Abstract
BACKGROUND AND PURPOSE: Supracricoid horizontal partial laryngectomy (SCPL) is increasingly used to treat endolaryngeal carcinoma. However, few radiologic reports of these procedures exist. Our purpose was to evaluate the normal CT appearance of the neolarynx after surgery.
METHODS: SCPL includes cricohyoidopexy (CHP), cricohyoidoepiglottopexy (CHEP), and tracheocricohyoidoepiglottopexy (TCHEP). We examined CT scans obtained from 18 patients without local superficial recurrence who underwent SCPL: 10, CHEP; seven, CHP; and one, TCHEP. Three reference sections were used to analyze the main surgical reconstruction: an upper section through the hyoid bone, a lower section through the cricoid cartilage, and a middle section in between. The distance between the hyoid bone and cricoid cartilage was measured.
RESULTS: The epiglottis and valleculae were visible in the upper section in seven of 10 patients who underwent CHEP; this finding allowed distinction between CHEP and CHP. The arytenoids were depicted in 13 of 18 cases and reflected neolaryngeal shortening. The lower section showed the empty cricoid lumen lined by a thin mucosa; the anterior arch of the cricoid was amputated at TCHEP. The middle section showed the neovestibule, the lateral boundaries of which were the hypertrophic neoaryepiglottic folds; the anterior limit was the epiglottis for CHEP or the base of the tongue for CHP. The average distance between the hyoid bone and cricoid cartilage was 11 mm.
CONCLUSION: Normal CT anatomy of the larynx after SCPL is defined. Three key sections may accurately distinguish the various types of SCPL. CT is a valuable tool for depicting tumor recurrence, especially when the tumor is submucosal.
The surgical management of malignancies of the larynx consists of total or partial removal of the larynx. Radiation therapy may be used as a cure or as an adjunct after surgery. Total laryngectomy deprives the patient of all vocal function. Conservative laryngeal surgery preserves a portion of the larynx so that a voice can be produced. Therefore, respiration is preserved without a permanent tracheostomy, and swallowing is possible without aspiration. The main goal of conservative laryngeal surgery or radiation therapy is to preserve the physiologic functions of the larynx while obtaining the same local control as that provided by total laryngectomy (1–3).
Supracricoid horizontal partial laryngectomy (SCPL) was introduced more than 20 years ago (4–6) and includes cricohyoidopexy (CHP) (7, 8), cricohyoidoepiglottopexy (CHEP) (9), and tracheocricohyoidoepiglottopexy (TCHEP) (10). The term SCPL best describes the surgical resection performed, while the terms CHP, CHEP, and TCHEP describe the reconstructive procedures (7–10). The usual postoperative assessment of patients after SCPL consists of physical examination and indirect laryngoscopy to evaluate tumor recurrence. Local recurrence after SCPL can be difficult to detect, because the tumor often is submucosal, and indirect laryngoscopy discloses only hypertrophy of the remaining laryngeal tissue (11, 12). CT, which focuses more on the deep tissue, may be most useful for depicting these recurrences, but its use requires a thorough knowledge of the usual postoperative laryngeal anatomy.
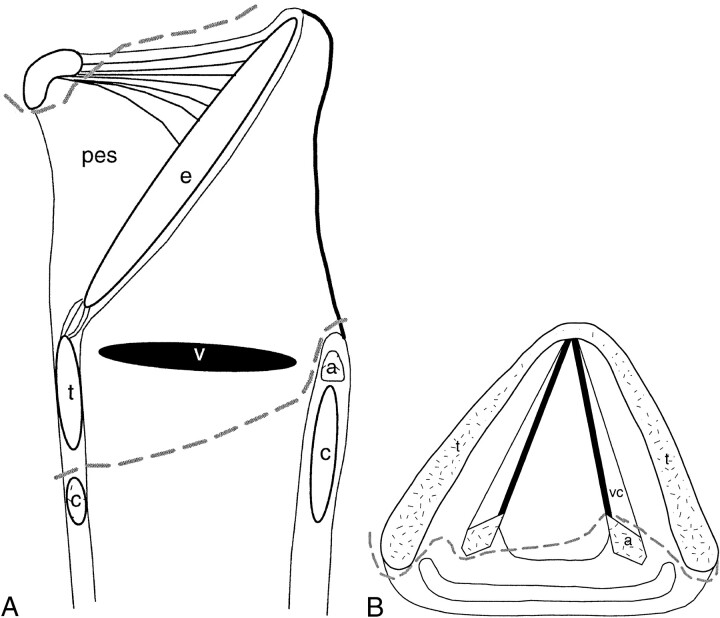
CHP is suitable for advanced supraglottic carcinoma involving the glottis, ventricle, or anterior commissure (3, 7, 8). It involves removing the whole thyroid cartilage, both the true and false cords, the ventricles, the epiglottis, and the paraglottic and preepiglottic spaces. At least one arytenoid must be spared to preserve phonation and sphincter functions (Fig 1). Reconstruction is accomplished by pulling together the hyoid bone and cricoid cartilage and then securing them together (Fig 2A).
