Abstract
Objective
The COVID-19 pandemic has dramatically changed health care, forcing providers to adopt and implement telehealth technology to provide continuous care for their patients. Amid this rapid transition from in-person to remote visits, differences in telehealth utilization have arisen among neurosurgical subspecialties. In this study, we analyze the impact of telehealth on neurosurgical healthcare delivery during the COVID-19 pandemic at our institution and highlight differences in telehealth utilization across different neurosurgical subspecialties.
Methods
To quantify differences in telehealth utilization, we analyzed all outpatient neurosurgery visits at a single academic institution. Internal surveys were administered to neurosurgeons and to patients to determine both physician and patient satisfaction with telehealth visits. Patient Likelihood-to-Recommend Press-Ganey scores were also evaluated.
Results
There was a decrease in outpatient visits during the COVID-19 pandemic in all neurosurgical subspecialties. Telehealth adoption was higher in spine, tumor, and interventional pain than in functional, peripheral nerve, or vascular neurosurgery. Neurosurgeons agreed that telehealth was an efficient (92%) and effective (85%) methodology; however, they noted it was more difficult to evaluate and bond with patients. The majority of patients were satisfied with their video visits and would recommend video visits over in-person visits.
Conclusions
During the COVID-19 pandemic, neurosurgical subspecialties varied in adoption of telehealth, which may be due to the specific nature of each subspecialty and their necessity to perform in-person evaluations. Telehealth visits will likely continue after the pandemic as they can improve clinical efficiency; overall, both patients and physicians are satisfied with health care delivery over video.
Key words: COVID-19 pandemic, Neurosurgery, Telehealth, Virtual medicine
Abbreviations and Acronyms: LTR, Likelihood-to-Recommend
Introduction
Telemedicine, or the remote diagnosis and treatment of patients by means of telecommunications technology, has been used in clinical practice for decades,1 with orthopedic surgeons reporting using traditional telephones to remotely examine patients in 1999.1 , 2 Although sometimes used interchangeably with telemedicine, telehealth is a broader term that describes the delivery of health care, health education, and health information services via remote technologies such as mobile health, video and audio technologies, and remote patient monitoring.1
The COVID-19 pandemic has led to rapid adoption and implementation of telehealth.3 At our institution, telehealth visits were implemented over 2 weeks in March 2020, a project that was initially intended to occur over several years. In this study, we present our experience with neurosurgery telehealth visits at a single academic institution before and during the COVID-19 pandemic. To the best of our knowledge, this is the first paper to assess telehealth utilization at different points during the pandemic and by different neurosurgical subspecialties, while also secondarily evaluating patient and physician satisfaction with telehealth visits during this time.
Methods
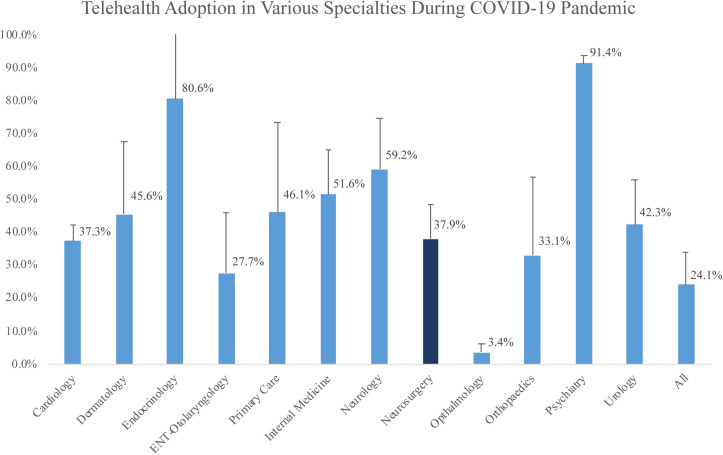
We retrospectively analyzed adoption of telehealth at our institution as a whole and in the following specialties during the COVID-19 pandemic (March 2020 to December 2020): cardiology, dermatology, endocrinology, ENT-otolaryngology, primary care, internal medicine, neurology, neurosurgery, ophthalmology, orthopaedics, psychiatry and urology (Figure 1 ).
Figure 1.
Percentage of monthly telehealth (phone and video) visits of various subspecialties during the COVID-19 pandemic.
Next, we retrospectively reviewed all neurosurgery visits performed from January 1, 2019, through November 2, 2020, at the outpatient clinic of a single academic institution. The following data were collected: date of clinic visit, type of visit (in-person, video, phone), and health care provider. Twenty-two neurosurgery providers were stratified by subspecialty: spine (n = 5), vascular (n = 2), functional (n = 2), trauma (n = 2), tumor (n = 6), and peripheral nerve (n = 1). Because interventional pain physicians (n = 4) also see patients in our neurosurgery clinic, we included them in our analysis.
