Abstract
COVID-19 is a pandemic illness caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV2). It has been estimated that 80% of subject infected are asymptomatic or have mild to moderate symptoms. Differently, in severe cases of COVID-19, cytokine storm, acute respiratory distress syndrome (ARDS), severe systemic inflammatory response and cardiovascular diseases were observed Even if all molecular mechanisms leading to cardiovascular dysfunction in COVID-19 patients remain to be clarified, the evaluation of biomarkers of cardiac injury, stress and inflammation proved to be an excellent tool to identify the COVID-19 patients with worse outcome. However, the number of biomarkers used to manage COVID-19 patients is expected to increase with the increasing knowledge of the pathophysiology of the disease. It is our view that soluble suppressor of tumorigenicity 2 (sST2) can be used as biomarker in COVID-19. sST2 is routinely used as prognostic biomarker in patients with HF. Moreover, high circulating levels of sST2 have also been found in subjects with ARDS, pulmonary fibrosis and sepsis. Keeping in mind these considerations, in this review the possible mechanisms through which the SARS-CoV2 infection could damage the cardiovascular system were summarized and the possible role of sST2 in COVID-19 patients with CVD was discussed.
Keywords: COVID-19, Cardiovascular disease, Inflammation, Suppressor of Tumorigenicity 2, Biomarker
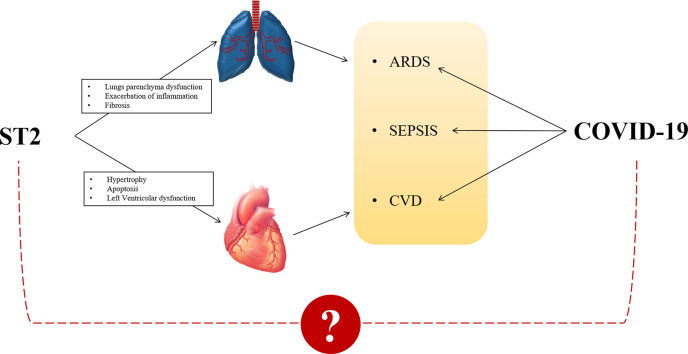
Graphical abstract
1. Introduction
Coronavirus disease-2019 (COVID-19) is a pandemic illness caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV2), a member of coronavirus family [1]. SARS-CoV2 showed high infectivity resulting in rapid global transmission of disease with 53,164,830 confirmed cases and 1,300,576 deaths in the world as of 13 November 2020 [2].
A rapid diagnosis of COVID-19 is essential for lower virus spread among subjects. The laboratory methods that are routinely employed for the COVID-19 diagnosis are Real-Time PCR and deep sequencing test that allow virus genome detection [3]. These tests use the RNA extracted from nose and throat swabs [3]. Generally, the E gene, that encode for envelope protein, is use for the first-line screening, followed by RNA-dependent RNA polymerase (RdRp) gene detection and nucleocapsid (N) gene determination, as additionally confirmatory tests [4]. However, false negative results can be obtained as a consequence of poor quality of specimen or of sample collection in the early stage of the disease [3]. For this reason, serological tests, such as IgM/IgG ELISA assay, should be used for the diagnosis of COVID-19 in combination with Real-Time PCR method [3].
The median SARS-CoV2 incubation period before symptoms manifestation is 4 days [interquartile range (IQR) 2–7 days] [5]. It has been estimated that 80% of subject infected are asymptomatic or have mild to moderate symptoms, such as fever, cough, fatigue, sputum production and shortness of breath [5]. Generally, patients with mild symptoms recover at home with supportive cure and isolation [6]. Differently, the more severe cases of COVID-19 manifest “cytokine storm” followed to acute respiratory distress syndrome (ARDS), severe systemic inflammatory response and consequently multi-organ failure with poorer outcome and even death [1,6,7]. Clinical data suggest that cardiovascular diseases (CVD) are the most common adverse events in COVID-19 progression and that older age, pre-existing hypertension, diabetes, and pre-existing coronary heart disease or heart failure (HF) could be considered important risk factors for a worse prognosis in these patients [1,8,9].
Considering the role of inflammation in the severity of disease, the evaluation of cytokines profile in these patients could be useful for a quick recognition of a worsening in the prognosis and progression of multi-organ failure. Indeed, several studies found increased levels of cytokines [interleukin 6 (IL-6), tumor necrosis factor alpha (TNFα), IL-2] and chemokines [monocyte chemoattractant protein-1 (MCP-1)] in the blood of patients with a fatal outcome of COVID-19 [6,8,10] Moreover, changes in other markers as leucocytosis, lymphocytopenia and neutrophilia are described as important indicators of severe illness [6,10]. In addition to inflammatory markers, other bio-humoral elements such as lactic dehydrogenase (LDH), alanine aminotransferase (ALT), aspartate aminotransferase (AST), creatinine, bilirubin, procalcitonin, D-dimer have been identified for their ability to discriminate COVID-19 patients with poor prognosis [6,10]. Finally, considering that SARS-CoV2 infection combined with systemic inflammatory response could have deleterious effects on cardiovascular system, biomarkers of cardiac stress and injury as B-type natriuretic peptide B (BNP) and cardiac troponin (cTn) T and I were quickly included in the panel of COVID-19 prognostic biomarkers [11,12].
The advantage to use more biomarker for the diagnosis and prognosis of a disease is to ensure a better management of the patients. For this reason, we think that the panel of biomarkers employed in COVID-19 patients should be improved through the addition of soluble suppressor of tumorigenicity 2 (sST2). sST2 is one of more complex known biomarkers whit different role in several diseases. sST2 is routinely used as prognostic biomarker in patients with HF [13]. However, high circulating levels of sST2 have also been found in subjects with ARDS, asthma and sepsis. [14]. With these considerations in mind, it was supposed that sST2 could be taken as common ground among SARS-CoV2 infection and cardiovascular disease (CVD).
In this review, the possible mechanisms through which the SARS-CoV2 infection could damage the cardiovascular system will be summarized. Moreover, the possible role of ST2 in COVID-19 patients with CVD will be discussed.
2. Cardiovascular disease is a common complication in COVID-19 patients
2.1. The phases of COVID-19 progression
The molecular and cellular mechanisms related to SARS-CoV2 infection have not been well clarified. However, it has been proposed to divide the COVID-19 disease progression in three phases [1].
During the first phase, SARS-CoV2 infects the alveolar epithelial cells and begins to proliferate [9]. Data suggested that SARS-CoV2 is able to contact the cell of host by the binding of its spike protein (S) to Angiotensin-Converting Enzyme 2 (ACE2), a membrane-bound glycoprotein [7]. Once internalized into the cell, via endocytosis, SARS-CoV2 released its genome, a positive-sense single-strand RNA, in the cytoplasm of host through a mechanism of membrane fusion mediated by transmembrane serine protease 2 (TMPRSS2) [1,7]. In the cytoplasm, the viral genome is massively replicated and translated in structural and non-structural virus proteins [1,7]. Upon completing the replication phase, the new copies of virus leave the host cell through exocytosis [1,7].
