Abstract
BACKGROUND AND PURPOSE: Although prefrontal lobotomy is an obsolete treatment for schizophrenia, we still encounter patients who have undergone this procedure. The purpose of this study was to describe the MR imaging findings of sequelae of prefrontal lobotomy.
METHODS: We retrospectively reviewed cranial MR images of eight patients with schizophrenia who underwent prefrontal lobotomy approximately 50 years previously.
RESULTS: In all patients, a bilateral cavitary lesion with a thick wall was found in the frontal white matter. The genu of the corpus callosum was mildly to markedly atrophic. The size and location of the cavity and the degree of callosal atrophy were correlated.
CONCLUSION: MR imaging is useful for the diagnosis of sequelae of prefrontal lobotomy, including cavitary lesions with dense walls of gliosis and secondary degeneration of the genu of the corpus callosum.
In 1935, Moniz (1), a Portuguese neurologist, first reported “prefrontal leucotomy” for the treatment of mental disorders. In the 1940s, Freeman and Watts (2) developed a modified “prefrontal lobotomy” procedure that was quickly adopted worldwide. This psychosurgery produced a good therapeutic response, and in 1949, Moniz won the Nobel Prize in physiology for his discovery. Popularity of prefrontal lobotomy decreased during the 1960s after the development of effective psychopharmacologic agents, including chlorpromazine, for the treatment of mental diseases (3).
Patients with schizophrenia who have undergone prefrontal lobotomy still live in mental hospitals. As seen on CT scans, the prefrontal lobotomy has a symmetrical white matter cavitary lesion in the anterior portion of the frontal lobes (3–9). MR imaging of the prefrontal lobotomy rarely has been reported (10, 11). We report the cranial MR imaging findings of eight patients who underwent prefrontal lobotomy approximately 50 years previously.
Methods
During the past 3 years, eight patients with schizophrenia who had undergone prefrontal lobotomy underwent MR imaging in a national psychiatric hospital. The patients were six men and two women, ranging in age from 63 to 84 years at the time of MR imaging, with a mean age of 73 years (Table). The patient age at the time of lobotomy ranged from 18 to 38 years (unknown for patient 8), with a mean age of 26 years. MR imaging was performed a mean of 47 years after prefrontal lobotomy.
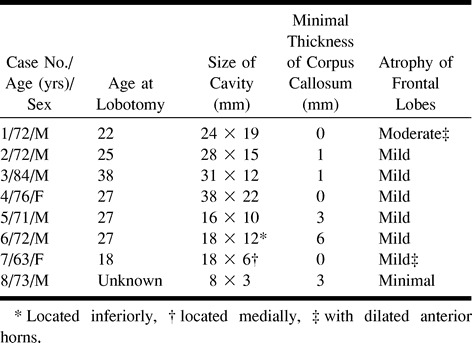
Characteristics and MR findings in eight schizophrenic prefrontal lobotomy patients
MR imaging was performed on a 1.0-T scanner (Shimadzu; Magnex XP, Kyoto, Japan) with a quadrature head coil. Sagittal and axial T1-weighted images (spin-echo, 325/12 [TR/TE], and spin-echo, 520/12), axial T2-weighted images (fast spin-echo, 4300/110), and axial fast fluid-attenuated inversion recovery (FLAIR) images (6744/1588/110 [TR/TI/TE]) were obtained. The field of view was 22 × 22 cm. The section thickness was 6 mm with a 1-mm intersection gap. The imaging matrix was 256 × 256. The number of excitations was 2 or 4. FLAIR images and midsagittal T1-weighted images were reviewed retrospectively and analyzed by an experienced neuroradiologist (A.U.).
Results
In all patients, a cavitary lesion containing a fluid resembling CSF was found bilaterally and nearly symmetrically in the anterior portion of the frontal white matter (Figs 1A and 2). The maximum diameter of the cavities varied from 8 to 38 mm. The cavities were relatively large in four patients and relatively small in the other four. Small cavities were located medially (Fig 3A and B) in one patient and inferiorly in another. Each cavitary lesion was surrounded by a thick wall of hyperintensity, shown on the FLAIR images.
