Abstract
While substantial public health investment in anti-smoking initiatives has had demonstrated benefits on health and fiscal outcomes, similar investment in reducing obesity has not been undertaken, despite the substantial burden obesity places on society. Anti-obesity medications (AOMs) are poorly prescribed despite evidence that weight loss is not sustained using other strategies alone.
We used a simulation model to estimate the potential impact of 100% uptake of AOMs on Medicare and Medicaid spending, disability payments, and taxes collected relative to status quo with negligible AOM use. Relative to status quo, AOM use simulation would result in Medicare and Medicaid savings of $231.5 billion and $188.8 billion respectively over 75 years. Government tax revenues would increase by $452.8 billion. Overall, the net benefit would be $746.6 billion. Anti-smoking efforts have had substantial benefits for society. A similar investment in obesity reduction, including broad use of AOMs, should be considered.
Keywords: obesity, public health, anti-obesity agents, Medicaid, Medicare, weight loss, economic modeling, microsimulation, health policy
What do we already know about this topic?
Despite the substantial societal burden of obesity, substantial public health investment in reducing obesity has not been undertaken.
How does your research contribute to the field?
We simulated the potential fiscal impacts of 100% uptake of anti-obesity medications relative to status quo with negligible anti-obesity medications use.
What are your research’s implications toward theory, practice, or policy?
We found a net benefit of $746.6 billion, suggesting public health investment in obesity reduction, including broad use of AOMs, should be considered.
Introduction
As the proportion of Americans who have obesity rises, the epidemic is having broadly negative consequences. Approximately 72% of United States (US) adults is overweight, while 39.8% of Americans has obesity1 based on the anthropomorphic calculation of body mass index (BMI), a clinical indicator for obesity (BMI ≥ 30).2 This excess weight costs the US $116 billion in additional healthcare costs on an annual basis, with most of these costs impacting Medicare and Medicaid.3 Health concerns caused or exacerbated by obesity include hypertension, dyslipidemia, polycystic ovary syndrome, fatty liver disease, type 2 diabetes, and respiratory problems.4 Increased prevalence of obesity-related comorbidities accounted for significant growth in Medicare spending between 1987 and 2011.5 Further, 77.6% of healthcare spending growth is attributable to patients with chronic conditions related to obesity.6 Analysis by Wang et al3found that class II patients with obesity (BMI = 35-40) cost the US approximately $69 billion, accounting for 60% of all obesity-related costs.3 41% of these costs were borne by Medicaid, Medicare, and other federal spending.
The impact of obesity is compounded by the downward pressure that the disease puts on work force participation and the associated decrease in tax revenues.7-9 Workers with a BMI > 30 are more likely to report lost productive time (LPT) than workers with a normal or somewhat elevated BMI and cost an estimated $42.29 billion in LPT, of which 67.8% is accounted for by presenteeism.10 Previous reports have also shown that increasing BMI is associated with lower workforce participation, independent of associated comorbidity and sociodemographic factors.11 The obesity epidemic deserves equal, if not more, attention as other public health fronts, such as smoking prevention and cessation.
Since the US Surgeon General’s Tobacco Report in 1964 causally linking smoking with cancer,12 smoking prevention and cessation have been prominent initiatives in public health, resulting in a 67% decline in smoking from 1965 to 2018, when prevalence of cigarette smoking reached an all-time low among US adults. While the advent of “vaping” and legalized marijuana have created new fronts in public health efforts to reduce the impact of negative health behaviors on society, the investment in smoking cessation has been a remarkable success. In fact, public spending on smoking prevention and cessation initiatives has been substantial, amounting to $658 million in 2011.13
Prior research has demonstrated the substantial potential impact of reducing BMI (weight loss) on morbidity, mortality, healthcare expenditures and revenues.14-17 Several research studies have suggested that investing in reducing weight in society will have a larger benefit in terms of healthcare savings and productivity relative to smoking reductions. A microsimulation by Goldman et al14found that reducing weight in people with BMI > 30 had a demonstrably larger impact on Medicare and Medicaid compared to reducing smoking. The Goldman model estimated a $252 billion reduction in Medicare costs, and a $265 billion reduction in Medicaid costs over a 50-year simulation period by reducing obesity to 1978 levels. In comparison, achieving 1% smoking prevalence had miniscule savings of $2.5 billion. Similarly, research by the Robert Wood Johnson Foundation estimated federal government savings from obesity prevention would grow over a 60+ year time horizon, whereas tobacco use prevention has early benefits but decline over time due to increased longevity of the non-smoking population.18-20
Despite efforts to induce dietary change and to increase physical activity (commonly referred to as lifestyle change), the majority of people with obesity fail to achieve meaningful and sustainable weight loss.19,21,22 While some FDA-approved anti-obesity medications (AOMs) have been available to patients and their physicians for decades, uptake of AOMs remains low.22 This may in part reflect payer limits on access and reimbursement, misconceptions by health-care professionals about the use of these treatments, and lingering safety concerns from the Fenfluramine-Phentermine scare, where some patients experienced pulmonary hypertension and heart valve malfunction prompting market withdrawal by the FDA.23-26 While Fenfluramine-Phentermine was removed from the market many years ago, misconceptions persist around the modern, safe and effective FDA-approved class of AOMs.
