Abstract
Objective
Recent policy making aims to prevent health systems, lectronic health record (EHR) vendors, and others from blocking the electronic sharing of patient data necessary for clinical care. We sought to assess the prevalence of information blocking prior to enforcement of these rules.
Materials and Methods
We conducted a national survey of health information exchange organizations (HIEs) to measure the prevalence of information blocking behaviors observed by these third-party entities. Eighty-nine of 106 HIEs (84%) meeting the inclusion criteria responded.
Results
The majority (55%) of HIEs reported that EHR vendors at least sometimes engage in information blocking, while 30% of HIEs reported the same for health systems. The most common type of information blocking behavior EHR vendors engaged in was setting unreasonably high prices, which 42% of HIEs reported routinely observing. The most common type of information blocking behavior health systems engaged in was refusing to share information, which 14% of HIEs reported routinely observing. Reported levels of vendor information blocking was correlated with regional competition among vendors and information blocking was concentrated in some geographic regions.
Discussion
Our findings are consistent with early reports, revealing persistently high levels of information blocking and important variation by actor, type of behavior, and geography. These trends reflect the observations and experiences of HIEs and their potential biases. Nevertheless, these data serve as a baseline against which to measure the impact of new regulations and to inform policy makers about the most common types of information blocking behaviors.
Conclusion
Enforcement aimed at reducing information blocking should consider variation in prevalence and how to most effectively target efforts.
Keywords: health information exchange, interoperability, information blocking, electronic health records, health information technology
INTRODUCTION
A decade of concerted effort to achieve interoperable health information exchange has revealed myriad challenges.1 One persistent challenge is that health information exchange between health systems and across electronic health record (EHR) vendors’ platforms may not be perceived as strategically beneficial to these entities.2–4 For health systems, health information exchange may make it easier for competitors to gain market share by facilitating patient receipt of care via more seamless access to their prior medical history.3 For EHR vendors, the high cost to health systems associated with switching vendors may make it appealing to charge high prices for additional services, such as connectivity to other applications.5 Further, limiting sharing of information with other vendors may make it more difficult for healthcare providers to easily switch between vendors’ platforms.6,7 These incentives can lead to business practices that actively block the sharing of information.
While there is limited data on the extent of information blocking, defined as a practice that “is likely to interfere with, prevent, or materially discourage access, exchange, or use of electronic health information,”8 the anecdotal and empirical data that do exist suggest that information blocking is common.9,10 In response, the 2016 21st Century Cures Act targeted these behaviors by requiring that they be specifically defined and by identifying the actors—healthcare providers, EHR vendors, and health information exchange networks and exchanges—that would be subject to penalties if found to engage in them (though disincentives were not specified). After extensive debate, the Office of the National Coordinator for Health Information Technology (ONC) published the Cures Act final rule on May 1, 2020 to implement the information blocking provision in the 21st Century Cures Act. It specifies the actors that are subject to the provisions and establishes “exceptions” to the provisions: 8 categories of reasonable and necessary activities that do not constitute information blocking (eg, when an actor does not fulfill a request to exchange patient information in order to protect an individual’s privacy).11
As we transition into the enforcement phase to curtail information blocking, it is critical to not only identify individual cases that merit enforcement but also to assess the impact of the regulation on overall levels of information blocking. Enforcement will largely depend on individual reports by individuals or organizations that encounter information blocking; however, it is likely that many instances of information blocking will not be reported, resulting in an incomplete, and potentially biased picture of the type and extent of behaviors that are occurring. Ongoing national data on information blocking would shed light on the prevalence of these behaviors in a manner that reports alone would not.
We therefore conducted a national survey of health information exchange organizations (HIEs) to assess the current state of information blocking. HIEs are well-positioned to provide surveillance data on information blocking behaviors of both healthcare providers and EHR vendors (which are included in the Cures Rule as “health IT developer of certified health IT”), 2 of the actors identified in the recently published ONC Cures Act final rule. As third-party organizations that enable interoperable exchange between healthcare organizations, HIEs directly observe these actors’ behaviors and also have a high level of technical sophistication to assess when lack of sharing is due to business practices versus legitimate exceptions. In surveying these organizations, we addressed 3 research questions: First, what is the prevalence of information blocking practices by EHR vendors and health systems? Second, what types of information blocking behaviors are EHR vendors and health systems engaging in? And finally, does the prevalence of information blocking behavior depend on the competitiveness of the local market? We examined this final question under the hypothesis that both health systems and EHR vendors would be more likely to block the sharing of information with other organizations, including their competitors, in highly competitive markets. Addressing these questions provides critical insight into information blocking practices across the United States prior to enforcement of regulations designed to reduce these practices.