In the second phase of COVID-19 progression the devastating effect of virus on the pulmonary parenchyma can be observed. The replication of virus in the lungs can: reduce the physiological function of ACE2 with dysfunction of renin-angiotensin system (RAS) and pulmonary vasoconstriction; induce extreme epithelial and endothelial apoptosis followed to vascular injury; lead to a massive release of pro-inflammatory cytokines [type I interferon (type1 INF), TNFα, IL-1β and IL-6] and chemokines [chemokine (C-C motif) ligand 3 (CCL3), CCL5, CCL2, and chemokine (C-X-C motif) ligand 10 (CXCL10)] (cytokine storm) and inflammatory cellular infiltration in pulmonary parenchyma [15]. Even if the inflammatory response is a defence mechanism against the virus, a dysregulation of this system was observed in COVID-19 patients [15]. In this subjects the immune composition of lung is altered, with high presence of monocytes/macrophages and aberrant activation of T helper (Th) cell, type 1, 2 and 17 [15]. All these elements contributed to ARDS, pulmonary fibrosis and systemic inflammatory response activation [15].
The third stage of COVID-19 progression is characterized by systemic hyper-inflammatory responses associated with multi-organ failure, in particular to cardiovascular diseases, and worse prognosis of patients [1].
2.1.1. Severe COVID-19 without pulmonary complications
In a recent retrospective study, Dreher et al. showed that severe COVID-19 patients (>60 years, age) do not necessarily develop ARDS even if circulating cytokine levels were high and patients require oxygen therapy for a week [16]. Data suggest that patients that developed ARDS had a pre-existing respiratory disease, were frequently obese and were characterized to persistent elevated levels of IL-6, CRP, D-dimer and LDH compared to patients without ARDS [16].
2.1.2. Severe COVID-19 with extra-pulmonary manifestation
COVID-19 is a syndrome characterized not only by respiratory complication, with varying degrees of severity, but other adverse events may be observed in these patients [17]. SARS-CoV2 principally by indirect ways such as systemic inflammatory response, endothelial dysfunction, coagulopathy and complement activation can induce neurological complication (cerebral hemorrhage and ischemia are found in 36% of old patients), acute kidney injury (AKI) and cardiovascular disease in some cases of severe COVID-19 patients [[17], [18], [19]].
2.2. Cardiovascular disease: Risk factor or result of COVID-19?
It has been estimated that around 40% of deaths in a Wuhan cohort of COVID-19 patients are related to myocardial injury or HF [1,8,9]. At the moment it has not been clarified whether the virus, by direct or indirect effects, can be considered the trigger of onset of complications to the cardiovascular system or if the COVID-19 progression worsening a pre-existing CVD [1,8,9].
2.2.1. Pathophysiological mechanisms of myocardial injury in COVID-19 patients
As previous described ACE2 is the access point of SARS-CoV2 in the host cells. The presence of ACE2 in all cardiac cell types including cardiomyocytes, coronary endothelial cells and cardiac fibroblast gives a plausible theory for a direct viral infection in the heart resulting in cardiac injury [[20], [21], [22], [23], [24], [25]]. Even if only few studies detected SARS-CoV2 genome in cardiac biopsies collected from COVID-19 patients [26], data obtained from patients infected with SARS-CoV1, a virus of the same family of SARS-CoV2, can be used to explain the possible direct actions of SARS-CoV2 in the heart [9,27]. Similar to SARS-CoV2, SARS-CoV1 used ACE2 as access point in cardiac cells. After infection SARS-CoV1 patients showed lower levels of ACE2 in the heart cells with a consequently increased of cardiac injury [9,27]. ACE2 is a monocarboxypeptidase that can cleave both Ang I to Ang (1–9), limiting the substrate for ACE, and Ang II to Ang (1–7), reducing the RAS signal, and increasing the vasodilator, natriuretic/diuretic, and antifibrotic effects by Ang (1–7)/Mas receptor (MasR) pathway [20]. Moreover, an anti-inflammatory role for ACE2/Ang (1–7)/MasR axis was abundantly described in the last years. In a rat model of myocarditis, the use of angiotensin receptor blockers (ARBs) increased ACE2/Ang-(1–7)/MasR resulting in a reduction of leukocyte migration, release of pro-inflammatory cytokines as TNFα, IL-1β, IL-6, IFNγ, and cardiac remodeling [28,29]. Possibly, intracellular translocation of SARS-CoV2 coupled with ACE2 leads to its depletion in cell membranes and the consequent loss of his cardioprotective function [20].
In addition to this direct effect of virus on the heart, there are other reports that describe the indirect effect of SARS-CoV2, such as cardiomyocyte necrosis or left ventricular dysfunction mediated by systemic inflammatory response and, consequently, macrophages and CD4+ T cell infiltrate and release other pro-inflammatory cytokines in the heart [[30], [31], [32]]. The role of inflammation in the heart dysfunction has been well documented. Indeed, on isolated myocytes, TNFα stimulation provokes changes in cells that are relevant to process of left ventricular dysfunction such as myocytes hypertrophy, contractile defects with fetal genes re-expression and apoptosis [[33], [34], [35]]. In particular, stimulation of cardiomyocytes with TNFα resulted in a negative inotropic action by alteration of calcium homeostasis or in an activation of apoptotic response by binding of TNFα to TNF receptor I (TNFRI) [[33], [34], [35]]. Moreover, the chronic stimulation of cardiac fibroblast with TNFα can destroy the balance among the synthesis and the release of matrix metalloproteinase and their inhibitors carried out to extracellular matrix (ECM) degradation and cardiac remodeling [[33], [34], [35], [36]]. Moreover, the pro-inflammatory cytokine IL-1β demonstrated a negative inotropic effect much stronger than TNFα alteration of calcium homeostasis and destruction of the β-adrenergic receptor [36]. This cytokine can contribute also to apoptosis activation in cardiomyocytes and collagen synthesis in fibroblasts resulting in cardiac fibrosis [36]. Similarly, the exposition of cardiomyocytes to high levels of IL-6 depresses the basal contractility of the myocytes as well as the beta-adrenergic responsiveness of the cells leading to decreased heart function [37].
2.2.2. Acute coronary syndrome and acute myocardial infarction
In COVID-19 patients with pre-existing atherosclerotic plaque, high circulating levels of pro-inflammatory mediators such as IL-6, could stimulate endothelial cell to over express adhesion molecule and tissue factor, favouring the recruitment of more leukocytes in atheroma and making the lesion more thrombogenic [18:38]. Moreover, the same inflammatory mediators could stimulate the macrophages within atherosclerotic plaque to release more cytokines and so to promote the progression of disease up to the rupture of fibrous cap inducing acute coronary syndrome (ACS) [38].
