Abstract
Cardiac arrhythmias are important causes of death among populations and are always responsible for a high percentage of mortality in hospitalized patients. The aim of this descriptive analytical study was to evaluate the frequency of arrhythmias in patients with coronavirus disease 2019 (COVID-19) in the Shahid Mostafa Khomeini Hospital of Ilam from March to August 2020. All the COVID-19 patients with a cardiac condition admitted to the intensive care unit were enrolled in the study by census. Electrocardiography (ECG) and Holter monitoring were used to diagnose arrhythmias. Data analysis was performed in Microsoft Excel using descriptive statistics (frequency and percentage). The total number of eligible patients was 45, of whom 26 (57.8%) were men and 19 (42.2%) were women. The mortality rate of arrhythmias among COVID-19 patients was 17.77% (8 out of 45 patients), and the recovery rate was 82.13% (37 out of 45 patients). Tachycardia and a lack of response to heart-rate-reducing drugs were observed in patients with COVID-19. Owing to an overlap between these symptoms and those of heart diseases, there is a need to further evaluate patients with arrhythmias. Although arrhythmias are not common in COVID-19 patients, they can be fatal and have a high mortality rate, which can be prevented by early detection.
Keywords: Arrhythmia, atrial fibrillation, coronavirus disease 2019, electrocardiography, Holter monitor
Introduction
Coronavirus disease 2019 (COVID-19) has become a global problem in recent months, spreading to more than 150 countries in a globe pandemic [1]. In a study by Ruan et al., the mortality rate of individuals with COVID-19 significantly increased in the presence of cardiovascular abnormalities [2]. Another study noted that underlying diseases such as hypertension can increase the mortality rate up to 2.5 times [3]. Although the clinical manifestations of COVID-19 in patients with cardiac failure are unknown, the clinical features of patients with end-stage heart disease indicate cardiac injury by the virus [[4], [5], [6]].
Manifestations of COVID-19 are also linked to demographic parameters. The highest mortality is found in older men with a mean age of 75 years, who also present with histories of underlying conditions such as diabetes, hypertension, heart problems, chronic respiratory disease, cancer and previous surgery. COVID-19 exaggerates cardiovascular complications by promoting arterial and venous thrombosis through inducing inflammation, activating platelets and causing vascular dysfunction and blockade. Because of this, antithrombotic drugs are recommended to be prescribed in these patients [7].
In addition to promoting inflammatory responses and myocardial injury, COVID-19 also augments the risk of acute coronary artery syndrome, heart failure and arrhythmias [8]. Cardiac arrhythmias are the most threatening complications of heart diseases and cause the deaths of a large number of patients. The aim of this study was to investigate the frequency of arrhythmias in patients with COVID-19 in the Shahid Mostafa Khomeini Hospital of Ilam from March to August 2020.
Materials and methods
In this descriptive analytical study, all patients with COVID-19 and a cardiac condition admitted to the intensive care unit during March to August 2020 were enrolled by census. A definite diagnosis of COVID-19 by PCR was applied as an inclusion criterion. Electrocardiography (ECG) and Holter monitoring were used to diagnose cardiac status. Data analysis was performed in Microsoft Excel applying descriptive statistics (frequency and percentage).
Results
In total, 45 eligible patients were enrolled, of whom 26 (57.8%) were men, and 19 (42.2%)were women. Twelve people (26.7%) were <60 years old, 23 (51.1%) were between 60 and 70 years old, and 10 (22.3%) were >70 years old. Of these patients, 40 (88.9%) had a history of hospitalization before admission. The criterion for being hospitalized was a positive PCR test.
After the diagnosis of COVID-19 based on clinical symptoms, treatment and supportive care were started, and after confirmation by PCR (which generally takes around 48–72 hours), the patient was subjected to major therapeutic measures. The medications used for these patients included ciprofloxacin, vancomycin, ceftriaxone, dexamethasone, recigen and remdesivir, according to clinical signs and symptoms. The genotype of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) during this period was D614G.
