Abstract
BACKGROUND AND PURPOSE: It is widely recognized that tumor hormone receptor status correlates with overall survival in metastatic breast carcinoma; however, the influence of hormone receptors on the pattern of disease spread is not well known.
PURPOSE: We set out to determine the common distributions of metastatic disease spread in metastatic breast carcinoma, and to evaluate tumor hormone receptor status as predictor of disease spread.
METHODS: Thirty-six patients being imaged for possible metastatic breast carcinoma between 1995 and 1998, in whom the presence or absence of tumor estrogen and progesterone receptors (ER+ or ER− / PR+ or PR−) was known, who underwent both contrast-enhanced MR of the brain and total body skeletal scintigraphy, were studied retrospectively.
RESULTS: Of twelve patients with skeletal metastases but no brain metastases, 83% were ER+/PR+. Ten patients had brain metastases but no skeletal involvement, 80% of which were ER−/PR−. Seven patients had no brain or osseous metastases, but had metastatic disease in the chest or abdomen. Eighty-six percent of patients in this group were ER−/PR−. The tumor receptor status was statistically different between these three distribution groups (P = .01). A final group, consisting of seven patients, showed widespread disease, with diffuse metastases to the brain, viscera, and skeleton. In this group, no patients were ER+/PR+.
CONCLUSION: There are two major patterns of disease spread in metastatic breast carcinoma, excluding patients with extensive diffuse metastases. Patients with ER+/PR+ tumors tend to develop osseous but not brain metastases. Patients with ER−/PR− tumors tend to develop brain but not osseous metastases. Appreciation of these distributions can aid the radiologist in detecting metastatic lesions, and will help the clinician to estimate the likelihood of metastases to various organ systems, as well as to potentially target therapy.
Carcinoma of the breast remains one of the leading cancers in women today, with an estimated lifetime risk of 13% (1). Despite many advances in diagnosis and screening, the disease is frequently discovered after spread to regional lymph nodes or even after dissemination of distant metastases. A large number of studies have correlated the presence or absence of tumor estrogen receptors (ER) or progesterone receptors (PR) with ultimate clinical outcomes (2–5). Little attention, however, has focused on the potential correlation between tumor receptor status and patterns of disease spread. We set out to determine the most common patterns of disease spread in metastatic breast carcinoma, and to evaluate tumor ER and PR status as a predictor of metastatic distribution.
Methods
Patient Population
Using a computerized radiology report search application, 100 women being imaged with both gadolinium-enhanced MR of the brain and total body skeletal scintigraphy for metastatic breast carcinoma between January 1995 and December 1998 were identified retrospectively. Pathologic data was also reviewed retrospectively from patients for whom primary tumor specimens were available at our institution.
Thirty-six patients had tumor samples evaluated for tumor hormone (estrogen and progesterone) receptor status at our institution. These 36 patients composed our study group.
Each patient was scored for the presence or absence of metastases to the skeleton, abdominal viscera, thorax, and brain as determined by interpretations of the radiologic studies. Suspicious findings were scored as positive for metastasis, and suspected benign findings were scored as negative for the purposes of this study. Findings of osseous metastases, as suggested by uptake on bone scintigraphy, were confirmed with conventional radiography or CT findings in all cases. Patients were divided into four distinct groups, as described in results, and a two-tailed Fisher's exact test was used to determine statistical significance of differences between groups.
Results
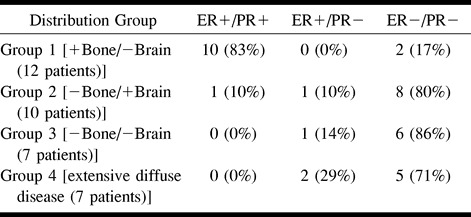
Thirty-six patients had pathologic specimens available for review at our institution, and had tumor samples evaluated for ER and PR status. Thirty-three patients had invasive ductal carcinoma, and three patients had invasive lobular carcinoma. All patients underwent contrast-enhanced MR imaging of the brain as well as total body skeletal scintigraphy. Most patients also underwent CT or MR imaging of the abdomen (75%), and CT or radiography of the chest (98%). Metastatic distributions fell into four distinct groups, as shown in the Table.
The first patient group, consisting of 12 women with a mean age of 60.4 years, had numerous osseous metastases, but no brain metastases. As shown in the Table, 10 of these patients (83%) were ER+ / PR+, and two patients (17%) were ER− / PR −.
The second group, consisting of 10 patients with a mean age of 57.4 years, had no osseous metastases, but showed numerous brain metastases. As shown in the Table, the vast majority of patients (80%) in this group were ER− / PR−.