fig. 1. A and B, Sagittal and axial drawings of structures resected during CHP (dashed lines). pes indicates preepiglottic space; e, epiglottis; a, arytenoid; c, cricoid cartilage; v, ventricle; t, thyroid cartilage; vc, vocal cords
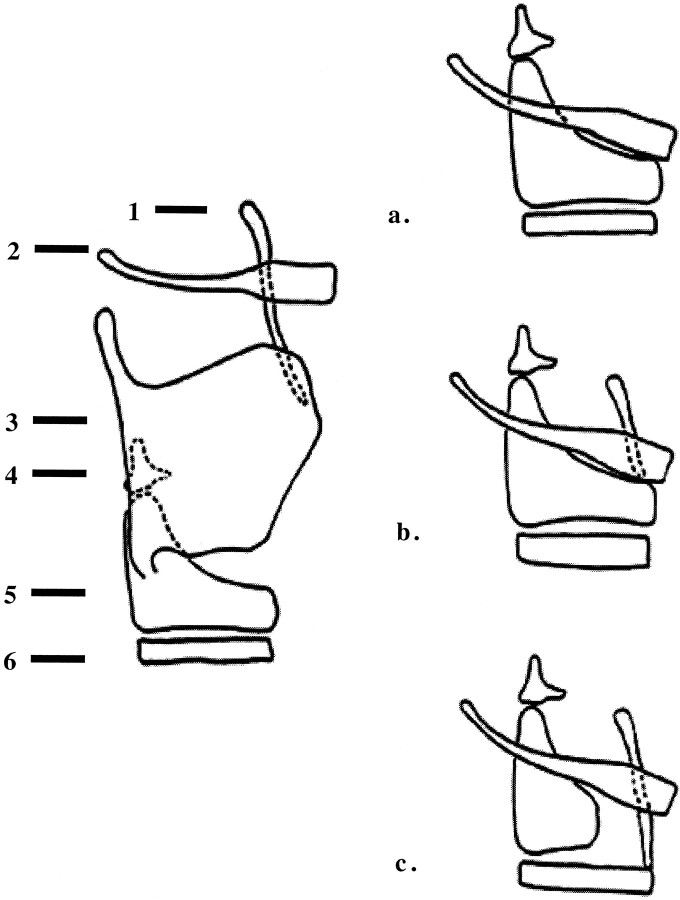
fig. 2. Types of reconstruction with SCPL. 1 indicates epiglottis; 2, hyoid bone; 3, thyroid cartilage; 4, arytenoid cartilage; 5, cricoid cartilage; 6, tracheal ring.
A, CHP.
B, CHEP.
C, TCHEP.
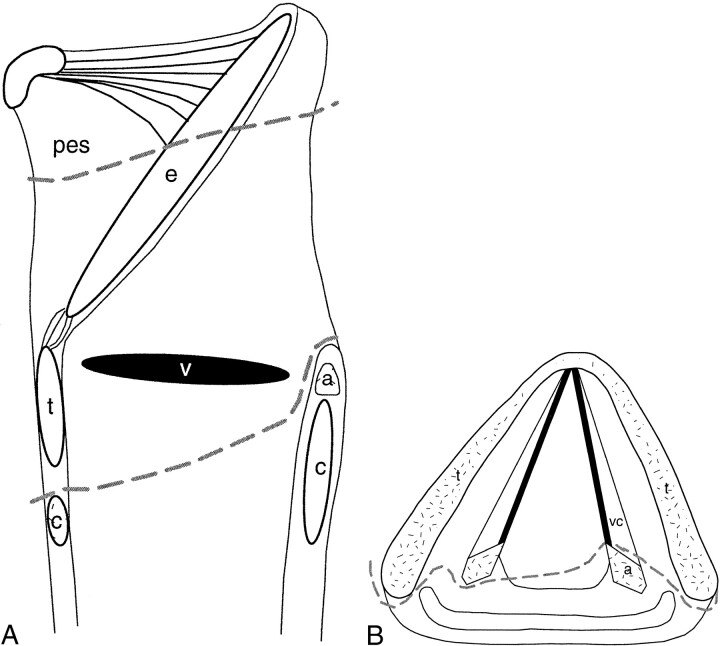
CHEP is used to treat cases of advanced glottic carcinoma that cannot be treated with endoscopic cordectomy (9, 13, 14) or with vertical partial laryngectomy (15). It involves resection of the infrahyoid part of the epiglottis and the preepiglottic space (Fig 3). Reconstruction consists of suturing the hyoid bone and the suprahyoid epiglottis closely together and to the cricoid cartilage (Fig 2B). As with CHP, one arytenoid is spared with CHEP.
fig. 3. A and B, Sagittal and axial drawings of structures resected during CHEP (dashed lines).
Note.—pes indicates preepiglottis space; e, epiglottis; a, arytenoid; c, cricoid cartilage; v, ventricle; t, thyroid cartilage; vc, vocal cords.
