Abstract
Although paclitaxel plus bevacizumab (PB) therapy is an effective chemotherapeutic regimen for HER2-negative advanced breast cancer (ABC), predictive markers for its effectiveness remain undefined. We investigated the usefulness of systemic immunity markers associated with lymphocytes as predictive markers for PB therapy in patients with HER2-negative ABC. We retrospectively reviewed data from 114 patients with HER2-negative ABC who underwent PB therapy from November 2011 to December 2019. We calculated the absolute lymphocyte count (ALC), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and lymphocyte-to-monocyte ratio (LMR) as representative systemic immunity markers. The time to treatment failure (TTF) and overall survival (OS) of the patients with high ALC, low NLR, and high LMR were significantly longer compared with those of the patients with low ALC, high NLR, and low LMR. A multivariable analysis revealed that high ALC, low NLR, and low PLR were independent predictors for TTF and high ALC, low NLR, and high LMR were independent predictors for OS. Systemic immunity markers were significantly associated with longer TTF and OS in patients who underwent PB therapy and may represent predictive markers for PB therapy in patients with HER2-negative ABC.
Subject terms: Breast cancer, Medical research, Biomarkers, Oncology, Cancer therapy, Chemotherapy
Introduction
Paclitaxel plus bevacizumab (PB) therapy increases the progression-free survival (PFS) and overall response rate (ORR) of patients with human epidermal growth factor receptor 2 (HER2)-negative advanced breast cancer (ABC)1–4. The French Epidemiological Strategy and Medical Economics study reported a significant increase in overall survival (OS) with PB therapy for HER2-negative ABC5. In an earlier study, we showed significant increases in the time to treatment failure (TTF) and ORR for HER2-negative ABC and identified a patient subgroup in which OS benefited from PB therapy through propensity score matching6. However, biomarkers that identify patients who will experience a survival benefit from PB therapy remain unclear3,7.
Inflammatory cells and mediators in the tumor microenvironment play an important role in cancer progression8. The presence of an elevated peripheral neutrophil-to-lymphocyte ratio (NLR), a marker of systemic immunity, has been recognized as a poor prognostic factor in various cancers9,10. The absolute lymphocyte count (ALC)11, platelet-to-lymphocyte ratio (PLR)12, and lymphocyte-to-monocyte ratio (LMR)13 are also useful systemic immunity markers as a combined prognostic factor. The usefulness of these systemic immunity markers in association with lymphocytes as a combined prognostic marker has been investigated in breast cancer14–17. Studies have identified NLR and ALC as predictive markers for eribulin mesylate (eribulin) therapy for ABC18–20 and bevacizumab therapy for advanced non-small-cell lung cancer and metastatic colorectal cancer21,22. However, it is unclear whether these systemic immunity markers are useful as predictive markers for PB therapy in patients with ABC. Therefore, the aim of this retrospective study was to evaluate the effectiveness of these systemic immunity markers (ALC, NLR, PLR, and LMR) for predicting TTF and OS associated with PB therapy for HER2-negative ABC.
Results
Patient characteristics
We enrolled 122 patients with HER2-negative ABC who underwent PB therapy at the Fukuyama City Hospital (Japan) from November 2011 to December 2019. We excluded one patient due to missing systemic immunity marker data and seven patients who had not undergone at least two cycles of PB therapy. The final study sample included 114 patients whose characteristics at the beginning of PB therapy are shown in Table 1. Of these, 82 (71.9%) were estrogen receptor (ER)-positive, 93 (81.6%) had multiple (≥ 3) metastatic sites, and 93 (81.6%) had visceral metastases. Patient characteristics based on systemic immunity marker status are shown in Supplemental Table S1. Patients exhibiting high ALC had previously undergone fewer chemotherapy regimens for ABC compared with those exhibiting low ALC. There was no difference between the high and low NLR groups, high and low PLR groups, or high and low LMR groups (Supplemental Table S1).
Table 1.