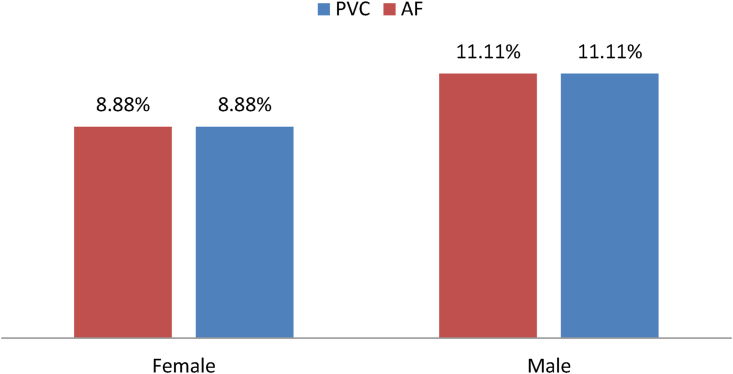
Table 1 demonstrates the frequencies of different types of arrhythmias and non-arrhythmias observed in ECG. Fig. 1 shows the frequencies of atrial fibrillation (AF) and premature ventricular contraction (PVC) arrhythmias in each gender. The fatality rate of arrhythmias among COVID-19 patients was 17.77% (8 out of 45 patients), of whom 6 (13.33%) were men and 2 (4.44%) were women. The recovery rate was 82.13% (37 out of 45), of whom 20 (46.44%) were men and 17 (37.77%) were women. Among deceased patients, each of AF, ventricular tachycardia (VT), and ventricular fibrillation (VF) was detected in two patients.
Table 1.
The frequency of arrhythmias in patients with coronavirus disease 2019
| ECG findings | Type | n | % |
|---|---|---|---|
| Arrhythmia | PAC | 2 | 4.44 |
| PVC | 9 | 20 | |
| AF | 9 | 20 | |
| PSVT | 2 | 4.44 | |
| VT | 2 | 4.44 | |
| VF | 1 | 2.22 | |
| AV Block | 1 | 2.22 | |
| Non-arrhythmia | BBB | 10 | 22.22 |
| Bradycardia | 3 | 6.66 | |
| Tachycardia | 11 | 24.44 |
Abbreviations: AF, atrial fibrillation; BBB, bundle branch block; PAC, premature atrial contraction; PVC, premature ventricular contraction; PSVT, paroxysmal supraventricular tachycardia; VF, ventricular fibrillation; VT, ventricular tachycardia.
Fig. 1.
Atrial fibrillation (AF) and premature ventricular contraction (PVC) arrhythmias in men and women with coronavirus disease 2019. Out of nine patients with each of AF and PVC arrhythmias, five were male and four were female.
Holter monitoring was performed to verify arrhythmia in three patients, one of whom was diagnosed with VT, and the other two with sinus tachycardia. Table 2 shows the frequency of death in COVID-19 patients with arrhythmia and non-arrhythmia disorders. Fig. 1 shows the prevalence of AF and PVC arrhythmias in each gender.
Table 2.
Comparison of the rates of recovery and mortality between coronavirus disease 2019 patients with arrhythmia and non-arrhythmia problems
| COVID-19 patients with cardiac abnormality | Total |
Deceased |
Recovered |
|||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Arrhythmia | 45 | 1 | 8 | 7.62 | 37 | 1 |
| Non-arrhythmia | 4653 | 99 | 97 | 92.38 | 3963 | 99 |
| Total | 4698 | 100 | 105 | 100 | 4000 | 100 |
Discussion
The aim of this study was to investigate the frequency of ECG abnormalities (arrhythmias and non-arrhythmias) in COVID-19 patients admitted to the Shahid Mostafa Khomeini Hospital of Ilam between March and August 2020. This hospital is the only centre for referral of COVID-19 patients in Ilam province, which has a population of about 800 000 and is located in the west of Iran.
Our results showed that arrhythmias were identified in 45 COVID-19 patients diagnosed over a period of 3 months. This comprised about 1% of all patients diagnosed during this period. This observation was in line with the finding of Wang et al., who noted an association between the SARS-CoV-2 infection and inflammatory mediators that may play important roles in the path physiology of cardiac events and arrhythmias. In one study, the rate of heart damage was 1% in around 19% of the patients diagnosed with COVID-19, and this event was associated with a higher risk of in-hospital mortality [9].
The mortality rate of arrhythmias in COVID-19 patients was 17.77%, and the recovery rate was 82.13%. Although acute lung injury is a common problem in patients with COVID-19, which leads to significant morbidity and mortality, clinical and epidemiological evidence suggests that SARS-CoV-2 infection is also associated with myocardial damage and arrhythmias [2].