In TCHEP, the same structures are removed as in CHEP, with the main difference being the reconstruction. In TCHEP, reconstruction is performed by suturing the epiglottis to the first two tracheal rings, since the anterior arch of the cricoid cartilage is resected (Fig 2C). TCHEP is suitable for a few cases of glottic carcinoma that have limited anterior infraglottic extension and are not amenable to CHEP (10). The surgical technique must preserve the recurrent laryngeal nerve, which runs between the cricoid cartilage and the inferior horn of the thyroid cartilage, to allow the recovery of both phonation and sphincter functions. Therefore, the inferior horn of the thyroid is spared or simply resected to spare a portion of the perichondrium.
The base of the tongue is involved in the pexis in all types of SCPL; it is pulled back behind the hyoid bone and fixed to it. The oncologic contraindications of SCPL are arytenoid cartilage fixation, extension of the tumor below the glottis reaching the upper border of the cricoid cartilage (anterior subglottic extension greater than 10 mm, posterior subglottic extension greater than 5 mm), cricoid cartilage invasion, and extralaryngeal spread of tumor (7–9, 16). Massive invasion of the preepiglottic space is a contraindication for SCPL with CHEP, but it does not limit the use of SCPL with CHP, because the preepiglottic space is entirely resected in this procedure.
Recent reports have illustrated the usefulness of CT scans in the depiction of the irradiated larynx (17, 18). Some authors (2, 3, 19) have discussed the oncologic and functional results after SCPL. However, we found few reports of radiologic data about the postoperative CT appearance of the larynx (16, 20–23). To our knowledge, only one study (22) documented the CT evaluation of the larynx after SCPL; the study also included horizontal supraglottic laryngectomy and vertical laryngectomy. Therefore, we focused on the postoperative CT appearance of the larynx after SCPL.
Methods
Patients
Eighteen patients (17 men, one woman; age range, 48–71 y; mean age, 56 y) were included in this prospective study, and all had a well-differentiated invasive endolaryngeal squamous cell carcinoma that was managed with SCPL. At the time of SCPL, 10 patients had reconstruction with CHEP; seven patients, with CHP; and one patient, with TCHEP. Total resection of the arytenoid cartilage ipsilateral to the tumor was performed for six patients, and partial resection was performed for three patients. One patient underwent postoperative radiation therapy to the larynx (45 Gy). The initial tumor staging was performed according to the 1987 American Joint Comittee on Cancer classification system (T1, n = 1; T2, n = 7; T3, n =10) without the need for a permanent tracheostomy. Findings from clinical examination performed with nasal fibroscopy prior to CT imaging ruled out local superficial recurrence. The mean period between the surgical procedure and CT imaging was 37 mo (range, 23–62 mo).
Imaging Technique
Postoperative laryngeal CT was performed with a nonspiral conventional scanner (Elite Plus; Elscint, Israel) with the following technical parameters: 120 kV, 315 mAs, 2.1-s scanning time. Scans were obtained from the base of the tongue to the tracheal cartilage by using 2.5-mm-thick contiguous sections. The gantry angle was parallel to the C5–C6 intervertebral space corresponding to the theoretical plane of the true vocal cords. The patient lay supine with neck hyperextended and was asked to breath quietly and avoid swallowing. In a few cases, sections were repeated by using phonation and a modified Valsalva maneuver. The CT appearance of the anatomic postoperative changes was then analyzed. The distance between the hyoid bone and the inferior border of the cricoid cartilage at the cricotracheal junction, which was used to detect a release of the pexis, was measured.
To appreciate the height of the pexis, we determined the distance separating the section passing through the hyoid bone and the cricoid cartilage. We measured the distance between these two structures while taking into account the section passing the lower margin of the hyoid bone and the lower border of the cricoid cartilage.
Results
Analysis of the postoperative CT appearance revealed that three reference sections were useful for analyzing the main postsurgical reconstructions, regardless of the type of reconstruction (CHEP or CHP). The sections were an upper section passing through the body of the hyoid bone, a lower section including the cricoid cartilage, and a middle section between the two. For all patients, the average distance between the lower edge of the hyoid bone and the lower edge of the cricoid cartilage was 11 mm (range, 2–30 mm).
CHEP Group
The upper section showed the two valleculae immediately behind the hyoid bone outlining the remaining upper part of the epiglottis. The epiglottis was clearly visualized in a median position in seven of the 10 cases involving CHEP (Fig 4A). It was not possible to clearly identify the epiglottis in two cases, and they could not be distinguished from a CHP on a single view. The epiglottis was visualized in one case, but it appeared eccentric and slightly rotated. The arytenoids could be identified posteriorly. The upper section was through the apex or base of the arytenoid in all 10 cases. Its visibility depended on the degree of shortening of the neolarynx during pexis.