Patient characteristics at the beginning of paclitaxel plus bevacizumab therapy.
| Variables | Number of patients (%) |
|---|---|
| Age, years, median (range) | 62.0 (32–89) |
| ER status | |
| Positive | 82 (71.9) |
| Negative | 32 (28.1) |
| Diagnosis | |
| Advanced | 44 (38.6) |
| Recurrence | 70 (61.4) |
| Metastatic sites | |
| CNS | 10 (8.8) |
| Bone | 61 (53.5) |
| Lungs | 55 (48.2) |
| Pleura and/or lymphangiopathy | 46 (40.4) |
| Lymph node | 90 (78.9) |
| Liver | 53 (46.5) |
| Soft tissue | 73 (64.0) |
| Type of metastases | |
| Visceral | 93 (81.6) |
| Non-visceral | 21 (18.4) |
| Number of metastatic sites, median (range) | 3.5 (1–8) |
| Number of metastatic sites | |
| ≥ 3 | 93 (81.6) |
| < 3 | 21 (18.4) |
| Prior (neo) adjuvant chemotherapy* | |
| Yes | 37 (32.5) |
| No | 77 (67.5) |
| Disease-free interval | |
| < 24 months | 67 (58.8) |
| ≥ 24 months | 47 (41.2) |
| Number of previous chemotherapies | |
| 0–1 | 89 (78.1) |
| ≥ 2 | 25 (21.9) |
CNS central nervous system, ER estrogen receptor.
*Chemotherapy included anthracycline and/or taxane.
Overall efficacy
The median follow-up time for the study was 17.9 months. The median chemotherapy regimen line before PB therapy was 0 (range 0–10). The overall efficacy of PB therapy for all included patients was as follows: ORR, 69.3%; median TTF, 210 days (95% confidence interval [CI] 196–250); and median OS, 538 days (95% CI 428–703).
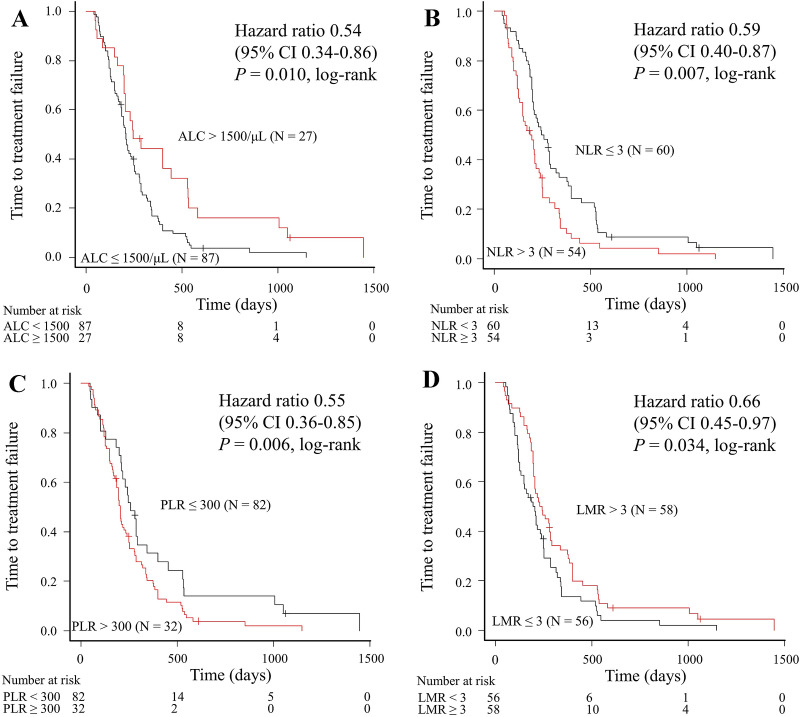
Correlation between systemic immunity markers and TTF
We compared TTF relative to the systemic immunity markers (Fig. 1). The TTF for patients with high ALC, low NLR, low PLR, and high LMR was significantly longer compared with that for patients with low ALC (245 days vs. 209 days, log-rank P = 0.010; Fig. 1A), high NLR (252 days vs .186 days, log-rank P = 0.007; Fig. 1B), high PLR (244 days vs. 173 days, log-rank P = 0.006; Fig. 1C), and low LMR (236 days vs. 196 days, log-rank P = 0.034; Fig. 1D), respectively.
Figure 1.
Time to treatment failure according to baseline levels of (A) ALC, (B) NLR, (C) PLR, and (D) LMR in patients treated with paclitaxel plus bevacizumab. ALC absolute lymphocyte count, CI confidence interval, LMR lymphocyte-to-monocyte ratio, NLR neutrophil-to-lymphocyte ratio, PLR platelet-to-lymphocyte ratio.