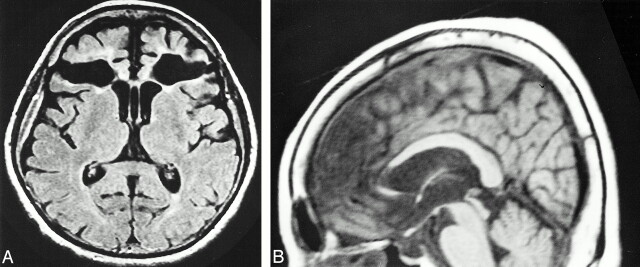
fig 1.
Images of patient 4.
A, Axial FLAIR image shows a large bilateral cavitary lesion containing CSF-like fluid with a thick wall in the frontal white matter. The cortical sulci of bifrontal lobes are dilated mildly. The cavum septum pellucidum is also observed.
B, Midsagittal T1-weighted image shows markedly atrophic genu of the corpus callosum.
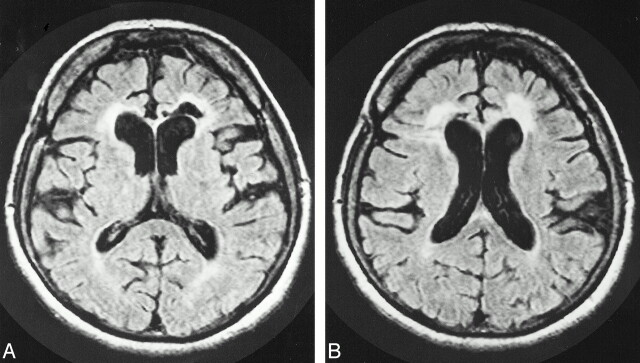
fig 3.
Images of patient 7.
A and B, Two contiguous axial FLAIR image shows a small bilateral cavitary lesion in the medial frontal white matter. The cortical sulci of bifrontal lobes are dilated mildly. Markedly atrophic genu of the corpus callosum was observed on the midsagittal T1-weighted image (not shown).
In all patients, the cortical sulci of the anterior frontal lobes and/or the frontal horns of the lateral ventricles were dilated minimally to moderately, indicative of focal brain atrophy. The genu of the corpus callosum was mildly to markedly atrophic in all patients. The degree of these secondary changes was correlated to the size of the cavitary lesions (Fig 1B). In one patient with small cavities located medially, the corpus callosum was markedly atrophic. In another patient, with inferiorly located cavities, the corpus callosal atrophy was mild. The only other focal abnormality detected was arteriosclerotic small white matter lesions. Thalamic lesions were not detected.
Discussion
Various prefrontal lobotomy procedures have existed. Moniz (1) initially used injection of alcohol into the frontal white matter via burr holes in the dorsal skull. He soon invented a metal probe with a small wire loop at its end, called a leucotome. Freeman and Watts (2) introduced a transorbital approach to the frontal white matter and an ice pick type of instrument. This Freeman-Watts operation was easier and was associated with fewer complications than those found in the Moniz procedure. All patients in our study seemed to have undergone this second-generation operation, but size and location of destroyed brain tissue differed in each patient. Neurologic outcomes for patients who have undergone prefrontal lobotomy are as good as that of well-matched psychiatric controls (10, 12–14). Current treatment with neuroleptics and previous treatment with lobotomy cannot account for the poor cognitive performance of the older schizophrenic patients (15, 16). Naeser et al (6) reported that the patients who achieved good recovery had significantly larger lesions in the low orbitofrontal region (especially in the left) than did patients who achieved moderate or no recovery. Prefrontal lobotomy produces an increased incidence of seizures (3). The incidence of homicides after lobotomy is extremely high considering that all patients were kept under continuous observation in hospitals (9). We did not analyze neuropsychiatric outcome in this study. Glioblastoma rarely arises at the lobotomy site, but the relationship between glioblastoma and previous lobotomy is unclear (17, 18).
Lobotomy is an aseptic iatrogenic trauma to the brain. The loss of injured tissue secondary to a prefrontal lobotomy results in bilateral cavitary lesions with fanlike shapes that are surrounded by dense gliosis (5). CT scans revealed that these lesions were CSF attenuation cavities (3–9). The surrounding unenhanced gliosis was unidentified on CT scans (4). The pathologic sequelae of prefrontal lobotomy in our patients were well revealed by MR imaging FLAIR pulse sequences. The fluid-containing cavity was hypointense, and the surrounding gliosis was hyperintense.