MATERIALS AND METHODS
We initially identified 151 HIEs from prior lists used in censuses of these organizations,12 contacts with leaders in each state, and from lists maintained by the Strategic Health Information Exchange Collaborative (SHIEC) and eHealth Initiative (eHI). After screening these organizations, we excluded 45 from the sampling frame because they were not operational (23), had merged/were duplicates (9), did not work across healthcare system (7), or used a single technology (7 respondents, counted as 1). The survey was administered online to the director of each organization or to the person in the organization who had responded to our previous surveys between May 2019 and February 2020, and participants were offered a small financial incentive. Nonrespondents were contacted a minimum of 3 times. Of the 106 HIEs that met inclusion criteria, 89 (84%) completed the survey.
Survey instrument
The first information blocking question on the survey asked: “What proportion of EHR vendors have you encountered engaging in information blocking?” HIEs had 5 response options: (1) All, (2) Most, (3) Some, (4) Few, (5) Don’t know or N/A (Don’t interact with EHR vendors). We then asked: “Among vendors that engage in information blocking, how often do they do it?” HIEs had 4 response options: (1) Often/Routinely, (2) Sometimes, (3) Rarely/Never, (4) Varies by vendor, and (5) Don’t know. We repeated these 2 questions focusing on health systems rather than EHR vendors.
We asked HIEs to report on the forms of information blocking that they encountered with EHR vendors and health systems and provided hypothetical examples of each form (Supplementary Appendix Table 1). For EHR vendors, we included 5 options: (1) Price, (2), Contract Language, (3) Artificial Technical, Process, or Resource Barriers, (4) Refusal, and (5) Other. For health systems, we included 3 options: (1) Artificial Technical, Process, or Resource Barriers, (2) Refusal and (3) Other. For each form of information blocking, HIEs had 4 response options: (1) Never/Rarely, (2) Sometimes, (3) Often/Routinely, and (4) Don’t Know. The full survey instrument is included as a Supplementary Appendix.
Measures of developer and hospital competition
We combined survey data with the 2018 American Hospital Association Annual Survey and 2018 and 2017 Information Technology Supplement. These data contain information on hospitals’ membership in multihospital systems and their EHR vendor (ie, their primary EHR developer), which allowed us to measure competition within geographic areas served by each HIE (which HIEs reported on the survey as the Hospital Service Areas and States in which they provide services). When data on primary developer were not available in 2018, we used 2017 data.
We created a population-weighted average of developer competition and of health system competition for each HIE to evaluate the relationship between competition and information blocking.13,14 To create these measures, we identified all zip codes within the HIE’s service area, which HIEs self-reported as part of the survey. Using the Hospital Service Area File, we then identified the hospitals that treated patients in each zip code, and the total number of fee-for-service Medicare discharges from beneficiaries in that zip code that were treated at each hospital. For each zip code, we calculated 2 Herfindahl–Hirschman Indices (HHIs): 1 for the hospitals that treated patients in that zip code and 1 for the EHR vendors serving those hospitals. HHIs are commonly used measures of the extent of market concentration, with an HHI near zero indicating a perfectly competitive market and higher HHIs indicating greater concentration. A HHI of 1 indicates a monopolistic market. For each HIE service area, we weighted each zip code by the proportion of that service area’s fee-for-service Medicare discharges that originated from the zip code to give greater weight to more populous zip codes and then summed across all zip codes in the HIE’s service area. For instance, if an HIE’s service area contained only 2 zip codes, and the first zip code accounted for 10% of the service area’s population and the other accounted for 90%, we would multiply the first zip code’s HHI by 0.10 and the second by 0.90 and then sum.
Analysis
We first generated descriptive measures of the prevalence of information blocking practices by EHR vendors and by health systems. We measured prevalence along 2 dimensions: the proportion of EHR vendors and of health systems engaging in information blocking and the frequency with which they did so. We then cross-tabulated responses about the proportion of entities engaging in information blocking and the frequency with which they did so. This generated a more holistic assessment of the overall level of information blocking and revealed whether these 2 dimensions were correlated. A negative correlation between these dimensions would indicate that HIEs observed relatively few bad actors (ie, a small proportion of entities engaging in information blocking, but those that engaged did so frequently). A positive correlation would indicate that some HIEs observed a low proportion of entities engage in information blocking and also observed those entities doing so infrequently while other HIEs observed a high proportion of entities engage in information blocking and also observed them doing so frequently. We excluded HIEs that responded “don’t know” or did not respond from these calculations and plots.