The systemic hyper-inflammatory condition typical of SARS-CoV2 infection could contribute to coronary vessels dysfunction also in COVID-19 patients without pre-existing atherosclerotic plaque. Indeed, in these subjects the high circulating levels of IL-6, IL-1β and TNFα could promote endothelial dysfunction and subsequently myocardial ischemia by increased monocytes adhesion to vessel wall and activation of both the extrinsic and intrinsic coagulation pathway in a process defined immune-thrombosis [1,39].
Finally, among the effects of SARS-CoV2 infection, hypoxemia and hypotension, dependent to alveolar dysfunction and systemic inflammation, were described. These conditions reduced the blood flow in the coronary artery and increased the request of myocardial oxygen preparing the heart of COVID-19 patient to ischemia without aterothrombotic plaque disruption (type 2 of myocardial infarction) [1,9,38].
2.3. HF in post-COVID-19 patients
The association between COVID-19 infection and HF has been increasingly demonstrated in the last few months, [40]. It is currently known that myocarditis, endothelial damage, coagulopathies and respiratory failure can be considered as possible risk factors for the onset of HF in severe COVID-19 patients [[40], [41], [42]].
Recently, the researchers are beginning to wonder what will be the long-term consequences of COVID-19 in patients discharged after SARS-CoV2 infection. At the present, no studies have been conducted on post-COVID-19 subjects and many of the hypotheses made on the follow-up of these patients are only suggestions dependent on the data obtained from SARS and MERS survival [[43], [44], [45]]. It has been estimated that around 30% of survivors to SARS and MERS diseases developed pulmonary complications such as fibrosis and hypertension [43,44]. In a recent study, Yu M et al. observed in a cohort of 32 post-COVID-19 patients that 14 subject developed an irreversible pulmonary fibrosis [45]. These patients were older and had higher pulmonary hypertension than non-fibrotic patients [45].
In recovered COVID-19 patients as in post-SARS subjects, irreversible pulmonary fibrosis could develop as a consequence of ARDS and cytokine storm activation after lung virus infection and progress even after eradicating the SARS-CoV2. The exacerbated release of IL-4, IL-8, IL-13, IL-33, IL-6, IL-1β and TNFα by Th2 and macrophages promotes the inflammatory response in the lungs but also the fibroblasts activation and collagen release [46]. The chronic increased of pulmonary resistance could contribute to cardiopulmonary diseases, in particular right ventricle hypertrophy and then HF. At present these are only suggestion and long-term studies in large cohorts are necessary to defined the quality of life and possible complications in post-COVID-19 patients.
3. Biomarkers of cardiac dysfunction in COVID-19 patients
Keeping in mind the relationship among COVID-19 and CVD, the evaluation of biomarkers of cardiac injury, stress and inflammation results essential for risk stratification purposes and for leading to beneficial interventions in patients.
3.1. Cardiac troponins
Circulating cardiac troponins (cTn) T and I are usually used as biomarkers of myocardial injury [acute myocardial infarction (AMI), ACS and myocarditis] but also of HF. From early studies, it became clear that biomarkers of cardiac stress and damage could be used to monitor the outcome of COVID-19 patients. Indeed, the levels of cTnT and cTnI remain in normal range in the majority of COVID-19 survival patients, differently the concentration in the blood of cTns increases together with the severity of disease in the non-survival patients [12,47,48]. In these patients the growth of cTnT and cTnI in the blood were related to myocardial injury, tachycardia, systemic hypoxemia and respiratory failure [12,47]. Retrospective studies confirmed these data and a strong association between elevated high sensitive (hs)-cTnI levels, myocardial injury and increased mortality in patients with severe COVID-19 was validated [49,50]. It was therefore recommended to measure hs-cTnI levels immediately after admission in patients with SARS-CoV2 and to follow any changes of this biomarker over time. In this way it will be possible to promptly intercept the onset of damage to the myocardium in order to be able to intervene accordingly [49,50]. Moreover, in SARS-CoV2 infected patients, increasing levels of cTnI can be correlated with inflammatory biomarkers as IL-6, D-dimer, ferritin and LDH confirming the critical role of inflammatory response on cardiovascular system in COVID-19 patients [12].
3.2. Natriuretic peptide
It is assumed that during SARS-CoV2 infection the reduction of ACE2 function and consequently the hyperstimulation of cardiovascular system by RAS and inflammatory mediators could contribute to increase the release of natriuretic peptides (NPs) [47,51]. Generally, these hormones help to regulate blood volume and arterial blood pressure by promoting vasodilation, diuresis, and natriuresis.
Among the NPs, B-type Natriuretic Peptide (BNP) and N-terminal proBNP (NT-proBNP) are known as gold standard biomarkers for myocardial stress and HF. At this moment only few studies investigated the role of these biomarkers as risk factors for in-hospital death in patients with severe COVID-19 [47,51]. In these works, circulating levels of NT-proBNP showed a dynamic escalation in conjunction with markers of cardiac injury (cTns) and inflammation (IL-1β, CRP, and cardiotrophin I) in older patients with a worse prognosis [47,50,51].
However, these are only pilot studies with few patients and with NT-proBNP was measured only at hospitalization. In the ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic, it was suggested a continuous monitoring of BNP/NT-proBNP in all patients in order to be able to confirm the prognostic value of NPs in severe COVID-19 patients for appropriate therapeutic strategies [52].
3.3. Pro-inflammatory cytokines and chemokines
The systemic inflammatory response dependent on SARS-CoV2 infection can contribute with greater force to the damage in the cardiovascular system, both inducing a new damage or promoting the progression of pre-existing illness.
Several studies confirmed the key role of C reactive protein (CRP), IL-6, IL-10, IL-1β as excellent biomarkers of severity and mortality in COVID-19 disease [[53], [54], [55], [56]]. Circulating levels of CRP are immediately higher in COVID-19 patient who will have a worse outcome [57]. Moreover, in severe COVID-19 patients, increased levels of IL-6, IL-1β and CRP can be related to activation of maladaptive remodeling pathways in different organs (including the heart), atrial fibrillation, in addition to endothelial activation, increased of adhesion molecules production and altered coagulation [[58], [59], [60]].
4. Suppressor of Tumorigenicity 2
In the attempt to improve the management of COVID-19 patients another biomarker could be added to the molecules described above, the Suppressor of Tumorigenicity 2 (ST2).
ST2, a member of IL-1 receptor family, was first described in a murine fibroblast cells line (BALB/c-3 T3) as a factor implicated in cell proliferation and so as element involved in cancer development [61]. Subsequently, the expression of ST2 was found also in other cell types such as macrophages, neutrophils, lymphocytes, endothelial cells, cardiomyocytes, osteoclasts, osteoblasts and adipocytes [62,63].
The ST2 gene is placed on human chromosome 2q12 and gives rise to four transcriptional products. However, only two isoforms, the transmembrane form (ST2L) and the soluble secreted form (sST2), are biologically relevant [62,63]. The ST2L containing 3 extracellular Ig domains, a trans membrane domain, and an intracellular SIR domain homologous of Toll/interleukin-1 receptor (TIR) cytoplasmic domain [64]. Differently, the circulating isoform, sST2, lacks the transmembrane and cytoplasmic domains observed in ST2L and includes only a unique nine amino acid C-terminal sequence [65].
