Abstract
Background
Evidence of the trend of the incidence of activities of daily living (ADL) disability among Chinese older people is limited. We aimed to investigate the time trends and potential risk factors for the incidence of ADL disability among Chinese older people (≥65 years).
Methods
We established two consecutive and nonoverlapping cohorts (6,857 participants in the 2002 cohort and 5,589 participants in the 2008 cohort) from the Chinese Longitudinal Healthy Longevity Survey. ADL disability was defined as the need for assistance with at least one essential activity (dressing, bathing, toileting, eating, indoor activities, and continence). Cox proportional hazards models were used to identify factors associated with the trend in the incidence of ADL disability from 2002 to 2014.
Results
The incidence (per 1,000 person-years) of ADL disability decreased significantly from 64.2 in the 2002 cohort to 46.6 in the 2008 cohort (p < .001), and decreasing trends in the incidence of ADL disability were observed for all sex, age, and residence subgroups (all p < .001), even after adjusting for multiple potential confounding factors. Moreover, we found that adjustment for sociodemographic, lifestyle information, and cardiovascular risk factors (hypertension, diabetes, heart disease, and stroke) explained less of the decline in ADL disability during the period from 2002 to 2014.
Conclusion
The incidence of ADL disability among the older adults in China appears to have decreased during the study period, and this finding cannot be explained by existing sociodemographic and lifestyle information and cardiovascular risk factors.
Keywords: Activities of daily living, Aging, China, Disability, Trends
Activities of daily living (ADL) disability is an adverse outcome of frailty that places a high burden on individuals and health care system (1). Several studies have reported that the incidence and prevalence of ADL disability have decreased in the past two decades in Western countries (2–4). In China, several studies have noted a decreased prevalence of ADL disability over the past decades among the older adults (5–7). The decreasing trend in the prevalence of ADL disability may be related to the decreasing incidence of ADL disability. However, the decreasing trends in the incidence of ADL disability have been documented by only one study using data from the China Health and Nutrition Survey from 1993 to 2006 (8); this work was limited by a relatively small sample size (n < 3,000). Furthermore, there have been no population-based studies evaluating the incidence of ADL disability during the last 10 years among Chinese older adults. The largest older adult population in the world currently, and for the foreseeable future, resides in China (9). Given that the profound impact of disability on quality of life and on health care system, elucidating time trends in ADL disability is expected to have important implications for public health.
ADL disability has been associated with numerous demographic factors (eg, age, sex, and residence) (10), lifestyle behaviors (eg, smoking status) (11), and cardiovascular risk factors (eg, hypertension, diabetes, and stroke) (12,13). Populations in several developed countries (eg, Netherlands) have observed increases in cardiovascular risk factors among the older adults (14,15), whereas trends in ADL disability are not consistently stable or in decline (16). Interestingly, the Chinese economy and health care system have changed dramatically over the past several years, leading to changes in factors that may influence ADL disability. Despite an increased prevalence of hypertension (from 18.0% to 29.6%) (17,18) and diabetes (from 5.5% to 11.6%) (19) from 2000 to 2010, the intensity of treatment for hypertension and diabetes has increased, with more patients achieving treatment goals. These treatment benefits may be translated into a net benefit manifesting as a decline in vascular-related risk factors for ADL disability. Given the increasing longevity of the world’s population (20), it is important to elucidate the longitudinal association between potential risk factors, especially cardiovascular risk factors, and ADL disability among the older adults.
In the present study, we used the Chinese Longitudinal Healthy Longevity Survey (CLHLS), a large nationally representative survey of community-based older adults, to estimate the incidence of ADL disability from 2002 to 2014. The current analysis also explored factors that may potentially contribute to ADL disability.
Methods
Setting and Participants
The study was based on the CLHLS, an ongoing national, community-based, longitudinal survey of the determinants of healthy aging for Chinese older adults. Details of the survey design have been described elsewhere (21,22). In brief, the CLHLS was based on a randomly selected sample of older adult individuals from 23 provinces in mainland China. The sampling area covered approximately 85% of the total population of China; the survey was initially launched in 1998, with subsequent implementation in the years 2000, 2002, 2005, 2008, 2011, and 2014. Younger older adult people (aged 65–79 years) were initially included in the CLHLS in the 2002 wave. Thus, to explore the age-related incidence of ADL disability in the older adults, we evaluated the data from two consecutive and nonoverlapping cohorts from CLHLS cohorts: the 2002 cohort (waves from 2002, 2005, and 2008) and the 2008 cohort (waves from 2008, 2011, and 2014). The first wave from each time period was considered the baseline survey; the two subsequent waves from each time period were considered follow-up surveys.
