Abstract
Summary: We report a case of a spinal epidermoid cyst in which diffusion-weighted imaging with a navigator-echo technique was useful for the differential diagnosis from other cystic tumors. Motion artifacts are inherent on diffusion-weighted images of the spinal region; however, the navigator-echo technique compensated for this problem and provided high-quality images. Diffusion-weighted imaging with navigator echoes is considered to be a potentially useful tool in the differential diagnosis of spinal cystic tumors.
Spinal epidermoid cysts are relatively rare. They comprise between 0.5% and 1.0% of all spinal tumors (1–6). Because the signal intensity of an epidermoid cyst is similar to that of CSF on MR images (2–5, 7, 8), epidermoid cysts are often misdiagnosed as another type of cystic tumor.
Diffusion-weighted imaging has been reported to be a helpful technique for diagnosing intracranial epidermoid cysts (9, 10); however, to our knowledge, diffusion-weighted imaging of a spinal epidermoid cyst has never been reported. Clinically, diffusion-weighted imaging of the thoracic spinal region is difficult because of inherent motion artifact, but the navigator-echo technique can overcome this problem. We report the utility of diffusion-weighted imaging with navigator echoes in distinguishing a spinal epidermoid cyst from other types of cystic tumors.
Case History
A 44-year-old man suffered from right leg numbness for 15 years. Gait disturbance gradually progressed during the most recent half year. The patient was examined with MR imaging of the thoracic spine. A thoracic spinal tumor was found on T2- and T1-weighted images. The patient was admitted to our hospital to undergo surgical treatment.
A neurologic examination revealed increased patellar-tendon reflex and pathologic plantar reflexes. The results of a plain radiographic examination of the thoracic spine were normal.
MR imaging of the thoracic spine, which was performed at our hospital, depicted a tumor with high and slightly inhomogeneous intensity on T2-weighted images (Fig 1A) and with low signal intensity on T1-weighted images (Fig 1B) at the T5–T9 level. After the IV administration of contrast material, the mass showed no contrast enhancement (Fig 1C). Diffusion-weighted imaging was performed to characterize the mass better.
fig 1.
MR images of spinal epidermoid cyst (arrow).
A, Slightly inhomogeneous high signal intensity mass on T2-weighted image (2888/110/3) at the T5–T9 level.
B, Low signal intensity mass on T1-weighted image (350/12/3).
C, No contrast enhancement is seen on T1-weighted image obtained after the IV administration of contrast material.
Spin-echo diffusion-weighted imaging with a navigator-echo technique, which corrects for the phase error on each line of k space from inherent motion (11–13), was performed. The navigated diffusion-weighted imaging sequence used a pair of diffusion-sensitizing gradients centered at the first 180° pulse of a double-echo imaging sequence; the first echo was acquired with non–phase encoding echo (navigator echo), and the second echo was acquired with phase-encoding echo. The interval between navigator echo and imaging echo was 13 ms, and the phase error due to this interval, was negligible compared with the effect of the diffusion gradients. To avoid the effects of CSF pulsation, the sequence was RR-gated by using a finger-pulse oximeter. The imaging parameters were as follows: 1714/84–97/1 (TR/TE/excitations); field of view, 30 × 30 cm; section thickness, 6 mm; and matrix, 256 × 128. The diffusion gradient was applied along the phase-encoding axes with gradient b-values of 0, 250, and 1000 s/mm2, respectively. The total examination time was 11 minutes for acquisition of three different b-value images. Apparent diffusion coefficient images were calculated from these diffusion-weighted images. All imaging was performed using a 1.5-T MR imager.
On the diffusion-weighted images of higher b-value, intensity of the mass remained high (Fig 2C). On the apparent diffusion coefficient images, signal intensity of the spinal mass was similar to that of the spinal cord (Fig 2D and E). These diffusion-weighted imaging findings are compatible with a solid nature (non-fluid), and we made a preoperative diagnosis of spinal epidermoid cyst.