Newer AOMs have demonstrated long-term safety and efficacy and offer an opportunity to enhance weight loss and weight maintenance. For example, AOMs have been shown to benefit a significantly larger group of patients versus placebo, with most patients achieving weight loss of ≥5%.26-30 Further, new and novel AOMs are currently in development which will likely achieve even greater magnitude of weight loss.31
Given the changing obesity landscape, both in terms of increasing prevalence, and in terms of new treatment opportunities, this study sought to estimate the potential benefits of an obesity reduction strategy using AOMs in the US population. We evaluated the potential impacts of AOM use on government expenditures for healthcare and disability payments, and on government revenues from employment participation, by comparing the status quo to a scenario where all patients with obesity are treated with current and next generation AOMs. The results of this study provide a framework for considering the impact of a large public-health effort similar to that seen in the area of smoking.
Methods
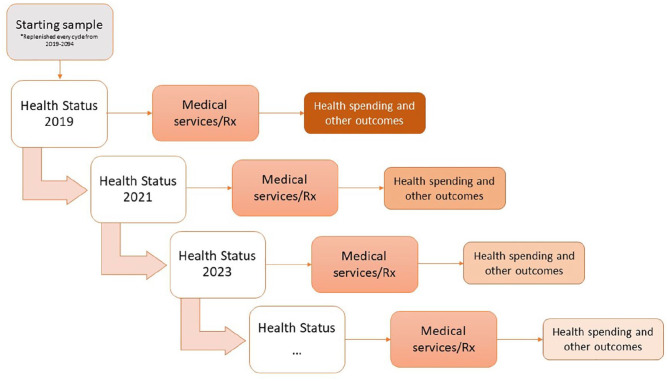
We used a well-established microsimulation model15,16,32-38 to evaluate the impact of broad use of FDA-approved and next generation AOMs on government revenues and expenditures. Public healthcare expenditures and federal and state tax revenues were estimated over 75 years, comparing a scenario with decreased obesity due to increased use of AOMs relative to a status quo scenario of little to no drug use. The 75-year analytic period was selected to parallel the Medicare Trustees report that projects 75-years into the future.39 The Health Economics Medical Innovation Simulation (THEMIS),32 an individual-level microsimulation model (Figure 1), estimates population health trends based on data from the Panel Study of Income Dynamics (PSID).40 As a nationally representative survey of population health and socioeconomic characteristics, the PSID allowed us to evaluate obesity trends under the current standard of care in a heterogeneous US population. The full technical specifications of THEMIS can be found in our online technical report.32
Figure 1.
THEMIS mechanistic diagram.
Note. “Health Status” represents risk factors, health conditions, and survival status of a simulated individual per 2-year model cycle. In each cycle, a simulated individual accessed treatment (if applicable) and accrued costs based on consumption of medical services. Health outcomes translated into health utility. The individual faced transitional probabilities in terms of acquiring new conditions and surviving, informing “Health Status” in the next cycle. Health spending was estimated according to health status. Other model outcomes included cost of absenteeism and presenteeism based on obesity status, labor force participation (full-time, part-time, or not employed) and earned income, quality adjusted life-years.
Statistical Analysis
THEMIS projects future health and economic outcomes using historical and current trends estimated using real-world data sources. PSID data from 1999 to 2015 was used to estimate health and economic transitions, while the National Health and Nutrition Examination Survey from 1999 to 2010 was used to estimate BMI trends. The Medical Expenditures Panel Survey and Medicare Current Beneficiary Survey were used to estimate medical costs and the impact of BMI on those costs.32 For this study we created an obesity risk model using an ordinary least squares regression to predict an individual’s log(BMI) given his/her demographic and health characteristics in the PSID (Supplemental Appendix Exhibit A1). THEMIS also estimated the probability of developing cardiovascular diseases, type 2 diabetes, osteoarthritis, and depression using probit regressions estimated based on the PSID data (upplemental Appendix Exhibit A2i). We estimated the additional medical costs of these comorbidities using statistical models developed based on the Medical Expenditures Panel Survey and Medicare Current Beneficiary Survey data. Additionally, estimation of the impact of reduced BMI on income was based on PSID data. For this analysis, we estimated future government expenditures and revenues calculated as the mean for 100 replications of the Monte Carlo simulation using R and C++.