The important roles of ST2 were achieved only after the discovery of its ligand, IL-33 [66]. IL-33 is an alarmin, member of IL-1 cytokine family that can be secreted by most cells type after damage [66]. Once release from damages tissue, IL-33 can bind its receptor ST2L and promote inflammatory responses by the activation of macrophages, mast cells, Th2 and cytokines and chemokines expression [[67], [68], [69]]. The IL-33/ST2L pathway can be locked in the presence of decoy receptor sST2. The soluble receptor binding avidly IL-33 prevents the interaction with ST2L and so the intracellular pathway activation [64].
In the last years, the role of sST2 as diagnostic and prognostic biomarker was discussed for several diseases. In particular, high circulating levels of sST2 were found closely involved to acute and chronic HF, AMI, pulmonary disease as asthma or ARDS, sepsis, fibrosis and gastro-intestinal disease [13,14].
4.1. ST2 in heart disease
As previously described, the ST2 gene can be expressed in several cell types and can be associated at different roles according to the tissue. In the heart, fibroblast and cardiomyocytes are involved in the expression of ST2 gene. Data suggested that the gene expression of IL-33 and ST2 increased in presence of cardiac stress or injury [70,71]. Consequently, IL-33/ST2L system plays a protective role in the heart [70,71]. Indeed, Sanada et al. demonstrated that IL-33/ST2L system abrogates Ang II and phenylephrine- hypertrophy on cardiomyocytes, whereas in mice subjected to overt pressure overload of ventricle, treatment with IL-33 reduced cardiac hypertrophy, fibrosis and premature mortality compared to ST2 knockdown mice [70]. In 2009, Seki et al. using an animal model of ischemia/reperfusion observed that IL-33 treatment reduced apoptosis, improved contractile function and survival in treated group compared to control group [71]. Moreover, it was found that sST2 is able to abrogate these protective pathways seizing IL-33. Indeed, sST2 reversed the anti-hypertrophic effect of IL-33 in cardiomyocytes stimulates with Ang II or phenylephrine [70]. Moreover, the pre-incubation of IL-33 with sST2 reduces the beneficial effects of IL-33/ST2L signalling in cardiomyocytes exposed for 72 h' to a hypoxia state [71].
Several studies showed that circulating levels of sST2, but not circulating levels of IL-33, were higher in patient with AMI but also in patient with acute and chronic HF and these levels correlated with cardiac remodeling, reduction of ejection fraction and neurohormonal derangement [[72], [73], [74], [75]]. The guidelines ACCF/AHA classified sST2 as a new prognostic biomarker for risk assessment of myocardial fibrosis and for predicting heart disease and life-threatening events [13]. The cut-off proposed for this new prognostic biomarker is 35 ng/mL (the measures are performed by Presage ST2 assay) [13]. It was found that increased levels of sST2 (>35 ng/mL) were always closely related with elevated mortality in patients with chronic HF, and that sST2 was a better predictor of long-term cardiovascular death that NPs for HF patients [76,77].
4.2. ST2 and pulmonary disease
Differently from the cardioprotective effect described for IL-33/ST2 system in the heart, data suggested a crucial role for this pathway in the pathogenesis and progression of lung disease [14].
As well-known IL-33 is an alarmin-cytokine that can be quickly released from endothelial alveolar cell after infection, stress or necrotic events. In the pathogenesis of pulmonary diseases such as asthma, growing levels of IL-33 promote the activation of inflammatory response by the interaction with ST2L [78]. In particular, IL-33/ST2L system induced the activation of mast cells, the differentiation of Th0 cell in Th2 and, consequently, the expression and release of pro-inflammatory cytokines, such as IL-6, IL-1β, TNFα and chemokines such as IL-8, IL-4, IL-5 and IL-13 [78]. The chemokines promote the recruitment of other inflammatory cells in the damaged tissue and the progression of inflammatory responses [78]. In murine model of asthma, Lohning et al. showed that the use of antibody against ST2L was able to reduce the activation of Th2 cell and so could reduce the severity of an inflammatory response in the lungs [79]. Similar results were obtained when the animal model was pre-treated with sST2 [80].
Overexpression of sST2 was found in asthmatic population compared to healthy subjects [81]. High levels of decoy receptor could suggest a natural mechanism to regulate the inflammation in the lungs, turning off IL-33/ST2L signalling. It was supposed that, in the severe cases of asthma, the IL-33 removal by sST2 binding promotes the differentiation of Th0 in Th1 and consequently exacerbates the pro-inflammatory process [14]. However, dedicated studies will be needed to confirm these assumptions. To date, it was found that when the circulating levels of sST2 were combined with neutrophilia provided a worse outcome for asthma patients [81].
In addition to allergic pulmonary disease, the pro-inflammatory effect of IL-33/ST2L axis was observed in ARDS patients [14]. ARDS can be the result of a direct insult, as pneumonia, or an indirect insult, as sepsis. Anyway, ARDS is characterized by a great release of pro-inflammatory cytokines (cytokines storm), neutrophils recruitment in the lungs, and alveolar endothelial barrier disruption [14,82]. In 2011, Le Goffic et al. observed the expression levels of IL-33 and other cytokines in mice treated with the influenza virus A/WSN/1933 (H1N1) [78]. The data showed that, until three days after infection, mRNA and protein levels of IL-33 increased both in pulmonary tissue and bronchoalveolar lavage in correlation with IL-6, TNFα and INFγ, suggesting that IL-33/ST2L system could play a role in the exacerbation of ARDS by cytokines storm induction, as described for asthmatic population [78]. These results are confirmed in an in vitro study, where the authors observed that the concentration of IL-33 in the media of epithelial cell infected with H1N1virus increased with the necrotic event [78].
However, in patients with ARDS circulating levels of IL-33 were lower. Differently, high circulating levels of sST2 (approximately ten times above those expected in HF) were found in ARDS patients and their relationship with worse severity disease and higher mortality rate have been verified [83,84].
Finally, the IL-33/ST2 system is involved in the pulmonary fibrosis. In vivo studies found that after the treatment of mice with pro-fibrotic drugs such as bleomycin, the expression levels of IL-33 increased simultaneously to pulmonary fibrosis [[85], [86], [87]]. In particular, the data suggest that the IL-33/ST2L pathway induces the polarization and activation of Th2 with a consequent release of IL-4, IL-5 and IL-13 [[85], [86], [87]]. These cytokines promote the differentiation of macrophages in type 2 macrophages (M2) and the activation of fibroblasts with consequently pulmonary extracellular matrix remodeling [85;87]. Li et al. showed that the pro-fibrotic effects of bleomycin decreased in mice after the use of ST2 antibody or silencing the ST2 gene [87]. In a retrospective study, Tajima et al. found that the circulating levels of sST2 were significantly higher in a group of 49 patients with idiopathic pulmonary fibrosis compared to control [88]. These data suggested the possibility to use sST2 as biomarker of pulmonary fibrosis [88].