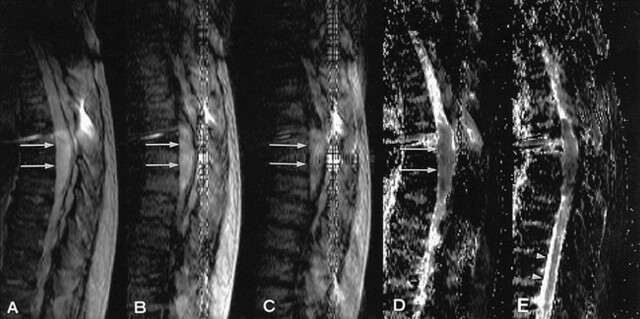
fig 2.
A–C, Diffusion-weighted images with a gradient b-values of 0 (A), 250 (B), and 1000 s/mm2 (C). On the diffusion-weighted image of higher b-value, tumor intensity remains high (arrow). The vertical artifact likely appeared because of pulsatile motion of superior sagittal sinus.
G–E, Calculated apparent diffusion coefficient maps. Apparent diffusion coefficient values of epidermoid cyst is 1.3 × 10−3 mm2/s (G) (arrow) and 1.6 × 10−3 mm2/s (arrowhead). The solid nature of the spinal epidermoid cyst is represented.
At surgery, a laminectomy from the T6 to T9 levels was performed. The tumor was intradural extramedullary in location. When the dura incision was made, the spinal cord was protruded posteriorly because of tumor compression. The tumor was covered with a capsule of “pearly” appearance and was filled with keratin. Subtotal removal and tumor decompression were performed. A pathologic examination confirmed the diagnosis of epidermoid cyst.
After surgery, gait disturbance remained. The patient gradually recovered during rehabilitation, as was revealed at the 4-month follow-up examination.
Discussion
Intraspinal epidermoid cysts can be congenital or acquired (1–5). Congenital epidermoids often have associated epidermal defects, such as spina bifida and hemivertebrae, whereas acquired lesions lack osseous abnormalities. Approximately 40% of intraspinal epidermoid cysts are acquired and are considered to be a late complication of lumbar puncture. Our patient did not have a history of a lumbar puncture, and no associated congenital bone anomalies or other central nervous system anomalies were evident. Therefore, we presumed our patient's epidermoid cyst was congenital in origin.
Although the signal intensity of epidermoid cysts varies, it is typically iso- or slightly hyperintense compared with that of CSF on all sequences and shows no contrast enhancement. These findings mimic those of cysts with fluid content. In the case reported herein, the signal intensity of the T1- and T2-weighted images was similar to that of CSF. There was slightly inhomogeneous signal intensity on the T2-weighted images. No contrast enhancement was seen, and the tumor location was indistinct with regard to whether it was intradural or extradural. From the slightly inhomogeneous signal intensity on the T2-weighted images, an epidermoid cyst was suspected; however, other cystic spinal tumors with fluid content could not be ruled out. Therefore, a diffusion-weighted imaging sequence was obtained to determine whether the pathologic abnormality was cystic or solid. On the diffusion-weighted images of higher b-value, the signal intensity of the mass was high and clearly more hyperintense than that of CSF. The apparent diffusion coefficient value was similar to that of spinal cord, which indicated the solid nature of the tumor. With these helpful findings on the diffusion-weighted images, we diagnosed an epidermoid cyst.
Many investigators have reported the utility of diffusion-weighted imaging for detecting intracranial disease, such as brain ischemia (11, 14), abscess (15), and epidermoid cyst (9, 10); however, diffusion-weighted imaging is rarely performed to investigate the spinal region because of the inherent motion sensitivity that causes artifact. One approach to eliminating motion artifact is diffusion-weighted imaging with single-shot echo-planar imaging; however, echo-planar imaging has a low signal-to-noise ratio and prominent susceptibility artifacts. For the thoracic spinal region, susceptibility distortions appear at the air-tissue interface, and motion artifacts from the heart and chest wall degrade the image quality. Based on these observations, we think single-shot echo-planar imaging is not a good technique for diffusion-weighted imaging of the thoracic spine. An alternative approach to eliminate the motion artifact is to measure and correct for the phase error on each line of k space, by recording a non–phase encoding echo (called a navigator echo). The navigator-echo technique allows diffusion-weighted imaging to be performed with a conventional spin-echo sequence, providing a high signal-to-noise ratio with fewer susceptibility artifacts (13, 14). Navigated diffusion-weighted imaging with spin-echo is an ideal solution to obtain high-quality diffusion-weighted images of the spinal region.