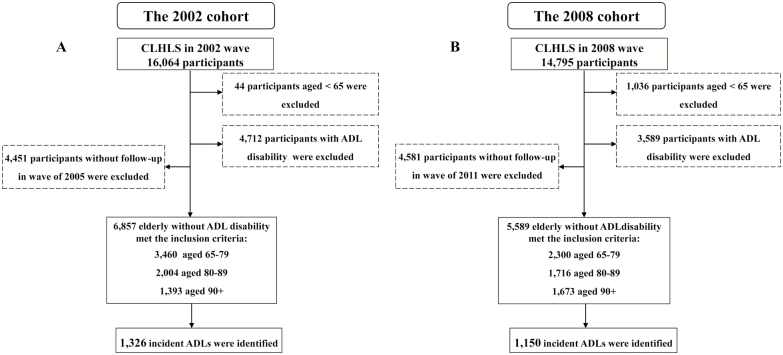
The final sample of older adult people who met the inclusion criteria (age ≥ 65 years, no ADL disability at baseline, and at least one follow-up visit) included 6,857 participants in the 2002 cohort and 5,589 participants in the 2008 cohort. In particular, the rates of ADL disability in the 2002 and 2008 cohorts were 29.3% and 24.3% at baseline, respectively. The characteristics of the participants in each cohort that died/lost to follow up were similar (Supplementary Table S1). A flowchart of participant enrollment in the present study is shown in Figure 1. All information of respondents was collected through in-home interviews, which were conducted by a well-trained local doctor/nurse and enumerator. The Research Ethics Committees of Peking University (IRB00001052-13074) granted approval for the CLHLS. All survey respondents or their proxy respondents provided informed consent before participation.
Figure 1.
Flowchart of the study population: the Chinese Longitudinal Healthy Longevity Survey, 2002–2014. (A) The 2002 cohort; (B) the 2008 cohort.
Ascertainment of ADL disability
ADL was assessed using the Katz Index scale (23), which includes six items: dressing, bathing, toileting, eating, indoor activities, and continence (24). The Chinese version of the questionnaire yields reliable and valid responses (25,26). Each item has three response options: “independent,” “needs help,” or “dependent.” An ADL disability was defined as a participant’s response of “independent” or “needs help” to at least one or more activities associated with one of the six items (4).
Covariates
Covariates were included and defined in this study as follows: sociodemographic information including age (in years), sex (male or female), residence (urban or rural), educational attainment (in years), and current marital status (married or not); lifestyle behaviors including smoking status (current smoker or nonsmoker), drinking status (current drinker or nondrinker), and regular exercise (yes or no); chronic medical conditions and cardiovascular risk factors including diabetes (yes or no), heart disease (yes or no), stroke (yes or no), and hypertension, which was defined as a self-reported diagnosis by a doctor or a systolic blood pressure ≥ 140 mm Hg and/or a diastolic blood pressure ≥ 90 mm Hg; and cognitive impairment (measured using the Mini-Mental State Examination), which was defined as a Mini-Mental State Examination score ≤ 18 (27).
Statistical Analysis
Overall, the missing data for any individual covariates amounted to less than 0.7%, and we used multiple imputation methods to correct for the missing covariate values through Multiple Imputation by Chained Equations (MICE) using the “mice” package in R software (28). For participants who remained free of ADL disability at their final survey point, the follow-up time was calculated from the baseline survey to the final survey. For those who developed ADL disability, the onset time of ADL disability was assumed to be at the midpoint between the two surveys owing to its insidious onset (8,29); thus, person-years of follow-up were estimated as the full time during which participants did not develop ADL disability plus half of the follow-up time during which ADL disability developed. Incidence rates (per 1,000 person-years) of ADL disability were calculated according to the number of person-years of follow-up.