4.3. ST2 and sepsis
Sepsis is defined as dysregulated inflammatory response of host to infection that can lead to multiple organ dysfunction [89]. Generally, many inflammatory cells such as macrophages, mast cells, neutrophils and Th2 are activated during sepsis and a large amount of cytokines (IL-2, IL-4, IL-6 and IL-10) and chemokines (IL-8) are released [89]. Immuno-paralysis, vasodilation, hypoxia, endothelial dysfunction and immune-thrombosis are some of the effects related to high production of pro-inflammatory and anti-inflammatory cytokines within sepsis [89].
During the last years it has become clear that sepsis is able to cause elevation in circulating levels of sST2 that is independent from the source of infection [90,91]. Serum levels of sST2 were found higher in non-survival sepsis patients compared to survival and healthy subjects [21;90–91]. Moreover, the circulating levels of sST2 were related to IL-6, IL-8 and IL-10 levels in the blood of sepsis patients [14;90–91]. However, the levels of IL-6, IL-8 and IL-10 tended to decrease within 5 days from the beginning of the sepsis [14;90]. Differently, the circulating levels of sST2 remain elevated in non-survivor patients even after 14 days from the onset of the disease [14;90–91]. The data collected suggest the use of sST2 as prognostic biomarker in subject with sepsis [14;89].
Unfortunately, the molecular mechanisms regulated by IL-33/ST2 system in the sepsis patients remain to be clarified. Hoogerwerf JJ et al. suggested that IL-33/ST2 system was involved in the differentiation of Th cells from Th0 to Th2 during sepsis and that the circulating levels of sST2 were directly correlated with the number of Th2 activated in these patients [90]. Other studies suggested that circulating levels of sST2 were related to degree of endothelial dysfunction [14]. Considering that the vessel wall is subjected to several insults in sepsis patients, it has been speculated that the fibroblast underneath the vascular endothelium produce sST2 and that the decoy receptor for IL-33 can be released in the blood only after endothelial disruption [14].
5. COVID-19 and sST2
Cytokines storm, ARDS, fibrosis, systemic inflammatory state and cardiovascular diseases are the most common severe complications observed in COVID-19 patients. Based on what has just been described in relation to the levels of sST2 in ARDS patients, it seems theoretically correct to assume that after infection of lungs by SARS-CoV2 and cytokines storm activation, the circulating levels of decoy receptor for IL-33 could increase dramatically in the blood in the same manner observed for the other inflammatory mediators [47,[53], [54], [55], [56]]. High sST2 concentration in the blood could affect the anti-hypertrophic and anti-apoptotic role of IL-33/ST2L system in the heart, contributing as IL-6 and TNFα to myocardial remodeling and worse outcome of COVID-19 patients.
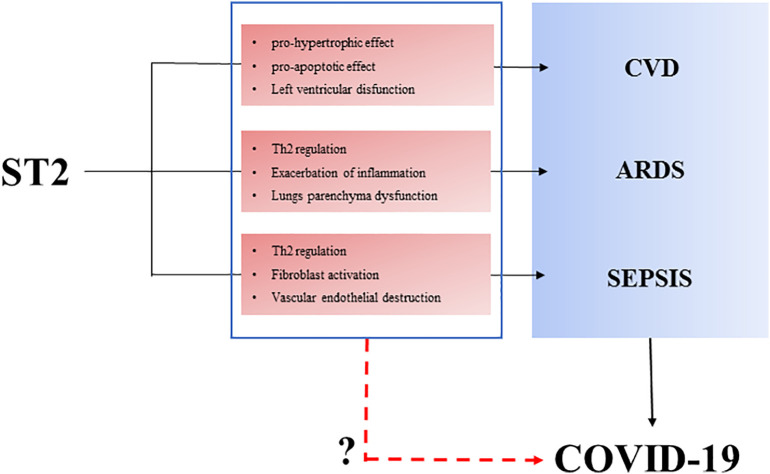
Analysis of the circulating levels of sST2 in the blood and of cardiac expression on IL-33 and ST2 genes in the heart of COVID-19 patients will be needed to provide information about the involvement of these elements in the pathogenesis of disease and, eventually, to take into account a role for sST2 as prognostic biomarker in SARS-CoV2 infected patients (Fig. 1 ).
Fig. 1.
Possible role of ST2 in COVID-19 disease. Cardiovascular disease (CVD), acute respiratory distress syndrome (ARDS) and sepsis are described among the main complications of SARS-CoV2 infection. ST2 is involved in all these diseases. In cardiovascular system, high circulating levels of soluble ST2 (sST2) are associated with pro-hypertrophic and pro-apoptotic pathway activation and consequently with a reduction of left ventricular physiological function. In the lungs, ST2 is involved in alveolar parenchyma disruption by activation of inflammatory processes (Th2 differentiation and cytokines production). Similarly, during sepsis, ST2 can contribute to exacerbation of inflammatory response, activation of fibroblast, and endothelial disruption. The questions are: due to the pro-inflammatory, profibrotic, pro-hypertrophic and pro-apoptotic role described for ST2, could ST2 be involved in the effects of SARS-CoV2 in the lung and in the cardiovascular system? Moreover, will it be possible to use ST2 as a prognostic biomarker in COVID-19 patients?
Finally, keeping in mind that pulmonary fibrosis could be the secondary complication in the post-COVID-19 patients and that IL-33/ST2 system is involved in fibroblast activation and extracellular matrix remodeling, the evaluation of circulating levels of sST2 could be used as prognostic biomarker in discharge COVID-19 patients. Obviously these are only hypotheses. Appropriate studies will clarify the long-term complications and the possible role of sST2 in post-COVID patients.
Very recently, Zeng Z et al. studied the role of sST2 in COVID-19 and its relationship with inflammatory status and disease severity, suggesting that monitoring of serum sST2 could be helpful in the early screening of inflammatory status and critical illness of COVID-19 [92,93].
6. Conclusion
Although the molecular and cellular mechanisms leading to cardiovascular dysfunction in COVID-19 patients remain to be clarified, the excessive release of pro-inflammatory mediators in the blood from infected lungs would appear the main tool of SARS-CoV2 to damage the cardiovascular system and so to worse the prognosis of patients.
In this review, it has been speculated the possible employed of sST2, the decoy receptor of IL-33, in the management of COVID-19 patients. It is known that high circulating levels of sST2 are involved in the aberrant inflammatory process of ARDS patients, whereas are engaged in hypertrophy and apoptosis processes of HF subjects.
