Abstract
Introduction
Our study describes changes in HIV care service delivery and continuity of HIV antiretroviral therapy (ART) for people living with HIV (PLHIV) during the 8 weeks before and after diagnosis of the first coronavirus disease 2019 (COVID-19) cases in Haiti on March 19, 2020.
Methods
Using data from 96 out of 167 health facilities offering ART services, we compared four ART program indicators: (1) count of HIV visits; (2) proportion of ART dispenses in community-based settings (DAC); (3) proportion of multi-month dispensing of ART medications > 6 months (> 6 m MMD); and (4) proportion of timely ART refills. We used uncontrolled interrupted time series (ITS) models to estimate slope and level changes in each indicator with the arrival of COVID-19.
Results and Discussion
From week 1 to week 16, the average number of HIV visits fell from 121.5 to 92.5 visits, the proportion of DAC rose from 22.7% to 36.7%, the proportion of > 6 m MMD rose from 29.4% to 48.4%, and the proportion of timely ART refills fell from 51.9% to 43.8%. The ITS models estimated abrupt increases of 36% in > 6 m MMD (p < 0.001) and 37% in DAC (p < 0.001) at the time of COVID-19 arrival, and no change after arrival of COVID-19. The was an abrupt decline of 18% in timely ART refills with the arrival of COVID-19 and a decline of 1% per week thereafter, both non-statistically significant changes.
Conclusions
The sudden changes in HIV service utilization represent dramatic adaptations needed to mitigate primary and secondary effects of the COVID-19 pandemic on PLHIV. This study underscores the urgency of optimizing ART delivery models in Haiti and beyond, in order to maintain progress toward HIV epidemic control.
Keywords: COVID-19 pandemic, HIV/AIDS, Haiti, Service disruption
Introduction
The global coronavirus disease 2019 (COVID-19) pandemic has had both primary and secondary effects on population health. By December 1, 2020, there were more than 65 million cases and 1.5 million deaths attributed to the global pandemic [1]. The World Health Organization (WHO) has warned of grave consequences of COVID-19-related disruptions to health systems and the vulnerability of hard-won gains in programs for controlling human immunodeficiency virus (HIV), tuberculosis and other diseases [2, 3]. Haiti’s Ministry of Public Health and Population (MSPP) announced the first confirmed cases of COVID-19 on March 19, 2020 and by December 1, 2020 reported more than 37,000 suspected cases, 9,347 confirmed cases and 233 deaths [1, 4].
Haiti has a generalized HIV epidemic: the national prevalence rate is estimated at 2.0% and 15.6% of deaths among adults aged 15–49 years are due to HIV [5, 6]. By the end of 2019, under the MSPP’s national policy of universal HIV treatment, more than 108,000 patients were active on HIV antiretroviral treatment (ART), representing 86% of people living with HIV (PLHIV) aware of their status [7].
In early March 2020, the MSPP published its COVID-19 prevention and control plan, promoting reduced use of health facilities for non-essential services, particularly for vulnerable groups, including PLHIV [8]. In parallel, the United States President’s Emergency Plan for AIDS Relief (PEPFAR), responsible for approximately 75% of funding for Haiti’s ART program [7], disseminated guidance on mitigating the impact of COVID-19 on the continuum of HIV care via several strategies, including: (1) use of telephone and short message service (SMS) to proactively communicate with HIV patients about COVID-19 risk and prevention; (2) promoting multi-month dispensing (MMD) for six or more months, reducing the need for frequent visits to health facilities for ART refills; and (3) promoting community-based ART distribution, through community health agents [9]. With the arrival of COVID-19 in Haiti, non-governmental partner organizations also rapidly mobilized to support COVID-19 prevention, testing, and case management, as well as continuity of HIV services [10].
Our observational study sought to describe changes in HIV service utilization, delivery, and continuity in Haiti during COVID-19, using retrospective data from a national electronic medical record (EMR) system.
Methods
We compared indicators of interest from January 24, 2020 to May 14, 2020, representing the eight weeks before and after the first two cases of COVID-19 were diagnosed in Haiti on March 19, 2020. Our study included data from 96 out of 134 facilities using the iSanté electronic medical record (EMR) data system and 167 facilities offering ART services. The project was approved by the University of Washington’s Human Subjects Division and the Haiti National Bioethics Committee. The project was reviewed in accordance with CDC human research protection procedures and was determined to be research. However, the study used only aggregated, de-identified data, and no investigators interacted with human subjects or had access to identifiable data or specimens for research purposes, so a consent waiver was obtained for the study.