Several neuropathologic studies of patients who underwent lobotomy showed atrophy of the frontal lobes and degenerative changes in the nucleus medialis thalami (2). According to the postmortem morphologic study by Pakkenberg (19), white matter and central gray structures of lobotomized brains were significantly reduced compared with a group of nonlobotomized schizophrenic brains. In patients with schizophrenia who have undergone lobotomy, the total number of nerve cells in the mediodorsal thalamic nucleus is statistically significantly reduced (20). The lobotomy-induced destruction of thalamocortical fibers originating in the nucleus medialis is mainly responsible for the postlobotomy behavior alteration. We detected no changes in the thalami or anterior limbs of the internal capsule as seen on MR images. Mild atrophy of these structures may not be identifiable by conventional MR imaging. In a previous study, bilateral frontal lobe atrophy was detected by CT as a secondary brain degeneration after prefrontal lobotomy (3, 9). Our patients showed atrophic frontal lobes and corpus callosum. The midsagittal T1-weighted MR images were useful in revealing corpus callosal abnormalities. The genu of the corpus callosum was atrophic in all patients, indicative of a wallerian degeneration of the connecting fibers (21). The size of the cavity correlated with the degree of callosal atrophy. One patient with medially located small cavities had a markedly atrophic corpus callosum, and another patient with inferiorly located cavities had a mildly atrophic corpus callosum. This contrast is probably due to different numbers of destroyed connecting fibers.
Differential diagnosis of prefrontal lobotomy includes sequelae of old contusions. In the case of head trauma, both cerebral cortex and white matter are damaged. In the case of prefrontal lobotomy, lesions do not involve the cortex except for the needle entry site. Bilateral border zone infarctions between the anterior and middle cerebral arteries should be differentiated from prefrontal lobotomy. Border zone infarctions usually have their maximum diameters in the anteroposterior directions, and central cavities are rarely seen. Without knowledge of patient history, prefrontal lobotomy can be easily diagnosed by using CT or MR imaging. MR imaging is more effective than CT in the diagnosis of prefrontal lobotomy and its secondary degenerations.
Conclusion
Although prefrontal lobotomy is an obsolete treatment for schizophrenia, patients who have undergone lobotomy continue to reside in mental hospitals. MR imaging is useful for the diagnosis of sequelae of prefrontal lobotomy and its secondary degenerations.
fig 2.
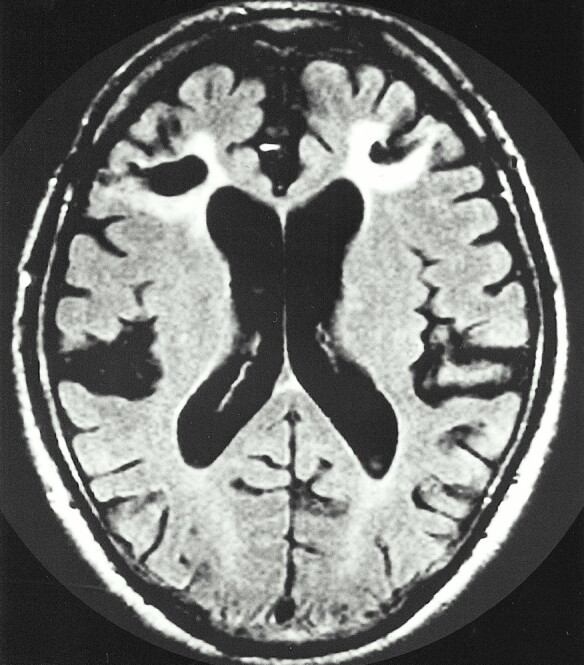
Axial FLAIR image of patient 5 shows a small cavity with a thick wall in the bifrontal white matter. The bifrontal cortical sulci are dilated mildly. Moderately atrophic genu of the corpus callosum was observed on the midsagittal T1-weighted image (not shown)
Footnotes
Address reprint requests to Akira Uchino, MD, Department of Radiology, Saga Medical School, 5-1-1, Nabeshima, Saga 849-8501, Japan.