Study Sample
We simulated a nationally representative sample of Americans aged ≥25 years from 2019 through 2094, in parallels to the time horizon of the annual report on the Medicare trust fund. The sample was initially created from the PSID 2009 data. Birth rates, death rates, health trends, including obesity risk, were estimated from the historical PSID data through 2019 to create the starting sample. The starting sample was replenished every cycle from 2019 to 2094 by adding new cohorts of 25-year-old individuals that represented future US health trends, estimated based on the National Health Interview Survey and Medical Expenditure Panel Survey data.
AOM Treatment Analyses
We first estimated the status quo of government expenditures and revenues assuming no AOM use, given that less than 2% of individuals eligible for AOMs receive such therapies.22,38,41 This analysis served as the base case against which the subsequent scenario was compared. We then estimated a scenario where 100% of eligible, treatment-naïve individuals initiated use of a currently available AOM. We selected the 100% uptake as our scenario to provide perspective on the maximum potential benefits of AOM therapy given realistic assumptions on adherence and discontinuation. While a 100% uptake rate is likely unrealistic, understanding the potential benefits, particularly given the on-going concerns around public funding for Medicare and Medicaid, is warranted. Current FDA-approved AOMs included liraglutide 3.0 mg (Saxenda), lorcaserin (Belviq), phentermine-topiramate (Qsymia), and naltrexone-bupropion (Contrave). At the time of this analysis, lorcaserin (Belviq) had not been withdrawn from market. AOM efficacy was assumed to be 8.9%29,30,42-44 as a 1-time BMI reduction following initiation of therapy based on clinical trial results for these therapies. Starting in 2023 through the end of the simulation period, all eligible treatment-naïve individuals initiated therapy using next generation AOMs to represent the launch of pipeline AOMs (eg, semaglutide). The estimated efficacy was increased to 14% based on current clinical evidence for the next generation AOMs.31
Costs of AOMs were not estimated, as none are currently covered by Medicare and the goal of the study was to evaluate the potential impact of a public health effort, which will include unknown amounts of investment at the local, state and federal level.
Treatment eligibility was established using current clinical guidelines; anyone with BMI ≥ 30 kg/m2 was eligible for treatment, while patients with BMI ≥ 27 kg/m2 were required to have at least 1 weight-related comorbidity (hypertension or type 2 diabetes).45 We assumed that all treated patients adhered to therapy, followed a reduced-calorie diet, and increased physical activity.
To capture likely real world use, we assumed 30% of treated individuals would discontinue AOM treatment every year, similar to the rate observed with oral antidiabetic therapies.46 Once discontinued, a patient was assumed not to resume treatment. Following discontinuation, a patient’s BMI was assumed to follow the BMI trajectory as estimated by the predictive model for log(BMI), starting from their reduced BMI.
Outcomes
For our assessment of the impact of full uptake of AOMs, we estimated government expenditures and revenues over a 75-year observation period matching the projection window published in the Medicare Trustees report.39 We calculated the results at 10, 25, and 50 years to demonstrate how the expenditures and revenues would change over time. Expenditures included Medicare and Medicaid expenditures, and disability insurance expenditures (Supplemental Security Income [SSI] and Social Security Disability Insurance [SSDI]). Revenues included state and federal income taxes, Medicare payroll taxes and Old-Age and Survivors Insurance (OASI) payroll taxes. All outcomes were calculated as the difference from the status quo. The present values of monetized outcomes were discounted by 3% per year and converted to 2018 US dollars using the consumer price index.47
Results
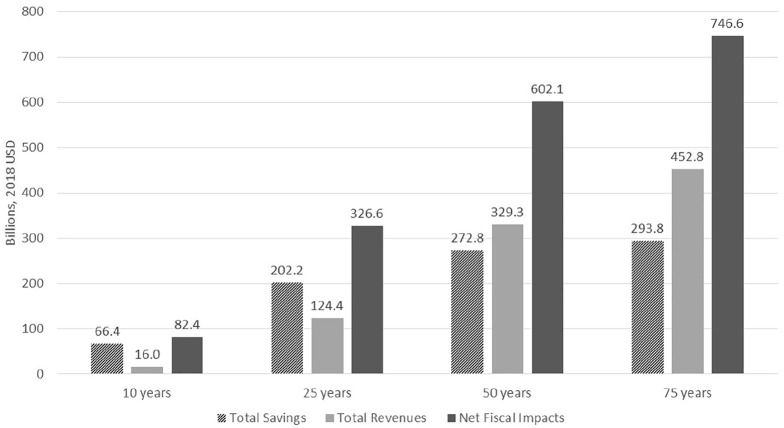
Over the 75-year observation period, the number of treated patients fell as the pool of untreated individuals decreased (Figure 2). Because we did not consider re-treatment among patients who discontinued AOMs, only newly indicated patients—either newly added 25 year-olds who met treatment criteria or existing patients who developed the characteristics indicated for—were potential treatment candidates.
Figure 2.
Number of treated patients given 100% anti-obesity medication uptake among patients.