The third group, which contained seven patients with a mean age of 58.8 years, had no osseous or brain metastases, but had scattered metastases to the chest or abdomen or both. As shown in the Table, the majority of patients (86%) with this distribution of metastatic spread were ER− / PR−.
A final group, consisting of seven patients with a mean age of 55.6 years, had diffuse osseous metastases as well as multiple brain metastases, in addition to “many” or “diffuse” metastases to virtually all organ systems imaged. No patients in this group were ER+ / PR+, as shown in the Table.
Fisher's exact test revealed a statistically significant difference between these groups (P =. 01). Similarly, there was a statistically significant difference between the occurrence of these various metastases between patients with and those without ER+ tumors. Specifically, patients with ER+ tumors were more likely to experience bone metastases, whereas patients with ER− tumors were more likely to have brain metastases (P =. 01).
Discussion
Given the overall prevalence of breast carcinoma today and the poor long-term prognosis afforded by metastatic disease of any cell type, a substantial portion of research today has appropriately focused on methods of early diagnosis and prevention of metastatic disease. Metastatic breast carcinoma, however, is unique compared with many other tumors in that its course and prognosis can be highly variable, owing in large part to a variety of poorly understood factors.
The development of histologic assays for ER and PR led to a great deal of interest in these receptors as possible prognostic factors in the disease. A number of small- and large-scale studies over the past 15 years have addressed this very issue, each reporting similar results. Specifically, ER+ / PR+ tumors have been repeatedly shown to be correlated with a more favorable long-term prognosis than tumors that do not express these receptors (2–5). It has been suggested by some that the improved prognosis in receptor-positive tumors is afforded by the response to endocrine (tamoxifen) treatment that these patients commonly receive (5). A much larger study, however, recently evaluated 2257 women, none of whom received any adjuvant therapy, and confirmed the prognostic value of tumor hormone receptors, independent of hormone therapy (2).
Despite all the emphasis that has been placed upon the long-term prognostic value of tumor receptor status, little emphasis has been placed on the predictive value of receptor data with respect to patterns of disease spread. In 1984, a review of 25 patients at Johns Hopkins Hospital correlated the tumor receptor status with visceral metastases found at autopsy (6). The study found that ER+ tumors metastasized more frequently to the thyroid and parathyroid glands, and that ER− tumors spread more extensively to the leptomeninges. In addition, PR+ tumors spread more frequently to the myocardium and small bowel. They did not report on prevalence of metastases to the skeleton or brain parenchyma. In 1985, a study published by the Helsinki University Central Hospital followed 397 patients to evaluate prognostic value of tumor receptor status for prediction of disease-free interval and site of first metastasis (5). Their results, scored simply as soft tissue, bone, or simply “visceral” as site of the first metastasis, showed that ER+ tumors were associated with approximately twice the rate of osseous spread as site of first metastases as compared with ER− tumors. Finally, a more recent report from the University Hospital Nijmegen of the Netherlands described a correlation between the site of first metastasis and the tumor hormone receptor data, which was available from 188 patients (7). The data showed that patients with ER+ tumors developed bone metastases, as the site of first metastasis, three times more often than did patients with ER− tumors. Similarly, PR+ tumors were associated with a twofold increased risk of osseous spread. As for visceral disease spread, no prognostic value could be given to either ER or PR status. Combined ER− / PR− status was associated with a much higher occurrence of CNS metastases, although this was not statistically significant because of the low number of patients in whom the CNS was a site of first metastasis.
Although the above studies address the site of first metastasis, and not the overall distribution of metastases as we studied, our data confirms what one might expect from extrapolation of the data from these studies. Specifically, we found that ER+ / PR+ tumors were strongly associated with the presence of osseous metastases, and frequently associated with extensive osseous disease spread. Tumors in this group involved the thoracoabdominal viscera commonly, but very rarely involved the CNS. Conversely, tumors that were ER− / PR− were highly associated with brain and visceral metastases, and were only rarely associated with osseous metastases. These differences were statistically significant, despite a small patient population.
One might ask how the other two distribution groups fit into the overall picture. The group that showed extensive diffuse metastases to the bones, chest, abdomen, and brain likely represents those patients with very aggressive tumors and far-advanced disease. In these tumors, the prognostic value of receptor status is probably small because other features that convey their very aggressive nature, such as tumor cell dedifferentiation, probably outweigh the ER− / PR− correlation. The patients who developed metastases to the thoracoabdominal viscera, without metastases to the brain or bones, were almost all ER− / PR−, and this finding likely represented a very early tumor stage for the patients of the group who developed CNS metastases.