We performed univariable and multivariable analyses to evaluate independent predictors of PB therapy (Tables 2 and 3). Each of the four multivariable analyses identified high ALC, low NLR, and low PLR as independent predictive markers for TTF (P = 0.013, P = 0.023, and P = 0.004, respectively). The respective results of the four multivariate Cox regression analyses are shown in Supplemental Table S2.
Table 2.
Univariable analysis of time to treatment failure and overall survival (Cox hazard model).
| Variables | TTF | OS | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | |
| Age (≥ 65 vs. < 65 years) | 1.16 | 0.79–1.70 | 0.454 | 1.27 | 0.81–1.98 | 0.295 |
| ER (negative vs. positive) | 1.09 | 0.72–1.67 | 0.678 | 1.02 | 0.63–1.66 | 0.929 |
| Diagnosis (recurrence vs. advanced) | 1.36 | 0.92–2.00 | 0.127 | 1.35 | 0.86–2.14 | 0.195 |
| Metastatic sites (yes vs. no) | ||||||
| CNS | 1.28 | 0.66–2.47 | 0.463 | 1.39 | 0.67–2.89 | 0.380 |
| Bone | 0.96 | 0.65–1.40 | 0.818 | 0.98 | 0.63–1.53 | 0.945 |
| Lung | 0.58 | 0.39–0.86 | 0.007 | 0.65 | 0.42–1.02 | 0.060 |
| Pleura and/or lymphangiopathy | 0.97 | 0.66–1.43 | 0.876 | 0.83 | 0.53–1.30 | 0.425 |
| Lymph node | 0.97 | 0.61–1.54 | 0.895 | 0.77 | 0.46–1.31 | 0.334 |
| Liver | 1.37 | 0.93–2.00 | 0.110 | 1.44 | 0.92–2.24 | 0.109 |
| Soft tissue | 0.76 | 0.51–1.14 | 0.184 | 0.92 | 0.59–1.45 | 0.729 |
| Visceral metastasis (yes vs. no) | 0.81 | 0.50–1.31 | 0.392 | 0.96 | 0.55–1.68 | 0.880 |
| Number of metastatic sites (≥ 3 vs. < 3) | 0.70 | 0.43–1.14 | 0.153 | 0.79 | 0.45–1.38 | 0.403 |
| Prior (neo) adjuvant chemotherapy* (yes vs. no) | 1.54 | 1.02–2.32 | 0.039 | 1.28 | 0.80–2.05 | 0.304 |
| Disease-free interval (< 24 months vs. ≥ 24 months) | 1.16 | 0.79–1.70 | 0.438 | 1.23 | 0.79–1.91 | 0.367 |
| Number of previous chemotherapies (< 2 vs. ≥ 2) | 0.90 | 0.57–1.41 | 0.644 | 0.46 | 0.28–0.75 | 0.002 |
| Marker of systemic immunity | ||||||
| ALC > 1500/μL versus ALC ≤ 1500/μL | 0.54 | 0.34–0.86 | 0.010 | 0.38 | 0.21–0.71 | 0.002 |
| NLR ≤ 3 versus NLR > 3 | 0.59 | 0.40–0.87 | 0.007 | 0.54 | 0.35–0.84 | 0.006 |
| PLR ≤ 300 versus PLR > 300 | 0.55 | 0.36–0.85 | 0.006 | 0.65 | 0.40–1.06 | 0.083 |
| LMR > 3 versus LMR ≤ 3 | 0.66 | 0.45–0.97 | 0.034 | 0.58 | 0.37–0.90 | 0.016 |
ALC absolute lymphocyte count, CI confidence interval, CNS central nervous system, ER estrogen receptor, HR hazard ratio, LMR lymphocyte-to-monocyte ratio, NLR neutrophil-to-lymphocyte ratio, OS overall survival, PLR platelet-to-lymphocyte ratio, TTF time to treatment failure.
*Chemotherapy included anthracycline and/or taxane.
Table 3.