At the moment, the use of sST2 as marker of prognosis for COVID-19 remains merely a hypothesis. For this reason, new rigorous investigation will be necessary before to clarify its role in SARS-CoV2 infection. Increasing the number of information on COVID-19 patients by expanding the number of biomarkers used to date represents an opportunity to learn more about the pathophysiology of disease and to start thinking about adequate pharmacological treatments in order to improve patient outcome.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Atri D., Siddiqi H.K., Lang J., et al. COVID-19 for the cardiologist: a current review of the virology, clinical epidemiology, cardiac and other clinical manifestations and potential therapeutic strategies. JACC Basic Transl. Sci. 2020;10 doi: 10.1016/j.jacbts.2020.04.002. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization 2020. https://www.who.int/publications/m/item/weekly-operational-update-on-covid-19---13-november-2020
- 3.Guo L., Ren L., Yang S., et al. Profiling early humoral response to diagnose novel coronavirus disease (COVID-19) Clin. Infect. Dis. 2020;21 doi: 10.1093/cid/ciaa310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lippi G., Mattiuzzi C., Bovo C., Plebani M. Current laboratory diagnostics of coronavirus disease 2019 (COVID-19) Acta Biomed. 2020;91(2):137–145. doi: 10.23750/abm.v91i2.9548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;18:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frater J.L., Zini G., d'Onofrio G., Rogers H.J. COVID-19 and the clinical hematology laboratory. Int. J. Lab. Hematol. 2020;20 doi: 10.1111/ijlh.13229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou P., Yang X.L., Wang X.G., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruan Q., Yang K., Wang W., et al. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intens. Care Med. Intens. Care Med. 2020;5:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akhmerov A., Marban E. COVID-19 and the Heart. Circ. Res. 2020;10 doi: 10.1161/CIRCRESAHA.120.317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;10223:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi S., Qin M., Shen B., et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yancy C.W., Jessup M., Bozkurt B., et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2013;128:240–327. doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 14.Homsak E., Gruson D. Soluble ST2: a complex and diverse role in several diseases. Clin. Chim. Acta. 2020;507:75–87. doi: 10.1016/j.cca.2020.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Yang P., Gu H., Zhao Z., et al. Angiotensin-converting enzyme 2 (ACE2) mediates influenza H7N9 virus-induced acute lung injury. Sci. Rep. 2014;4:7027. doi: 10.1038/srep07027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dreher M., Kersten A., Bickenbach J., et al. The characteristics of 50 hospitalized COVID-19 patients with and without ARDS. Dtsch. Arztebl. Int. 2020;117:271–278. doi: 10.3238/arztebl.2020.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Romagnoli S., Peris A., De Gaudio A.R., Geppetti P. SARS-CoV-2 and COVID-19: from the bench to the bedside. Physiol. Rev. 2020;100:1455–1466. doi: 10.1152/physrev.00020.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Del Turco S., Vianello A., Ragusa R., Caselli C., Basta G. COVID-19 and cardiovascular consequences: Is the endothelial dysfunction the hardest challenge? Thromb. Res. 2020;196:143–151. doi: 10.1016/j.thromres.2020.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Munhoz R.P., Pedroso J.L., Nascimento F.A., et al. Neurological complications in patients with SARS-CoV-2 infection: a systematic review. Arq. Neuropsiquiatr. 2020;78:290–300. doi: 10.1590/0004-282x20200051. [DOI] [PubMed] [Google Scholar]
- 20.Abassi Z., Assady S., Khoury E.E., Heyman S.N. Letter to the editor: angiotensin-converting enzyme 2: an ally or a Trojan horse? Implications to SARS-CoV-2-related cardiovascular complications. Am. J. Physiol. Heart Circ. Physiol. 2020;5:H1080–H1083. doi: 10.1152/ajpheart.00215.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tipnis S.R., Hooper N.M., Hyde R., et al. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J. Biol. Chem. 2000;275:33238–33243. doi: 10.1074/jbc.M002615200. [DOI] [PubMed] [Google Scholar]
- 22.Burrell L.M., Risvanis J., Kubota E., et al. Myocardial infarction increases ACE2 expression in rat and humans. Eur. Heart J. 2005;26:369–375. doi: 10.1093/eurheartj/ehi114. [DOI] [PubMed] [Google Scholar]
- 23.Gallagher P.E., Ferrario C.M., Tallant E.A. Regulation of ACE2 in cardiac myocytes and fibroblasts. Am. J. Physiol. Heart Circ. Physiol. 2008;295:H2373–H2379. doi: 10.1152/ajpheart.00426.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Inciardi R.M., Lupi L., Zaccone G., et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:819–824. doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu H., Ma F., Wei X., Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur. Heart J. 2021;42:206. doi: 10.1093/eurheartj/ehaa190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tavazzi G., Pellegrini C., Maurelli M., et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur. J. Heart Fail. 2020;22:911–915. doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oudit G.Y., Kassiri Z., Jiang C., et al. SARScoronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur. J. Clin. Investig. 2009;39:618–625. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.e Silva A.C. Simões, Silveira K.D., Ferreira A.J., Teixeira M.M. ACE2, angiotensin-(1–7) and Mas receptor axis in inflammation and fibrosis. Br. J. Pharmacol. 2013;169:477–492. doi: 10.1111/bph.12159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sukumaran V., Veeraveedu P.T., Gurusamy N., et al. Cardioprotective effects of telmisartan against heart failure in rats induced by experimental autoimmune myocarditis through the modulation of angiotensin-converting enzyme-2/angiotensin 1-7/mas receptor axis. Int. J. Biol. Sci. 2011;7:1077–1092. doi: 10.7150/ijbs.7.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yao X.H., Li T.Y., He Z.C., et al. A pathological report of three covid-19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi. 2020;49:E009. doi: 10.3760/cma.j.cn112151-20200312-00193. [DOI] [PubMed] [Google Scholar]
- 31.Xu Z., Shi L., Wang Y., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aretz H.T. Myocarditis: the Dallas criteria. Hum. Pathol. 1987;18:619–624. doi: 10.1016/s0046-8177(87)80363-5. [DOI] [PubMed] [Google Scholar]
- 33.Krown K.A., Page M.T., Nguyen C., et al. Tumor necrosis factor alpha-induced apoptosis in cardiac myocytes: involvement of the sphingolipid signalingcascade in cardiac cell death. J. Clin. Invest. 1996;98:2854–2865. doi: 10.1172/JCI119114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yokoyama T., Nakano M., Bednarczyk J.L., et al. Tumor necrosis factor-α provokes a hypertrophic growth response in adult cardiac myocytes. Circulation. 1997;95:1247–1252. doi: 10.1161/01.cir.95.5.1247. [DOI] [PubMed] [Google Scholar]