Data Source
The iSanté EMR system is operated by MSPP and is the largest of Haiti’s three main EMR systems [11–13]. The iSanté central data repository, located in Port-au-Prince, contains data from 134 health facilities which routinely use the EMR for HIV clinical management. Data were extracted from the central repository in June 2020. Health facilities were excluded if they failed to replicate their data to the central repository following the study close date of May 14, 2020; this ensured that the central data mirrored the data available at the sites through the full study period.
Outcomes of Interest
The study included patient data aggregated in weekly values at the health facility level. Our study sought to assess time trends before and after the confirmation of the first cases of COVID-19 in Haiti on March 19, 2020 (referred to as “COVID-19 arrival”), using four indicators:
Count of unique visits to the health facility for HIV care (referred to as “HIV visits”);
Proportion of ART dispenses occurring in community-based settings (referred to by its French acronym, as “DAC”);
Proportion of ART dispenses with six or more months of medication dispensed (referred to as “ > 6 m MMD”);
Proportion of patients with timely ART refills in either the clinic or community, as indicated by receiving medication within seven days of the expected refill date.
Data Analysis
In descriptive analyses, we estimated the mean weekly value of each indicator along with the 95% confidence interval (CI) across the 96 health facilities over the 16 weeks of the study. We used uncontrolled interrupted time series (ITS) models to estimate slope and level changes in each indicator following the arrival of COVID-19 in Haiti. ITS is a useful quasi-experimental method for leveraging routine data sources to estimate the effects of sudden events or policy changes, in the context of observational data [14]. Our ITS models used the form:
The models included estimated baseline levels (, rates of change (slopes) for the period before ( and after ( March 19th, and a parameter for number of days health facilities were closured each week due to public holidays (. The models allowed for an immediate discontinuous level effect (, to detect sudden changes as of March 19th. The ITS models used mixed effects negative binomial regression models, which assumed a Poisson-like count process, suitable for overdispersed count data, as was the case in these data. The models for the three indicators expressed as proportions also included an exposure or offset parameter reflecting the value of the denominator, constraining estimated outcome values to 1.0. The ITS models allowed for random intercepts by health facility and used a first-order auto-regressive model to account for autocorrelation. To assess the robustness of the ITS model, we conducted a date falsification test for an unknown break point, and used a Bonferroni-like correction to address multiple testing [15]. To address concerns about data quality, we carried out sensitivity analyses which included only health facilities with data available during all 16 weeks of interest (n = 75). We used R (https://www.r-project.org/) and Stata 15.1 (StataCorp, College Station, TX) for all analyses.
Results
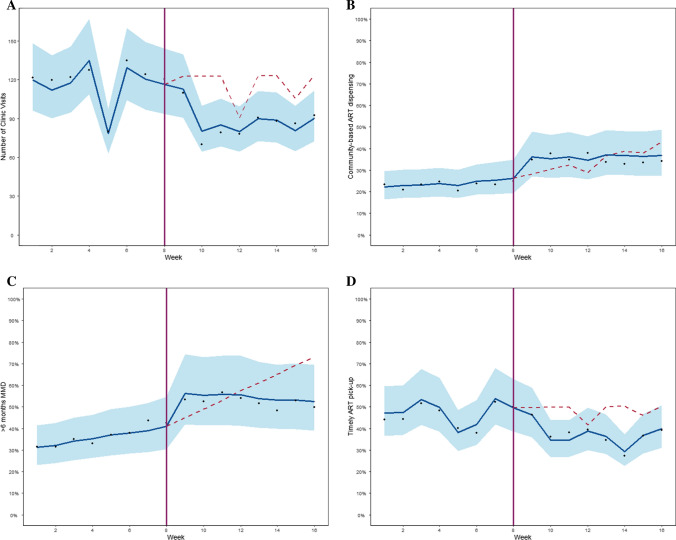
The 96 health facilities included in the study contributed 6‒16 weeks of data each. There were 152,766 HIV consultations, 89,265 (58.4%) before and 63,503 (41.6%) after arrival of COVID-19. The mean number of HIV visits per week per facility fell from 121.5 visits during week 1 to 92.5 during week 16 (Fig. 1 Panel A). The ITS model estimated a marginally-significant abrupt decline of 18% in the number of HIV visits with the arrival of COVID-19 in Haiti, as estimated by the discontinuous level parameter in the ITS model (incidence rate ratio [IRR] = 0.82; 95% CI: 0.66–1.00, p = 0.05), and no change in slope before or after arrival of COVID-19. Each public holiday resulted in a decline of 14% in the estimated number of clinical visits (IRR = 0.86, 95% CI: 0.79–0.93, p < 0.001).