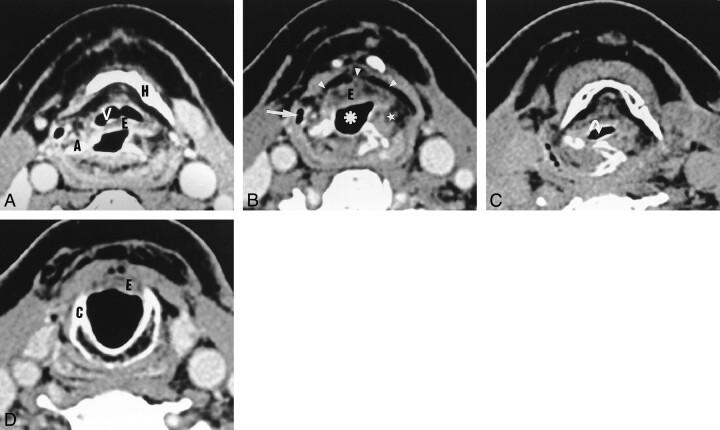
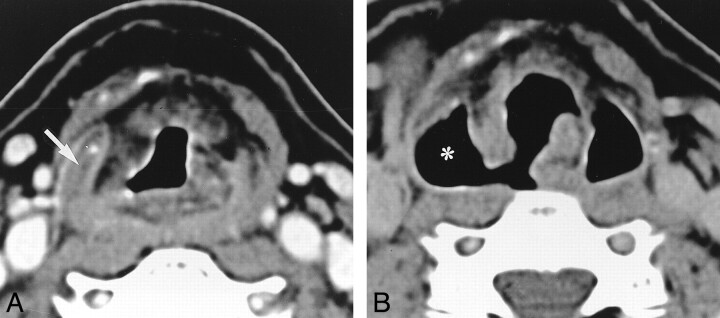
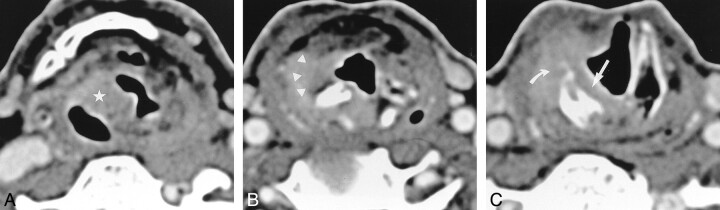
fig. 4. Axial CT scans obtained after SCPL with CHEP.
A, The vallecula (V) and epiglottis (E) are depicted at the level of the hyoid bone (H).
B, Below the level of the hyoid bone, the neovestibule (asterisk) is limited anteriorly by the epiglottis (E) and laterally by the NAFs (star). The lateral recess of the hypopharynx (arrow) and the preepiglottic space (arrowheads) are depicted.
C, During phonation, the neoglottis is oval and transversally oriented (arrow).
D, At the level of the cricoid cartilage (C), the subglottic lumen is empty and outlined by a thin mucosa. The inferior border of the epiglottis (E) cannot be distinguished.
The middle section below the hyoid bone showed the lumen of the neolarynx, which was thin. Immediately deep to the mucosa, fat density was demonstrated anteriorly and posteriorly (Fig 4B).
The remaining upper part of the neoaryepiglottic fold (NAF) could be seen on either side of the epiglottis. The NAF looked relatively thick, slightly heterogeneous, and rather hypoattenuating, without any significant enhancement (Figs 4B and 5B).
This hypertrophic appearance was well documented with sections by using the Valsalva maneuver (Fig 6). The visibility of the NAF depended on the degree of shortening of the neolarynx. It was best identified on successive sections if the impaction was long. Thus, the neovestibule was situated between the remaining epiglottis anteriorly and the NAF on either side (Fig 4B). The NAF is the medial limit of the lateral recess of the hypopharynx. The piriform sinus was better visualized on the sections for which the Valsalva maneuver was used.
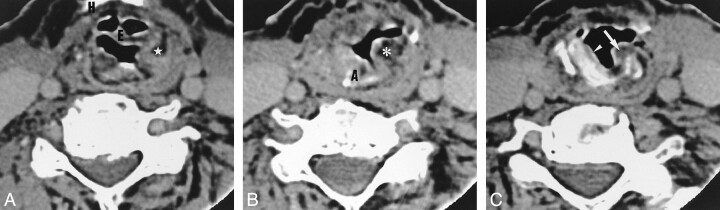
fig. 6. Axial CT scans obtained after SCPL with CHEP below the level of the hyoid.
A, The lateral recess of the hypopharynx is virtual (arrow).
B, During the Valsalva maneuver, the recess unfolds completely. Its medial limit is the neoaryepiglottic fold, which is thickened and slightly heterogeneous.
The section passing through the cricoid cartilage showed a well-centered cartilage on the midline. The upper part of the epiglottis merged with the soft tissue of the anterior cricoid region. The lumen of the cricoid was free, and the mucosa covering its inner surface was invisible or very thin (Fig 4D).