- 35.Kubota T., Bounoutas G.S., Miyagishima M., et al. Soluble tumor necrosis factor receptor abrogates myocardial inflammation but not hypertrophy in cytokine-induced cardiomyopathy. Circulation. 2000;101:2518–2525. doi: 10.1161/01.cir.101.21.2518. [DOI] [PubMed] [Google Scholar]
- 36.Hanna A., Frangogiannis N.G. Inflammatory cytokines and chemokines as therapeutic targets in heart failure. Cardiovasc. Drugs Ther. 2020;34:849–863. doi: 10.1007/s10557-020-07071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prabhu S.D., Frangogiannis N.G. The biological basis for cardiac repair after myocardial infarction: from inflammation to fibrosis. Circ. Res. 2016;119:91–112. doi: 10.1161/CIRCRESAHA.116.303577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Libby P. The heart in COVID19: primary target or secondary bystander? JACC Basic Transl. Sci. 2020;5:537–542. doi: 10.1016/j.jacbts.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Henry B.M., Vikse J., Benoit S., et al. Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: A novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. Clin. Chim. Acta. 2020;507:167–173. doi: 10.1016/j.cca.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Adeghate E.A., Eid N., Singh J. Mechanisms of COVID-19-induced heart failure: a short review. Heart Fail. Rev. 2020;16:1–7. doi: 10.1007/s10741-020-10037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Amraei R., Rahimi N. COVID-19, renin-angiotensin system and endothelial dysfunction. Cells. 2020;7:1652. doi: 10.3390/cells9071652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mikami T., Miyashita H., Yamada T., Harrington M., Steinberg D., Dunn A., Siau E. Risk factors for mortality in patients with COVID-19 in New York City. J. Gen. Intern. Med. 2020;30:1–10. doi: 10.1007/s11606-020-05983-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spagnolo P., Balestro E., Aliberti S., et al. Pulmonary fibrosis secondary to COVID-19: a call to arms? Lancet Respir. Med. 2020;S2213-2600:30222–30228. doi: 10.1016/S2213-2600(20)30222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.George P.M., Wells A.U., Jenkins R.G. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir. Med. 2020;S2213-2600 doi: 10.1016/S2213-2600(20)30225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yu M., Liu Y., Xu D., et al. Prediction of the development of pulmonary fibrosis using serial thin-section CT and clinical features in patients discharged after treatment for COVID-19 pneumonia. Korean J. Radiol. 2020;6:746–755. doi: 10.3348/kjr.2020.0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kotsiou O.S., Gourgoulianis K.I., Zarogiannis S.G. IL-33/ST2 Axis in organ fibrosis. Front. Immunol. 2018;9:2432. doi: 10.3389/fimmu.2018.02432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Guo T., Fan Y., Chen M., et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lala A., Johnson K.W., Januzzi J.L., et al. Mount sinai COVID informatics center. prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J. Am. Coll. Cardiol. 2020;76:533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Michela S., Barbara B., Cioffi S.M.G., et al. Association between cardiac troponin I and mortality in patients with COVID-19. Biomarkers. 2020;2:1–22. doi: 10.1080/1354750X.2020.1831609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stefanini G.G., Chiarito M., Ferrante G., et al. Humanitas COVID-19 task force. Early detection of elevated cardiac biomarkers to optimise risk stratification in patients with COVID-19. Heart. 2020;106:1512–1518. doi: 10.1136/heartjnl-2020-317322. [DOI] [PubMed] [Google Scholar]
- 51.Gao L., Jiang D., Wen X.S., et al. Prognostic value of NT-proBNP in patients with severe COVID-19. Respir. Res. 2020;1:83. doi: 10.1186/s12931-020-01352-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.The European Society for Cardiology ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. 2020. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESCCOVID-19-Guidance (Last update: 28 May 2020)
- 53.Burian E., Jungmann F., Kaissis G.A., et al. Intensive care risk estimation in COVID-19 pneumonia based on clinical and imaging parameters: experiences from the Munich cohort. J. Clin. Med. 2020;9:1514. doi: 10.3390/jcm9051514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen X., Zhao B., Qu Y., et al. Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely correlated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients. Clin. Infect. Dis. 2020;71:1937–1942. doi: 10.1093/cid/ciaa449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chi Y., Ge Y., Wu B., et al. Serum cytokine and chemokine profile in relation to the severity of coronavirus disease 2019 (COVID-19) in China. J. Infect. Dis. 2020;222:746–754. doi: 10.1093/infdis/jiaa363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gao Y., Li T., Han M., et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J. Med. Virol. 2020;92:791–796. doi: 10.1002/jmv.25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tan C., Huang Y., Shi F., et al. C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J. Med. Virol. 2020;92:856–862. doi: 10.1002/jmv.25871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu P.P., Blet A., Smyth D., Li H. The science underlying COVID-19:implications for the cardiovascular system. Circulation. 2020;142:68–78. doi: 10.1161/CIRCULATIONAHA.120.047549. [DOI] [PubMed] [Google Scholar]
- 60.Bruins P., te Velthuis H., Yazdanbakhsh A.P., et al. Activation of the complement system during and after cardiopulmonary bypass surgery: postsurgery activation involves C-reactive protein and is associated with postoperative arrhythmia. Circulation. 1997;96:3542–3548. doi: 10.1161/01.cir.96.10.3542. [DOI] [PubMed] [Google Scholar]
- 61.Tominaga S. A putative protein of a growth specific cDNA from BALB/c-3T3 cells is highly similar to the extracellular portion of mouse interleukin 1 receptor. FEBS Lett. 1989;258:301–304. doi: 10.1016/0014-5793(89)81679-5. [DOI] [PubMed] [Google Scholar]
- 62.Yanagisawa K., Takagi T., Tsukamoto T., et al. Presence of a novel primary response gene ST2L, encoding a product highly similar to the interleukin 1 receptor type 1. FEBS Lett. 1993;318:83–87. doi: 10.1016/0014-5793(93)81333-u. [DOI] [PubMed] [Google Scholar]
- 63.Tominaga S., Kuroiwa K., Tago K., et al. Presence and expression of a novel variant form of ST2 gene product in human leukemic cell line UT-7/GM. Biochem. Biophys. Res. Commun. 1999;264:14–18. doi: 10.1006/bbrc.1999.1469. [DOI] [PubMed] [Google Scholar]
- 64.Pascual-Figal D.A., Januzzi J.L. The biology of ST2: the international ST2 consensus panel. Am. J. Cardiol. 2015;115:3B–7B. doi: 10.1016/j.amjcard.2015.01.034. [DOI] [PubMed] [Google Scholar]
