Abstract
Summary: We herein present the imaging findings in a case of diffuse primary cutaneous B-cell lymphoma of the cranial vault with orbital and brain invasion. MR imaging revealed first concomitant orbital and parenchymal invasion in a case of primary diffuse non-Hodgkin lymphoma of the cranial vault. Contrast-enhanced MR imaging revealed a diffuse mass in the scalp of the frontoparietal region bilaterally and invasion of the right orbit and left frontoparietal lobe. Histologic and immunopathologic examinations revealed diffuse primary cutaneous B-cell lymphoma.
Non-Hodgkin lymphoma represents only 3% to 4% of all neoplasms in the general population; however, it occurs more frequently in patients with AIDS. Direct involvement of the CNS occurs in only 1% to 2% of patients with lymphoma (1, 2). A literature search revealed that none of the reported cases included unilateral proptosis and diffuse involvement of cranial vault and brain parenchyma, as did the case reported herein.
Case Report
A 65-year-old man was admitted to the dermatology department because of a right frontoparietal nodule that included ulcers. He had had the lesions for 6 months and swelling on the right lid for 1 month. He had no other signs or symptoms. A dermatologic examination revealed a firm, nontender (10 × 8 cm) nodule that included several ulcers in the right frontoparietal region. Diffuse edema and erythema were observed on the right lid. He had several mobile lymph nodes measuring approximately 1 × 2 cm at the cervical region. The results of another dermatologic examination were normal. Corneal infiltration, orbital invasion, and proptosis were revealed by ophthalmologic examination. A laboratory examination showed that serum lactate dehydrogenase activity was 1135 U/L (normal range, 225–450 U/L). The results of other laboratory examinations were normal. The patient had no history of HIV definition and had not received any medication for this disease. CT of the thorax and abdomen showed no abnormal findings. Bone marrow biopsy showed hypocellularity but no findings of lymphoma or leukemia infiltrations.
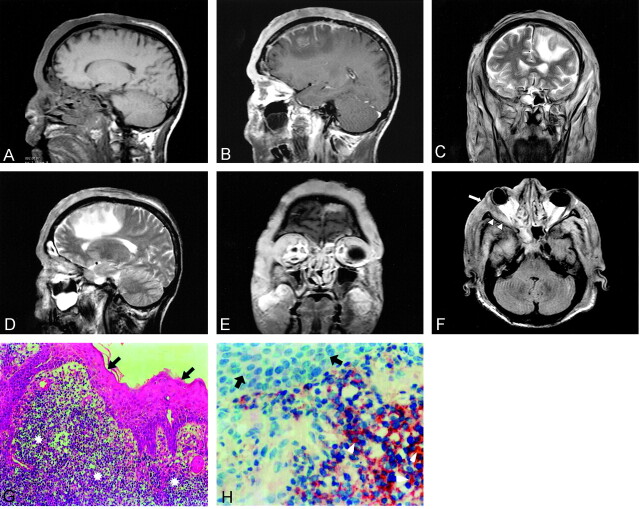
Unenhanced and contrast-enhanced sagittal T1-weighted MR imaging were performed. Marked contrast enhancement of a diffuse mass in the bilateral frontoparietal region of the scalp was shown. It was attached to the dura and vascular and medial frontal gyrus (Fig 1A and B). The coronal and sagittal T2-weighted images showed an isointense lesion and surrounding hyperintense edema on the left medial frontal gyrus (Fig 1C and D). Contrast-enhanced coronal T1-weighted images showed marked enhancement in the right lateral orbital wall and lateral rectus muscle, and axial fluid-attenuated inversion recovery images showed invasion of the orbital wall and the muscle (Fig 1E and F). We performed a wedge biopsy for further analysis under hematoxylin and eosin microscopy. The biopsy revealed a diffuse, large cell type of lymphoma. Histologic sections showed skin with a dermal and focal subcutaneous infiltrate composed of large cells with oval to irregular nuclei and vesicular chromatin. Immunohistochemistry revealed numerous positive cells reacting with CD20, which is a marker for B cells (Fig 1G and H).
Fig 1.
Images of a 65-year-old man who presented with a 6-month history of a right frontoparietal nodule that included ulcers and a 1-month history of swelling on the right lid.
A, Unenhanced sagittal T1-weighted MR image does not show any cranial invasion.
B, Contrast-enhanced sagittal T1-weighted MR image shows strong enhancement of a diffuse mass in the scalp bilateral frontoparietal region and invasion of the dura and left gyrus frontalis medius.
C, Coronal view T2-weighted image shows isointense lesion and peripheral hyperintense edema on the left medial frontal gyrus.
D, Sagittal T2-weighted image shows hyperintense edema on the frontal lobe.
E, Contrast-enhanced coronal T1-weighted image shows marked enhancement at the right lateral orbital wall and muscle rectus lateralis.
F, Axial fluid-attenuated inversion recovery image shows invasion of orbital wall (arrow) and muscle (arrowheads).
G, Photomicrograph of a specimen shows tumoral cells (stars) in stratified squamous epithelium (arrows) (hematoxylin and eosin; original magnification, ×200).
H, Photomicrograph shows CD20-positive tumoral cells (arrowheads) (strep ABC; original magnification, ×100) and stratified squamous epithelium (arrows).
Discussion
The incidence of CNS lymphoma has increased in both immunocompromised and immunocompetent persons (3). Non-Hodgkin lymphoma represents only 3% to 4% of all neoplasms in the general population; however, it is more common in patients with AIDS. Diffuse large B-cell lymphoma is an adult lymphoma accounting for 30% to 40% of all non-Hodgkin lymphomas, and the peak age at onset is during the 6th decade.