Next, to assess how vendors and health systems engaged in information blocking, we generated descriptive measures of the frequency of forms of information blocking by vendors and health systems observed by HIEs. In calculating these measures, we again excluded nonresponses and responses of “don’t know” from both the numerator and denominator.
Finally, we examined the relationship between EHR vendor competition and their information blocking behaviors as well as between health system competition and their information blocking behaviors. Because our survey included many items measuring different dimensions of information blocking behaviors, we sought to create composite measures across correlated items. We used exploratory factor analysis to identify relationships between 10 survey items measuring information blocking behaviors (excluding only the “other” category listed above). We found 1 factor that consisted of all items related to developer information blocking practices and a second related to all items related to health system information blocking practices (Supplementary Appendix Table 1). We therefore summed survey items within each factor, creating 2 scales and divided the responses into high, medium, and low developer and health system information blocking by identifying terciles in each scale and compared these categories to levels of competition in the service area covered by each health system.
RESULTS
More than half of HIEs (55%) indicated that at least some EHR vendors engaged in information blocking, and 14% indicated that most or all vendors did so (Figure 1). In contrast, only 24% of respondents indicated that at least some health systems engaged in information blocking, with 6% indicating that most did so.
Figure 1.
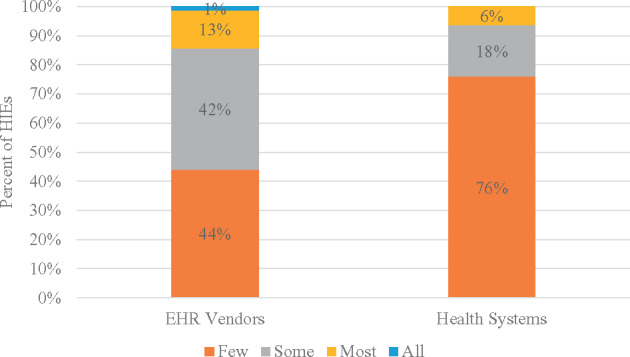
Proportion engaging in information blocking.
A majority (55%) of HIEs reported that EHR vendors sometimes, often, or routinely engage in information blocking, while only 30% of HIEs reported the same frequencies among health systems. (Figure 2) The single most common response for both vendors and health systems was that frequency of information blocking varied by the specific organization. Responses to the proportion of EHR vendors that engaged in information blocking and the frequency that those entities engaged in information blocking were moderately correlated (Spearman’s rank correlation of 0.40; Supplementary Appendix Figure 1); the correlation was stronger for health systems (0.66; Supplementary Appendix Figure 2).
Figure 2.
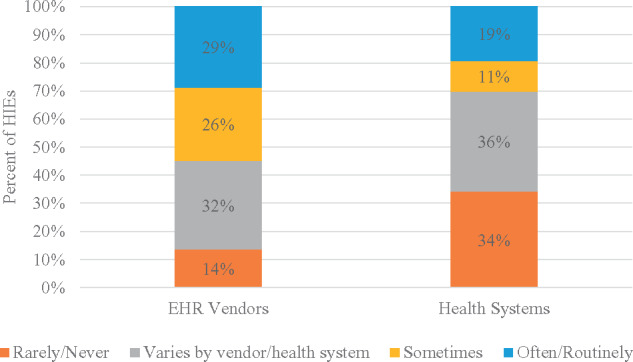
Frequency of information blocking among EHR vendors and health systems that engage in it.
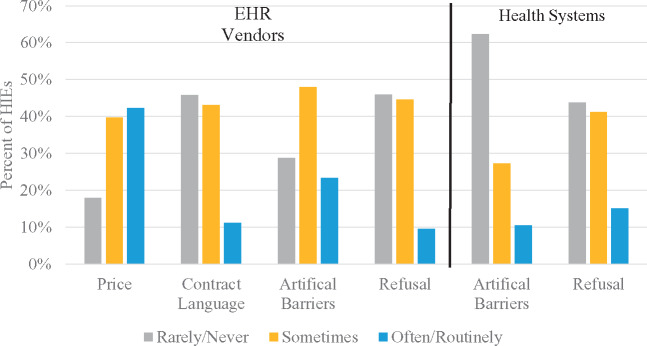
Among vendors, the most common form of information blocking was through price, with 42% of HIEs reporting that they often or routinely observed information blocking through price (Figure 3). Artificial barriers were the next most common form of information blocking: 23% of HIEs reporting that they often/routinely observed it. Contract language and refusal were less commonly reported as often/routinely occurring (11% and 9%, respectively) but were still frequently reported as “sometimes” occurring (43% and 45%, respectively). Among health systems, refusal was the most common form of information blocking, with 15% of HIEs reporting that this often/routinely occurred and 41% reporting that health systems sometimes engaged in it. Artificial barriers were less common, with only 10% of HIEs reporting often/routinely experiencing it and 27% reporting sometimes experiencing it.