The mean and SD (continuous variables) or number and proportion (categorical variables) were used to present the participants’ baseline characteristics. We pooled data from the 2002 cohort and the 2008 cohort and performed Cox proportional hazards analysis with a dichotomous dependent variable to indicate whether a participant had ADL disability. A trend variable that was assigned a value of 0 in the 2002 cohort and 1 in the 2008 cohort was included in the Cox proportional hazards models. A hazard ratio (HR) of less than 1 for this trend variable indicated a decrease in the incidence of ADL disability between the 2002 cohort and 2008 cohort. Time trends of ADL disability were assessed according to age group (65–79, 80–89, and ≥90 years), sex, and residence. Cox proportional hazards models were used to examine the association between various factors and ADL disability in both cohorts. We estimated 4 separate Cox proportional hazards models with different sets of independent variables that were added sequentially (Model 1: trend variable only [2002 cohort vs 2008 cohort]; Model 2: Model 1 plus age and sex; Model 3: Model 2 and sociodemographic variables; Model 4: Model 3 and health variables) to better assess which variables were associated with a change in the incidence of ADL disability between the 2002 cohort and the 2008 cohort. We tested for interactions between each independent variable and the cohort of observations with likelihood ratios. We used R software version 3.5.0 (R Foundation for Statistical Computing, Vienna, Austria) for analyses. A two-tailed P value less than .05 was regarded as significant.
Results
Characteristics of the Study Participants
The baseline characteristics of the participants in the 2002 cohort and the 2008 cohort are given in Table 1. The study population consisted of 12,546 participants, of whom 51.7% were women. Participants in the 2008 cohort were older and more likely to live in an urban area; to currently smoke; and to have hypertension, diabetes, and cognitive impairment (all p < .05). However, they were less likely to exercise regularly or drink alcohol (all p < .05) than those in the 2002 cohort.
Table 1.
Baseline Characteristics (Data Are Expressed as Counts [Percentages]) of 12,546 Chinese Older Participants in the Chinese Longitudinal Healthy Longevity Survey, 2002–2014
| Characteristic | The 2002 Cohort (n = 6,857) | The 2008 Cohort (n = 5,689) | P* |
|---|---|---|---|
| Age, y | <.001 | ||
| 65–79 | 3,460 (50.5) | 2,300 (40.4) | |
| 80–89 | 2,004 (29.2) | 1,716 (30.2) | |
| ≥90 | 1,393 (20.3) | 1,673 (29.4) | |
| Sex | .925 | ||
| Male | 3,280 (47.8) | 2,727 (47.9) | |
| Female | 3,577 (52.2) | 2,962 (52.1) | |
| Residence | <.001 | ||
| Urban | 2,858 (41.7) | 1,855 (33.5) | |
| Rural | 3,999 (58.3) | 1,993 (66.5) | |
| Educational attainment | 0.443 | ||
| Illiterate | 3,809 (55.5) | 3,200 (56.2) | |
| Literate | 3,048 (44.5) | 2,489 (43.8) | |
| Marital status | .009 | ||
| Married | 2,939 (42.9) | 2,572 (45.2) | |
| Unmarried | 3,918 (57.1) | 3,117 (54.8) | |
| Drinking status | .002 | ||
| Nondrinker | 5,180 (75.5) | 4,430 (77.9) | |
| Current drinker | 1,677 (24.5) | 1,259 (22.1) | |
| Smoking status | .981 | ||
| Nonsmoker | 5,295 (77.2) | 4,395 (77.3) | |
| Current smoker | 1,562 (22.8) | 1,294 (22.7) | |
| Regular exercise | <.001 | ||
| No | 4,150 (60.5) | 3,843 (67.6) | |
| Yes | 2,707 (39.5) | 1,846 (32.4) | |
| Cognitive impairment | 0.011 | ||
| No | 6,359 (92.7) | 5,205 (91.5) | |
| Yes | 498 (7.3) | 484 (8.5) | |
| Cardiovascular risk factors | |||
| Hypertension | 1,055 (15.4) | 1,148 (20.2) | <.001 |
| Diabetes | 129 (1.9) | 152 (2.7) | .004 |
| Heart disease | 560 (8.2) | 455 (8.0) | .755 |
| Stroke | 245 (3.6) | 241 (4.2) | .061 |
Note: *The chi-square test was employed.