According to Mandeep et al., in a study of cardiovascular risk factors in patients with heart conditions, 30.5%, 26.3%, 14.3%, 16.8% and 5.5% of the patients reported hyperlipidaemia, hypertension, diabetes, a history of smoking and current smoking, respectively [10]. In the recent study, cardiovascular diseases included coronary artery disease (11.3%), congestive heart failure (2.1%) and cardiac arrhythmia (3.4%). The patients' average length of hospital stay was between 8 and 12 days, and the overall in-hospital mortality rates were 5.8% in total (515 out of 8910 patients) and 24.7% for the patients hospitalized in the intensive care unit [2].
The most common arrhythmias in the deceased patients were AF, VF and VT, respectively. This was in line with the study of Pietro et al., who asserted that the virus-induced aberrant function of the immune system increased the risk of arrhythmic events, including severe ventricular arrhythmias [11].
We noticed that the mortality rate was higher among men than women. Along with age and gender, many other complications and parameters have been associated with severity and mortality rate in COVID-19 and SARS. Nevertheless, age was comparable between men and women in our study. However, the disease was more severe in men than women. Despite a similar distribution in men and women, the number of men who died of COVID-19 was 2.4 times higher than the number of women. Regardless of age, men with SARS-CoV-2 infection are at a higher risk for severe consequences and death [12].
Novel clinical experiences
Tachycardia and failure to respond to heart-rate-reducing drugs may be features of COVID-19 patients. These can overlap with the symptoms of heart diseases, and therefore, there is a need for further investigation of a possible SARS-CoV-2 infection in patients with arrhythmic symptoms.
Limitations
The low power of the study was one of our limitations, which was due to the relatively small number of COVID-19 patients in the province.
Conclusion
Although arrhythmias are not common in COVID-19 patients, they have a high mortality rate, necessitating early diagnostic and therapeutic interventions.
Recommendations
It is recommended to screen for cardiac abnormalities in COVID-19 patients, which can affect their prognosis and survival by early diagnosis of arrhythmias.
Conflict of interest
The authors declare that they have no conflicts of interest.
Acknowledgements
This research was approved and supported by the Deputy of Research and Technology of Ilam University of Medical Sciences under the ethical code of IR.MEDILAM.REC.1399.125.
Contributor Information
H. Tavan, Email: hamedtavan@gmail.com.
S. Norozi, Email: cyrus_norozi@yahoo.com.
References
- 1.Arnold S.L.M., Buckner F. Hydroxychloroquine for treatment of SARS-CoV-2 infection? Improving our confidence in a model-based approach to dose selection. Clin Transl Sci. 2020;13:642–645. doi: 10.1111/cts.12797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruan Q., Yang K., Wang W., Jiang L., Song J. Correction to: clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:1294–1297. doi: 10.1007/s00134-020-06028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lippi G., Wong J., Henry B.M. Hypertension and its severity or mortality in Coronavirus Disease 2019 (COVID-19): a pooled analysis. Pol Arch Intern Med. 2020;130:304–309. doi: 10.20452/pamw.15272. [DOI] [PubMed] [Google Scholar]
- 4.Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Synd. 2020;14:247–250. doi: 10.1016/j.dsx.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dong N., Cai J., Zhou Y., Liu J., Li F. End-stage heart failure with COVID-19: strong evidence of myocardial injury by 2019-nCoV. JACC Heart Fail. 2020;8:515–517. doi: 10.1016/j.jchf.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hulot J.-S. COVID-19 in patients with cardiovasculardiseases. Arch Cardiovasc Dis. 2020;113:225–226. doi: 10.1016/j.acvd.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tam C.-C.F., Cheung K.-S., Lam S., Wong A., Yung A., Sze M. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ Cardiovas Qual Outcome. 2020 Apr;13(4) doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehra M.R., Desai S.S., Kuy S.R., Henry T.D., Patel A.N. Cardiovascular disease, drug therapy, and mortality in COVID-19. N Engl J Med. 2020;382 doi: 10.1056/NEJMoa2007621. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Pietro E.L., Mohamed B., Pier L.C. COVID-19, arrhythmic risk and inflammation. Circulation. 2020;142:7–9. doi: 10.1161/CIRCULATIONAHA.120.047293. [DOI] [PubMed] [Google Scholar]
- 12.Jin J.-M., Peng B., Wei H., Wu F., Liu X.-F., Han D.-M. Gender differences in patients with COVID-19: focus on severity and mortality. Front Publ Health. 2020;8:152. doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]