Figure 3.
Frequency of forms of information blocking.
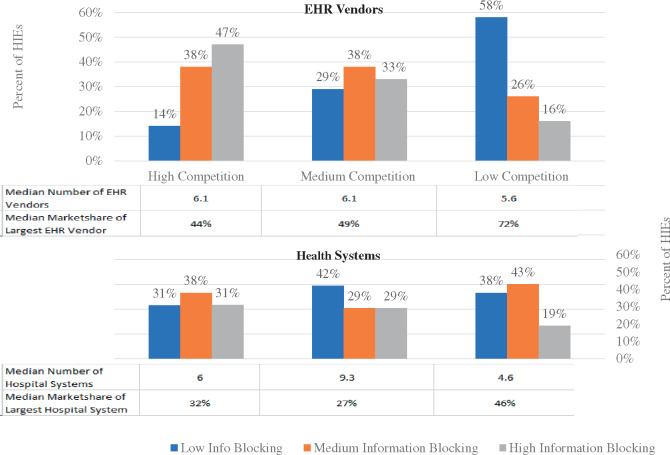
Greater developer competition was associated with higher reported levels of information blocking (Figure 4). In relatively competitive developer markets, 47% of HIEs reported high levels of information blocking by vendors, and 14% reported low levels. In contrast, 16% of HIEs located in relatively low competition markets reported high levels of information blocking, while 58% reported low levels of information blocking. This trend was less evident for health system competition with the same percent of HIEs (31%) indicating high and low information blocking in markets with high health system competition. In less competitive markets, 19% of HIEs reported high levels of information blocking, and 38% reported low levels of information blocking.
Figure 4.
Relationship between information blocking prevalence and competition.
Note: For each HIE, the number of hospital systems/vendors represents the weighted average number of systems/vendors that discharge patients from each zip code covered by the HIE. For each HIE, market share represents the weighted average of hospital discharges across all zip codes served by the HIE that occur at the hospital system/by hospitals using the vendor that serves the largest share of patients for that zip code.
DISCUSSION
The regulations enforcing key provisions of the 21st Century Cures Act are important steps to address the persistent problem of silos of information across the health system. Our baseline data reveal that information blocking is prevalent, with over half of HIEs reporting that at least some EHR vendors engage in it and one quarter of HIEs reporting that at least some health systems do so. Reduction in information blocking behaviors is therefore a critical component of policy efforts to facilitate greater sharing of patient information. As enforcement of the new regulations begins, surveillance of stakeholders with knowledge of information blocking, including HIEs, will be critical to identify where reductions occur, where information blocking practices persist, and how best to target continued efforts.
Our findings are notably consistent with a prior information blocking survey of HIEs in 2016. In both surveys, HIEs reported encountering moderate levels of information blocking by EHR vendors and health systems, and EHR vendors were reported to engage in information blocking substantially more often in both surveys.9 This consistency suggests that HIE survey responses about information blocking are reliable, an essential property of any data source. HIE survey data therefore provide an important baseline against which to measure the impact of enforcement efforts moving forward. More importantly, this consistency indicates that information blocking remains common 5 years after the initial congressional report on the issue and subsequent actions.
Given persistently high levels of information blocking reported by knowledgeable actors, our findings support the importance of defining and addressing it through the planned implementation of the final regulation, definition of penalties, and enforcement for those found to engage in information blocking.15 Our findings also provide insight into how enforcement efforts might be targeted and one useful approach to monitoring their effectiveness.