Relative to status quo, adding obesity treatment resulted in a substantial decrease in expenditures for Medicare, Medicaid, and disability payments over the 75-year simulation period (Table 1). The simulation estimated that Medicare would experience a reduction of $231.5 billion in expenditures due to obesity treatment over the period from 2019 to 2094. Similarly, Medicaid savings would reach $188.8 billion by the end of the 75-year simulation period. Offsetting these savings, more patients would survive to retirement and collect OASI, resulting in an increase in these retirement outlays of $184.8 billion. Net change in expenditures showed a substantial reduction in fiscal burden of obesity from widespread use of AOMs, with savings reaching $293.8 billion over the 75-year simulation period.
Table 1.
Changes in Cumulative Expenditures and Revenues Over 75 Years From 100% Uptake of Anti-Obesity Medications.
| Outcome (billions, 2018 USD) | Impact of 100% treatment of obesity with AOMs over 75 years ($ billions) | |||
|---|---|---|---|---|
| At 10 years | At 25 years | At 50 years | At 75 years | |
| Government expenditures | ||||
| Medicare | −30.4 | −113.6 | −188.9 | −231.5 |
| Medicaid | −34.2 | −103.6 | −163.8 | −188.8 |
| SSI and SSDI | −4.0 | −20.6 | −44.4 | −58.3 |
| OASI | 2.2 | 35.6 | 124.3 | 184.8 |
| Total | −66.4 | −202.2 | −272.8 | −293.8 |
| State and federal revenues | ||||
| Federal income taxes | 18.0 | 106.7 | 244.2 | 316.8 |
| State income taxes | 3.1 | 18.9 | 44.1 | 57.2 |
| Medicare and OASI payroll taxes | −5.1 | −1.2 | 41.0 | 78.8 |
| Total | 16.0 | 124.4 | 329.3 | 452.8 |
| Net fiscal impacts | 82.4 | 326.6 | 602.1 | 746.6 |
| Percent change relative to status quo | (+3.08%) | (+18.5%) | (+27.2%) | (+10.1%) |
Note. AOMs = anti-obesity medication; SSI = supplemental security income; SSDI = social security disability insurance; OASI = old-age and survivors insurance. Net fiscal impact = revenues − expenditures.
Expenditure changes observed in the first 10 years of the simulation were relatively modest—$66.4 billion relative to the status quo. Savings accrued to Medicaid and Medicare with a slightly larger benefit to the Medicaid program from the initial population receiving treatment in the simulation. By the end of the 75-year simulation, the benefits of reducing obesity through 100% uptake of AOMs was 22% greater in Medicare than Medicaid.
The change in federal income taxes relative to status quo was a cumulative $18 billion after 10 years of AOM use, climbing to a cumulative $316.8 billion increase in federal income taxes after 75 years. Overall revenues increased from a cumulative $16 billion after 10 years of AOM use, to a cumulative $452.8 billion after 75 years.
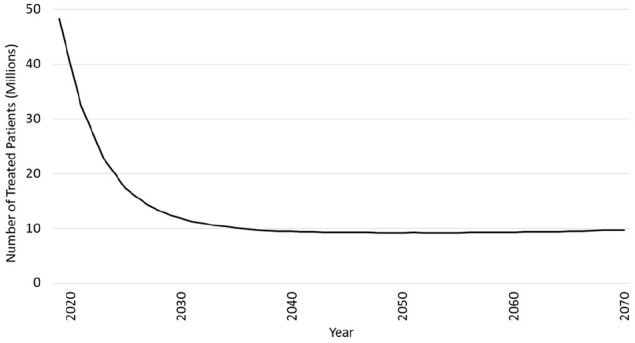
The net change in fiscal impacts (ie, the difference between expenditures and revenue) of increased use of AOMs relative to status quo, increased from a cumulative $82.4 billion after just 10 years (+3.08% from status quo) to a cumulative $746.6 billion at the end of 75 years (+10.1% from status quo; Figure 3).
Figure 3.
Net fiscal impacts of 100% uptake of anti-obesity medications over 75 years.
Note. Net fiscal impact = revenues + savings. Savings reflect negative government expenditures.
Discussion
Obesity is endemic in the US, and is projected to get substantially worse. A recently published study suggests that by 2030, nearly half of all Americans will have obesity. Using data from the Behavioral Risk Factor Surveillance System Survey, researchers estimated that the prevalence of obesity will be higher than 50% in 29 states and not below 35% in any state. Nearly 25% of adults will have severe obesity (BMI ≥ 40).48 As obesity in the population increases over time, the consequences are likely to be substantial, both in terms of health and economic impact.
Our study demonstrated that taking a broad public-health approach that includes AOMs to address the impacts of obesity has the potential to generate substantial savings while simultaneously increasing revenues through productivity gains from a healthier population. We took an expansive approach to estimating the impact of savings from widespread use of current and future medications for treating obesity. This approach allowed us to estimate the magnitude of the benefit that may be achieved with a major shift in public health efforts to reduce obesity.