Fig. 1.
*Mean values by week shown with scatter points; blue trend line shows the ITS model-predicted trend with 95% confidence interval; vertical line shows the date of arrival of COVID-19 in Haiti (March 19 2020); dashed line show the counterfactual scenario of continuation of the before COVID-19 trend (with autoregression and adjustment for public holidays as a time-varying factor)
The use of both > 6 m MMD and DAC increased. Among 59,591 ART dispenses, 28,437 (47.7%) occurred before and 31,354 (52.3%) occurred after COVID-19 arrival. From week 1 to week 16, the mean proportion of > 6 m MMD dispenses climbed from 29.4% to 48.4% (Fig. 1 Panel B) and the mean proportion of DAC climbed from 22.7% to 36.7% (Fig. 1 Panel C). Before COVID-19 arrival, > 6 m MMD increased by 4% per week (p < 0.001) and DAC increased by 2% per week (p = 0.05) (Table 1). Both indicators made an abrupt jump in level with the arrival of COVID-19 (IRR = 1.36; 95% CI: 1.21–1.53 for > 6 m MMD and IRR = 1.37; 95% CI: 1.22–1.53 for DAC; both p < 0.001) (Table 1). After the arrival of COVID-19, DAC exhibited no slope change, and < 6 m MMD declined by 4% per week (p < 0.01). The proportion of timely ART refills declined from 51.9% during week 1 to 43.8% during week 16 (Fig. 1 Panel D). The ITS model estimated an immediate drop of 18% (IRR: 0.82; 95% CI: 0.61–1.10, p = 0.20), but no change in slope before or after the arrival of COVID-19 (Table 1). A sensitivity analysis of only sites reporting data for all 16 weeks of the study (n = 75) produced consistent results (Table 2).
Table 1.
Time trends in key HIV care indicators before (January 24‒March 18, 2020) and after (March 19‒May 14, 2020) COVID-19 arrival in Haiti (n = 1,483 site weeks)
| Incidence Rate Ratio (95% Confidence Interval)Ϯ | ||||
|---|---|---|---|---|
| HIV visits (count) | > 6 months MMD | Community based ART (DAC) | Timely ART pick-up | |
| Baseline incidence | 51.06 (37.68, 69.06) | 0.26 (0.22, 0.30) | 0.18 (0.16, 0.22) | 0.43 (0.37, 0.57) |
| Before period slope | 1.00 (0.97, 1.03) | 1.04 (1.02, 1.06)** | 1.02 (1.00, 1.04)* | 1.00 (0.95, 1.05) |
| Level change | 0.82 (0.66, 1.00) | 1.36 (1.21, 1.53)*** | 1.37 (1.22, 1.53)*** | 0.82 (0.61, 1.10) |
| After period slope | 0.98 (0.94, .1.03) | 0.96 (0.93, 0.98)** | 0.98 (0.96, 1.01) | 0.99 (0.93, 1.06) |
| Public holiday (per day) | 0.86 (0.79, 0.93)*** | 1.00 (0.96, 1.04) | 0.97 (0.93, 1.02) | 0.96 (0.86, 1.07) |
***p < 0.001; **p < 0.01; *p < 0.05
ϮIndicator for HIV visits included 96 sites, while indicators for DAC, > 6 months MMD and timely ART pickup included 95 health facilities
Table 2.
