Pneumothorax (PNX) and pneumomediastinum (PMD) have been frequently observed in mechanically ventilated patients with coronavirus disease 2019 (COVID-19)-related acute respiratory distress syndrome (ARDS), with a reported rate up to 24% [1]. No study has evaluated so far the exact rate of these events in non-intubated COVID-19 patients. We therefore decided to perform an observational study to investigate the rate of PNX/PMD in non-intubated COVID-19 patients and to compare the rate of PNX/PMN between patients admitted during the first and second Italian pandemic wave.
Under our Institutional Review Board-approved protocol (protocol number 34/int/2020; ClinicalTrials.gov no. NCT04318366), we identified all patients with pneumothorax and/or pneumomediastinum documented at chest X-ray or computed tomography (CT) between March 1st, 2020 and June 1st, 2020 (first Italian wave) and between October 1st, 2020 and January 1st, 2021 (second Italian wave) (Fig. 1 ). Patients were included in the analysis if not invasively ventilated before PNX/PMD diagnosis. Details on hospital organization and clinical management have been previously published [2], [3], [4], [5]. The main change in patients’ management between first and second pandemic wave was the administration of dexamethasone to all patients requiring oxygen supplementation during the second wave and the avoidance of hydroxychloroquine [6]. We collected data as per Table 1 . Categorical variables are expressed as numbers and percentages; continuous variables are presented as median and interquartile range. Continuous measures were compared using Wilcoxon matched pairs signed rank test, while dichotomous data were compared using χ2 or Fisher's exact. Two-sided p-value < 0.05 defined statistical significance.
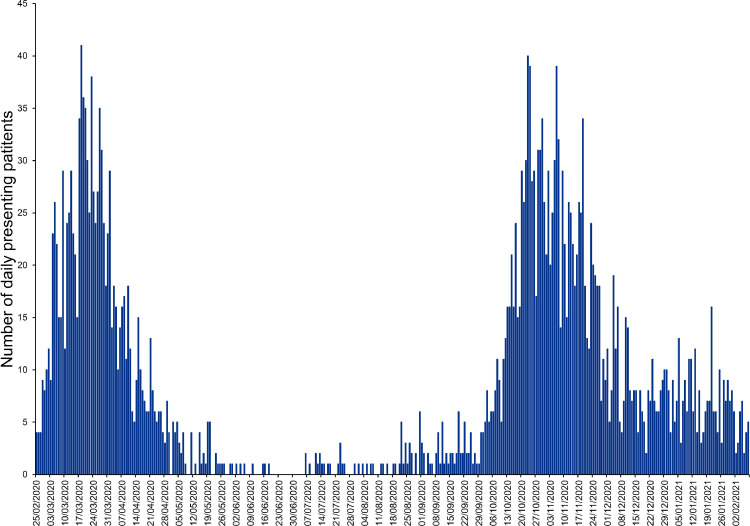
Fig. 1.
Number of Coronavirus Disease 2019 patients presenting to San Raffaele Scientific Institute per day, from February 25th, 2020 to February 9th, 2021.
Table 1.
Patients’ characteristics and treatment details. .
| Variable | First wave(N = 1) | Second wave(N = 13) |
|---|---|---|
| Age, years | 75 | 72 (65 – 76) |
| Male sex | Male | 12 (92.3) |
| CPAP | Yes | 7 (53.8) |
Steroid therapy
|
No | 13 (100)
|
| LMWH (4000 IU enoxaparin) | Yes | 13 (100) |
| Antibiotic therapy | Yes | 9 (69.2) |
| HCQ (400 mg daily) | Yes | 0 (0.0) |
Biologics
|
No | 5 (38.5)
|
Comorbidities
|
Yes:
|
3 (23.1)
|
Continuous variables are presented as median and interquartile range, while categorical variables are presented as number and percentages.
CPAP: continuous positive airway pressure; COPD: chronic obstructive pulmonary disease; DM: type-2 diabetes mellitus; HCQ: hydroxychloroquine; ILD: interstitial lung disease; IU: international units; LMWH: low molecular weight heparin.
All the 1151 patients of the first wave and 1484 patients of the second wave did multiple chest X-ray examinations and 813 non-intubated COVID-19 patients underwent at least one CT scan (418, first pandemic wave; 395, second pandemic wave). Fourteen non-intubated patients with radiologically proven PNX/PMD were identified: one patient during the first wave and 13 during the second wave (p = 0.005 when using all patients at denominator and p<0.001 when using only patients who underwent CT scan at denominator). Specifically, eight patients had PMD, two PNX, whereas the remaining three had both. Patients’ characteristics are summarized in Table 1. At the time of PNX/PMD development, eight patients were on CPAP, whereas six patients were on supplemental oxygen therapy only. All but the patient of the first wave were on steroid therapy (dexamethasone 6 mg daily in 12 cases and prednisone 60 mg daily in one case, p = 0.071). Median time from symptoms onset to PNX/PMD was 18 (17–24.5) days; median time form corticosteroid start to PNX/PMD was 15 (13–17) days. After PNX/PMD onset, four (29%) patients were admitted to ICU and seven (50%) patients died.
The rate of PNX/PMD in non-intubated COVID-19 was significantly higher in the second pandemic wave as compared with the first pandemic wave. To the best of our knowledge, this is the first report comparing incidence of PNX/PMD in non-intubated COVID-19 ARDS patients in the first and second pandemic wave.
As the only difference in treatment between the two waves was dexamethasone administration and hydroxychloroquine avoidance, it could be hypothesized that dexamethasone might have induced lung frailty and increased the risk of PNX/PMD, as already suggested in patients with interstitial inflammatory lung diseases [7]. Future studies are needed to confirm a different rate of PNX/PMD when using or not corticosteroids in COVID-19 patients.
Funding
None
Declaration of Competing Interests
None
Acknowledgements
We thank all the personnel of San Raffaele Scientific Institute for the dedication to these patients and for the support in data collection
References
- 1.Belletti A., Palumbo D., Zangrillo A. Predictors of pneumothorax/pneumomediastinum in mechanically ventilated COVID-19 patients. J Cardiothorac Vasc Anesth. 2021 doi: 10.1053/j.jvca.2021.02.008. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zangrillo A., Beretta L., Scandroglio A.M. Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy. Crit Care Resusc. 2020;22(3):200–211. doi: 10.1016/S1441-2772(23)00387-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramirez G.A., Bozzolo E.P., Castelli E. Continuous positive airway pressure and pronation outside the intensive care unit in COVID 19 ARDS. Minerva Med. 2020 doi: 10.23736/S0026-4806.20.06952-9. In press. [DOI] [PubMed] [Google Scholar]
- 4.Zangrillo A., Beretta L., Silvani P. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: facing the COVID-19 pandemic emergency. Crit Care Resusc. 2020;22(2):91–94. doi: 10.51893/2020.2.pov1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sartini C., Tresoldi M., Scarpellini P. Respiratory Parameters in Patients with COVID-19 after Using Noninvasive Ventilation in the Prone Position Outside the Intensive Care Unit. JAMA. 2020;323(22):2338–2340. doi: 10.1001/jama.2020.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dexamethasone in Hospitalized Patients with Covid-19 — Preliminary Report. N Engl J Med. 2021;384(8):693–704. doi: 10.1056/nejmoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nishimoto K., Fujisawa T., Yoshimura K. Pneumothorax in connective tissue disease-associated interstitial lung disease. PLoS ONE. 2020;15(7) doi: 10.1371/journal.pone.0235624. [DOI] [PMC free article] [PubMed] [Google Scholar]