death by a thousand paper cuts: microaggressions and their effects on the learning climate. Workshop presented at: Association of Pediatric Program Directors Annual Spring Meeting; March 20–23, 2018; Atlanta, GA. [Google Scholar]
- 24.Acholonu RG, Cook TE, Roswell RO, Greene RE. Interrupting microaggressions in health care settings: a guide for teaching medical students. MedEdPORTAL. 2020;16:10969. 10.15766/mep_2374-8265.10969 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- Facilitator's Guide.docx
- PowerPoint Presentation.pptx
- Sign-out Skit.docx
- Mindful Language Toolkit.docx
- Clinical Cases.docx
- Course Evaluation.docx
All appendices are peer reviewed as integral parts of the Original Publication.