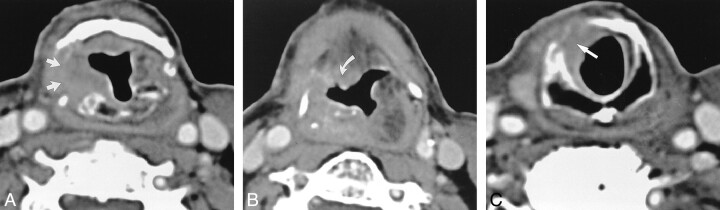
Three of the patients who underwent CHEP also underwent resection of the arytenoid. The arytenoid was replaced by a thickening of the soft tissue, forming a neoarytenoid. This neoarytenoid was made partly from the mucosa originally lining the posterior surface of the resected arytenoid. The neoarytenoid appeared continuous with the new NAF. The hypertrophic mucosa of the neoarytenoid may overflow into the cricoid cartilage lumen (Fig 5C). It was not possible to distinguish the patients who had not undergone arytenoid resection from those who had undergone partial arytenoid removal, which generally involves the anterior segment of the cartilage.
fig. 5. Axial CT scans obtained after SCPL with CHEP.
A, Hyoid bone (H), epiglottis (E), and neoaryepiglottic fold (star).
B, Slightly lower image shows that the left arytenoid has been resected and replaced by an exessive soft tissue (star). The right arytenoid (A) is depicted.
C, At the level of the cricoid cartilage, the excessive soft tissue is visible in the subglottic lumen (arrow). A slightly thickened aspect of the mucosa covering the cricoid cartilage is depicted (arrowhead).
During phonation, the arytenoids were in adduction. Thus, the lumen of the neoglottis lay in a transverse plane and was reduced compared with those depicted on sections obtained during quiet breathing. The neoglottis was defined by the merging of the arytenoids, the NAF, and the epiglottis (Fig 4C). The lower horns of the thyroid cartilage were seen at the level of the cricoid cartilage in six of 10 cases.
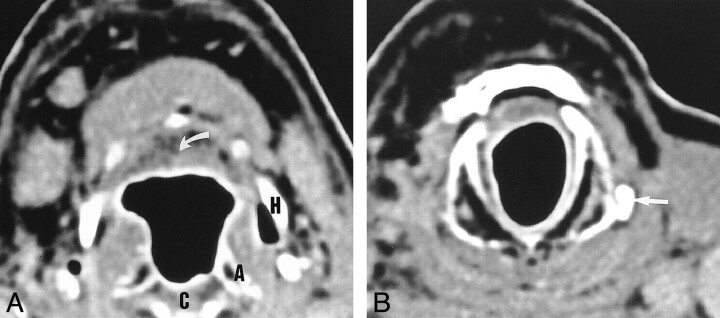
CHP Group
The postsurgical CT scans of patients who underwent CHP differed little from those of patients who underwent CHEP. The upper section was essential, because it could be used to distinguish between the two procedures. Because the resection of the epiglottis also involved the valleculae, soft tissue was present immediately behind the hyoid bone (Fig 7), which corresponded to the base of the tongue fixed to the hyoid bone. The other two reference sections were essentially superimposable on CHEP reconstructions. The NAFs were seen on fewer sections, because they were shorter than the NAFs in reconstructons with CHEP. By definition, a preepiglottic space no longer was present. The neoarytenoid was clearly seen in the three patients whose arytenoid had been resected. The lower horns of the thyroid cartilage were completely or partially visible in six of seven cases (Fig 7B).
fig. 7. Axial CT scans obtained after SCPL with CHP.
A, Soft tissue (arrow) corresponding to the base of the tongue is depicted behind the hyoid bone (H) instead of the epiglottis and valleculae. The pexis projects the arytenoids (A), upper border of the cricoid cartilage (C), and hyoid bone (H) to the same level.
B, At the level of the cricoid cartilage, the mucosa is thin and regular. The left inferior horn of the thyroid cartilage has been spared (arrow). The right horn is not visible.
TCHEP Group
We examined only one patient who underwent TCHEP. This patient differed from those in the CHEP group only because of the resected appearence of the anterior segment of the cricoid cartilage (Fig 8).
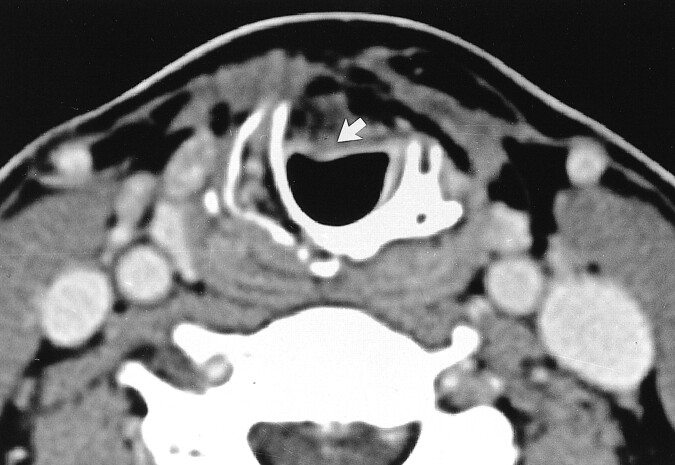
fig. 8. Axial CT scan obtained after SCPL with TCHEP. The anterior arch of the cricoid cartilage has been resected. Therefore, the remaining epiglottis (arrow) is anchored to the first two tracheal rings
Discussion
Although all sections must be carefully analyzed, especially when tumor recurrence is suspected, we believe that three key sections are useful for identifying the type of surgery performed for all the procedures investigated. The upper section passing through the hyoid bone provides important information about both the type of reconstruction (CHEP, CHP) and the quality of the pexis. The visibility of the epiglottis outlined by the valleculae can be used to unambiguously identify CHEP and CHP reconstructions. However, these procedures are difficult to distinguish if the epiglottis is not seen.