In conclusion, navigated diffusion-weighted imaging with spin-echo and calculated apparent diffusion coefficient images were helpful for reducing motion artifacts and for making a differential diagnosis of epidermoid cyst of the thoracic spine.
Footnotes
Address reprint requests to Keiichi Kikuchi, MD, Department of Radiology, Ehime University School of Medicine, Shitsukawa, Shigenobu-cho, Onsen-gun, Ehime 791-0295, Japan.
References
- 1.Donoghue V, Chuang SH, Chilton SJ, Fitz CR, Harwood-Nash DC. Intraspinal epidermoid cysts. J Comput Assist Tomogr 1984;8:143-144 [DOI] [PubMed] [Google Scholar]
- 2.Machida T, Abe O, Sasaki Y, et al. Acquired epidermoid tumour in the thoracic spinal canal. Neuroradiology 1993;35:316-318 [DOI] [PubMed] [Google Scholar]
- 3.Visciani A, Savoiardo M, Belastrini MR, Solero CL. Iatrogenic intraspinal epidermoid tumor: myelo-CT and MRI diagnosis. Neuroradiology 1989;31:273-275 [DOI] [PubMed] [Google Scholar]
- 4.Toro VE, Lacy C, Binet EF. MRI of iatrogenic spinal epidermoid tumor. J Comput Assist Tomogr 1993;17:970-972 [DOI] [PubMed] [Google Scholar]
- 5.Potgieter S, Dimin S, Lagae L, et al. Epidermoid tumours associated with lumbar punctures performed in early neonatal life. Dev Med Child Neurol 1998;40:266-269 [DOI] [PubMed] [Google Scholar]
- 6.Deogaonkar M, Goel A, Pandya SK. Thoracic intradural anterior epidermoid manifesting as sudden onset of paraplegia: case report. Neurol Med Chir 1995;35:678-679 [DOI] [PubMed] [Google Scholar]
- 7.Parizel PM, Baleriaux D, Rodesch G, et al. Gd-DTPA-enhanced MR imaging of spinal tumors. AJR Am J Roentgenol 1989;152:1087-1096 [DOI] [PubMed] [Google Scholar]
- 8.Steffey DJ, Filipp GJ, Spera T, Gabrielsen TO. MR imaging of primary epidermoid tumors. J Comput Assist Tomogr 1988;12:438-440 [DOI] [PubMed] [Google Scholar]
- 9.Tsuruda JS, Chew WM, Moseley ME, Norman D. Diffusion-weighted MR imaging of the brain: value of differentiating between extraaxial cysts and epidermoid tumors. AJR Am J Roentgenol 1990;155:1059-1065 [DOI] [PubMed] [Google Scholar]
- 10.Maeda M, Kawamura Y, Tamagawa Y, et al. Intravoxel incoherent motion (IVIM) MRI in intracranial, extraaxial tumors and cysts. J Comput Assist Tomogr 1992;16:514-518 [DOI] [PubMed] [Google Scholar]
- 11.Bammer R, Stollberger R, Augustin M, et al. Diffusion-weighted imaging with navigated interleaved echo-planar imaging and a conventional gradient system. Radiology 1999;211:799-806 [DOI] [PubMed] [Google Scholar]
- 12.Butts K, Pauly J, de-Crespigny A, Moseley M. Isotropic diffusion-weighted and spiral-navigated interleaved EPI for routine imaging of acute stroke. Magn Reson Med 1997;38:741-749 [DOI] [PubMed] [Google Scholar]
- 13.de-Crespigny AJ, Marks MP, Enzmann DR, Moseley ME. Navigated diffusion imaging of normal and ischemic human brain. Magn Reson Med 1995;33:720-728 [DOI] [PubMed] [Google Scholar]
- 14.Beauchamp NJ Jr, Barker PB, Wang PY, vanZijl PC. Imaging of acute cerebral ischemia. Radiology 1999;212:307-324 [DOI] [PubMed] [Google Scholar]
- 15.Ebisu T, Tanaka C, Umeda M, et al. Discrimination of brain abscess from necrotic or cystic tumors by diffusion-weighted echo planar imaging. Magn Reson Imaging 1996;14:1113-1116 [DOI] [PubMed] [Google Scholar]