Relative to projections based on current AOM use, we estimated that the net fiscal benefits of broad AOM use could be close to $750 billion over 75 years, with substantial savings to both Medicare and Medicaid, and additional earned revenues from paid taxes. While the initial benefits of widespread AOM use were higher in Medicaid, by the end of the 75-year simulation, the economic benefit was 22% greater in Medicare than Medicaid. These findings provide an important reflection point for policymakers with jurisdiction over both Medicare and Medicaid, where there is the opportunity to update outdated law and regulation to capture the savings from treating obesity that is not currently realized into government healthcare savings. Revenues generated from treating obesity, $16 billion after 10 years of AOM use rising to $452.8 billion after 75 years, highlight a common sense solution to strengthen the US’ economic competitiveness into the future.
While our analysis focused specifically on public healthcare spending and revenues, the potential impacts of a wide spread obesity treatment initiative leveraging proven medications to achieve meaningful weight loss could be enormous. These tremendous improvements might manifest as improvements in work productivity and decreases in other private healthcare spending.16,17,49,50
Potential benefits from a public-health initiative to reduce obesity can be drawn from the evidence from smoking cessation, where a multipronged approach has resulted in significant reductions in smoking. As one prong of this effort, improved coverage of smoking cessation treatments was shown to result in increased uptake of antismoking medications.51,52 The benefits of this uptake were modeled in a study which estimated that over 10 years a return of $3.22 in savings per dollar spent was generated for Medicare and $2.50 in savings per dollar spent was generated for Medicaid.53 We know from previous research that the potential savings generated from reducing obesity may be far greater than the gains observed from a focus on smoking.14,54-56 Our research similarly suggests substantial net benefits to society from such an investment.
Our findings are supported by other research examining the potential benefits of obesity reduction. One study modeling a 10-year period of widespread use of AOMs similarly found significant savings potential. In this study, for each beneficiary receiving AOMs, Medicare had the potential to save $6842 to $7155 over 10 years.57 Another study which modeled the impact of a 10% to 15% weight loss on Medicare spending over 10 years found gross savings per capita of $8287 to $9826, even when accounting for a weight rebound among most patients.58
Today, we know that having an elevated BMI contributes negatively to morbidity, mortality, healthcare expenditures and revenues. Yet, treatment for obesity appears to be going unchecked. For those who do get medical interventions, these often come in the form of lap band or bariatric surgery. One estimate suggests that the total number of metabolic and bariatric procedures performed increased from approximately 196 000 to 216 000 from 2015 to 2016.51,52 This estimate likely represents as little as 1% of the clinically eligible population for surgical obesity treatment. Research has shown that use of AOMs is low and remains relatively stagnant at roughly 2% of the population with obesity, and physician knowledge may be a part of this low rate of use.59 Yet, with available treatments today and next generation AOMs in the near future, the potential to have a broader impact on obesity treatment/chronic weight management is available.
Limitations
This study projected government expenditures and revenues over a 75-year time horizon. While all efforts were made to establish reasonable assumptions, the study could not take into account other potential changes to the Medicare benefit or other government programs, so it only estimates the fiscal impact relative to an assumption of the status quo. Further, we imputed medical expenses from information contained in the Medical Expenditures Panel Survey and Medicare Current Beneficiary Survey as medical expenditures from the PSID are considered unreliable. Our method is considered more reliable as the Medical Expenditures Panel Survey contains self-reports that have been calibrated to the National Health Expenditure accounts and the Medicare Current Beneficiary Survey takes spending from a combination of Medicare administrative data and calibrated self-reports, and has been widely published.
Additionally, there is likely more uncertainty associated with our outcomes related to the Markov transition probabilities and the sampling variability of the underlying PSID sample that was not accounted for by the simulation.
Further, we did not account for the costs of AOMs as none are currently covered by Medicare. Even if AOMs add a substantial cost to the system, even in the first 10 years, AOMs would need to cost $8.2 billion to offset the net savings to the system. Given the likely broader benefits of obesity reduction to society not captured in our model, even the additional cost of treatment will likely not diminish these important benefits.
We assumed that all patients who initiated treatment were adherent to their medication and the prescribed lifestyle modification program prior to the point they discontinue. Our assumption of a 30% discontinuation rate at each cycle, which paralleled literature on diabetes treatments, may be conservative. Our assumption of AOM adherence may overestimate the impact of AOMs, but our discontinuation rate may in fact underestimate the population that continues to benefit over time. Further, we assumed that a patient did not resume treatment once it is discontinued, although in reality an alternative treatment may be initiated. Given the poor access and use of AOMs today, no literature was available upon which to establish estimates of adherence and discontinuation. Broader coverage of AOMs may motivate better adherence and reduce discontinuation rates, making our estimates of the benefits conservative.