References
- 1.Moniz E. Prefrontal leucotomy in the treatment of mental disorders. Am J Psychiatry 1937;93:1379-1385 [DOI] [PubMed] [Google Scholar]
- 2.Freeman W, Watts JW. Retrograde degeneration of the thalamus following prefrontal lobotomy. J Comp Neurol 1947;86:65-93 [DOI] [PubMed] [Google Scholar]
- 3.Engelborghs S, Borggreve F, Pickut BA, Michiels K, Van de Mosselaer W, De Deyn PP. Case report of a patient with complex partial frontal lobe seizures as a complication of bifrontal lobotomy. Acta Neurol Belg 1998;98:199-203 [PubMed] [Google Scholar]
- 4.Banna M, Adams K, Tunks E, Finlayson MAJ. Computed tomography after psychosurgery. J Comput Assist Tomogr 1978;2:98-99 [DOI] [PubMed] [Google Scholar]
- 5.Duncan AW, Schoene WC, Rumbaugh CL. The computerized tomographic appearance of frontal lobotomy. Comput Tomogr 1980;4:255-260 [DOI] [PubMed] [Google Scholar]
- 6.Naeser MA, Levine HL, Benson DF, Stuss DT, Weir WS. Frontal leukotomy size and hemispheric asymmetries on computerized tomographic scans of schizophrenics with variable recovery: Northampton Veterans Administration study. Arch Neurol 1981;38:30-37 [DOI] [PubMed] [Google Scholar]
- 7.Benson DF, Stuss DT, Naeser MA, Weir WS, Kaplan EK, Levine HL. The long-term effects of prefrontal leukotomy. Arch Neurol 1981;38:165-169 [DOI] [PubMed] [Google Scholar]
- 8.Dorland JP, Dorland PR, Cioloca C. Computerized tomographic sequelae of frontal psychosurgery. J Neuroradiol 1986;13:195-208 [PubMed] [Google Scholar]
- 9.Hakola HP, Puranen M, Repo L, Tiihonen J. Long-term effects of bilateral frontal lobe lesions from neuropsychiatric and neuroradiological aspects. Dementia 1993;4:109-112 [DOI] [PubMed] [Google Scholar]
- 10.Karp BPI, Juliano DM, Berman KF, Weinberger DR. Neurologic outcome of patients with dorsolateral prefrontal leukotomy. J Neuropsychiatry Clin Neurosci 1992;4:415-421 [DOI] [PubMed] [Google Scholar]
- 11.Weinberger DR, Goldberg TE, Tamminga CA. Images in neuroscience: cortex, V. Prefrontal leukotomy. Am J Psychiatry 1995;152:330-331 [DOI] [PubMed] [Google Scholar]
- 12.Wehler R, Hoffmann H. Intellectual functioning in lobotomized and non-lobotomized long term chronic schizophrenic patients. J Clin Psychol 1978;34:449-451 [DOI] [PubMed] [Google Scholar]
- 13.Stuss DT, Benson DF, Kaplan EF, Weir WS, Della Malva C. Leucotomized and nonleucotomized schizophrenics: comparison on tests of attention. Biol Psychiatry 1981;16:1085-1100 [PubMed] [Google Scholar]
- 14.Benson DF, Stuss DT. Motor abilities after frontal leukotomy. Neurology 1982;32:1353-1357 [DOI] [PubMed] [Google Scholar]
- 15.Harvey PD, Mohs RC, Davidson M. Leukotomy and aging in chronic schizophrenia: a follow up study 40 years after psychosurgery. Schizophr Bull 1993;19:723-732 [DOI] [PubMed] [Google Scholar]
- 16.Davidson M, Harvey PD, Powchik P, et al. Severity of symptoms in chronically institutionalized geriatric schizophrenic patients. Am J Psychiatry 1995;152:197-207 [DOI] [PubMed] [Google Scholar]
- 17.Ogashiwa M, Muraoka I, Nakano H, Uesugi S, Okuma T. An autopsy case of glioblastoma occurred in the region after lobotomy. No To Shinkei 1990;42:1067-1073 [PubMed] [Google Scholar]
- 18.Fukushima H, Yamaguchi T, Arai T, et al. A case of glioblastoma manifesting 49 years after lobotomy. No To Shinkei 1998;50:755-760 [PubMed] [Google Scholar]
- 19.Pakkenberg B. What happens in the leucotomised brain? A postmortem morphological study of brains from schizophrenic patients. J Neurol Neurosurg Psychiatry 1989;52:156-161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pakkenberg B. Leucotomized schizophrenics lose neurons in the mediodorsal thalamic nucleus. Neuropathol Appl Neurobiol 1993;19:373-380 [DOI] [PubMed] [Google Scholar]
- 21.Anderson CV, Bigler ED. The role of caudate nucleus and corpus callosum atrophy in trauma-induced anterior horn dilation. Brain Inj 1994;8:565-569 [DOI] [PubMed] [Google Scholar]