We could not clearly visualize the epiglottis in three of 10 of our patients who underwent CHEP. Two reasons for this inability are possible. First, the length of the residual epiglottis can vary depending on the surgical resection. Second, the epiglottis and the valleculae can collapse on the base of the tongue during surgical reconstruction and thus become indistinguishable from it. Unlike Maroldi et al (22), we never clearly visualized the epiglottis within the lumen of the cricoid cartilage in our patients, even when the larynx had been particularly shortened. The lower part of the suprahyoid epiglottis sutured to the anterior arch of the cricoid is normally indistinguishable from the anterior cervical soft tissue. In CHP, a thickening (several millimeters) of retrohyoid soft tissue was always present; this corresponded to scarring of the posterior part of the tongue sutured to the hyoid bone.
Another important piece of information provided by the upper section pertains to the quality of the pexis. Measuring the distance between the hyoid bone and the cricoid cartilage is not always useful, because the arytenoid could be seen at the level of the hyoid bone in 13 of 18 cases. The shortening of the neolarynx occasionally was present such that the hyoid bone and the cricoid cartilage could be seen on a single section (Fig 7B). The middle section was mainly focused on the appearance of the neovestibule made anteriorly from the epiglottis (CHEP) or the base of the tongue (CHP) and laterally from the NAF. The NAFs were relatively thick and hypoattenuating, slightly heterogeneous, and displayed on several sections in the patients who underwent CHEP. They were less extensive in those who underwent CHP.
The active participation of the NAFs in phonation to maximally reduce the lumen of the neolarynx may explain their pseudohypertrophic appearance. The NAF is the medial limit of the piriform sinus, which was frequently collapsed in our patients and thus better analyzed with the Valsalva maneuver. The lumen of the piriform sinus did not appear to be dilated in our patients; this finding is in contrast to the findings of Maroldi et al (22), probably because of our technical procedure during surgery. Tension is applied to the pharyngeal constrictors to prevent the dilatation of the piriform sinuses. The presence of excessive soft tissue made up of the remaining arytenoid mucosa allows the confirmation of arytenoid resection. The neoarytenoid had the same density as that of the NAFs. The partial resection of the anterior part of the arytenoid could not be seen. The preepiglottic space was always visible in patients who underwent CHEP. Patients who underwent CHEP could be distinguished from those who underwent CHP, because the upper portion of the preepiglottic space was present in only those who underwent CHEP.
The section passing through the middle of the cricoid cartilage was the simplest to analyze. The cricoid mucosa was invisible or slightly thickened, generally symmetrically. The lower horns of the thyroid were usually visible (in 13 of 18 patients) outside the cricoid cartilage.
The inferior laryngeal nerve, which reaches the larynx via the cricoarytenoid joint, must be preserved during surgery to ensure phonation. Thus, the lower horns of the thyroid cartilage are preserved during surgery (8, 9, 22). However, they cannot be visualized if the larynx has been resected by sparing a portion of perichondrium.
The availability of data from postoperative scans is essential for differentiating between the simple postsurgical appearance and the possible recurrence of a tumor. One might carefully examine all the sections to detect an abnormal soft-tissue mass. Patients who undergo surgery are usually monitored with indirect laryngoscopy and monitoring for symptoms such as dyspnea or changes in voice quality.
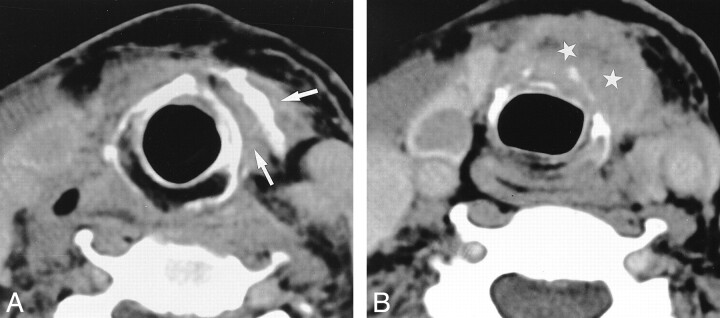
The most common type of tumor recurrence in SCPL involves a special submucosal extension, particularly in the cricoid or cricoarytenoid regions (11, 12). This type of recurrence can be confirmed only with endoscopy and deep biopsy. Hence, the CT scan is most important for detecting submucosal lesions indicated by abnormal thickening. A recurrent tumor in the cricoid region may spread along the lateral wall of the neovestibule via the NAF to the epiglottis (Fig 9) or to the base of the tongue (Fig 10). Because no more anatomic barriers exist, a reccurent tumor generally spreads as a submucosal pathway; however, it can also involve deep tissue, including residual paraglottic space, cartilages, and strap muscles (Fig 11).
fig. 9. Axial CT scans of recurrrent disease in a patient who underwent SCPL with CHEP 2 y before.