Sensitivity Analysis: Time trends in key HIV care indicators before (January 24‒March 18, 2020) and after (March 19‒May 14, 2020) COVID-19 arrival in Haiti (n = 1,232 site weeks)
| HIV visits (count) | > 6 months MMD | Community based ART (DAC) | Timely ART pick-up | |
|---|---|---|---|---|
| Baseline incidence | 77.64 (58.50, 103.03) | 0.26 (0.22, 0.31) | 0.19 (0.16, 0.23) | 0.45 (0.35, 0.60) |
| Before period slope | 1.00 (0.97, 1.03) | 1.04 (1.01, 1.05)** | 1.02 (1.01, 1.04)* | 1.00 (0.95, 1.05) |
| Level change | 0.83 (0.68, .1.00) | 1.40 (1.23, 1.58)*** | 1.33 (1.18, 1.50)*** | 0.80 (0.60, 1.08) |
| After period slope | 0.99 (0.95, .1.03) | 0.96 (0.94, 0.99)** | 0.98 (0.96, 1.01) | 0.99 (0.93, 1.06) |
| Public Holiday (days) | 0.85 (0.79, 0.92)*** | 1.00 (0.96, 1.05) | 0.97 (0.93, 1.02) | 0.96 (0.86, 1.07) |
***p < 0.001; **p < 0.01; *p < 0.05
Discussion
Keeping PLHIV out of clinics was an important COVID-19 mitigation strategy and it is likely that anticipation of the arrival of the pandemic in Haiti accelerated pre-existing programmatic shifts towards ART delivery models involving MMD and DAC. Despite the increases in these strategies to reduce barriers to ART retention, we found some evidence of an abrupt decline in continuity of care for ART patients in Haiti with the arrival of COVID-19, as indicated by the trend in timely ART refills across clinic and community settings. While not statistically significant, the decline from what was already a sub-optimal level is highly concerning, and gives credence to WHO’s projections of devastating secondary health impacts of COVID-19 in terms of disruption to HIV treatment programs [16].
In recent years, Haiti has experienced novel outbreaks of cholera (2010) [17, 18], chikungunya (2013), and Zika (2015) [19], as well as disruption to healthcare delivery due to the earthquake of 2010 [20], hurricanes, health worker strikes, and political unrest. The resiliency of ART patients and providers has been evident in the face of such challenges. For example, within five months of the 2010 earthquake that killed over 200,000 people, HIV testing, prevention, and treatment services had largely rebounded following focal investment in rebuilding [20–22]. In contrast, the timeframe for COVID-19 disruption is more uncertain, and global economic hardship could make it very difficult to mobilize investment to support the MSPP-led COVID-19 response, as Haiti has seen with past health crises.
There were several limitations to our study. The number of time points before and after March 19th (8 each) is less than is recommended for ITS analyses, leading to low power to detect differences in time trends [23]. We were not able to separately estimate timely ART refills in clinic vs. community settings, and we did not assess whether this outcome translated into enduring attrition from the ART program. We could not determine whether the decrease in HIV visits was appropriate, or whether HIV patients may have missed necessary care. It is possible that data entry was disrupted, leading to measurement error in the indicators we studied; however, our sensitivity analysis, a proxy for data completeness, produced consistent results. There may have been different phases during the period after arrival of COVID-19, with additional break points, which we did not model. Indeed, the date falsification tests revealed significant break points in both week 8 (the break point in our primary model) and week 9. Further research on the effects of COVID-19 on HIV care delivery could explore evidence for distinct phases.
Further research on COVID-19 related disruptions in HIV testing, linkage to care, ART initiation, or in the ART drug supply chain in low and middle-income countries is warranted. While the sharp increase in > 6 m MMD in our study suggested no drug supply interruptions, it is unclear if a stable drug supply will persist [16]. In addition, we studied only a short period after the arrival of COVID-19 in Haiti. On May 14, 2020, the closing date of our study, there were 18 observed deaths from COVID-19 and fewer than 150 observed cases in Haiti [4]. Given the growth in the number of COVID-19 cases in the ensuing weeks, it will be important to monitor long-term effects of the COVID-19 pandemic on continuity of HIV services.
Conclusions
Overall, this study showed a concerning signal of short-term disruption to HIV services in Haiti with the arrival of COVID-19. The decline in HIV visits at health facilities and the shift toward DAC and > 6 m MMD reflected the adaptability of the health system, and represented a desirable opportunity to mitigate COVID-19 risk while preserving ART continuity; however, it is discouraging that timely ART refills across clinic and community settings worsened after the arrival of COVID-19. The COVID-19 pandemic’s direct and secondary effects on population health are considerable. Our study from Haiti brings concrete, specific evidence that underscores the urgency of optimizing DAC and MMD and identifying additional strategies to support continuity of HIV care in Haiti and beyond.