Our survey data offer a broad view of the information blocking behaviors observed by HIEs and indicates that there is substantial information blocking activity across actors and types of behavior. The enforcement approach, which will rely primarily on complaints to identify potential information blocking, is likely to identify important and egregious instances of information blocking but may provide an incomplete portrait of the full breadth of information blocking behaviors. For instance, relative to EHR vendors, a substantially larger proportion of health systems’ information blocking was through outright refusal, which is a more obvious form of information blocking. This may lead to high rates of reported complaints. In contrast, high prices, the most common way that vendors engaged in information blocking, may be viewed as more subjective and therefore more challenging to identify and use as a basis for enforcement. Broad monitoring could indicate where enforcement efforts are most effective and where they less effectively identify and reduce information blocking, suggesting ways to retarget efforts.16
Our data provide some insight into how to effectively approach individual enforcement of information blocking. We found a high degree of correlation between the proportion of entities that engaged in information blocking and the frequency with which they did so (as well as other dimensions). In other words, when an HIE observes that actors are high in 1 measure, the HIE is also likely to observe that they are high in others (and vice versa). This positive correlation suggests that there are information blocking “hot spots”—with some areas of the country that have high levels of information blocking among many actors and other areas in which the number of entities and frequency of information blocking are low. However, this correlation only holds within entity types, as EHR vendor and health system behaviors were not correlated. Therefore, developer information hot spots are different than health system ones.
Areas of high and low information blocking could arise due to different market dynamics affecting vendors and health systems in a given market. Supporting this, we found a strong correlation between EHR vendor competition and information blocking, with more developer information blocking reported in markets in which vendors were more competitive with each other (but not necessarily high levels of health system competition). This relationship is consistent with a reactive form of information blocking—where vendors engage in these behaviors in markets that are already competitive, perhaps to maintain or marginally gain market share. This is in contrast to proactive information blocking in which information blocking by a few vendors in a concentrated market could work to prevent that market from becoming more competitive. The reactive form of information blocking is consistent with prior evidence that showed higher levels of information exchange between hospitals in markets with a single dominant developer, even among those hospitals that did not use the dominant developer’s EHR, relative to more competitive markets that had lower overall exchange.7 Taken together, these findings suggest that sharing data is viewed as particularly strategically disadvantageous in areas with multiple EHR vendors and no clear market-dominant developer. Vendors may view these markets as less settled and actively engage in behaviors that provide competitive advantages, and the extent to which this occurs may depend on the specific vendors operating in a given area.7,17
While competition between health systems is also correlated with information blocking by health systems, the relationship is not as strong as among vendors. This may be due to nuances in how health systems choose to share information. Prior work on health system behavior has indicated that these systems may strategically choose how and with whom to exchange information to reflect their business interests.18,19 Similarly, health systems may not pursue information exchange with specific partners with whom they are highly competitive despite a need for such exchange because competitors often treat a shared patient population.20 Though not all of these practices represent information blocking, they do indicate the influence of idiosyncratic market dynamics on health system behavior. This suggests the need for further research to identify why more health systems engage in information blocking in certain areas and to target business practices that represent active information blocking. Policy makers, particularly those leading enforcement efforts, may want to proactively investigate information blocking “hot spots,” which are markets where information blocking appears to occur at higher levels due to developer competition and other dynamics.
Limitations
The measures used to assess information blocking in this survey do not completely capture information blocking as defined in current regulations because the final regulations were published after the survey was fielded and therefore did not probe about the prevalence of exceptions to information blocking. Specifically, the survey did not ask about all of the actors who may engage in information blocking, including HIEs themselves, and used the terminology “EHR vendors” rather than “health IT developers” which is the term used in the rule and covers a broader set of actors.11 Although HIEs are uniquely situated to provide insights into EHR vendors’ and providers’ information blocking practices, they may not have complete insight into these practices and when lack of information sharing is for legitimate reasons. Thus, our measures may underestimate some forms of information blocking, while potentially overestimating others (for instance, HIEs could not have assessed whether observed information blocking occurred because of exceptions that were defined in the published rule after the survey was fielded). Further, HIEs’ responses may not be completely unbiased and in particular HIEs may in some cases find themselves in competition with vendors in providing interoperability capability, which may be reflected in their perception of information blocking. Given the multiple actors involved, gathering insights from various perspectives will be necessary to obtain a complete and unbiased assessment of information blocking for ongoing surveillance.
CONCLUSION
Our study offers baseline measures of the prevalence of information blocking behaviors among 2 key actors. As regulation in this area continues, these measures will indicate whether information blocking activities are decreasing and, in particular, whether the rate of change in information blocking varies across the different actors that might engage in information blocking, the specific forms they pursue, and the dynamics of local markets that may alter incentives to block information. Such insights are essential in order to assess the effects of these regulations on a complex and pervasive barrier to interoperability.