Visit data were analyzed (n = 28,228 visits) in 4 time phases, as follows:
-
(1)
Phase 0 (Jan 1–Dec 20, 2019): control/baseline;
-
(2)
Phase 1 (Dec 30, 2019–Mar 9, 2020): beginning of COVID-19 outbreak;
-
(3)
Phase 2 (Mar 16–Apr 30, 2020): shelter-in-place guidelines, hospital suspension of elective surgery; and
-
(4)
Phase 3 (May 4-Nov 2, 2020): Resumption of hospital elective surgery, gradual easing of shelter-in-place.
To assess provider satisfaction with video visits, we performed an online 5-question survey of neurosurgery providers in October 2020 via Survey Monkey (n = 13, 59% response rate). At least 1 neurosurgeon from each subspecialty responded (spine [n = 4], vascular [n = 2], tumor [n = 4], trauma [n = 1], and pain [n = 2]), except for peripheral nerve and functional (Supplemental Figure 1).
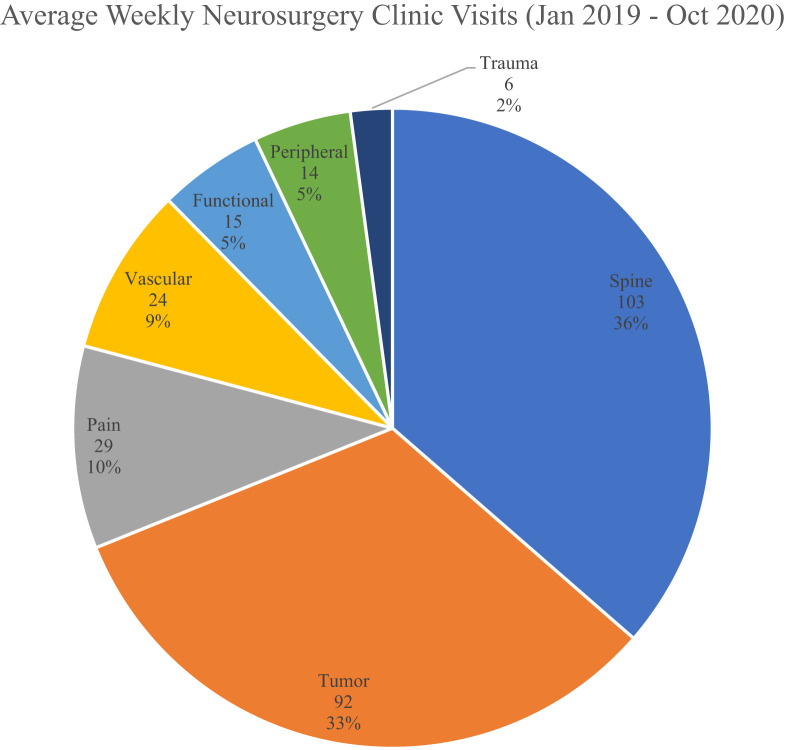
Supplemental Figure 1.
Weekly neurosurgery outpatient clinic visits by neurosurgical subspecialty, averaged January 2019 through November 2020.
To evaluate patient satisfaction with video visits, an institution-specific survey was performed over Stanford MyHealth, a digital tool for patients to securely access their health information and connect to their Stanford care team. Telehealth patient-satisfaction scores (n = 521 responses) from June 22, 2020, through November 2, 2020, were gathered. The following data were collected: rating of visit, likelihood of choosing a video visit over in-person visit, likelihood to recommend video visit (in general), and likelihood to recommend video visit with provider.
We also collected Press-Ganey Likelihood-to-Recommend (LTR) scores that were sent to patients via e-mail and mail for our spine (n = 5), tumor (n = 5), vascular (n = 2), functional (n = 2), trauma (n = 1), and peripheral nerve (n = 1) providers. Scores (n = 1917) were provided per month, and we estimated the phases as close to our four time phases.
Standard descriptive statistics, including means and standard deviations, were calculated (Microsoft Excel, Redmond, WA). Continuous variables were analyzed using Student's t test and categorical variables were analyzed using the χ2 test. Significance was set at α = 0.05.
Results
During the COVID-19 pandemic, our institution used phone or video for an average (±SD) 24.1% (±9.8%) of all patient visits. The neurosurgery department observed a higher adoption of telehealth visits, 37.9% (±10.7%) (Figure 1).
Over the study period, our neurosurgery outpatient clinic had a mean (±SD) of 284 ± 69 visits per week, of which 36% were spine, 33% tumor, 10% pain, 8% vascular, 5% functional, 5% peripheral nerve, and 2% trauma (Supplemental Figure 1).