Multivariable analysis of time to treatment failure and overall survival (Cox hazard model).
| Variable | TTF | OS | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | |
| ALC > 1500/μL versus ALC ≤ 1500/μL | 0.53 | 0.32–0.88 | 0.013 | 0.44 | 0.23–0.82 | 0.010 |
| NLR ≤ 3 versus NLR > 3 | 0.63 | 0.43–0.94 | 0.023 | 0.62 | 0.39–0.99 | 0.045 |
| PLR ≤ 300 versus PLR > 300 | 0.51 | 0.33–0.81 | 0.004 | 0.63 | 0.38–1.02 | 0.062 |
| LMR > 3 versus LMR ≤ 3 | 0.70 | 0.47–1.03 | 0.069 | 0.60 | 0.38–0.96 | 0.034 |
ALC absolute lymphocyte count, CI confidence interval, HR hazard ratio, LMR lymphocyte-to-monocyte ratio, NLR neutrophil-to-lymphocyte ratio, OS overall survival, PLR platelet-to-lymphocyte ratio, TTF time to treatment failure.
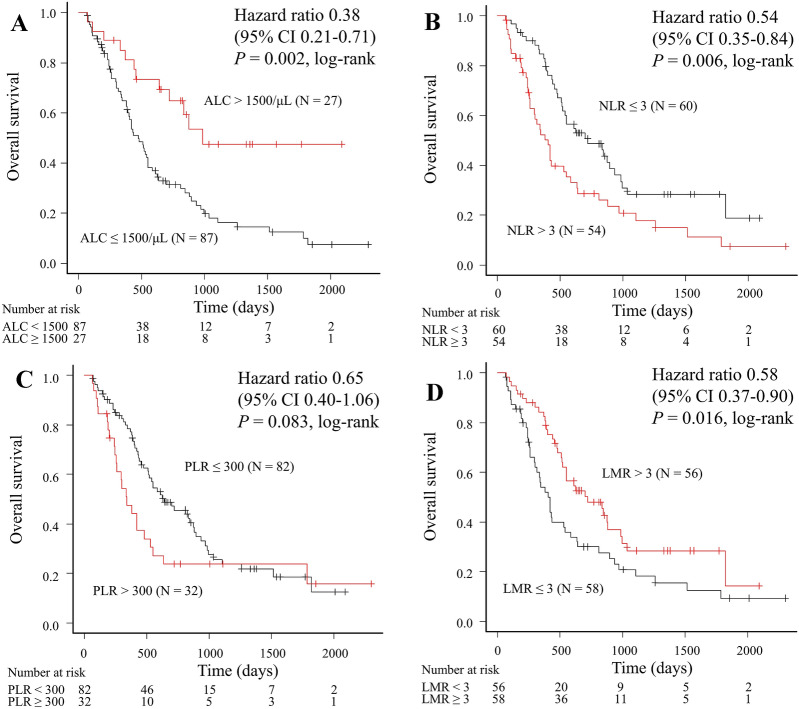
Correlation between systemic immunity markers and OS
We compared OS relative to the systemic immunity markers (Fig. 2). The OS for patients with high ALC, low NLR, and high LMR was significantly longer compared with that for patients with low ALC (988 days vs. 475 days, log-rank P = 0.002; Fig. 2A), high NLR (722 days vs. 403 days, log-rank P = 0.006; Fig. 2B), and low LMR (722 days vs. 418 days, log-rank P = 0.016; Fig. 2D), respectively. Although PLR showed a favorable tendency, no significant difference was observed (639 days vs. 342 days, log-rank P = 0.083 for low PLR; Fig. 2C).
Figure 2.
Overall survival according to baseline levels (A) ALC, (B) NLR, (C) PLR, and (D) LMR in patients treated with paclitaxel plus bevacizumab. ALC absolute lymphocyte count, CI confidence interval, LMR lymphocyte-to-monocyte ratio, NLR neutrophil-to-lymphocyte ratio, PLR platelet-to-lymphocyte ratio.
We performed univariable and multivariable analyses to evaluate independent predictors of PB therapy (Tables 2 and 3). Each of the four multivariable analyses identified high ALC, low NLR, and high LMR as independent predictive markers for OS (P = 0.010, P = 0.045, and P = 0.034, respectively). The respective results of the four multivariate Cox regression analyses are shown in Supplemental Table S3.
Correlation between systemic immunity markers and ORR
We compared the ORR relative to the systemic immunity markers and found no significant differences in ORR between the groups: 81.5% and 65.5% for the patients with high and low ALC, respectively (P = 0.15); 76.7% and 61.1% for the patients with low and high NLR, respectively (P = 0.10); 73.2% and 59.4% for the patients with low and high PLR, respectively (P = 0.18); and 74.1% and 64.3% for the patients with high and low LMR, respectively (P = 0.31).