There remains limited information on the potential efficacy of next generation AOMs. We used an efficacy estimate based on published phase 2 clinical trial results of semaglutide.31 Future AOMs may offer better or worse efficacy than our estimate which would change the results of our analyses in either a positive or negative direction.
We did not adjust any other healthcare utilization inputs that might change with an increased use of AOMs, such as physician visits and monitoring. However, published research in the area of type 2 diabetes prevention suggests that the incremental cost of increased healthcare utilization is very small relative to the large improvement in health outcomes.60,61
Finally, we assumed a 100% uptake scenario for this model. While we recognize this is likely unrealistic, understanding the potential benefits, particularly given the on-going concerns around public funding for Medicare and Medicaid, is warranted. Fundamentally, as this is a forward looking model, any scenario will have its limitations and our approach allows us to provide an upper bound possibility even within the context of the other assumptions around adherence, retreatment and changes in behaviors relative to baseline.
Conclusions
With current obesity rates and projections of a vastly growing population of Americans living with obesity, continuing to rely on recommendations of modifying diet and exercise is clearly not enough to address this epidemic, for which the negative health and economic consequences are substantial. This study demonstrated the potential benefits to federal and state budgets of using AOMs as a weight management treatment in the US. Broad use of AOMs, especially anticipated next generation AOMs, should offer an important tool in the medical arsenal for treating obesity in America. In addition, this study identifies policy solutions for sustainability of the Medicare Trust Fund.39 A broad and multipronged approach to reducing obesity in the US, similar to the successful public health initiatives to reduce smoking, is critical to stemming the tide of a growing wave of obesity-related consequences in the very near future.
Supplemental Material
Supplemental material, sj-pdf-1-inq-10.1177_0046958021990516 for Simulating the Fiscal Impact of Anti-Obesity Medications as an Obesity Reduction Strategy by Mina Kabiri, Alison Sexton Ward, Abhilasha Ramasamy, Rebecca Kee, Rahul Ganguly, Brian Gabriel Smolarz, Tracy Zvenyach, James R. Baumgardner and Dana P. Goldman in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Rebecca Kee and James Baumgardner are employees of precisionHEOR, a research consulting firm paid by Novo Nordisk Inc. to conduct this study. Mina Kabiri and Alison Sexton Ward were employees of precisionHEOR at the time that this research was conducted. Abhilasha Ramasamy, B. Gabriel Smolarz, Tracy Zvenyach, and Rahul Ganguly are employees of Novo Nordisk Inc. and hold equity in this company. Dana Goldman was a consultant to precisionHEOR and is a professor at the University of Southern California. He holds equity (<1%) in precisionHEOR; and reports personal fees or honoraria from the Aspen Institute, ACADIA Pharmaceuticals, Amgen, Avanir Pharmaceuticals, and Celgene, outside this study.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by Novo Nordisk Inc.
ORCID iDs: Rebecca Kee  https://orcid.org/0000-0003-0807-8374
https://orcid.org/0000-0003-0807-8374
Brian Gabriel Smolarz  https://orcid.org/0000-0002-8591-3858
https://orcid.org/0000-0002-8591-3858
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Center for Disease Control and Prevention. Obesity and Overweight. 2016. Accessed November 14, 2019. https://www.cdc.gov/nchs/fastats/obesity-overweight.htm
- 2. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang YC, Pamplin J, Long MW, Ward ZJ, Gortmaker SL, Andreyeva T. Severe obesity in adults cost state medicaid programs nearly $8 billion in 2013. Health Aff (Project Hope). 2015;34(11):1923-1931. [DOI] [PubMed] [Google Scholar]
- 4. Apovian CM. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care. 2016;22(7 Suppl):s176-s185. [PubMed] [Google Scholar]
- 5. Allen L, Thorpe K, Joski P. The effect of obesity and chronic conditions on medicare spending, 1987-2011. Pharmacoeconomics. 2015;33(7):691-697. [DOI] [PubMed] [Google Scholar]
- 6. Thorpe KE, Allen L, Joski P. The role of chronic disease, obesity, and improved treatment and detection in accounting for the rise in healthcare spending between 1987 and 2011. Appl Health Econ Health Policy. 2015;13(4):381-387. [DOI] [PubMed] [Google Scholar]
- 7. Goettler A, Grosse A, Sonntag D. Productivity loss due to overweight and obesity: a systematic review of indirect costs. BMJ Open. 2017;7(10):e014632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lehnert T, Sonntag D, Konnopka A, Riedel-Heller S, König H-H. Economic costs of overweight and obesity. Best Pract Res Clin Endocrinol Metabol. 2013;27(2):105-115. [DOI] [PubMed] [Google Scholar]