Incidence and HRs of ADL Disability
Table 2 presents the incidence of ADL disability stratified by age, sex, and residence for the 2002 cohort and the 2008 cohort. After controlling for covariates, the incidence (per 1,000 person-years) of ADL disability decreased significantly from 64.2 in the 2002 cohort to 46.6 in the 2008 cohort (p < .001). The decrease in the incidence of ADL disability was significant (p < .001) for each age group: 65–79 years (25.8 vs 13.8), 80–89 years (66.7 vs 49.3), and ≥90 years (161.6 vs 110.7). The decline in the incidence of ADL disability was also significant (all p < .001) for men (51.9 in the 2002 cohort vs 36.6 in the 2008 cohort) and women (75.7 vs 56.2) and for those living in rural (60.2 vs 45.4) and urban (69.7 vs 49.1) areas.
Table 2.
Incidence Rates (per 1,000 Person-Years) of ADL Disability Stratified by Age, Sex, and Residence, 2002–2014
| Characteristic | The 2002 Cohort | The 2008 Cohort | Absolute Decrease | P b | ||||
|---|---|---|---|---|---|---|---|---|
| n/N | Person-Years | IRa | n/N | Person-Years | IR | |||
| All | 1,326/6,857 | 20,643.2 | 64.2 | 1,150/5,689 | 24,694.0 | 46.6 | 17.6 | <.001 |
| Age, y | ||||||||
| 65–79 | 257/3,460 | 9,957.5 | 25.8 | 161/2,300 | 11,685.6 | 13.8 | 12.0 | <.001 |
| 80–89 | 463/2,004 | 6,937.8 | 66.7 | 362/1,716 | 7,343.1 | 49.3 | 17.4 | <.001 |
| ≥90 | 606/1,393 | 3,749.0 | 161.6 | 627/1,673 | 5,665.3 | 110.7 | 50.9 | <.001 |
| Sex | ||||||||
| Male | 518/3,280 | 9,971.6 | 51.9 | 705/2,962 | 12,536.8 | 36.6 | 15.0 | <.001 |
| Female | 808/3,577 | 10,671.7 | 75.7 | 445/2,727 | 12,157.2 | 56.2 | 19.5 | <.001 |
| Residence | ||||||||
| Urban | 612/2,858 | 8,775.3 | 69.7 | 394/1,887 | 8,020.0 | 49.1 | 20.6 | <.001 |
| Rural | 714/3,999 | 11,868.0 | 60.2 | 756/3,802 | 16,674.1 | 45.4 | 14.8 | <.001 |
Notes: ADL = activities of daily living; IR = incidence rate.
aPer 1,000 person-years. bAdjusted for educational attainment (in y), current smoking status (yes or no), current drinking status (yes or no), hypertension (yes or no), heart disease (yes or no), stroke (yes or no), diabetes (yes or no), and cognitive impairment (yes or no); if applicable, adjusted for age (65–79, 80–89, and ≥90), sex (male or female), and residence (urban and rural).
Table 3 shows the results, using pooled data from the 2002 cohort and the 2008 cohort, of four different models with the incidence of ADL disability as the outcome variable. The trend variable in the first row of the table is the HR of ADL disability in the 2008 cohort compared with the 2002 cohort. Model 1 shows a significant decrease (HR: 0.72; 95% confidence interval [95% CI]: 0.66–0.78) in the unadjusted incidence of ADL disability; Model 2 shows the HR for the trend over time adjusted for age and sex (HR: 0.64; 95% CI: 0.59–0.70). After accounting for age and sex (Model 2, HR: 0.64; 95% CI: 0.61–0.73) or additional multiple risk factors (Model 3, HR: 0.67; 95% CI: 0.61–0.73, adjusted for educational attainment, marital status, smoking status, drinking status, and regular exercise), only 2%–3% of the decline in the incidence of ADL disability over time (from the 2002 cohort and the 2008 cohort) could be explained by cardiovascular risk factors (Model 4, HR: 0.66; 95% CI: 0.61–0.71). In the fully adjusted model, older age and a history of hypertension, diabetes, stroke, heart disease, and cognitive impairment were all associated with an increased risk of ADL disability (all p < .05). For the trend analyses, there were no significant interactions between the independent variables in the model (Supplementary Table S2).