Safety
Of the 114 patients, 81 (71.1%) discontinued PB therapy as a result of disease progression, 16 (14.0%) discontinued because of adverse events, 12 (10.5%) discontinued due to “other reasons,” and 5 (4.4%) continued the therapy to the data cut-off point. There were no new recorded therapy-related adverse events.
Discussion
Our results identified that patients with HER2-negative ABC and high ALC, low NLR, and low PLR at baseline had significantly improved TTF compared with those with low ALC, high NLR, and high PLR, respectively. We also found that high ALC, low NLR, and high LMR were associated with longer OS. We demonstrated the usefulness of these systemic immunity markers as predictive markers of PB therapy for patients with HER2-negative ABC. These markers can be easily calculated from readily available blood tests routinely measured in clinical practice.
Recent studies have demonstrated that systemic immunity markers (ALC, NLR, PLR, and LMR) are associated with better outcomes for patients with various carcinomas, including breast cancer9–17. It has been reported that a low ALC before the initiation of systemic therapy is associated with shorter OS and PFS in advanced carcinomas, sarcomas, and lymphomas. In addition, a low baseline ALC is strongly associated with reduced disease-free survival (DFS) (hazard ratio [HR] 5.24, 95% CI 2.23–12.30, P < 0.001) and OS (HR 6.13, 95% CI 2.21–17.0, P < 0.001) for patients with breast cancer who undergo primary chemotherapy11,14. High ALC (≥ 1000/μL or 1500/µL) was identified as an independent predictive marker for better OS in patients with ABC receiving eribulin therapy19,20. In a previous meta-analysis of patients with unselected solid tumors, high NLR was associated with poor OS (HR 1.81, 95% CI 1.67–1.97, P < 0.001). In patients with breast cancer, high NLR (higher than the cut-off value) was significantly associated with poor OS (HR 2.56, 95% CI 1.96–3.35, P < 0.001) and DFS (HR 1.74, 95% CI 1.47–2.07, P < 0.001)10,15. Further, low NLR (< 3) at baseline was significantly associated with longer PFS18 and OS20 in patients treated with eribulin in ABC, thereby demonstrating that low NLR (< 3) was an independent predictive marker for eribulin therapy. It has been reported that high PLR is associated with shorter OS for various solid tumors and a meta-analysis showed that high PLR was associated with poor OS (HR 1.55, 95% CI 1.07–2.25, P = 0.022) and DFS (HR 1.73, 95% CI 1.30–2.30, P < 0.001) in patients with breast cancer12,16. Another systematic review and meta-analysis that included 11,197 patients from 29 studies showed that low LMR (lower than the cut-off) was associated with poor OS (HR, 1.73 95% CI 1.55–1.93, P < 0.001) and DFS (HR 1.56, 95% CI 1.31–1.86, P < 0.001) in non-hematologic solid tumors13. Ni et al. demonstrated that high LMR predicted a favorable response and prognosis in ABC17. However, the utility of PLR and LMR as predictive markers for patients with ABC remains unclear. Our results showed that high ALC (≥ 1500/µL) and low NLR (< 3) were associated with longer TTF and OS compared with low ALC and high NLR, respectively. Furthermore, we found that low PLR was associated with longer TTF and high LMR was associated with longer OS.
Our results support those of a previous study reporting that systemic immunity marker expression at the beginning of PB therapy exhibited a significant association with improved prognosis and that these markers were readily available as predictive markers of PB therapy in ABC23. In contrast, NLR and ALC showed no significant association with increased PFS and OS in patients with ABC treated with nab-paclitaxel or a treatment of the physician’s choice, such as taxanes18,20. In advanced non-small-cell lung cancer and metastatic colorectal cancer, NLR was associated with survival outcome and was useful as a predictive marker in patients treated with combination chemotherapy and bevacizumab, but not with chemotherapy alone21,22. Therefore, we conclude that systemic immunity markers can be useful as predictive markers by addition of bevacizumab to chemotherapy.