A, Image depicts strong enhancement (star) of the right NAF compared with that of the left. This finding is very suggestive of recurrence.
B, The enhancement follows the lateral wall of the neovestibule (arrowheads). C, The enhancement proceeds down to the cricoid cartilage mucosa, which is thicker than usual (straight arrow), with the extralaryngeal spread of tumor (curved arrow).
fig. 10. Axial CT scans of recurrence 3 y after SCPL with CHP.
A, Enhancement of the right lateral wall of the neovestibule (arrows).
B, Enhancement spreading downward to the submucosa of the cricoid cartilage (arrow). C, Enhancement extending upward to the right side of the base of the tongue (arrow).
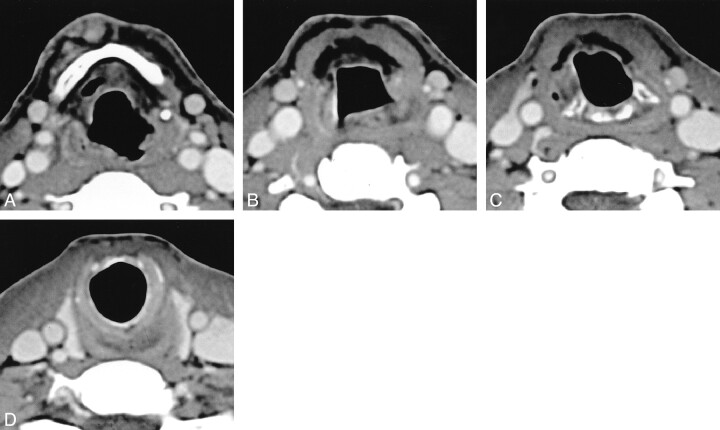
fig. 11. Axial CT scans in a patient who underwent SCPL with CHEP 5 y before. At nasofibroscopy, the patient had an anterior cervical cutaneous fistula with an arytenoid that was only slightly thickened.
A, Massive extralaryngeal recurrence around the cricohyoidopexy (arrows).
B, Recurrence spreading downward to the pretracheal tissue (stars).
CT also will be useful for depicting early complications, such as detachment of the pexis (ie, separation of the hyoid bone and the cricoid cartilage). The average distance between the lower borders of the hyoid bone and the cricoid cartilage was 11 mm (range, 3–30 mm) in our patients. This distance reflected the shortening of the neolarynx during surgical reconstruction that is essential for proper swallowing. The shortening of the neolarynx was evident from the first section involving the hyoid bone in two of three cases, when the arytenoid was visible. We believe that, when the distance between the lower borders of the hyoid bone and the cricoid cartilage is greater than 30 mm in a patient having difficulty swallowing, it should be considered as a failure of the pexis (Fig 12).
fig. 12. Axial CT scans obtained 6 mo after SCPL with CHEP in a patient with severe swallowing disorders. The distance between the lower limit of the hyoid bone (in A) and the lower limit of the cricoid cartilage (in D) is more than 3.5 cm. This finding implies failure of the pexis, which was confirmed at surgery
In conclusion, the simple analysis of three CT sections is enough to differentiate between CHP and CHEP reconstructions. However, all sections must be carefully analyzed to detect tumor recurrence, which usually is submucosal and difficult to detect with clinical endoscopy.
Footnotes
Address reprint requests to N. Bely-Toueg, MD, Department of Radiology, Hospital Laennec, University of Paris V 42, rue de Sevres, 75340 Paris Cedex 07, France.