Table 3.
Multivariable Hazard Ratios and 95% Confidence Intervals for the Incidence of ADL Disability in Men and Women, 2002–2014
| Characteristic | Models, HR (95% CI) | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| The 2008 cohort vs. the 2002 cohorta | 0.72 (0.66–0.78)* | 0.64 (0.59–0.70)* | 0.67 (0.61–0.73)* | 0.66 (0.61–0.71)* |
| Age (y) | 1.08 (1.07–1.08)* | 1.08 (1.07–1.08)* | 1.08 (1.07–1.08)* | |
| Female | 1.16 (1.07–1.26)* | 1.08 (0.97–1.19) | 1.06 (0.96–1.18) | |
| Residence | ||||
| Urban | 1.00 (reference) | 1.00 (reference) | ||
| Rural | 0.85 (0.78–0.92)* | 0.87 (0.80–0.94)* | ||
| Marital status | ||||
| Married | 1.00 (reference) | 1.00 (reference) | ||
| Unmarried | 0.98 (0.88–1.09) | 0.97 (0.87–1.07) | ||
| Educational attainment | ||||
| Illiterate | 1.00 (reference) | 1.00 (reference) | ||
| Literate | 0.95 (0.86–1.05) | 0.94 (0.85–1.04) | ||
| Smoking status | ||||
| Nonsmoker | 1.00 (reference) | 1.00 (reference) | ||
| Current smoker | 0.98 (0.88–1.08) | 0.98 (0.87–1.10) | ||
| Drinking status | ||||
| No | 1.00 (reference) | 1.00 (reference) | ||
| Yes | 0.83 (0.74–0.92)* | 0.85 (0.76–0.94)* | ||
| Regular exercise | ||||
| No | 1.00 (reference) | 1.00 (reference) | ||
| Yes | 1.01 (0.92–1.10) | 0.99 (0.91–1.08) | ||
| Cognitive impairment | 1.15 (1.02–1.30)* | |||
| Cardiovascular risk factors | ||||
| Hypertension | 1.25 (1.13–1.39)* | |||
| Heart disease | 1.26 (1.09–1.46)* | |||
| Stroke | 1.52 (1.26–1.84)* | |||
| Diabetes | 1.59 (1.23–2.04)* |
Notes: ADL = activities of daily living; CI = confidence interval; HR = hazard ratio.
aThe 2002 cohort as reference.
*p < .05.
Discussion
The present study of a nationally representative Chinese older adult sample provides updated evidence for trends in the incidence of ADL disability from 2002 to 2014. Our study demonstrates that the incidence of ADL disability in people aged 65 years and older decreased significantly from 2002 to 2014 and identifies decreases in sex, age, and resident subgroups. These trends in ADL disability were independent of risk factors, including sex, age, education, body mass index, physical activity, fruit and vegetable consumption, alcohol consumption, smoking status, major comorbidities, and other confounding factors. Although there has been an increase in the prevalence of cardiovascular risk factors over the past decades in China (30–32) and although we and others (33) have found that cardiovascular risk factors (eg, hypertension, diabetes, heart disease, and stroke) are associated with an increased risk of ADL disability in the older adults, cardiovascular risk factors explained very little of the decline in ADL disability over time (a decade) in China after adjustment for multiple potential risk factors (eg, sociodemographic information, lifestyle behaviors) for ADL disability. One plausible explanation is that cardiovascular risk factors have become less disabling over time owing to improvements in early diagnosis, medical treatment, and rehabilitation for these disorders (32,34).
Our findings are consistent with those of several studies in developed countries (2–7,35), which supports the hypothesis that the decreasing prevalence of ADL disability among the Chinese older adult population (6) is partly attributable to the decreasing incidence of ADL disability. Our current study of 12,546 Chinese older adults is consistent with a previous notably smaller (n < 3,000) study examining the incidence of ADL disability from 1993 to 2006 based on the China Health and Nutrition Survey (8). Hence, previous and present studies provide updated evidence describing the declining trends in the incidence of ADL disability from 1993 to 2014.