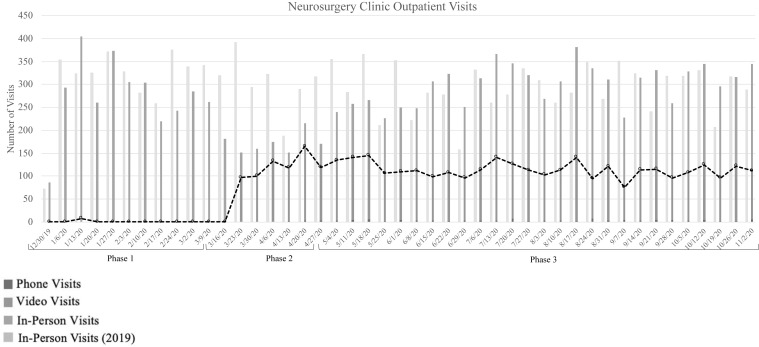
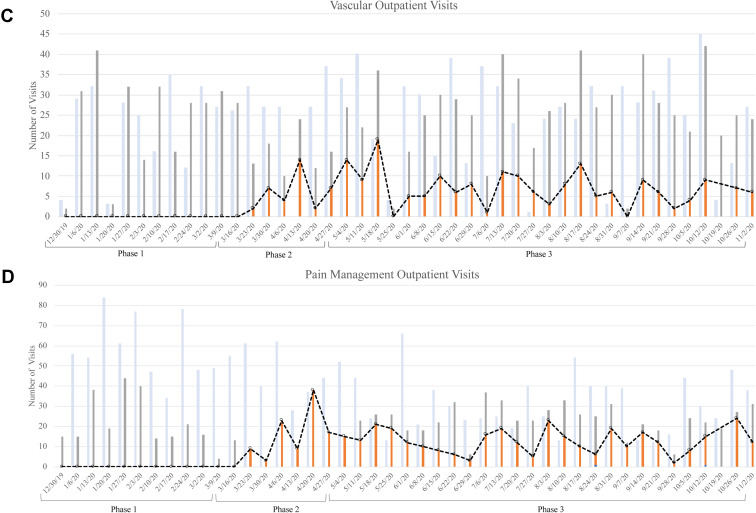
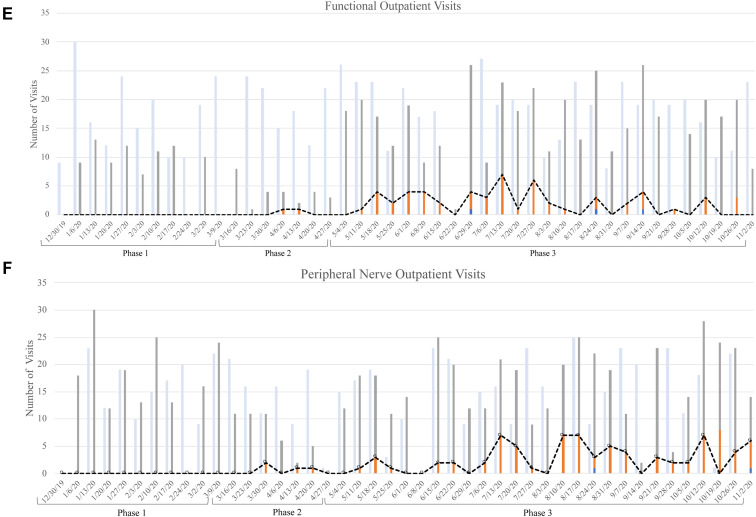
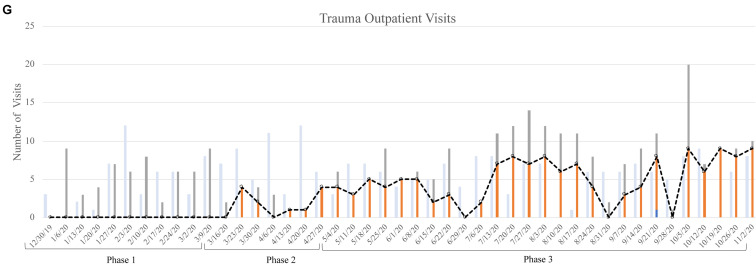
Between phase 0 (control/baseline, 2019) and phase 1 (Jan–March 9, 2020; beginning of COVID outbreak), mean weekly patient visits did not change significantly (294 ± 47 and 275 ± 51, respectively, P = 0.23). During phase 2 (Mar 16–Apr 30, 2020), which corresponded to our region's shelter-in-place, mean weekly neurosurgery clinic visits decreased significantly, from 294 ± 47 to 171 ± 20 (P < 0.05). All subspecialties, except for vascular neurosurgery, had a significant decrease in mean weekly visits from phase 0 to phase 2 (Table 1 ). During phase 3 (May 4–Nov 2, 2020), mean weekly visits (300 ± 31) returned to baseline and were not significantly different from our control phase 0 (P = 0.55; Table 1, Supplemental Figure 2).
Table 1.