- 9. Runge CF. Economic consequences of the obese. Diabetes. 2007;56(11):2668-2672. [DOI] [PubMed] [Google Scholar]
- 10. Ricci JA, Chee E. Lost productive time associated with excess weight in the U.S. workforce. Occup Environ Med. 2005;47(12):1227-1234. [DOI] [PubMed] [Google Scholar]
- 11. Klarenbach S, Padwal R, Chuck A, Jacobs P. Population-based analysis of obesity and workforce participation. Obesity (Silver Spring, Md). 2006;14(5):920-927. [DOI] [PubMed] [Google Scholar]
- 12. Bayne-Jones S, Burdette W, Cochran W, et al. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. U.S. Department of Health, Education, and Welfare; 1964. [Google Scholar]
- 13. Huang J, Walton K, Gerzof RB, King BA, Chaloupka FJ. State Tobacco Control Program Spending — United States, 2011. Centers for Disease Control and Prevention; 2015. [PMC free article] [PubMed] [Google Scholar]
- 14. Goldman D, Pierre-Carl M, Lakdawalla D, Zheng Y, Gailey A, Vaynman I. The fiscal consequences of trends in population health. Natl Tax J. 2010;63(2):307-330. [Google Scholar]
- 15. Kabiri M, Sexton Ward A, Ramasamy A, et al. The societal value of broader access to antiobesity medications. Obesity. 2019;28:429-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes Metab Syndr Obes Targets Ther. 2010;3:285-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Oster G, Thompson D, Edelsberg J, Bird AP, Colditz GA. Lifetime health and economic benefits of weight loss among obese persons. Am J Publ Health. 1999;89(10):1536-1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Roehrig C, Miller G., Smoking v. obesity: the economics of prevention and its dependence on treatment. 2016. https://www.healthaffairs.org/do/10.1377/hblog20160222.053270/full/
- 19. Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004;89(6):2583-2589. [DOI] [PubMed] [Google Scholar]
- 20. Baumgardner JR, Bilheimer LT, Booth MB, Carrington WJ, Duchovny NJ, Werble EC. Cigarette taxes and the federal budget—report from the CBO. N Engl J Med. 2012;367(22):2068-2070. [DOI] [PubMed] [Google Scholar]
- 21. Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res. 2004;12(S12):151S-162S. [DOI] [PubMed] [Google Scholar]
- 22. Hampp C, Kang EM, Borders-Hemphill V. Use of prescription antiobesity drugs in the United States. Pharmacotherapy. 2013;33(12):1299-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kohn D. Investigating Fen-Phen. 1999. https://www.cbsnews.com/news/investigating-fen-phen/
- 24. Gomez G, Stanford FC. US health policy and prescription drug coverage of FDA-approved medications for the treatment of obesity. Int J Obes (2005). 2018;42(3):495-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Casazza K, Fontaine KR, Astrup A, et al. Myths, presumptions, and facts about obesity. N Engl J Med. 2013;368(5):446-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Davies MJ, Bergenstal R, Bode B, et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE diabetes randomized clinical trial. JAMA. 2015;314(7):687-699. [DOI] [PubMed] [Google Scholar]
- 27. Lau DC, Krempf M, Astrup A, et al. Liraglutide 3.0 mg reduces body weight and improves cardiometabolic risk factors in adults with overweight/obesity: the SCALE obesity and prediabetes randomised trial. Can J Diabetes. 2015;39:S48-S49. [Google Scholar]
- 28. Wadden TA, Hollander P, Klein S, et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE maintenance randomized study. Int J Obes (Lond). 2013;37(11):1443-1451. [DOI] [PubMed] [Google Scholar]
- 29. Gadde KM, Allison DB, Ryan DH, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomised, placebo-controlled, phase 3 trial. Lancet (Lond, Engl). 2011;377(9774):1341-1352. [DOI] [PubMed] [Google Scholar]
- 30. Garvey WT, Ryan DH, Look M, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr. 2012;95(2):297-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. O’Neil PM, Birkenfeld AL, McGowan B, et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet (Lond, Engl). 2018;392(10148):637-649. [DOI] [PubMed] [Google Scholar]
- 32. Precision Health Economics. Technical documentation: the health economic medical innovation simulation - PSID version. 2018. Accessed December 20, 2018. https://www.precisionmedicinegrp.com/phe/wp-content/uploads/sites/5/2018/12/THEMIS_PSID_appendix.pdf
- 33. Sexton Ward A, Kabiri M, Yucel A, et al. The long-term social value of granulocyte colony-stimulating factors. Am J Manag Care. 2019;25(10):486-493. [PubMed] [Google Scholar]
- 34. Moreno G, van Eijndhoven E, Benner J, Sullivan J. The long-term impact of price controls in medicare part D. Forum Health Econ Policy. 2017;20(2):20. [DOI] [PubMed] [Google Scholar]