Recently, vascular endothelial growth factor (VEGF) has been recognized as an important mediator of immune suppression, and VEGF blockade may be effective in the antitumor immune response in addition to its direct effects on tumor vasculature. VEGF modulates the various processes of cancer immunity, including promotion of T-regulatory cells, suppression of dendritic cell maturation, stimulation of tumor-associated macrophages, and infiltration of myeloid-derived suppressor cells, leading to an immunosuppressive state24. Given that bevacizumab modulates this immunosuppressive state through angiogenesis inhibition, a strategy that combines bevacizumab and immune checkpoint inhibitors has been explored. Combined ipilimumab and bevacizumab therapy in patients with melanoma resulted in encouraging antitumor activity and had beneficial effects on the host antitumor immune response25. In patients with metastatic non-squamous non-small-cell lung cancer, the addition of atezolizumab to bevacizumab and chemotherapy significantly increased PFS and OS26. Therefore, it is reasonable to suggest that systemic immunity markers can predict systemic antitumor activity resulting from PB therapy in patients with ABC.
This study had several limitations. First, it was a retrospective single-center study with a small number of subjects. Given that this was a single-center study, however, the patients were treated consistently and only two (1.8%) patients were untraceable. Second, the optimal cut-off values for the systemic immunity markers are unclear. Because the cut-off values for ALC at 1500/μL and NLR at 3 have often been reported as useful in ABC18,20,23, we followed these parameters. Finally, which systemic immunity marker is the most effective at predicting survival remains unclear. Therefore, further prospective studies are warranted to resolve this issue. Overall, our study demonstrated the usefulness of systemic immunity markers associated with lymphocytes as predictive markers of PB therapy for patients with HER2-negative ABC. We also demonstrated that these systemic immunity markers may play an important role in selecting candidates with HER2-negative ABC for bevacizumab therapy.
Methods
Study population and treatment
We reviewed the medical records of 114 patients with HER2-negative ABC who underwent at least two cycles of PB therapy at the Fukuyama City Hospital (Japan) from November 2011 to December 2019. We excluded patients with missing systemic immunity marker data and patients who had not undergone at least two cycles of PB therapy. The data cut-off was May 31, 2020. We defined the subtype from the pathology reports at the time of surgery, initial biopsy, or at the time of recurrence. The subtype was based on ER and HER2 expression, and ER-positivity was defined as ER ≥ 1% positive. HER2 overexpression was defined according to the American Society of Clinical Oncology/College of American Pathologists guidelines27.
The treatment schedule was the same as that of the E2100 study1: Bevacizumab (10 mg/kg) was administered on days 1 and 15 in combination with paclitaxel (90 mg/m2) on days 1, 8, and 15 of each 28-day cycle. Treatment was continued until disease progression, unacceptable toxicity, or patient/physician decision. Tumor response to treatment was assessed according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1, and the physician determined the timing of the lesion assessment.
All procedures that involved human subjects were performed in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This retrospective study was approved by the Fukuyama City Hospital’s review board. Informed consent was obtained in the form of an opt-out on the website from all individual participants included in the study.
Measurements of systemic immunity markers
Neutrophil, lymphocyte, platelet, and monocyte counts were performed automatically using a Sysmex XE-2100 or XE-5000 automated hematology system (Sysmex Co., Kobe, Japan). ALC, NLR, PLR, and LMR were calculated from blood cell counts prior to administering PB therapy, and the cut-off values for these markers were set in accordance with previous studies as follows: 1500/μL for ALC, 3 for NLR, 300 for PLR, and 3 for LMR12,13,15,20. All patients were divided into “low” and “high” groups according to the cut-off values, respectively: low ALC (≤ 1500/μL, n = 87), high ALC (> 1500/μL, n = 27); low NLR (≤ 3, n = 60), high NLR (> 3, n = 54); low PLR (≤ 300, n = 82), high PLR (> 300, n = 32); and low LMR (≤ 3, n = 56), high LMR (> 3, n = 58). Neutrophil, lymphocyte, platelet, and monocyte counts are routinely measured in clinical practice during treatment and the systemic immunity markers are easily calculated from these blood cell counts. Therefore, these markers can be measured and analyzed easily and inexpensively without additional equipment, software, or personnel specialized in analyzing the results.