Mean Number of Weekly Outpatient Clinic Visits in Each Subspecialty of Neurosurgery
| Subspecialty | Phase 0 12/31/2018–12/23/2019 |
Phase 1 12/30/2019–3/9/2020 |
Phase 2 3/16/2020–4/27/2020 |
Phase 3 5/4/2020–11/2/2020 |
P Value Phase 0 to Phase 1 | P-value Phase 0 to Phase 2 | P-value Phase 0 to Phase 3 | P-value Phase 2 to Phase 3 |
|---|---|---|---|---|---|---|---|---|
| Spine | 107 ± 33 | 108 ± 36 | 60 ± 8 | 105 ± 20 | 0.93 | P<0.05 | P = 0.77 | P<0.05 |
| Tumor | 89 ± 22 | 94 ± 29 | 65 ± 11 | 106 ± 17 | 0.52 | P<0.05 | P<0.05 | P<0.05 |
| Vascular | 25 ± 12 | 23 ± 13 | 17 ± 7 | 26 ± 10 | 0.62 | P = 0.09 | P = 0.71 | P<0.05 |
| Pain | 36 ± 20 | 22 ± 13 | 16 ± 12 | 23 ± 8 | <0.05 | P<0.05 | P<0.05 | P = 0.07 |
| Functional | 17 ± 7 | 8 ± 5 | 3 ± 2 | 16 ± 6 | <0.05 | P<0.05 | P = 0.53 | P<0.05 |
| Peripheral nerve | 14 ± 8 | 15 ± 9 | 7 ± 5 | 16 ± 7 | 0.71 | P<0.05 | P = 0.28 | P<0.05 |
| Trauma | 6 ± 3 | 5 ± 3 | 3 ± 1 | 8 ± 4 | 0.32 | P<0.05 | P<0.05 | P<0.05 |
| Total | 294 ± 47 | 275 ± 51 | 171 ± 20 | 300 ± 31 | 0.23 | P<0.05 | P = 0.55 | P<0.05 |
Supplemental Figure 2.
Number of outpatient neurosurgery visits in 2020 in comparison with 2019.
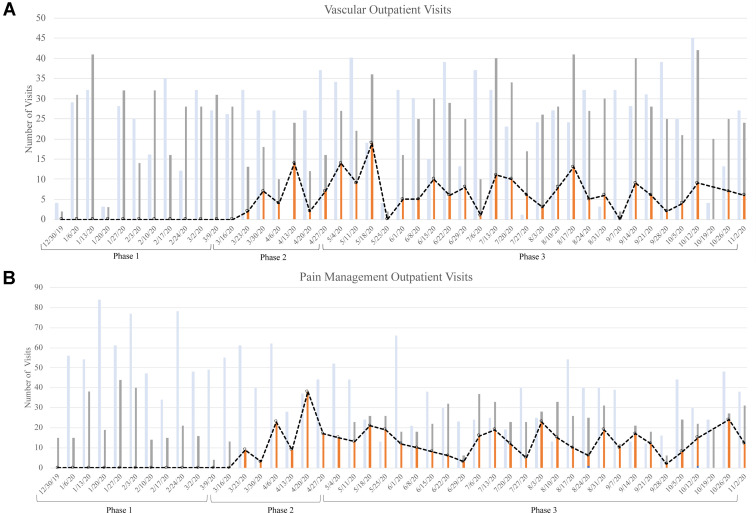
There were no telehealth visits in phase 0 and phase 1, as this technology had not yet been made available to our providers. After telehealth technology was implemented in the second week of March 2020, we saw a significant increase in video visit utilization in phase 2 to 60.3% (P < 0.05), with a decrease in video visit use to 37.4% in phase 3 (P < 0.05; Table 2 , Supplemental Figure 2). Overall, spine, tumor, pain, and trauma subspecialties had higher video visit utilization than peripheral nerve or functional neurosurgery (Table 2, Supplemental Figure 3). During phase 3, a few subspecialties are notable for their continued high video visit utilization rate, specifically tumor (48.3%), trauma (60.9%), and pain (53.7%) (Table 2, Supplemental Figure 3).
Table 2.