Although the exact reasons for the favorable decline in the incidence of ADL disability are not fully understood (8), this decline is probably determined by multiple complex and influential factors. One factor may be the considerable improvements in environmental factors and living conditions in the past decades in China. For example, the use of assistive technology (eg, walkers) and improvements in the home environment (eg, use of showers instead of bathtubs) (36,37) have improved the ADL capacity of the older adults. Other possible factors include advancements in medical and health services that lead to earlier diagnosis of and better treatments for chronic diseases (eg, hypertension and diabetes), which may decrease the incidence of ADL disability. Moreover, the risk factors of ADL disability identified in this study, such as old age, urban residence, suffering from cognitive impairment, hypertension, diabetes, stroke, and heart disease are also supported by the previous studies (38–40). Thus, the better prevention and treatment of disease, such as cognitive impairment, hypertension, diabetes, stroke, and heart disease, can reduce risk of ADL disability.
The major strength of this study is the nationwide sample derived from a large, longitudinal, population-based the CLHLS in China. Furthermore, the methods of data collection and survey questions in the present study have rarely changed over time. Nevertheless, our study also has several limitations. First, the use of self-reported information on lifestyle factors and cardiovascular risk factors might misestimate their true prevalence and associations with ADL disability. Second, although the potential effects of these factors on the time trends of ADL disability were examined, it was not possible to explore the effects of certain factors (eg, improved medical techniques and public transportation). Third, the time to ADL disability was defined as the period from baseline to the first time a participant developed disability; however, the participants might have developed this disability at any time during a 2- to 3-year interval, and the exact date of the event is not known, which might bias the current findings. Fourth, the 2002 and 2008 cohorts only allowed a 6-year comparison of the incidence of ADL disability. Further studies with a longer duration are needed to better analyze the trends in the incidence of ADL disability. Moreover, we did not consider whether those who died during the follow-up period had developed ADL disability, which might have resulted in underestimation of the incidence of ADL disability; however, our results were no material changed when the Cox models included participants who dropping out of the data as right censored (Supplementary Table S3).
Conclusions
In conclusion, this study provided evidence supporting a significant decline in the incidence of ADL disability among Chinese older adults from 2002 to 2014. However, the full set of sociodemographic information, lifestyle behaviors, and cardiovascular risk factors contributing to the decline in the incidence of ADL disability is still unknown. Continued monitoring of trends in the incidence of ADL disability will be important for better gauging the full future societal impact of ADL disability as the number of older adult individuals increases in the decades ahead and for clarifying potential protective and risk factors for ADL disability.
Funding
The Chinese Longitudinal Healthy Longevity Study (CLHLS), which provided the data analyzed in this article, is jointly supported by the National Natural Sciences Foundation of China (81573207, 71233001, 71490732, and 81573247) and the U.S. National Institute of Aging (2P01AG031719 and 3P01AG031719-07S1). This work also supported by the National Key R&D Program of China (2018YFC2000400) and the Construction of High-Level University in Guangdong (C1050008 and C1051007) and the University Revitalization Program in Eastern, Western and Northern Guangdong (G619080438). The funders played no role in study design or implementation; data collection, management, analysis, and interpretation; manuscript preparation, review, or approval; or the decision to submit the manuscript for publication.
Conflict of Interest
None reported.