FUNDING
Jordan Everson received support from the Agency for Healthcare Research and Quality under award 5K12HS026395-02. The opinions expressed in this document are those of the authors and do not reflect the official position of AHRQ or the US Department of Health and Human Services. Julia Adler-Milstein received support from a contract from the Office of the National Coordinator for Health IT (HHSP233201700049C).
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
CONFLICT OF INTEREST STATEMENT
None declared.
Supplementary Material
REFERENCES
- 1. Lin SC, Everson J, Adler‐Milstein J. Technology, incentives, or both? Factors related to level of hospital health information exchange. Health Serv Res 2018; 53 (5): 3285–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Miller AR, Tucker C. Health information exchange, system size and information silos. J Health Econ 2014; 33: 28–42. [DOI] [PubMed] [Google Scholar]
- 3. Everson J, Adler‐Milstein J. Sharing information electronically with other hospitals is associated with increased sharing of patients. Health Serv Res 2020; 55 (1): 128–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vest JR, Gamm LD. Health information exchange: persistent challenges and new strategies. J Am Med Inform Assoc 2010; 17 (3): 288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Eastaugh SR. The total cost of EHR ownership: healthcare organizations should consider support costs, upgrade fees, and other long-term costs of EHR systems in determining the total cost of ownership. Healthc Financ Manage 2013; 67 (2): 66–71. [PubMed] [Google Scholar]
- 6.Office of the National Coordinator for Health Information Technology. Report to Congress: Report on Health Information Blocking. Washington, DC: Department of Health and Human Services; 2015. [Google Scholar]
- 7. Everson J, Adler-Milstein J. Engagement in hospital health information exchange is associated with vendor marketplace dominance. Health Aff 2016; 35 (7): 1286–93. [DOI] [PubMed] [Google Scholar]
- 8.21st Century Cures Act, Pub. L. No. 114-255 Stat. §107 Stat. 2226 (2016).
- 9. Adler‐Milstein J, Pfeifer E. Information blocking: is it occurring and what policy strategies can address it? Milbank Q 2017; 95 (1): 117–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pylypchuk Y, Johnson C, Patel V. (March 2020). State of Interoperability and Methods Used for Interoperable Exchange among U.S. Non-federal Acute Care Hospitals in 2018 ONC Data Brief, No.51. Office of the National Coordinator for Health Information Technology: Washington DC. https://www.healthit.gov/sites/default/files/page/2020-03/State-of-Interoperability-among-US-Non-federal-Acute-Care-Hospitals-in-2018.pdf Accessed October 2, 2020. [Google Scholar]
- 11.Office of the National Coordinator for Health In. ONC's Cures Act Final Rule 2020. https://www.healthit.gov/curesrule/ Accessed October 2, 2020.
- 12. Adler-Milstein J, Lin SC, Jha AK. The number of health information exchange efforts is declining, leaving the viability of broad clinical data exchange uncertain. Health Aff 2016; 35 (7): 1278–85. [DOI] [PubMed] [Google Scholar]
- 13. Chang DC, Shiozawa A, Nguyen LL, et al. Cost of inpatient care and its association with hospital competition. J Am Coll Surg 2011; 212 (1): 12–9. [DOI] [PubMed] [Google Scholar]
- 14. Wong HS, Zhan C, Mutter R. Do different measures of hospital competition matter in empirical investigations of hospital behavior. Rev Ind Organ 2005; 26 (1): 27–60. [Google Scholar]
- 15. Black JR, Hulkower RL, Ramanathan T. Health information blocking: responses under the 21st Century Cures Act. Public Health Rep 2018; 133 (5): 610–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Measure the Impact of the ONC’s New Interoperability Rules Now. Health Affairs Blog, July 7, 2020. DOI: 10.1377/hblog20200701.58142.
- 17. Holmgren AJ, Adler-Milstein J, McCullough J. Are all certified EHRs created equal? Assessing the relationship between EHR vendor and hospital meaningful use performance. J Am Med Inform Assoc 2018; 25 (6): 654–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vest JR, Kash BA. Differing strategies to meet information‐sharing needs: publicly supported community health information exchanges versus health systems’ enterprise health information exchanges. Milbank Q 2016; 94 (1): 77–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vest JR, Campion TR, Kaushal R, Investigators H, for the HITEC Investigators. Challenges, alternatives, and paths to sustainability for health information exchange efforts. J Med Syst 2013; 37 (6): 9987. [DOI] [PubMed] [Google Scholar]
- 20. Everson J, Adler-Milstein J. Gaps in health information exchange between hospitals that treat many shared patients. J Am Med Inform Assoc 2018; 25 (9): 1114–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.