Types of Outpatient Clinic Visits During 4 Phases of the COVID-19 Pandemic in the Neurosurgical Subspecialties
| Subspecialty | Type of Visit | Phase 0 12/31/2018–12/23/2019 |
Phase 1 12/30/2019–3/9/2020 |
Phase 2 3/16/2020–4/27/2020 |
Phase 3 5/4/2020–11/2/2020 |
P Value Phase 0 to Phase 1 | P Value Phase 0 to Phase 2 | P Value Phase 0 to Phase 3 | P Value Phase 2 to Phase 3 |
|---|---|---|---|---|---|---|---|---|---|
| Spine | Phone | 0% ± 0% | 0% ± 0% | 0.2% ± 0.6% | 1.4% ± 1.4% | <0.05 | <0.05 | <0.05 | <0.05 |
| Video | 0% ± 0% | 0% ± 0% | 67.9% ± 30.5% | 30.3% ± 13.1% | |||||
| In-person | 100% ± 0% | 100% ± 0% | 31.9% ± 30.5% | 68.4% ± 14% | |||||
| Tumor | Phone | 0% ± 0% | 0% ± 0% | 1.8% ± 1.9% | 2.3% ± 1.2% | <0.05 | <0.05 | <0.05 | <0.05 |
| Video | 0% ± 0% | 0% ± 0% | 60.7% ± 26.9% | 48.3% ± 6.7% | |||||
| In-person | 100% ± 0% | 100% ± 0% | 37.5% ± 27.8% | 49.5% ± 6.2% | |||||
| Vascular | Phone | 0% ± 0% | 0% ± 0% | 0% ± 0% | 0% ± 0% | <0.05 | <0.05 | <0.05 | <0.05 |
| Video | 0% ± 0% | 0% ± 0% | 30.4% ± 20.3% | 23.7% ± 13.6% | |||||
| In-person | 100% ± 0% | 100% ± 0% | 69.6% ± 20.3% | 76.3% ± 13.6% | |||||
| Pain | Phone | 0% ± 0% | 0% ± 0% | 0% ± 0% | 0.3% ± 1.1% | <0.05 | <0.05 | <0.05 | <0.05 |
| Video | 0% ± 0% | 0% ± 0% | 85.7% ± 37.8% | 53.7% ± 24.4% | |||||
| In-person | 100% ± 0% | 100% ± 0% | 14.3% ± 37.8% | 46% ± 24.3% | |||||
| Functional | Phone | 0% ± 0% | 0% ± 0% | 0% ± 0% | 0.4% ± 1.2% | <0.05 | <0.05 | <0.05 | <0.05 |
| Video | 0% ± 0% | 0% ± 0% | 10.7% ± 19.7% | 14.7% ± 12.8% | |||||
| In-person | 100% ± 0% | 100% ± 0% | 89.3% ± 19.7% | 84.8% ± 12.7% | |||||
| Peripheral Nerve | Phone | 0% ± 0% | 0% ± 0% | 0% ± 0% | 0.4% ± 1.6% | <0.05 | <0.05 | <0.05 | <0.05 |
| Video | 0% ± 0% | 0% ± 0% | 14.7% ± 19.7% | 17.7% ± 14% | |||||
| In-person | 100% ± 0% | 100% ± 0% | 85.3% ± 19.7% | 81.8% ± 14.4% | |||||
| Trauma | Phone | 0% ± 0% | 0% ± 0% | 0% ± 0% | 0.3% ± 1.7% | <0.05 | <0.05 | <0.05 | <0.05 |
| Video | 0% ± 0% | 0% ± 0% | 64.3% ± 47.6% | 60.9% ± 30.5% | |||||
| In-person | 100% ± 0% | 100% ± 0% | 35.7% ± 47.6% | 35.1% ± 28.9% | |||||
| Total | Phone | 0% ± 0% | 0% ± 0% | 0.8% ± 0.9% | 1.4% ± 0.5% | <0.05 | <0.05 | <0.05 | <0.05 |
| Video | 0% ± 0% | 0% ± 0% | 60.3% ± 27% | 37.4% ± 7% | |||||
| In-person | 100% ± 0% | 100% ± 0% | 38.9% ± 27.4% | 61.3% ± 7.2% |
Supplemental Figure 3.
Outpatient visit type (in-person: gray; phone: dark blue; video: orange) in 2020 versus in-person visits (light blue) in 2019 among neurosurgery providers. Stratified by subspecialty: spine (A), tumor (B), vascular (C), pain management (D), functional (E), peripheral nerve (F), and trauma (G).
Telephone visits were generally underutilized throughout the COVID-19 pandemic, making up less than 2% of visit types during all phases of our assessment.
Most neurosurgeons agreed or strongly agreed that telehealth visits are effective (84%) and efficient (92%). Eighty-four percent of neurosurgeons agreed or strongly agreed that they would continue to see patients via telehealth video visits after the COVID-19 pandemic. All trauma and pain neurosurgeons agreed or strongly agreed that telehealth video visits were appropriate for a large subset of their patients. There was not a consensus among the spine, tumor, and vascular providers regarding whether a large or small subset of their patients were appropriate for video visits (Figure 2 ).
Figure 2.
Internal survey results for neurosurgery providers regarding physician satisfaction with video visits (n = 13 responses).
Overall, patients were very satisfied with their video visits across all neurosurgical subspecialties. A total of 96% rated their video visit as “excellent” or “good”; 83% were “extremely” or “very likely” to recommend video visits. Additionally, 95% were “extremely” or “very likely” to recommend video visits with their provider, and 83% would choose a video visit over an in-person visit (Figure 3 ).
