Abstract
Summary: Irregular, concentric zones of increased signal on T2-weighted cranial MR imaging studies may strongly suggest Balo concentric sclerosis (BCS), a rare but recognized variant of multiple sclerosis. Differentiating BCS from multiple sclerosis or neoplasm can be difficult clinically, but MR imaging findings noted in this case may be pathognomonic.
Balo concentric sclerosis (BCS) is widely believed to be a rare variant of multiple sclerosis. It may present as clinically similar to multiple sclerosis, affecting young adults with mild cognitive impairment without frank dementia, or be associated with altered behavior and focal CNS deficits. Historically, the diagnosis was made post mortem or histopathologically in the presence of specific CNS lesions consisting of concentric rings of demyelination alternating with myelinated white matter. Current literature and research, however, suggest that BCS exhibits characteristic radiographic findings that aid in antemortem diagnosis (1). The following case further confirms this impression. Additionally, differentiating between demyelinating lesions and CNS tumors, such as gliomas, in the presence of solitary lesions has always been difficult and problematic. The pathognomonic MR imaging findings presented herein resolve this issue. Finally, initial reports of BCS also predicted that the disease was rapidly progressive and fatal (2), but others have concluded that antiinflammatory corticosteroids have shown efficacy against neurologic deficits associated with BCS (3). Therefore, the role of MR imaging in patients with BCS can dramatically influence the course of the disease, allowing earlier diagnosis and therapy.
Case Report
A 34-year-old right-handed Caucasian woman accompanied by her parents was admitted to an outlying hospital. Her parents reported that 5 days earlier she had exhibited some questionable seizure activity followed by 2 days of a continuous facial and motor retardation described as a “blank stare.” During the next 2 or 3 days, the patient displayed limited verbal ability, responding only to questions and with one- or two- word answers. CT scanning and MR imaging initially suggested a left frontal lobe lesion with minimal mass effect. Importantly, no other lesions were seen. Her symptoms were tentatively explained by a suspected tumor of the superior and middle frontal gyri anterior to the Rolandic fissure and adjacent vasogenic edema, which was producing an expressive aphasia, typical of a Broca aphasia. The patient underwent a stereotactically guided biopsy to confirm the clinician's suspicion.
Specimens from the biopsy were sent for definitive pathologic determination, and immediate frozen pathologic sections suggested that the lesion was likely a malignant glioma, either an anaplastic astrocytoma or glioblastoma multiforme. As a result, the patient was referred to a local National Cancer Institute Designated Cancer Center for consultation, evaluation, and treatment. Approximately 2 weeks after the biopsy, a final histologic impression was rendered and revealed the lesion contained abundant reactive astrocytes, many lipid-laden macrophages and rare lymphocytes without atypical glial cells, mitotic figures, and necrosis or vascular proliferation and was consistent with an inflammatory demyelinating process.
A review of initial and follow-up MR imaging studies revealed that the lesion was consistent with a demyelinating process without any mass effect. A distinct pattern of concentric demyelination suggested the diagnosis of BCS in contrast to a neoplastic process. The final diagnosis of BCS was made because of the patient's clinical findings (4, 5) in association with the pathologic analysis and follow-up contrast-enhanced MR imaging studies revealing characteristic lesions.
Discussion
This case report supports the limited but growing body of evidence for a classical MR imaging appearance of BCS (An MD Consult literature search consisting of over 50 selected clinical journals and Clinics of North America plus complete MEDLINE, AIDSLINE, HealthSTAR, and CANCERLIT citations revealed eight documented reports of BCS). BCS is a rare demyelinating disease related to multiple sclerosis. Concentric lesions of demyelination occur while sparing adjacent white matter in a pattern that is directly identifiable on contrast- enhanced MR imaging. The ability of MR imaging to diagnose BCS earlier in its progression may have a significant effect on morbidity and mortality associated with the disease.
Characteristic MR findings suggest the diagnosis of BCS in lieu of previous postmortem histologic analysis. T2-weighted images suggest separate concentric zones of demyelination (Fig 1A). T1-weighted images following administration of IV Gd-DTPA readily depict separate rings of enhancement at sites of increased blood brain–barrier permeability and inflammatory white cells responsible for demyelination in a characteristic concentric pattern (Fig 1B). As a result of the pathognomonic MR imaging findings clearly identified in our case, the role of MR imaging in diagnosis may prove to influence the morbidity and mortality of BCS significantly by allowing clinicians earlier diagnosis of and intervention for patients suffering from this unusual but radiographically distinct variant of multiple sclerosis.
fig 1.