Acknowledgements
The authors would like to acknowledge the Haiti Ministry of Health and Population for its leadership of the iSanté data system and for its support of this analysis. The iSanté data system depends upon the dedicated efforts of the many individuals who care for patients, enter data, and work to assure data quality within iSanté, including health care workers, disease reporting officers, regional strategic information officers, and PEPFAR implementing partners.
Authors' Contributions
KC, MV, JGH, CW, JSV, KG, NK, JF, JBTK, GP, and NP contributed to the concept for the presented work. KC and KF contributed to the acquisition of the data. NP and AA proposed the methodology and conducted the analysis. All authors contributed to the interpretation of the results. NP, MV, KC drafted the manuscript. AA, SB, NK, JBTK and JF revised critically for important intellectual content. All authors have read and approved the final version of the manuscript.
Funding
This research has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the US Centers for Disease Control and Prevention (https://www.cdc.gov/), under award number NU2GGH002226-02, made to the Centre Haïtien de Renforcement du Système Sanitaire (CHARESS). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
Data Availability
Data may be obtained from the study authors, with written permission from the Haiti Ministry of Health National AIDS Control Program.
Code Availability
Code may be obtained from the study authors.
Declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical Approval
The project was approved by the University of Washington’s Human Subjects Division and the Haiti National Bioethics Committee. The project was reviewed in accordance with CDC human research protection procedures and was determined to be research. However, he study used only aggregated, de-identified data, and no investigators interacted with human subjects or had access to identifiable data or specimens for research purposes, so a consent waiver was obtained for the study.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kemar Celestin, Email: kemarcelestin@charess.org.
Adrien Allorant, Email: allorant@uw.edu.
Michelle Virgin, Email: mrv@uw.edu.
Elisma Marinho, Email: marinhoelisma@charess.org.
Kesner Francois, Email: kesnerf@yahoo.fr.
Jean Guy Honoré, Email: jeanguyhonore@charess.org.
Christina White, Email: nodinx23@uw.edu.
Jean Solon Valles, Email: hnn4@cdc.gov.
Georges Perrin, Email: ydr1@cdc.gov.
Nicolas De Kerorguen, Email: fju9@cdc.gov.
Jan Flowers, Email: jflow2@uw.edu.
Jean Gabriel Balan, Email: jeangabrielbalan@charess.org.
Jean Baptiste T. Koama, Email: hqt2@cdc.gov
Scott Barnhart, Email: sbht@uw.edu.
Nancy Puttkammer, Email: nputt@uw.edu.
References
- 1.JHU. COVID-19 Dashboard Baltimore, MD USA: Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU); 2020 [cited 2020 October 30]. Available from: https://coronavirus.jhu.edu/map.html.
- 2.Jewell BL, Mudimu E, Stover J, et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. The Lancet HIV. 2020;7(9):e629–e640. doi: 10.1016/S2352-3018(20)30211-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. The cost of inaction: COVID-19-related service disruptions could cause hundreds of thousands of extra deaths from HIV Geneva: World Health Organization; [cited 2020 Aug 5]. Available from: https://www.who.int/news-room/detail/11-05-2020-the-cost-of-inaction-covid-19-related-service-disruptions-could-cause-hundreds-of-thousands-of-extra-deaths-from-hiv
- 4.MSPP. COVID-19: Sitaution of Pandemic in Haiti Port-au-Prince, Haiti: Republique d'Haiti, Ministère de la Santé Publique et de la Population; 2020 [cited 2020 Aug 5]. Available from: https://www.mspp.gouv.ht/.
- 5.UNAIDS. Country Profile Overview Geneva2020 [cited 2020 Jul 8]. Available from: https://www.unaids.org/en/regionscountries/countries/haiti.
- 6.IHME. GBD Compare Viz Hub (Global Burden of Disease) Seattle, WA: Institute for Health Metrics and Evaluation (IHME); 2020 [cited 2020 Jul 8]. Available from: https://vizhub.healthdata.org/gbd-compare/.