Figure 3.
Internal survey results of patient satisfaction with video visits from June 22, 2020, through November 2, 2020 (n = 521 responses).
We did not see any significant differences in patient LTR scores at any point before or during the COVID pandemic (Table 3 ).
Table 3.
Results of Stanford Press-Ganey Likelihood-to-Recommend (LTR) Scores from January 2019 Through August 2020
| Press-Ganey LTR | ||||||||
|---|---|---|---|---|---|---|---|---|
| Subspecialty | Phase 0 Jan 2019–Dec 2019 |
Phase 1 Jan 2020–Feb 2020 |
Phase 2 Mar 2020 - Apr 2020 |
Phase 3 May 2020–Aug 2020 |
P-value Phase 0 to Phase 1 |
P Value Phase 0 to Phase 2 |
P Value Phase 0 to Phase 3 |
P Value Phase 2 to Phase 3 |
| Spine | 84.4% ± 36.2% | 90.1% ± 29.9% | 91.3% ± 28.5% | 87.3% ± 33.5% | 0.1 | 0.21 | 0.45 | 0.48 |
| Tumor | 88.1% ± 32.4% | 87.7% ± 33.1% | 85.7% ± 35.6% | 81% ± 39.6% | 0.92 | 0.71 | 0.12 | 0.59 |
| Vascular | 87.9% ± 32.7% | 87.5% ± 33.8% | 85.7% ± 36.3% | 92.6% ± 26.7% | 0.96 | 0.81 | 0.49 | 0.49 |
| Functional | 91.1% ± 28.6% | 81.8% ± 39.5% | 100% ± 0% | 88.9% ± 32.3% | 0.19 | 0.35 | 0.77 | 0.32 |
| Peripheral Nerve | 95.1% ± 21.7% | 100% ± 0% | 85.7% ± 36.3% | 95% ± 22.4% | 0.58 | 0.17 | 0.99 | 0.36 |
| Trauma | 90.9% ± 30.2% | 100% ± 0% | 0.69 | |||||
| Total | 87.3% ± 33.3% | 88.7% ± 31.7% | 89.2% ± 31.2% | 87% ± 33.8% | 0.54 | 0.56 | 0.9 | 0.56 |
Discussion
Development and use of telehealth technologies have increased worldwide over the last decade. Prior to the COVID pandemic, the market value of telehealth in the United States was expected to reach $36.2 billion by 2022.4 In 2013, 22 million telehealth visits were performed in the United States, increasing to 30 million in 2017, with an anticipated 46–81 million telehealth visits by 2022.5 In June 2018, over 50% of U.S. hospitals had telehealth programs, and 90% of executives stated their hospitals were developing or had telehealth options.6 Another study reported that 76% of hospitals used telehealth in some capacity in 2017.7 In a 2017 survey, 66% of Americans stated they would be willing to see a doctor over video, including 72% of patients aged 45–54 years and 53% of those over 65 years old. Also, 53% of patients responded that they would be interested in using video visits for post-surgical or hospital stay follow-up.4
The COVID-19 pandemic has led to implementation of telehealth at rapid rates that far surpass these prior estimates. In this study, we present our institutional experience with outpatient neurosurgery telehealth visits during the COVID-19 pandemic. On average, the neurosurgery department saw a higher adoption of telehealth than the institution as a whole. There was a significant decrease in overall clinic volume during phase 2, when our region instituted its shelter-in-place order and the hospital canceled elective surgeries. All neurosurgical subspecialties except for vascular neurosurgery, which is primarily a non-elective subspecialty, saw a significant reduction in clinic visits during this time. During phase 3, we saw a revival in clinic visits across all neurosurgical subspecialties, with tumor and trauma exceeding the baseline period, although the volume of the primarily “elective” pain subspecialty still remained below pre-COVID levels.