References
- 1.De Vincentis M, Minni A, Gallo A. Supracricoid laryngectomy with cricohyoidopexy (CHP) in the treatment of laryngeal cancer: a functional and oncologic experience. Laryngoscope 1996;106:1108-1114 [DOI] [PubMed] [Google Scholar]
- 2.Chevalier D, Laccourreye O, Brasnu D, Laccourreye H, Piquet JJ. Cricohyoidoepiglottopexy for glottic carcinoma with fixation or impaired motion of the true vocal cord—5-year oncological results with 112 patients: a combined study. Ann Otol Rhinol Laryngol 1997;106:364-369 [DOI] [PubMed] [Google Scholar]
- 3.Chevalier D, Piquet JJ. Subtotal laryngectomy with cricohyoidopexy for supraglottic carcinoma: review of 61 cases. Am J Surg 1994;168:472-473 [DOI] [PubMed] [Google Scholar]
- 4.Labayle J, Bismuth R. Laryngectomie totale avec reconstruction. Ann Otolaryngol Chir Cervicofac 1971;88:219-228 [PubMed] [Google Scholar]
- 5.Majer HRA. Technique de laryngectomie permettant de conserver la perméabillité respiratoire: la crico-hyoïdopexie. Ann Otolaryngol Chir Cervicofac 1959;76:677-683 [Google Scholar]
- 6.Piquet J, Desaulty A, Decroix G. Crico-hyoïdo-pexie: technique opératoire et résultats fonctionnels. Ann Otolaryngol Chir Cervicofac 1974;91:421-426 [PubMed] [Google Scholar]
- 7.Laccourreye O, Brasnu D, Merite-Drancy A, et al. Cricohyoidopexy in selected infrahyoid epiglottic carcinomas presenting with pathological preepiglottic space invasion. Arch Otolaryngol Head Neck Surg 1993;119:881-886 [DOI] [PubMed] [Google Scholar]
- 8.Laccourreye H, Laccourreye O, Weinstein G, Menard M, Brasnu D. Supracricoid laryngectomy with cricohyoidopexy: a partial laryngeal procedure for selected supraglottic and transglottic carcinomas. Laryngoscope 1990;100:735-741 [DOI] [PubMed] [Google Scholar]
- 9.Laccourreye H, Laccourreye O, Weinstein G, Menard M, Brasnu D. Supracricoid laryngectomy with cricohyoidoepiglottopexy: a partial laryngeal procedure for glottic carcinoma. Ann Otol Rhinol Laryngol 1990;99:421-426 [DOI] [PubMed] [Google Scholar]
- 10.Laccourreye O, Ross J, Brasnu D, Charbades E, Kelly J, Laccourreye H. Extended supracricoid partial laryngectomy with tracheocricohyoidoepiglottopexy. Acta Otolaryngol 1994;114:669-674 [DOI] [PubMed] [Google Scholar]
- 11.Laccourreye O, Laccourreye L, Muscatello L, Périé S, Weinstein G, Brasnu D. Local failure after supracricoid partial laryngectomy: symptoms, management, and outcome. Laryngoscope 1998;108:339-344 [DOI] [PubMed] [Google Scholar]
- 12.Glazer HS, Niemeyer JH, Balfe DM, et al. Neck neoplasms: MR imaging: Part II, posttreatment evaluation. Radiology 1986;160:349-354 [DOI] [PubMed] [Google Scholar]
- 13.Steiner W, Ambroch P. CO2 laser microsurgery for laryngeal cancer. In: Smee R, Bridger GP, eds. Proceedings of the Second World Congress on Laryngeal Cancer. Amsterdam, the Netherlands: Elsevier; 1994; 369–372
- 14.Peretti G, Capiello J, Nicolai P, Smussi C, Antonelli AR. Endoscopic laser excisional biopsy for selected glottic carcinomas. Laryngoscope 1994;104:1276-1279 [DOI] [PubMed] [Google Scholar]
- 15.Mohr RM, Quenelle DJ, Shumrick DA. Certical fronto-lateral laryngectomy (hemilaryngectomy). Arch Otolaryngol Head Neck Surg 1983;109:384-395 [DOI] [PubMed] [Google Scholar]
- 16.Curtin H. Imaging of the larynx: current concepts. Radiology 1989;173:1-11 [DOI] [PubMed] [Google Scholar]
- 17.Mukherji S, Mancuso A, Kotzur I, et al. Radiologic appearance of the irradiated larynx, part I. Radiology 1994;193:141-148 [DOI] [PubMed] [Google Scholar]
- 18.Mukherji S, Mancuso A, Kotzur I, et al. Radiologic appearance of the irradiated larynx, part II. Radiology 1994;193:149-154 [DOI] [PubMed] [Google Scholar]
- 19.Laccourreye O, Crevier-Buchmann L, Weinstein G, Biacabe B, Laccourreye H, Brasnu D. Duration and frequency characteristics of speech and voice following supracricoid partial laryngectomy. Ann Otol Rhinol Laryngol 1995;104:516-521 [DOI] [PubMed] [Google Scholar]
- 20.Disantis D, Balfe D, Hayden R, Sessions D, Sagel S. The neck after vertical hemilaryngectomy: computed tomography study. Radiology 1984;151:683-687 [DOI] [PubMed] [Google Scholar]
- 21.Disantis DJ, Balfe DM, Hayden RE, Sagel SS, Sessions D, Lee JKT. The neck after total laryngectomy: CT study. Radiology 1984;153:713-717 [DOI] [PubMed] [Google Scholar]
- 22.Maroldi R, Battaglia G, Nicolai P, et al. CT appearance of the larynx after conservative and radical surgery for carcinomas. Eur Radiol 1997;7:418-431 [DOI] [PubMed] [Google Scholar]
- 23.Weinstein G, Laccourreye O, Brasnu D, Youssem D. The role of computed tomography and magnetic resonance imaging in planning for conservation laryngeal surgery. Neuroimaging Clin North Am 1996;6:497-504 [PubMed] [Google Scholar]