It has been previously suggested that differences in prognosis may be influenced by endocrine therapy (5), and it could be argued that we did not stratify our population by presence or absence of tamoxifen therapy. A substantial portion of patients with ER+ / PR+ tumors, however, refuse endocrine therapy for a variety of personal reasons, and recent studies have suggested that differences in prognosis and outcome exist that are independent of adjuvant therapy (2). The small sample size of our patient population, particularly those with receptor data, must be considered a weakness of the study. As noted already, our results were nonetheless statistically significant despite the small sample size, which speaks for the strength of the observed correlation. A prospective study with a larger sample size and stratification for adjuvant therapy would be of value to validate these findings further.
Although it is uncertain why hormone receptor status influences the pattern of metastatic disease spread, at least two possibilities seem quite plausible. First, hormone receptors on a cell surface might influence where a tumor cell, which is passing through the bloodstream, implants and begins growing. Second, tumor cells that have implanted in various regions throughout the body might selectively flourish in tissues where hormone levels are relatively higher (or lower) than other tissues.
Conclusion
We observed two common patterns of disease spread in metastatic breast carcinoma, excluding patients with extensive diffuse metastases. Patients with ER+ / PR+ tumors tended to develop osseous spread but no brain metastases. Patients with ER− / PR− tumors tended to develop brain metastases but tended not to develop osseous metastases. Appreciation of these distributions will aid the radiologist in the detection of metastatic lesions, and may serve to allow structured follow-up imaging of these patients. For example, it may be appropriate to follow up patients with ER+ / PR+ tumors with frequent skeletal scintigraphy, only performing brain MR imaging if symptoms develop that suggest CNS disease. Similarly, it may be appropriate to follow up patients with ER− / PR− tumors with intermittent brain MR imaging, perhaps using double or triple-dose gadolinium (8) for enhanced sensitivity, but only to perform skeletal scintigraphy if new symptoms develop that suggest osseous spread. Knowledge of these patterns of metastases will also help the clinician to estimate the likelihood of metastases to various organ systems, which may potentially allow targeted prophylactic therapy.
Estrogen/progesterone receptor data
Footnotes
Address reprint requests to Robert I. Grossman, MD, Dept. of Radiology, One Silverstein, Hospital of the University of Pennsylvania, 3400 Spruce St., Philadelphia, PA 19104.
References
- 1.Ries LAG, Kosary CL, Hankey BF, Miller BA, Harras A, Edwards BK, eds SEER Cancer Statistics Review, 1973–1994. Bethesda, MD: National Cancer Institute 1997;124:97-2789 [Google Scholar]
- 2.Pichon MF, Broet P, Magdelenat H, et al. Prognostic value of steroid receptors after long-term follow-up of 2257 operable breast cancers. Br J Cancer 1996;73:1545-1551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sheikh MS, Garcia M, Pujol P, Fontana JA, Rochefort H. Why are estrogen-receptor-negative breast cancers more aggressive than the estrogen-receptor-positive breast cancers? Invas & Metast 1994;14:329-336 [PubMed] [Google Scholar]
- 4.Warde P, Detsky AS. Is steroid receptor data useful in patients with metastatic breast cancer? Am J Med Sci 1992;304:9-13 [DOI] [PubMed] [Google Scholar]
- 5.Alanko A, Heinonen E, Scheinin T, Tolppanen EM, Vihko R. Significance of estrogen and progesterone receptors, disease-free interval, and site of first metastasis on survival of breast cancer patients. Cancer 1985;56:1696-1700 [DOI] [PubMed] [Google Scholar]
- 6.De la Monte SM, Hutchins GM, Moore GW. Estrogen and progesterone receptors in prediction of metastatic behavior of breast carcinoma. Am J Med 1984;76:11-17 [DOI] [PubMed] [Google Scholar]
- 7.Koenders PG, Beex LV, Langens R, Kloppenborg PW, Smals AG, Benraad TJ. Steroid hormone receptor activity of primary human breast cancer and pattern of first metastasis. The Breast Cancer Study Group. Breast Ca Res & Treat 1991;18:27-32 [DOI] [PubMed] [Google Scholar]
- 8.Yuh WT, Fisher DJ, Runge VM, et al. Phase III multicenter trial of high-dose gadoteridol in MR evaluation of brain metastases. AJNR Am J Neuroradiol 1994;15:1037-1051 [PMC free article] [PubMed] [Google Scholar]