Statistical analysis
The Wilcoxon rank sum test was used to compare continuous variables (such as median age) and Fisher’s exact test was used to compare the proportions of categorical variables (such as metastasis type) between groups. The distribution of TTF and OS was estimated by the Kaplan–Meier method. We performed a univariate Cox regression analysis to determine the association between baseline patient characteristics and TTF and OS. To evaluate the association between each systemic immunity marker (ALC, NLR, PLR, and LMR) and TTF or OS, we conducted a multivariate Cox regression analysis. We considered the baseline patient characteristics with P < 0.20 in the univariate Cox regression analysis as confounders and included them in the multivariate analysis. Since the systemic immunity markers (ALC, NLR, PLR, and LMR) were correlated with each other, we did not include these four markers simultaneously in the multivariate analysis. These markers were included independently in each multivariate analysis of TTF and OS. Finally, we performed this analysis eight times. A P value < 0.05 was considered statistically significant, and all statistical analyses were performed with EZR software (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria)28.
We defined TTF as the time from the administration of PB therapy to the discontinuation of treatment for any reason, including disease progression, treatment toxicity, patient/physician decision, and death from any cause. OS was defined as the time from the administration of PB therapy to the date of death from any cause. ORR was defined as the percentage of patients who achieved a complete or partial response according to the RECIST criteria.
Supplementary Information
Acknowledgements
We would like to thank Enago for editing a draft of this manuscript.
Author contributions
All authors contributed to the study conception and design. S.N. prepared the materials and performed the data collection and analysis. S.N. wrote the first draft of the manuscript, and all authors commented on the previous versions of the manuscript. All authors have read and approved the final manuscript.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Competing interests
Dr. Nakamoto reports having received personal fees from Chugai Pharmaceuticals, Eisai, and Taiho Pharmaceuticals outside of the submitted work; Dr. Ikeda reports having received personal fees from AstraZeneca, Chugai Pharmaceuticals, Daiichi-Sankyo, Eisai, Eli-Lilly, Kyowa Kirin, Pfizer, Nippon Kayaku, Novartis, Mundipharma, Celltrion Healthcare, and Sawai Pharmaceuticals outside of the submitted work; Dr. Kubo has received lecture fees from Eli-Lilly outside of the submitted work; Dr. Yamamoto has received lecture fees from Bayer outside of the submitted work. The other authors have no conflicts of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-85948-2.
References
- 1.Miller K, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N. Engl. J. Med. 2007;357:2666–2676. doi: 10.1056/NEJMoa072113. [DOI] [PubMed] [Google Scholar]
- 2.Gray R, Bhattacharya S, Bowden C, Miller K, Comis RL. Independent review of E2100: a phase III trial of bevacizumab plus paclitaxel versus paclitaxel in women with metastatic breast cancer. J. Clin. Oncol. 2009;27:4966–4972. doi: 10.1200/JCO.2008.21.6630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miles D, et al. Bevacizumab plus paclitaxel versus placebo plus paclitaxel as first-line therapy for HER2-negative metastatic breast cancer (MERiDiAN): a double-blind placebo-controlled randomised phase III trial with prospective biomarker evaluation. Eur. J. Cancer. 2017;70:146–155. doi: 10.1016/j.ejca.2016.09.024. [DOI] [PubMed] [Google Scholar]
- 4.Miles D, Cameron D, Hilton M, Garcia J, O'Shaughnessy J. Overall survival in MERiDiAN, a double-blind placebo-controlled randomised phase III trial evaluating first-line bevacizumab plus paclitaxel for HER2-negative metastatic breast cancer. Eur. J. Cancer. 2018;90:153–155. doi: 10.1016/j.ejca.2017.10.018. [DOI] [PubMed] [Google Scholar]
- 5.Delaloge S, et al. Paclitaxel plus bevacizumab or paclitaxel as first-line treatment for HER2-negative metastatic breast cancer in a multicenter national observational study. Ann. Oncol. 2016;27:1725–1732. doi: 10.1093/annonc/mdw260. [DOI] [PubMed] [Google Scholar]
- 6.Nakamoto S, Watanabe J, Ohtani S, Morita S, Ikeda M. Bevacizumab as first-line treatment for HER2-negative advanced breast cancer: paclitaxel plus bevacizumab versus other chemotherapy. In Vivo. 2020;34:1377–1386. doi: 10.21873/invivo.11917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miles DW, et al. Biomarker results from the AVADO phase 3 trial of first-line bevacizumab plus docetaxel for HER2-negative metastatic breast cancer. Br. J. Cancer. 2013;108:1052–1060. doi: 10.1038/bjc.2013.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 9.Guthrie GJ, et al. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit. Rev. Oncol. Hematol. 2013;88:218–230. doi: 10.1016/j.critrevonc.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 10.Templeton AJ, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J. Natl. Cancer Inst. 2014;106:124. doi: 10.1093/jnci/dju124. [DOI] [PubMed] [Google Scholar]