These outpatient trends correlate with surgery cancellation estimates during the 12 peak weeks of the COVID-19 pandemic in North America and globally (which roughly correlates with our phase 2). Surgeries for benign disease in North America and globally were canceled at a rate of 83.1% and 81.7%, whereas cancer surgeries were canceled at a considerably lower rate of 31.0% and 37.7%.8
Although our clinic remained physically open throughout the COVID pandemic, telehealth video visits were highly utilized across all neurosurgical subspecialties, particularly at the peak of the outbreak (phase 2). Our findings are consistent with another single-site study that reported a 40-fold increase in telemedicine use in neurosurgery after shelter-in-place orders.9 At a high-volume tertiary care hospital in India, the neurosurgery center similarly relied on teleconsultations for outpatient visits during the pandemic and shutdown in India. This hospital found that patients coming in for postoperative visits or with vascular pathology or brain tumors were easily assessed and advised over video. However, peripheral nerve and spine pathologies that require examinations were harder to evaluate using telehealth.10
We also found that telehealth adoption was higher in spine, tumor, trauma, vascular, and interventional pain than in functional and peripheral nerve neurosurgery. Our internal survey reveals several potential reasons for these differences, including the difficulty of older patients with movement disorders such as Parkinson disease to perform televisits, the importance of the in-person physical exam to evaluate peripheral nerve patients, and an overall loss of important social cues and bonding between patient and physician in video visits. In a study on virtual visits for Parkinson disease patients, physicians rated video visits as only moderately favorable, and reported difficulty performing in-depth motor examinations remotely.11 In contrast, vascular neurosurgery may have adopted video visits well, as the National Institute of Health Stroke Scale can be performed reliably over video.12 Additionally, telestroke visits are well-documented and studied, and patients have generally reported positive experiences and improved quality of care.13 Similarly, pain patients may be uniquely well-suited for video visits, as these provide pain practitioners with an efficient way to assess pain and monitor progress/treatment efficacy in a more convenient setting for patients whose pain often limits their mobility. Video visits may also serve as an effective way for neurosurgeons to remotely monitor postoperative patients.14
Our work reveals that both patients and providers were generally satisfied with video visits. Press-Ganey LTR scores did not change during the period of time that video visits were implemented. These findings are consistent with survey responses from 254 patients and 61 physicians in psychiatry, neurology, cardiology, oncology, and primary care at Massachusetts General Hospital showing no difference in quality between video and in-person visits.15 These also likely reflect the multiple advantages of telehealth that have been touted in prior studies, including improved access to care and decreased patient wait, travel time, and cost. One study reported the average in-person doctor's visit takes 121 minutes, with only 20 minutes spent with the doctor. In contrast, the average video visit involves 5 minutes of waiting, and 8–10 minutes spent with the doctor.3
Our results support the findings of a recently published report from the neurosurgical department at Baylor College of Medicine in Houston, Texas, which reported a positive experience with telehealth for both providers and patients.16 Interestingly, however, only 46.3% of the patients in their study (vs. 80.8% of our patients) preferred video visits over in-person visits. This may reflect logistical differences in our clinic at Stanford versus the Baylor clinic, ease of access, and/or patient demographics. In addition, only 42.5% of their providers preferred telehealth visits over in-person visits, and only 27.5% of their providers felt their telehealth clinical exam was comprehensive.
This latter point underscores an important drawback of telehealth—namely, the inability to perform an in-person physical examination. Other disadvantages include reimbursement challenges and lack of technology access/familiarity with telehealth technologies (from both the provider and patient perspectives). Reimbursement has been addressed by the 1135 Waiver, which allows Medicare coverage for telehealth services at the same level as in-person visits. Many commercial insurance companies are taking similar steps to ensure that patients are seen over video visits, although this is changing throughout the pandemic. Clinic staff have also increased their familiarity with telehealth technology. Many places now include step-by-step computer video visit guides to patients and provide staff support to call patients if they encounter difficulties.
A major limitation of our study is that we present the experience of one academic institution in one part of the country (Palo Alto, California), a high-income city in the United States. The patient demographics and socioeconomic status that our institution serves may have a positive impact on the adoption and satisfaction of telehealth. Studies have indicated a higher adoption of telehealth among patients who are educated and employed.17 Globally, the majority of experiential reports of telehealth during the COVID-19 pandemic have occurred in high-income countries such as the United States, whereas low- and middle-income countries have few publications indicating a stable telehealth program.18 , 19 Although telehealth may be effective for patient visits, a critical impediment to sustainable telehealth programs may be the lack of resources, especially in lower-income countries. The disparities in telehealth adoption will need to be examined to achieve policy that will provide the option of telehealth for patients who will benefit regardless of socioeconomic status.
Our subspecialty findings are limited in that certain subspecialties have only 1 or 2 providers (peripheral nerve, functional), and thus individual provider preferences may significantly impact these subspecialty trends. In addition, we are unable to directly correlate patient satisfaction scores with visit type: specifically, new patient versus return versus postoperative visits. It is certainly possible that both patient and provider satisfaction with video visits changes as a result of the physical exam needs and bonding expectations of different visit types.
Multi-site studies are needed with more heterogeneous providers and patient populations to better understand the national and global impact of telehealth in neurosurgery. Further research into the cost-effectiveness and clinical efficiency of telehealth visits in neurosurgery is also warranted. In addition, an evaluation of new patient telehealth visits and whether patients proceed to surgery, with or without an in-person evaluation, would also be of great benefit to our field.
CONCLUSIONS
Patients and providers uniformly reported positive experiences with video visits at our institution. There are differences in telehealth utilization across neurosurgical subspecialties, with certain specialties (pain, tumor, trauma) being more amenable to video visits than others (e.g., peripheral nerve or functional neurosurgery). Patient LTR did not change with the implementation of video visits. Given these findings, we believe that telehealth will be a valuable tool for neurosurgeons to perform effective and efficient outpatient visits even after the COVID-19 pandemic.