Supplementary Material
References
- 1. Rochat S, Cumming RG, Blyth F, et al. Frailty and use of health and community services by community-dwelling older men: the Concord Health and Ageing in Men Project. Age Ageing. 2010;39:228–233. doi:10.1093/ageing/afp257 [DOI] [PubMed] [Google Scholar]
- 2. Freedman VA, Spillman BC, Andreski PM, et al. Trends in late-life activity limitations in the United States: an update from five national surveys. Demography. 2013;50:661–671. doi:10.1007/s13524-012-0167-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berlau DJ, Corrada MM, Peltz CB, Kawas CH. Disability in the oldest-old: incidence and risk factors in the 90+ study. Am J Geriatr Psychiatry. 2012;20:159–168. doi:10.1097/JGP.0b013e31820d9295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Angleman SB, Santoni G,Von Strauss E, Fratiglioni L. Temporal trends of functional dependence and survival among older adults from 1991 to 2010 in Sweden: toward a healthier aging. J Gerontol A Biomed Sci Med Sci. 2014;70:746–752. doi:10.1093/gerona/glu206 [DOI] [PubMed] [Google Scholar]
- 5. Feng Q, Zhen Z, Gu D, Wu B, Duncan PW, Purser JL. Trends in ADL and IADL disability in community-dwelling older adults in Shanghai, China, 1998–2008. J Gerontol B Psychol Sci Soc Sci. 2013;68:476–485. doi:10.1093/geronb/gbt012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liang Y, Song A, Du S, Guralnik JM, Qiu C. Trends in disability in activities of daily living among Chinese older adults, 1997–2006: the China Health and Nutrition Survey. J Gerontol A Biomed Sci Med Sci. 2014;70:739–745. doi:10.1093/gerona/glu204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Martin LG, Feng Q, Schoeni RF, Zeng Y. Trends in functional and activity limitations among Chinese Oldest-Old, 1998 to 2008. Popul Dev Rev. 2014;40:475–495. do:10.1111/j.1728-4457.2014.00694.x [Google Scholar]
- 8. Liang Y, Welmer AK, Wang R, Song A, Fratiglioni L, Qiu C. Trends in incidence of disability in activities of daily living in Chinese older adults: 1993–2006. J Am Geriatr Soc. 2017;65:306–312. doi:10.1111/jgs.14468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Peng X. China’s demographic history and future challenges. Science. 2011;333:581–587. doi:10.1126/science.1209396 [DOI] [PubMed] [Google Scholar]
- 10. Jiang J, Tang Z, Meng XJ, Futatsuka M. Demographic determinants for change in activities of daily living: a cohort study of the elderly people in Beijing. J Epidemiol. 2002;12:280–286. doi:10.2188/jea.12.280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Artaud F, Dugravot A, Sabia S, Singh-Manoux A, Tzourio C, Elbaz A. Unhealthy behaviours and disability in older adults: three-City Dijon cohort study. BMJ. 2013;347:f4240. doi:10.1136/bmj.f4240 [DOI] [PubMed] [Google Scholar]
- 12. Sousa RM, Ferri CP, Acosta D, et al. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet. 2009;374:1821–1830. doi:10.1016/S0140-6736(09)61829-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Andersen MM, Kritchevsky SB, Morgan TM, et al. Increased cardiovascular stiffness and impaired age-related functional status. J Gerontol A Biol Sci Med Sci. 2015;70:545–553. doi:10.1093/gerona/glu085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. van Gool CH, Picavet HSJ, Deeg DJ, et al. Trends in activity limitations: the Dutch older population between 1990 and 2007. Int J Epidemiol. 2011;40:1056–1067. doi:10.1093/ije/dyr009 [DOI] [PubMed] [Google Scholar]
- 15. Puts M, Deeg D, Hoeymans N, Nusselder W, Schellevis F. Changes in the prevalence of chronic disease and the association with disability in the older Dutch population between 1987 and 2001. Age Ageing. 2008;37:187–193. doi:10.1093/ageing/afm185 [DOI] [PubMed] [Google Scholar]
- 16. Lafortune G, Balestat G. Trends in severe disability among elderly people: assessing the evidence in 12 OECD countries and the future implications (OECD health working paper, No 26). Paris: Organisation for Economic Co-operation and Development; 2007. doi:10.1787/18152015 [Google Scholar]
- 17. Wu Y, Huxley R, Li L, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 2008;118:2679–2686. doi:10.1161/CIRCULATIONAHA.108.788166 [DOI] [PubMed] [Google Scholar]
- 18. Wang J, Zhang L, Wang F, Liu L, Wang H. Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens. 2014;27:1355–1361. doi:10.1093/ajh/hpu053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Xu Y, Wang L, He J, et al. ; 2010 China Noncommunicable Disease Surveillance Group . Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310:948–959. doi: 10.1001/jama.2013.168118 [DOI] [PubMed] [Google Scholar]