- 7.PEPFAR. Haiti Country Operational Plan (COP/ROP) 2020 Strategic Direction Summary. US Presidents Emergency Plan for AIDS Relief (PEPFAR); 2020 April 1, 2020.
- 8.MSPP. Plan de Préparation et de réponse du MSPP au Coronavirus Port-au-Prince, Haiti2020 [updated Mar 10, 2020; cited 2021 February 9]. Available from: https://mspp.gouv.ht/site/downloads/Plan%20de%20Pr%C3%A9paration%20et%20de%20R%C3%A9ponse%20du%20MSPP%20au%20CoronaVirus.pdf.
- 9.PEPFAR. PEPFAR Technical Guidance in Context of COVID-19 Pandemic. 20 Mar, 2020.
- 10.Rouzier V, Liautaud B, Deschamps MM. Facing the Monster in Haiti. N Engl J Med. 2020;383(1):e4. doi: 10.1056/NEJMc2021362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.deRiel E, Puttkammer N, Hyppolite N, et al. Success factors for implementing and sustaining a mature electronic medical record in a low-resource setting: a case study of iSanté in Haiti. Health Policy Plan. 2017 doi: 10.1093/heapol/czx171. [DOI] [PubMed] [Google Scholar]
- 12.Matheson AI, Baseman JG, Wagner SH, et al. Implementation and expansion of an electronic medical record for HIV care and treatment in Haiti: an assessment of system use and the impact of large-scale disruptions. Int J Med Informatics. 2012;81(4):244–256. doi: 10.1016/j.ijmedinf.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Domercant J, Puttkammer N, Young P, et al. Attrition from antiretroviral treatment services among pregnant and non-pregnant patients following adoption of Option B+ in Haiti. Glob Health Action. 2017;10(1):1330915. doi: 10.1080/16549716.2017.1330915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Svoronos T. Evaluating Health Interventions Over Time: Empirical Tests of the Validity of the Single Interrupted Time Series Design. Cambridge, MA: Harvard University; 2016. [Google Scholar]
- 16.WHO. Access to HIV medicines severely impacted by COVID-19 as AIDS response stalls 2020 [cited 2020 Aug 5 ]. Available from: https://www.who.int/news-room/detail/06-07-2020-who-access-to-hiv-medicines-severely-impacted-by-covid-19-as-aids-response-stalls.
- 17.Tappero JW, Tauxe RV. Lessons learned during public health response to cholera epidemic in Haiti and the Dominican Republic. Emerg Infect Dis. 2011;17(11):2087–2093. doi: 10.3201/eid1711.110827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barzilay EJ, Schaad N, Magloire R, et al. Cholera Surveillance during the Haiti Epidemic — The First 2 Years. N Engl J Med. 2013;368(7):599–609. doi: 10.1056/NEJMoa1204927. [DOI] [PubMed] [Google Scholar]
- 19.Journel I, Andrécy LL, Metellus D, et al. Transmission of Zika Virus — Haiti, October 12, 2015–September 10, 2016. MMWR. 2017 doi: 10.15585/mmwr.mm6606a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walldorf JA, Joseph P, Valles JS, et al. Recovery of HIV service provision post-earthquake. AIDS. 2012;26(11):1431–1436. doi: 10.1097/QAD.0b013e328352d032. [DOI] [PubMed] [Google Scholar]
- 21.Delcher C, Bae J, Rich SN, Klann EM, Puttkammer N, Joseph N. Impact of the 12 January 2010 earthquake on HIV case reporting in Haiti. AIDS. 2020;34(5):777–782. doi: 10.1097/QAD.0000000000002466. [DOI] [PubMed] [Google Scholar]
- 22.Puttkammer NH, Zeliadt SB, Balan JG, et al. Before and after the earthquake: a case study of attrition from the HIV antiretroviral therapy program in Haiti. Global Health Action. 2014 doi: 10.3402/gha.v7.24572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang F, Wagner AK, Ross-Degnan D. Simulation-based power calculation for designing interrupted time series analyses of health policy interventions. J Clin Epidemiol. 2011;64(11):1252–1261. doi: 10.1016/j.jclinepi.2011.02.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data may be obtained from the study authors, with written permission from the Haiti Ministry of Health National AIDS Control Program.
Code may be obtained from the study authors.