CRediT authorship contribution statement
Christopher Leung: Methodology, Formal analysis, Investigation, Writing - original draft, Visualization. Harsh Wadhwa: Formal analysis, Writing - review & editing. Matthew Sklar: Methodology, Validation. Kunj Sheth: Conceptualization. Sophia Loo: Methodology. John Ratliff: Writing - review & editing. Corinna C. Zygourakis: Conceptualization, Writing - review & editing, Supervision.
Footnotes
Conflict of interest statement: C.C. Zygourakis is a consultant for Stryker, 7D, Globus, and SpineAlign.
Supplementary Data
References
- 1.Catalyst NEJM. What Is Telehealth? NEJM Catalyst. 2018. Available at: https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0268. Published February 1, 2018. 20 November 2020.
- 2.Aarnio P., Lamminen H., Lepistö J., Alho A. A prospective study of teleconferencing for orthopaedic consultations. J Telemed Telecare. 1999;5:62–66. doi: 10.1258/1357633991932405. [DOI] [PubMed] [Google Scholar]
- 3.Harden K.D. A ‘seismic shift’ moves medicine online during COVID-19 crisis through telehealth technology. https://www.steamboatpilot.com/news/a-seismic-shift-moves-medicine-online-during-covid-19-crisis-through-telehealth-technology Available at:
- 4.Americanwell.com. Telehealth Index: 2017 Consumer Survey. http://go.americanwell.com/rs/335-QLG-882/images/American_Well_Telehealth_Index_2017_Consumer_Survey.pdf Available at:
- 5.Mikulic M.U.S. telehealth visits 2013-2022. https://www.statista.com/statistics/820756/number-of-telehealth-visits-in-us Available at:
- 6.Sugapong G. Just the facts: 30 telehealth statistics for doctors to know. https://www.ortholive.com/blog/just-the-facts-30-telehealth-statistics-for-doctors-to-know Available at:
- 7.American Hospital Association Fact Sheet: Telehealth. https://www.aha.org/factsheet/telehealth Available at:
- 8.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans: elective surgery during the SARS-CoV-2 pandemic. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mouchtouris N., Lavergne P., Montenegro T.S., et al. Telemedicine in neurosurgery: Lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–e394. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raheja A., Agarwal N., Mohapatra S., et al. Preparedness and guidelines for neurosurgery in the COVID-19 era: Indian perspective from a tertiary care referral hospital. Neurosurg Focus. 2020;49:E3. doi: 10.3171/2020.9.FOCUS20564. [DOI] [PubMed] [Google Scholar]
- 11.Mammen J.R., Elson M.J., Java J.J., et al. Patient and physician perceptions of virtual visits for Parkinson’s disease: a qualitative study. Telemed J E Health. 2018;24:255–267. doi: 10.1089/tmj.2017.0119. [DOI] [PubMed] [Google Scholar]
- 12.Shafqat S., Kvedar J.C., Guanci M.M., Chang Y., Schwamm L.H. Role for telemedicine in acute stroke: feasibility and reliability of remote administration of the NIH stroke scale. Stroke. 1999;30:2141–2145. doi: 10.1161/01.str.30.10.2141. [DOI] [PubMed] [Google Scholar]
- 13.Johansson T., Wild C. Telemedicine in acute stroke management: systematic review. Int J Technol Assess Health Care. 2010;26:149–155. doi: 10.1017/S0266462310000139. [DOI] [PubMed] [Google Scholar]
- 14.Viers B.R., Lightner D.J., Rivera M.E., et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015;68:729–735. doi: 10.1016/j.eururo.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 15.Donelan K., Barreto E.A., Sossong S., et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25:40–44. [PubMed] [Google Scholar]
- 16.Mohanty A., Srinivasan V.M., Burkhardt J.-K., et al. Ambulatory neurosurgery in the COVID-19 era: patient and provider satisfaction with telemedicine. Neurosurg Focus. 2020;49:E13. doi: 10.3171/2020.9.FOCUS20596. [DOI] [PubMed] [Google Scholar]
- 17.Liaw W.R., Jetty A., Coffman M., et al. Disconnected: a survey of users and nonusers of telehealth and their use of primary care. J Am Med Inform Assoc. 2019;26:420–428. doi: 10.1093/jamia/ocy182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doraiswamy S., Abraham A., Mamtani R., Cheema S. Use of telehealth during the COVID-19 pandemic: scoping review. J Med Internet Res. 2020;22:e24087. doi: 10.2196/24087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scott R., Mars M. Telehealth in the developing world: current status and future prospects. Smart Homecare Technol Telehealth. 2015;3:25. [Google Scholar]