- 20. Beard JR, Officer A, de Carvalho IA, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387:2145–2154. doi:10.1016/S0140-6736(15)00516-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lv YB, Gao X, Yin ZX, et al. Revisiting the association of blood pressure with mortality in oldest old people in China: community based, longitudinal prospective study. BMJ. 2018;361:k2158. doi:10.1136/bmj.k2158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zeng Y, Feng Q, Hesketh T, Christensen K, Vaupel JW. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet. 2017;389:1619–1629. doi:10.1016/S0140-6736(17)30548-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi:10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- 24. Lv YB, Yuan JQ, Mao C, et al. Association of body mass index with disability in activities of daily living among Chinese adults 80 years of age or older. JAMA Netw Open. 2018;1:e181915. doi:10.1001/jamanetworkopen.2018.1915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yi Z, Vaupel JW, Zhenyu X, Chunyuan Z, Yuzhi L. The healthy longevity survey and the active life expectancy of the oldest old in China. Population. 2001;13:95–116. doi:10.2307/3030261 [Google Scholar]
- 26. Zeng Y, Poston DL, Vlosky DA, Gu D. Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions. Springer; 2008:61–79. doi:10.1080/00324720903216903 [Google Scholar]
- 27. Chei CL, Raman P, Yin ZX, Shi XM, Zeng Y, Matchar DB. Vitamin D levels and cognition in elderly adults in China. J Am Geriatr Soc. 2014;62:2125–2129. doi:10.1111/jgs.13082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8:3–15. doi:10.1177/096228029900800102 [DOI] [PubMed] [Google Scholar]
- 29. Liao WC, Li CR, Lin YC, et al. Healthy behaviors and onset of functional disability in older adults: results of a national longitudinal study. J Am Geriatr Soc. 2011;59:200–206. doi:10.1111/j.1532-5415.2010.03272.x [DOI] [PubMed] [Google Scholar]
- 30. Wong MC, Leung MC, Tsang CS, Lo SV, Griffiths SM. The rising tide of diabetes mellitus in a Chinese population: a population-based household survey on 121,895 persons. Int J Public Health. 2013;58:269–276. doi:10.1007/s00038-012-0364-y [DOI] [PubMed] [Google Scholar]
- 31. Liang Y, Liu R, Du S, Qiu C. Trends in incidence of hypertension in Chinese adults, 1991–2009: the China Health and Nutrition Survey. Int J Cardiol. 2014;175:96–101. doi:10.1016/j.ijcard.2014.04.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Liu M, Wu B, Wang WZ, Lee LM, Zhang SH, Kong LZ. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol. 2007;6:456–464. doi:10.1016/S1474-4422(07)70004-2 [DOI] [PubMed] [Google Scholar]
- 33. Heiland EG, Welmer AK, Wang R, Santoni G, Fratiglioni L, Qiu C. Cardiovascular risk factors and the risk of disability in older adults: variation by age and functional status. J Am Med Dir Assoc. 2019;20:208–212.e3. doi:10.1016/j.jamda.2018.05.013 [DOI] [PubMed] [Google Scholar]
- 34. Yang W, Lu J, Weng J, et al. ; China National Diabetes and Metabolic Disorders Study Group . Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–1101. doi:10.1056/NEJMoa0908292 [DOI] [PubMed] [Google Scholar]
- 35. Sulander T, Martelin T, Sainio P, Rahkonen O, Nissinen A, Uutela A. Trends and educational disparities in functional capacity among people aged 65–84 years. Int J Epidemiol. 2006;35:1255–1261. doi:10.1093/ije/dyl183 [DOI] [PubMed] [Google Scholar]
- 36. Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi:10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- 37. Falk H, Johansson L, Ostling S, et al. Functional disability and ability 75-year-olds: a comparison of two Swedish cohorts born 30 years apart. Age Ageing. 2014;43:636–641. doi:10.1093/ageing/afu018 [DOI] [PubMed] [Google Scholar]
- 38. Vermeulen J, Neyens JC, van Rossum E, Spreeuwenberg MD, de Witte LP. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr. 2011;11:33. doi:10.1186/1471-2318-11-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wong E, Backholer K, Gearon E, et al. Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013;1:106–114. doi:10.1016/S2213-8587(13)70046-9 [DOI] [PubMed] [Google Scholar]
- 40. den Ouden ME, Schuurmans MJ, Arts IE, van der Schouw YT. Physical performance characteristics related to disability in older persons: a systematic review. Maturitas. 2011;69:208–219. doi:10.1016/j.maturitas.2011.04.008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.