- 65.Gächter T., Werenskiold A.K., Klemenz R. Transcription of the interleukin-1 receptor-related T1 gene is initiated at different promoters in mast cells and fibroblasts. J. Biol. Chem. 1996;271:124–129. doi: 10.1074/jbc.271.1.124. [DOI] [PubMed] [Google Scholar]
- 66.Schmitz J., Owyang A., Oldham E., et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23:479–490. doi: 10.1016/j.immuni.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 67.Demyanets S., Konya V., Kastl S.P., et al. Interleukin-33 induces expression of adhesion molecules and inflammatory activation in human endothelial cells and in human atherosclerotic plaques. Arterioscler. Thromb. Vasc. Biol. 2011;31:2080–2089. doi: 10.1161/ATVBAHA.111.231431. [DOI] [PubMed] [Google Scholar]
- 68.Kakkar R., Hei H., Dobner S., Lee R.T. Interleukin 33 as a mechanically responsive cytokine secreted by living cells. J. Biol. Chem. 2012;287:6941–6948. doi: 10.1074/jbc.M111.298703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Miller A.M., Liew F.Y. The IL-33/ST2 pathway—a new therapeutic target in cardiovascular disease. Pharmacol. Ther. 2011;131:179–186. doi: 10.1016/j.pharmthera.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 70.Sanada S., Hakuno D., Higgins L.J., Schreiter E.R., McKenzie A.N., Lee R.T. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J. Clin. Invest. 2007;117:1538–1549. doi: 10.1172/JCI30634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Seki K., Sanada S., Kudinova A.Y., et al. Interleukin-33 prevents apoptosis and improves survival after experimental myocardial infarction through ST2 signaling. Circ. Heart Fail. 2009;2:684–691. doi: 10.1161/CIRCHEARTFAILURE.109.873240. [DOI] [PubMed] [Google Scholar]
- 72.Weinberg E.O., Shimpo M., De Keulenaer G.W., MacGillivray C., Tominaga S., Solomon S.D., Rouleau J.L., Lee R.T. Expression and regulation of ST2, an interleukin-1 receptor family member, in cardiomyocytes and myocardial infarction. Circulation. 2002;106:2961–2966. doi: 10.1161/01.CIR.0000038705.69871.D9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Weinberg E.O., Shimpo M., Hurwitz S., Tominaga S., Rouleau J.L., Lee R.T. Identification of serum soluble ST2 receptor as a novel heart failure biomarker. Circulation. 2003;107:721–726. doi: 10.1161/01.cir.0000047274.66749.fe. [DOI] [PubMed] [Google Scholar]
- 74.Januzzi J.L., Peacock W.F., Maisel A.S., et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (pro-brain natriuretic peptide investigation of dyspnea in the emergency department) study. J. Am. Coll. Cardiol. 2007;50:607–613. doi: 10.1016/j.jacc.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 75.Caselli C. Inflammation in cardiac disease: focus on Interleukin-33/ST2 pathway. Inflamm. Cell Signal. 2014;1 [Google Scholar]
- 76.Ky B., French B., McCloskey K., et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ. Heart Fail. 2011;2:180–187. doi: 10.1161/CIRCHEARTFAILURE.110.958223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Felker G.M., Fiuzat M., Thompson V., et al. Soluble ST2 in ambulatory patients with heart failure: association with functional capacity and long-term outcomes. Circ. Heart Fail. 2013;6:1172–1179. doi: 10.1161/CIRCHEARTFAILURE.113.000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Le Goffic R., Arshad M.I., Rauch M., et al. Infection with influenza virus induces IL-33 in murine lungs. Am. J. Respir. Cell Mol. Biol. 2011;45:1125–1132. doi: 10.1165/rcmb.2010-0516OC. [DOI] [PubMed] [Google Scholar]
- 79.Lohning M., Stroehmann A., Coyle A.J., et al. T1/ST2 is preferentially expressed on murine Th2 cells, independent of interleukin 4, interleukin 5, and interleukin 10, and important for Th2 effector function. PNAS. 1998;12:6930–6935. doi: 10.1073/pnas.95.12.6930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hayakawa H., Hayakawa M., Kume A., Tominaga S. Soluble ST2 blocks interleukin-33 signaling in allergic airway inflammation. J. Biol. Chem. 2007;282:26369–26380. doi: 10.1074/jbc.M704916200. [DOI] [PubMed] [Google Scholar]
- 81.Watanabe M., Nakamoto K., Inui T., et al. Serum sST2 levels predict severe exacerbation of asthma. Respir. Res. 2018;19:169. doi: 10.1186/s12931-018-0872-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhao J., Zhao Y. Interleukin-33 and its receptor in pulmonary inflammatory diseases. Crit. Rev. Immunol. 2015;35:451–461. doi: 10.1615/CritRevImmunol.2016015865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bajwa E.K., Volk J.A., Christiani D.C., et al. Prognostic and diagnostic value of plasma soluble suppression of tumorigenicity-2 concentrations in acute respiratory distress syndrome. Crit. Care Med. 2013;41:2521–2531. doi: 10.1097/CCM.0b013e3182978f91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bajwa E.K., Mebazaa A., Januzzi J.L. ST2 in pulmonary disease. Am. J. Cardiol. 2015;115 doi: 10.1016/j.amjcard.2015.01.040. [DOI] [PubMed] [Google Scholar]
- 85.Gao Q., Li Y., Pan X., et al. Lentivirus expressing soluble ST2 alleviates bleomycin-induced pulmonary fibrosis in mice. Int. Immunopharmacol. 2016;30:188–193. doi: 10.1016/j.intimp.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 86.Xu J., Zheng J., Song P., et al. IL33/ST2 pathway in a bleomycin induced pulmonary fibrosis model. Mol. Med. Rep. 2016;14:1704–1708. doi: 10.3892/mmr.2016.5446. [DOI] [PubMed] [Google Scholar]
- 87.Li D., Guabiraba R., Besnard A.G., et al. IL-33 promotes ST2-dependent lung fibrosis by the induction of alternatively activated macrophages and innate lymphoid cells in mice. J. Allergy Clin. Immunol. 2014;134:1422–1432. doi: 10.1016/j.jaci.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tajima S., Oshikawa K., Tominaga S., Sugiyama Y. The increase in serum soluble ST2 protein upon acute exacerbation of idiopathic pulmonary fibrosis. Chest. 2003;124:1206–1214. doi: 10.1378/chest.124.4.1206. [DOI] [PubMed] [Google Scholar]
- 89.Xu H., Turnquist H.R., Hoffman R., Billiar T.R. Role of the IL-33-ST2 Axis in Sepsis. Mil. Med. Res. 2017;4:3. doi: 10.1186/s40779-017-0115-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hoogerwerf J.J., Tanck M.W., van Zoelen M.A., et al. Soluble ST2 plasma concentrations predict mortality in severe sepsis. Intensive Care Med. 2010;36:630–637. doi: 10.1007/s00134-010-1773-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hack C.E., Aarden L.A., Thijs L.G. Role of cytokines in sepsis. Adv. Immunol. 1997;66:101–195. doi: 10.1016/s0065-2776(08)60597-0. [DOI] [PubMed] [Google Scholar]
- 92.Zeng Z., Hong X.Y., Li Y., et al. Serum-soluble ST2 as a novel biomarker reflecting inflammatory status and illness severity in patients with COVID-19. Biomark. Med. 2020:1619–1629. doi: 10.2217/bmm-2020-0410. [DOI] [PubMed] [Google Scholar]
- 93.Zizzo G., Cohen P.L. Imperfect storm: is interleukin-33 the Achilles heel of COVID-19? Lancet Rheumatol. 2020:e779–e790. doi: 10.1016/S2665-9913(20)30340-4. [DOI] [PMC free article] [PubMed] [Google Scholar]