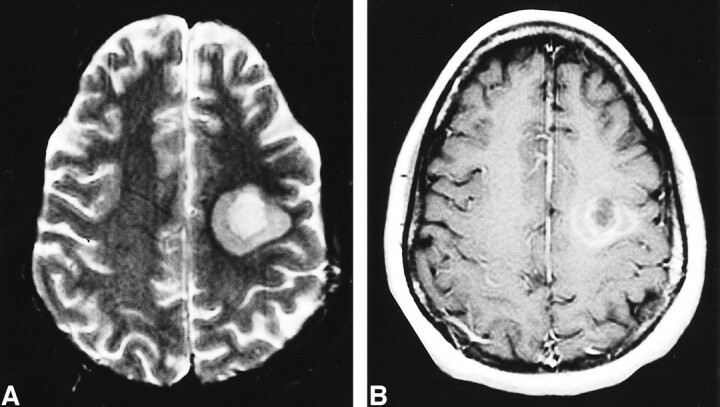
A, Fast spin-echo T2-weighted axial MR image through the centrum semiovale. This shows two separate concentric zones of demyelination in the left frontoparietal deep white matter represented as two different degrees of increased T2 signal (5300/82.2/1 [TR/TE/excitations]).
B, T1-weighted axial MR image after IV administration of Gd-DTPA at the same level as A. This clearly depicts multiple enhancing concentric rings representing two separate zones of active demyelination and increased blood brain–barrier permeability (550/9/1).
In contrast to multiple sclerosis, BCS is believed to run a fulminant and fatal course (6, 7). With the application of radiographic techniques, however, BCS can be identified earlier when the characteristic pattern of demyelination is seen. As a result, early interventional therapy can be instituted to provide symptomatic relief and slow the progression of inflammatory demyelination. Specifically, reports of clinical improvement after the administration of corticosteroids (ie, prednisolone 60mg/d) have been published (3, 8).
Various theories have been proposed to explain the pathogenesis of BCS and radiographic findings. Early researchers suggested that the alternating zones of myelinated and demyelinated white matter reflected a vascular obstructive process resulting from embolization of lipid particles produced at primary multiple sclerosis lesions (7). Others have hypothesized that the areas of myelination represent regions of remyelination at the outer edges of multiple sclerosis plaques after acute demyelination (4). More recent reports dismiss the notion of remyelination and suggest that the regions of myelination are more indicative of myelin breakdown at an earlier stage of development than seen in frank demyelination. These same reports highlight the limited supportive evidence for the role of toxins and infectious/inflammatory agents in the pathogenesis of BCS (5).
This report confirms that a pathognomonic MR imaging appearance is present in BCS. The alternating zones of demyelinated and myelinated white matter best appreciated on MR imaging after IV administration of Gd-DTPA presented in this case define BCS. The difficulty in differentiating this rare demyelinating process from the more common entities such as multiple sclerosis and CNS neoplasm can be eliminated when the classical lesion outlined herein exists.
Footnotes
Address reprint requests to Jamie T. Caracciolo, University Diagnostic Institute, 3301 Alumni Drive, Tampa, FL 33612-9413.
References
- 1.Chen C-J, Chu N-S, Lu C-S, Sung C-Y. Serial magnetic resonance imaging in patients with Balo's concentric sclerosis: natural history of lesion development. Ann Neurol 1999;46:651-656 [DOI] [PubMed] [Google Scholar]
- 2.Chen CJ, Ro LS, Wang LJ, Wong YC. Balo's concentric sclerosis: MRI. Neuroradiology 1996;38:322-324 [DOI] [PubMed] [Google Scholar]
- 3.Ng S-H, Ko S-F, Cheung Y-C, Wong H-F, Wan Y-L. MRI features of Balo's concentric sclerosis. Br J Radiol 1999;72:400-403 [DOI] [PubMed] [Google Scholar]
- 4.Moore W, Neumann PE, Suzuki K, et al. Balo's concentric sclerosis: new observations on lesion development. Ann Neurol 1985;17:604-611 [DOI] [PubMed] [Google Scholar]
- 5.Yao L, Webster H, Hudson L, et al. Concentric sclerosis (Balo): morphometric and in situ hybridization study of lesions in six patients. Ann Neurol 1994;35:18-30 [DOI] [PubMed] [Google Scholar]
- 6.Balo J. Encephalomyelitis periaxialis concentrica. Arch Neurol Psychiatry 1928;19:242-264 [Google Scholar]
- 7.Courville CB. Concentric sclerosis. In: Vincken PJ, Bruyn GW, eds. Handbook of Clinical Neurology, Volume 9. Amsterdam: North Holland 1970;437-451
- 8.Bolay H, Karabudak R, Tacal T, Onol B, Selekler K, Saribas O. Balo's concentric sclerosis: report of two patients with magnetic resonance imaging follow-up. J Neuroimag 1996;6:98-103 [DOI] [PubMed] [Google Scholar]