- 35. Thornton Snider J, Sullivan J, van Eijndhoven E, et al. Lifetime benefits of early detection and treatment of diabetic kidney disease. PLoS One. 2019;14(5):e0217487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhong L, Tran AT, Tomasino T, Nugent E, Smith JA. Cost-effectiveness of niraparib and olaparib as maintenance therapy for patients with platinum-sensitive recurrent ovarian cancer. J Manage Care Spec Pharm. 2018;24(12):1219-1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Samaranayake NR, Ong KL, Leung RY, Cheung BM. Management of obesity in the National Health and Nutrition Examination Survey (NHANES), 2007-2008. Ann Epidemiol. 2012;22(5):349-353. [DOI] [PubMed] [Google Scholar]
- 39. The Boards of Trustees Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. 2019 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. 2019. [Google Scholar]
- 40. National Institute on Aging. Panel Study of Income Dynamics (PSID). 2019. Accessed November 23, 2019. https://www.nia.nih.gov/research/resource/panel-study-income-dynamics-psid
- 41. Xia Y, Kelton CML, Guo JJ, Bian B, Heaton PC. Treatment of obesity: pharmacotherapy trends in the United States from 1999 to 2010. Obesity. 2015;23(8):1721-1728. [DOI] [PubMed] [Google Scholar]
- 42. Apovian CM, Aronne L, Rubino D, et al. A randomized, phase 3 trial of naltrexone SR/bupropion SR on weight and obesity-related risk factors (COR-II). Obesity (Silver Spring, Md). 2013;21(5):935-943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pi-Sunyer X, Astrup A, Fujioka K, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373(1):11-22. [DOI] [PubMed] [Google Scholar]
- 44. Smith SR, Weissman NJ, Anderson CM, et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. N Engl J Med. 2010;363(3):245-256. [DOI] [PubMed] [Google Scholar]
- 45. Food and Drug Administration. SAXENDA Prescribing Information. 2014. [Google Scholar]
- 46. Yeaw J, Benner JS, Walt JG, Sian S, Smith DB. Comparing adherence and persistence across 6 chronic medication classes. J Manag Care Spec Pharm. 2009;15(9):728-740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bureau of Labor Statistics. Consumer Price Index. 2018. https://www.bls.gov/cpi/.
- 48. Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440-2450. [DOI] [PubMed] [Google Scholar]
- 49. Wang LY, Denniston M, Lee S, Galuska D, Lowry R. Long-term health and economic impact of preventing and reducing overweight and obesity in adolescence. J Adolesc Health. 2010;46(5):467-473. [DOI] [PubMed] [Google Scholar]
- 50. Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who’s paying? Health Aff (Project Hope). 2003;W3:219-226. [DOI] [PubMed] [Google Scholar]
- 51. Kahende J, Malarcher A, England L, et al. Utilization of smoking cessation medication benefits among medicaid fee-for-service enrollees 1999-2008. PLoS One. 2017;12(2):e0170381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Jarlenski M, Hyon Baik S, Zhang Y. Trends in use of medications for smoking cessation in medicare, 2007-2012. Am J Prev Med. 2016;51(3):301-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Baker CL, Ding Y, Ferrufino CP, Kowal S, Tan J, Subedi P. A cost-benefit analysis of smoking cessation prescription coverage from a US payer perspective. CEOR. 2018;10:359-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Michaud P-C, Goldman D, Lakdawalla D, Zheng Y, Gailey A. Understanding the Economic Consequences of Shifting Trends in Population Health. National Bureau of Economic Research; 2009: 2898-2937. [Google Scholar]
- 55. Goldman DP, Zheng Y, Girosi F, et al. The benefits of risk factor prevention in Americans aged 51 years and older. Am J Publ Health. 2009;99(11):2096-2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Goldman DP, Cutler DM, Shang B, Joyce GF. The value of elderly disease prevention. Forum Health Econ Policy. 2006;1:1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Chen F, Su W, Ramasamy A, et al. Ten-year medicare budget impact of increased coverage for anti-obesity intervention. J Med Econ. 2019;22(10):1096-1104. [DOI] [PubMed] [Google Scholar]
- 58. Thorpe KE, Yang Z, Long KM, Garvey WT. The impact of weight loss among seniors on medicare spending. Health Econ Rev. 2013;3(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Granara B, Laurent J. Provider attitudes and practice patterns of obesity management with pharmacotherapy. J Am Assoc Nurse Pract. 2017;29(9):543-550. [DOI] [PubMed] [Google Scholar]
- 60. Group DPPR. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet. 2009;374(9702):1677-1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Herman WH. The cost-effectiveness of diabetes prevention: results from the diabetes prevention program and the diabetes prevention program outcomes study. Clin Diabetes Endocrinol. 2015;1(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-inq-10.1177_0046958021990516 for Simulating the Fiscal Impact of Anti-Obesity Medications as an Obesity Reduction Strategy by Mina Kabiri, Alison Sexton Ward, Abhilasha Ramasamy, Rebecca Kee, Rahul Ganguly, Brian Gabriel Smolarz, Tracy Zvenyach, James R. Baumgardner and Dana P. Goldman in INQUIRY: The Journal of Health Care Organization, Provision, and Financing