- 11.Ray-Coquard I, et al. Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res. 2009;69:5383–5391. doi: 10.1158/0008-5472.CAN-08-3845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Templeton AJ, et al. Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol. Biomark. Prev. 2014;23:1204–1212. doi: 10.1158/1055-9965.EPI-14-0146. [DOI] [PubMed] [Google Scholar]
- 13.Nishijima TF, Muss HB, Shachar SS, Tamura K, Takamatsu Y. Prognostic value of lymphocyte-to-monocyte ratio in patients with solid tumors: a systematic review and meta-analysis. Cancer Treat. Rev. 2015;41:971–978. doi: 10.1016/j.ctrv.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Vicente Conesa MA, et al. Predictive value of peripheral blood lymphocyte count in breast cancer patients treated with primary chemotherapy. Breast. 2012;21:468–474. doi: 10.1016/j.breast.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res. 2017;19:2. doi: 10.1186/s13058-016-0794-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu Y, et al. Platelet-lymphocyte ratio acts as an indicator of poor prognosis in patients with breast cancer. Oncotarget. 2017;8:1023–1030. doi: 10.18632/oncotarget.13714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ni XJ, et al. An elevated peripheral blood lymphocyte-to-monocyte ratio predicts favorable response and prognosis in locally advanced breast cancer following neoadjuvant chemotherapy. PLoS ONE. 2014;9:e111886. doi: 10.1371/journal.pone.0111886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miyagawa Y, et al. Significant association between low baseline neutrophil-to-lymphocyte ratio and improved progression-free survival of patients with locally advanced or metastatic breast cancer treated with eribulin but not with nab-paclitaxel. Clin. Breast Cancer. 2018;18:400–409. doi: 10.1016/j.clbc.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe J, Saito M, Horimoto Y, Nakamoto S. A maintained absolute lymphocyte count predicts the overall survival benefit from eribulin therapy, including eribulin re-administration, in HER2-negative advanced breast cancer patients: a single-institutional experience. Breast Cancer Res. Treat. 2020;181:211–220. doi: 10.1007/s10549-020-05626-1. [DOI] [PubMed] [Google Scholar]
- 20.Miyoshi Y, et al. High absolute lymphocyte counts are associated with longer overall survival in patients with metastatic breast cancer treated with eribulin-but not with treatment of physician's choice-in the EMBRACE study. Breast Cancer. 2020;27:706–715. doi: 10.1007/s12282-020-01067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Botta C, et al. Systemic inflammatory status at baseline predicts bevacizumab benefit in advanced non-small cell lung cancer patients. Cancer Biol. Ther. 2013;14:469–475. doi: 10.4161/cbt.24425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Passardi A, et al. Inflammatory indexes as predictors of prognosis and bevacizumab efficacy in patients with metastatic colorectal cancer. Oncotarget. 2016;7:33210–33219. doi: 10.18632/oncotarget.8901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miyagawa Y, et al. Baseline neutrophil-to-lymphocyte ratio and c-reactive protein predict efficacy of treatment with bevacizumab plus paclitaxel for locally advanced or metastatic breast cancer. Oncotarget. 2020;11:86–98. doi: 10.18632/oncotarget.27423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ott PA, Hodi FS, Buchbinder EI. Inhibition of immune checkpoints and vascular endothelial growth factor as combination therapy for metastatic melanoma: an overview of rationale, preclinical evidence, and initial clinical data. Front. Oncol. 2015;5:202. doi: 10.3389/fonc.2015.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hodi FS, et al. Bevacizumab plus ipilimumab in patients with metastatic melanoma. Cancer Immunol. Res. 2014;2:632–642. doi: 10.1158/2326-6066.CIR-14-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Socinski MA, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N. Engl. J. Med. 2018;378:2288–2301. doi: 10.1056/NEJMoa1716948. [DOI] [PubMed] [Google Scholar]
- 27.Wolff AC, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American society of clinical oncology/college of American pathologists clinical practice guideline update. J. Clin. Oncol. 2013;31:3997–4013. doi: 10.1200/jco.2013.50.9984. [DOI] [PubMed] [Google Scholar]
- 28.Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transpl. 2013;48:452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.