According to the Kiel classification, centroblastic lymphoma, immunoblastic B-cell lymphoma, and large cell anaplastic B-cell lymphoma are synonyms of diffuse large B-cell lymphoma. According to Revised European-American Classification of Lymphoid Neoplasms, the large B-cell tumors were formerly described as centroblastic, immunoblastic, and anaplastic together. Clinically, a rapidly growing, often painful mass can be seen to be of single nodal or extranodal size. The disease may primarily involve the skin, particularly in the head and neck region (4).
According to age, sex, and involved region, our case is similar to other cases reported in the literature (5–7). However, the case reported herein included the diverse features of unilateral proptosis and diffuse involvement of cranial vault and brain parenchyma. The initial symptoms and signs of lymphoma in the skull include a painless scalp lump, headache due to bone destruction or tumor infiltration of meninges, seizures, and focal neurologic deficits resulting from the cortex infiltration. The disease involves the pericranium, underlying meninges, and subcutaneous tissue. In most of the cases, no bone destruction occurs. Bone destruction may not be seen in some cases because of the characteristic permeating growth pattern of lymphoma with a large soft-tissue component and very little bone destruction (7,8).
The signal intensity on MR images is nonspecific; most reported cases of skull lymphomas report the signal intensity to be isointense on unenhanced MR images and to show marked enhancement on contrast-enhanced images. Even when cranial vault lymphoma is suspected, MR imaging is not definitively diagnostic because the appearance can mimic those of metastatic carcinoma, osteomyelitis, or meningioma. Cancer metastasis to the skull may show osteolytic bone lesion with extradural or intraparenchymal spread. Patients with osteomyelitis have lytic bone lesions and soft-tissue masses; however, the systemic signs are usually present by the time soft-tissue masses develop. Meningiomas would have associated hyperostosis (9). One case of primary non-Hodgkin lymphoma of cranial vault with associated proptosis is reported in the literature. This case was diagnosed as diffuse high grade large B-cell lymphoma of follicle center cell origin. The present case is the first report of proptosis related to B-cell type diffuse non-Hodgkin lymphoma. A literature search revealed that none of the reported cases included unilateral proptosis and diffuse involvement of cranial vault and brain parenchyma, as did the case reported herein.
Our extensive literature search indicated that this is the first case of orbital and parenchymal invasion associated with primary diffuse non-Hodgkin lymphoma of the cranial vault to be revealed by MR imaging. Although the prognostic factors of this rare tumor are unknown, invasion of the CNS is likely to indicate a poor prognosis (10).
Conclusion
MR imaging is helpful in showing diffuse primary cutaneous lymphoma of the cranial vault with orbital and brain invasion and can thus aid in the decision making regarding different treatment strategies by revealing the invasion of tumor.
References
- 1.Curty B, Kernan J, Favre J. Malignant non-Hodgkin’s lymphoma of the cranial vault: a case report. Br J Neurosurg 1997;11:433–436 [DOI] [PubMed] [Google Scholar]
- 2.Braus DF, Schwechheimer K, Muller-Hermelink HK, Schwarzkopf G, Volk B, Mundinger F. Primary cerebral malignant non-Hodgkin’s lymphomas: a retrospective clinical study. J Neurol 1992;239:117–124 [DOI] [PubMed] [Google Scholar]
- 3.Baleydier F, Galambrun C, Manel AM, Guibaud L, Nicolino M, Bertrand Y. Primary lymphoma of the pituitary stalk in an immunocompetent 9-year-old child. Med Pediatr Oncol 2001;36:392–395 [DOI] [PubMed] [Google Scholar]
- 4.Braun-Falco O, Pleving G, Wolff HH, Burgdarf WH. Dermatology. 2nd ed. Berlin: Springer-Verlag;2000. :1611–1640
- 5.Agbi CB, Bannister CM, Turnbull IW. Primary cranial vault lymphoma mimicking a meningioma. Neurochirurgia (Stuttg) 1983;26:130–132 [DOI] [PubMed] [Google Scholar]
- 6.Maiuri F, Corriero G, Giamundo A. Primary lymphoma of the cranial vault. J Neurosurg Sci 1987;31:183–186 [PubMed] [Google Scholar]
- 7.Holtas S, Monajati A, Utz R. Computed tomography of malignant lymphoma involving the skull. J Comput Assist Tomogr 1985;9:725–727 [DOI] [PubMed] [Google Scholar]
- 8.Parekh HC, Sharma RR, Keogh AJ, Prabhu SS. Primary malignant non-Hodgkin’s lymphoma of cranial vault: a case report. Surg Neurol 1993;39:286–289 [DOI] [PubMed] [Google Scholar]
- 9.Jamjoom AB, Jamjoom ZA, Naim-Ur-Rahman, Cheema MA. Primary midline cranial vault lymphoma simulating a parasagittal meningioma: the role of angiography in preoperative diagnosis. Neurosurg Rev 1998;21:202–205 [DOI] [PubMed] [Google Scholar]
- 10.Wendum D, Sebban C, Gaulard P, et al. Follicular large-cell lymphoma treated with intensive chemotherapy: an analysis of 89 cases included in the LNH87 trial and comparison with the outcome of diffuse large B-cell lymphoma: Groupe d’Etude des Lymphomes de l’Adulte. J Clin Oncol 1997;15:1654–1663 [DOI] [PubMed] [Google Scholar]